Abstract
Introduction
Bone loss caused by primary hyperparathyroidism (PHPT) is an indication for parathyroidectomy (PTX). However, whether adding bisphosphonates would be superior to PTX alone to increase bone mass remains unclear. We thus aimed to compare the skeletal effects of the combination treatment of bisphosphonates and PTX with PTX alone.
Materials and methods
In this retrospective analysis, bone mineral density (BMD) changes after 1 year of combination treatment and PTX alone were compared. We also analyzed the correlation between changes in serum biochemical parameters and BMD after 1 year of treatment in both groups.
Results
The baseline characteristics of patients treated with PTX alone (n = 24) and combination treatment (n = 26) were comparable. BMD significantly increased after 1 year of treatment in both groups (all p < 0.001), and the increase in BMD at the femur neck was higher in the PTX alone group than in the combination group (p = 0.011). There was a decreasing trend in serum alkaline phosphatase (ALP) levels in PTX alone compared to the combination treatment group (p = 0.053). In the study cohort, lower BMD and higher ALP levels at baseline were associated with higher 1-year BMD changes at all sites. Interestingly, a significant association was found between changes in ALP and BMD at the femur neck in the PTX alone group (p = 0.003), but abolished in the combination group (p = 0.946).
Conclusions
There is no additional benefit of BMD in combination treatment with bisphosphonates and PTX over PTX alone in osteoporotic patients with PHPT. Combined bisphosphonate treatment might interfere with the increase in bone mass caused by PTX.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (PHPT) is characterized by hypercalcemia and elevated parathyroid hormone (PTH) levels. It can present as a wide spectrum of disease severity, from asymptomatic to grave disease with multiple complications, including skeletal and renal manifestations, increased incidence of cardiovascular disease, and neuropsychiatric diseases [1, 2]. Of these, skeletal involvement is a significant concern, as consistently increased PTH levels stimulate bone resorption, resulting in low bone mineral density (BMD) and subsequent fracture [3].
Bone disease of PHPT is characterized by an increase in the activation frequency of bone multicellular units (BMUs), resulting in an enlarged bone remodeling space. In particular, cortical bone porosity and endocortical bone resorption are increased, leading to cortical bone loss. These ultrastructural events account for the increase in markers of bone turnover and changes in bone mass. Because of the subsequently increased fracture risk, treatment approaches to increase BMD have garnered attention over the past few decades.
Currently, the only definitive treatment for PHPT is parathyroidectomy (PTX). PHPT patients with osteoporosis fulfill the criteria for surgical treatment to effectively reduce fracture risk [4,5,6], but those who refuse or are unable to undergo PTX due to comorbidities receive medical treatment as an alternative option [7, 8]. Biochemical parameters and BMD improved to a certain extent in patients who received a combination of cinacalcet and antiresorptive agents [9,10,11,12]. In a 10-year follow-up study investigating fracture risk, however, patients treated with bisphosphonates did not show superior results compared to the observation group, whereas patients that have received PTX had reduced fracture risk [13].
In clinical practice, a number of patients who undergo PTX are already on bisphosphonates or receive bisphosphonates postoperatively for adjuvant skeletal effects. Patients who were previously treated with bisphosphonates for osteoporosis may conjointly be diagnosed with PHPT and receive PTX afterwards. Whether this combination therapy would lead to an increased BMD compared to PTX alone, however, remains to be elucidated. In this study, we aimed to compare the combined effects of bisphosphonates and PTX compared to PTX alone.
Materials and methods
Patients
We retrospectively analyzed patients admitted to Seoul National University Hospital and Seoul Metropolitan Government Boramae Medical Center between January 2001 and June 2020. Patients were eligible for analysis if they had received a diagnosis of both PHPT and osteoporosis.
PHPT was diagnosed biochemically as hypercalcemia with high or inappropriately normal PTH levels. Patients with relatively normal serum calcium levels of 10.5 mg/dL or less were also diagnosed with primary hyperparathyroidism if they had an elevated PTH level after all known causes of secondary hyperparathyroidism were excluded. Osteoporosis was diagnosed if the BMD T score measured by dual-energy X-ray absorptiometry (DXA) scans was − 2.5 or less, in the lumbar spine (LS), femur (FN), or total hip (TH). Patients with previous fragility fractures were also defined as having osteoporosis regardless of baseline BMD.
Patients who did not have baseline DXA scans or follow-up data were excluded from the analysis. Patients who were treated with other osteoporosis drugs and those who had received bisphosphonate treatment for one or more years prior to PTX were also excluded. We additionally excluded patients with chronic kidney disease with a baseline estimated glomerular filtration rate of less than 45 mL/min/1.73 m2, and patients concomitantly diagnosed with malignancy. This is because the diagnosis of true PHPT may be obscured, and bisphosphonate may be used for purposes other than the treatment of osteoporosis for the latter, such as correcting hypercalcemia secondary to paraneoplastic syndrome.
Patients who received PTX alone were classified as group 1, and those who received bisphosphonate treatment for less than 6 months before PTX or were initiated within 6 months of PTX were designated as group 2. For clarity, only patients who used bisphosphonates for 1 year or longer were included. This study was conducted in accordance with the ethical standards of the Declaration of Helsinki and the national and international guidelines. This study was approved by the Institutional Review Board of Seoul National University Hospital (approval number: H-1306-101-499).
Outcome measurements
As regards clinical data, we reviewed the electronic medical records: sex, age, height, weight, menopause, diabetes mellitus, hypertension, cigarette smoking, alcohol consumption, history of fracture, family history of fracture, history of stone, and prescribed bisphosphonates and calcium/vitamin D supplements.
Laboratory parameters including serum calcium, ionized calcium, phosphorus, C-telopeptide, alkaline phosphatase (ALP), blood urea nitrogen, serum creatinine, glucose, 25-hydroxyvitamin D3, and PTH levels were evaluated. Serum 25-hydroxyvitamin D3 concentration was measured by Diels–Alder derivatization and ultra-high-performance liquid chromatography–tandem mass spectrometry using XevoTQ (Waters, Milford, MA, USA). The circulating concentration of intact PTH in serum was measured by an electrochemiluminescence immunoassay on the Modular Analytics E170 platform (Roche, Mannheim, Germany).
DXA (Prodigy™, Lunar, GE Medical Systems, Madison, WI, USA) was performed at the LS, FN, and TH to assess BMD. The change in BMD during the follow-up was assessed as follows: [current BMD (g/cm2) − baseline BMD (g/cm2)] × 100/baseline BMD (g/cm2).
The primary outcome was the change in BMD during the first year of follow-up. Secondary outcomes included changes in BMD over 2 years of follow-up and changes in biochemical parameters.
Statistical analyses
Baseline characteristics are presented as the mean ± standard deviation or number (%). Pearson’s Chi-squared tests were used to compare categorical variables, and independent t tests were used for normally distributed continuous variables. Normality of the data was examined with Kolmogorov–Smirnov test and Shapiro–Wilk test. For continuous variables that did not follow normal distribution, Mann–Whitney tests were performed.
Follow-up BMD data and biochemical parameters in each group were compared with baseline values using paired t tests, and changes in outcome variables by treatment groups were assessed using a generalized estimating equation. Correlational analysis was performed on potential variables to identify the relevant predictors of BMD change over the first year of follow-up. All statistical analyses were performed using SPSS version 25 (Statistical Package for the Social Sciences, IBM Corporation, Armonk, NY, USA). A two-sided p value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 447 patients from Seoul National University Hospital and Seoul Metropolitan Government Boramae Medical Center between January 2001 and June 2020 were screened. Of these, 93 patients did not have baseline DXA data, 44 patients did not receive PTX and 29 patients were diagnosed with malignancy or CKD. After excluding patients who did not meet the criteria for the duration of perioperative bisphosphonate treatment, and those who did not have adequate follow-up data, 50 patients were finally eligible for analysis. There were 24 patients who received PTX alone and 26 patients who received the combination treatment of both PTX and bisphosphonates (Supplementary Fig. 1). The choice of bisphosphonate treatment is listed in Table 1.
The mean age of patients in both groups were 62.1 ± 9.9 years, and 85.1% were women. The clinical and demographic characteristics of both treatment groups were well balanced with respect to age, sex, menopausal status, underlying comorbidities, baseline BMD, and laboratory parameters (Table 1). Patients in the combination group had shorter stature, weighed less, and had a higher proportion of calcium and/or vitamin D supplements at baseline. The proportion of normocalcemic PHPT were similar in both groups.
Longitudinal change in BMD and biochemical parameters
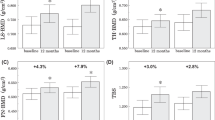
At 1 year after treatment, BMD significantly increased at LS, FN, and TH compared to baseline BMD in both groups (group 1: 16.17 ± 15.56%, 12.87 ± 12.79%, 12.22 ± 11.81%, group 2: 15.56 ± 17.63%, 6.62 ± 5.25%, 7.64 ± 5.41% for LS, FN, and TH, respectively; Table 2, Fig. 1). The extent of BMD increment was not different between the two groups, except for in FN, where group 1 had a higher increase in 1-year BMD compared to group 2 (group 1: 0.682 ± 0.104 vs. 0.766 ± 0.122 g/cm2, group 2: 0.639 ± 0.079 vs. 0.679 ± 0.068 g/cm2, respectively; p for interaction 0.009, Table 2). This trend remained consistent 2 years after treatment in both groups (Supplementary Table 1). Within group 2, no significance difference was observed between the patients who received before or after PTX. Further investigation revealed no interaction between initial hypercalcemic status and BMD change (p for interaction 0.810, 0.386, 0.720 for LS, FN, and TH, respectively; Table 2, Supplementary Table 1).
Changes in BMD according to treatment with parathyroidectomy alone or in combination with bisphosphonates. a Lumbar spine, b Femur neck, c Total hip. BMD, bone mineral density; PTX parathyroidectomy. Data are presented as the mean ± SEM. *p < 0.05, **p < 0.01, and ***p < 0.001 versus baseline value. #p < 0.05, versus treatment groups
In terms of the biochemical parameters, serum calcium, ionized calcium, phosphorus, PTH, and ALP normalized, and C-telopeptide decreased substantially 1 year after treatment in both groups (Table 2). In the study cohort, a decreasing trend was observed in serum ALP levels in group 1 compared to group 2 (p = 0.053). There was no significant difference in the extent of change in any of the other biochemical parameters between the treatment groups.
Association between change in BMD and biochemical parameters
Next, we performed correlation analysis to explore parameters that may be associated with 1-year BMD changes. Lower baseline BMD was significantly associated with higher BMD change (%) at 1 year after treatment at all measured sites (Spearman’s correlation coefficient r = − 0.376, − 0.467, − 0.430, p = 0.007, 0.001, 0.002 at LS, FN, and TH, respectively; Table 3, Fig. 2).
Changes of serum parameters according to treatment with parathyroidectomy alone or in combination with bisphosphonates. a Calcium, b phosphorus, c PTH, d C-Telopeptide, e 25(OH) Vitamin D, f ALP. ALP Alkaline phosphatase, PTX parathyroidectomy. Data are presented as the mean ± SEM. *p < 0.05, **p < 0.01, and ***p < 0.001 versus baseline value
Higher serum ALP at baseline was also strongly associated with BMD increase at 1 year (r = 0.336, 0.437, 0.570, p = 0.022, 0.004, < 0.001 at LS, FN, and TH, respectively; Table 3). When we performed analysis separately by treatment groups, the association remained significant only in group 1 (group 1: r = 0.608, p = 0.003; group 2: r = 0.042, p = 0.864; Table 4). Similarly, serum PTH initially revealed an association with BMD change at the FN site only (r = 0.244, 0.447, 0.215, p = 0.107, 0.004, and 0.162 at LS, FN, and TH, respectively, Table 3); no significant association was noted for group 2, but an association was noted for high baseline PTH in FN and TH sites for group 1 (Table 4).
Higher baseline C-telopeptide was associated with BMD increase in LS and TH, and was marginally significant in the FN area (r = 0.534, 0.348, 0.619, p = 0.001, 0.055, < 0.001 at LS, FN, and TH, respectively; Table 3). C-telopeptide demonstrated a high correlation with BMD change for both group 1 and group 2, even when assessed discretely (Table 4).
Discussion
In this retrospective cohort study, we investigated the skeletal effects of PTX and PTX combined with bisphosphonate treatment in osteoporotic patients with PHPT. BMD was significantly improved in both patients who received PTX alone and in those treated with PTX and bisphosphonates. Combined bisphosphonate treatment, however, did not confer additional benefits regarding BMD 1 year after PTX.
Previous studies have demonstrated a significant increase in BMD following parathyroidectomy. Due to the heterogeneity of PHPT patients undergoing PTX, the extent of BMD gain varies greatly, with one prior meta-analysis reporting a mean BMD change of 4.2% at LS and 3.5% at FN 1 year after PTX [5, 14,15,16,17]. The extent of postoperative increase in BMD is greater in patients with more severe disease and is positively correlated with preoperative serum biochemistry, such as calcium, PTH, and bone turnover markers. The majority of studies have evaluated the BMD response of PHPT patients in general, but not in PHPT patients with osteoporosis. Silverberg et al. [18] demonstrated a marked increase in BMD in PHPT patients with low preoperative BMD, which may explain the considerably higher BMD increase in the present study.
In our study, BMD was significantly improved at all measured sites in both groups 1 year after PTX. A remarkable increase in BMD at sites of the spine and hip, which mainly occurs during the first 6–12 months after PTX, reflects rapid refilling of the extensive remodeling space and the subsequent matrix mineralization [19]. Indeed, there was an average BMD increase of 15% at 1 year and 20% within 4 years after PTX in patients with spine bone loss [20]. No difference was noted between the two treatment groups at LS or TH, but a higher extent of BMD increase was observed at FN in group 1 compared to group 2 1 year after PTX. We also monitored serum parameters following PTX, of which the postoperative 1-year difference between the groups was marginally significant regarding serum levels of ALP only. There was more substantial serum ALP reduction in group 1, and a positive correlation was observed between baseline serum ALP and BMD increase.
The main increase in BMD following PTX seems to arise from a decrease in bone turnover, causing refilling of the remodeling spaces with increased mineralization. A high bone turnover status such as PHPT provokes an alteration in the activation frequency of BMU, subsequently resulting in a decrease in the lifespan of BMU [21]. Conversely, PTX or antiresorptive agents, which cause a remarkable reduction in the rate of bone remodeling, prolong the lifespan of BMU, allowing time for complete secondary mineralization [22].
In addition, there might be a transient postoperative uncoupling of the bone resorption and bone formation phase, resulting in an ‘anabolic window’ after PTX. Bone resorption markers, such as serum carboxy-terminal crosslinks of collagen and urinary deoxypyridoline, rapidly decline within the first 1–3 months after PTX, while bone ALP and osteocalcin, which are markers of bone formation, decline more gradually within 6 months [19]. Another study revealed that in iliac bone biopsy taken before and after PTX in secondary hyperparathyroidism, de novo osteoid formation and mineral apposition at trabecular sites are enhanced, with complete reversal of prior bone resorption within 12 weeks following PTX [23]. This suggests that modeling-based bone formation contributes to the initial increase in bone volume following parathyroidectomy.
Intriguingly, bisphosphonates significantly blunted osteoblast activity in rats [24]. A more recent study also revealed that bisphosphonates might impede osteoprogenitor recruitment required to initiate bone formation at bone remodeling sites [25]. Thus, the use of bisphosphonates in conjunction with PTX may precipitate in further reduction of bone formation than PTX alone, in which bone resorption is scrupulously coupled to bone formation. Bisphosphonates may also interfere with the suppression of expected bone remodeling accompanied by PTX. This result is supported by a previous study that demonstrated a decrease in serum ALP 6 months immediately after alendronate treatment, but not in the succeeding 6 months, whereas serum ALP steadily declined throughout the 12 months following PTX in patients with PHPT [26].
There are several limitations in this study. First, generalizability was constrained by the retrospective nature of this study with a small sample size. Second, only bisphosphonates were evaluated in combination with PTX; use of other antiresorptive agents, such as denosumab, has been reported to not only increase BMD efficaciously in lieu of PTX, but also to improve trabecular bone score [12, 27]. As denosumab does not seem to affect the onset of bone formation at the remodeling site, further studies are warranted to examine the additional effect of denosumab in combination with PTX in the treatment of PHPT with bone loss. Third, radius BMD was not routinely measured in our institution, and cortical bone and trabecular bone were not differentially assessed in this study. Although area BMD is a prevalent measure to assess bone strength, BMD alone is often insufficient to predict future fractures [28]. The recent advent of high-resolution peripheral quantitative computed tomography (HRpQCT) has demonstrated not only decreased cortical perimeter, but also lower trabecular volume in PHPT patients, both of which improved through 2 years following PTX [29]. It would be valuable to implement comprehensive measures such as HRpQCT with a longer follow-up to estimate skeletal microstructure in the future to predict fracture outcomes more precisely.
In conclusion, antiresorptive agents may be a feasible option in patients with PHPT who are unable or unwilling to undergo PTX, but combined perioperative use of bisphosphonates in patients who receive PTX may mitigate the desired skeletal effects. In patients with PHPT accompanied by bone loss, initiation of bisphosphonates shortly before or after PTX may not be warranted.
References
Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE et al (2017) Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int 28:1–19. https://doi.org/10.1007/s00198-016-3716-2
Walker MD, Silverberg SJ (2018) Primary hyperparathyroidism. Nat Rev Endocrinol 14:115–125. https://doi.org/10.1038/nrendo.2017.104
Mosekilde L (2008) Primary hyperparathyroidism and the skeleton. Clin Endocrinol (Oxf) 69:1–19. https://doi.org/10.1111/j.1365-2265.2007.03162.x
Vestergaard P, Mosekilde L (2004) Parathyroid surgery is associated with a decreased risk of hip and upper arm fractures in primary hyperparathyroidism: a controlled cohort study. J Intern Med 255:108–114. https://doi.org/10.1046/j.0954-6820.2003.01237.x
Khan R, Martin J, Das G (2020) The impact of observation versus parathyroidectomy on bone mineral density and fracture risk determined by FRAX tool in patients with primary hyperparathyroidism. J Clin Densitom. https://doi.org/10.1016/j.jocd.2020.12.005
Vestergaard P, Mollerup CL, Frokjaer VG, Christiansen P, Blichert-Toft M, Mosekilde L (2000) Cohort study of risk of fracture before and after surgery for primary hyperparathyroidism. BMJ 321:598–602. https://doi.org/10.1136/bmj.321.7261.598
Marcocci C, Bollerslev J, Khan AA, Shoback DM (2014) Medical management of primary hyperparathyroidism: proceedings of the fourth international workshop on the management of asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab 99:3607–3618. https://doi.org/10.1210/jc.2014-1417
Leere JS, Karmisholt J, Robaczyk M, Vestergaard P (2017) Contemporary medical management of primary hyperparathyroidism: a systematic review. Front Endocrinol (Lausanne) 8:79. https://doi.org/10.3389/fendo.2017.00079
Faggiano A, Di Somma C, Ramundo V, Severino R, Vuolo L, Coppola A, Panico F, Savastano S, Lombardi G, Colao A, Gasperi M (2011) Cinacalcet hydrochloride in combination with alendronate normalizes hypercalcemia and improves bone mineral density in patients with primary hyperparathyroidism. Endocrine 39:283–287. https://doi.org/10.1007/s12020-011-9459-0
Keutgen XM, Buitrago D, Filicori F, Kundel A, Elemento O, Fahey TJ 3rd, Zarnegar R (2012) Calcimimetics versus parathyroidectomy for treatment of primary hyperparathyroidism: retrospective chart analysis of a prospective database. Ann Surg 255:981–985. https://doi.org/10.1097/SLA.0b013e31824c5252
Cetani F, Saponaro F, Banti C, Cianferotti L, Vignali E, Chiavistelli S, Viccica G, Pinchera A, Marcocci C (2012) Cinacalcet efficacy in patients with moderately severe primary hyperparathyroidism according to the European Medicine Agency prescription labeling. J Endocrinol Invest 35:655–660. https://doi.org/10.3275/7970
Leere JS, Karmisholt J, Robaczyk M, Lykkeboe S, Handberg A, Steinkohl E, Frokjaer JB, Vestergaard P (2020) Denosumab and cinacalcet for primary hyperparathyroidism (DENOCINA): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol 8:407–417. https://doi.org/10.1016/S2213-8587(20)30063-2
Yeh MW, Zhou H, Adams AL, Ituarte PH, Li N, Liu IL, Haigh PI (2016) The relationship of parathyroidectomy and bisphosphonates with fracture risk in primary hyperparathyroidism: an observational study. Ann Intern Med 164:715–723. https://doi.org/10.7326/M15-1232
Miguel GA, Carranza FH, Rodriguez JCR, Ramos MA, Pablos DL, Herrero EF, Diaz-Guerra GM (2019) Trabecular Bone Score, bone mineral density and bone markers in patients with primary hyperparathyroidism 2 years after parathyroidectomy. Horm Metab Res 51:186–190. https://doi.org/10.1055/a-0850-8679
Christiansen P, Steiniche T, Brixen K, Hessov I, Melsen F, Heickendorff L, Mosekilde L (1999) Primary hyperparathyroidism: effect of parathyroidectomy on regional bone mineral density in Danish patients: a three-year follow-up study. Bone 25:589–595. https://doi.org/10.1016/s8756-3282(99)00207-0
Nakaoka D, Sugimoto T, Kobayashi T, Yamaguchi T, Kobayashi A, Chihara K (2000) Prediction of bone mass change after parathyroidectomy in patients with primary hyperparathyroidism. J Clin Endocrinol Metab 85:1901–1907. https://doi.org/10.1210/jcem.85.5.6604
Singh Ospina N, Maraka S, Rodriguez-Gutierrez R, Espinosa de Ycaza AE, Jasim S, Gionfriddo M, Castaneda-Guarderas A, Brito JP, Al Nofal A, Erwin P, Wermers R, Montori V (2016) Comparative efficacy of parathyroidectomy and active surveillance in patients with mild primary hyperparathyroidism: a systematic review and meta-analysis. Osteoporos Int 27:3395–3407. https://doi.org/10.1007/s00198-016-3715-3
Silverberg SJ, Gartenberg F, Jacobs TP, Shane E, Siris E, Staron RB, McMahon DJ, Bilezikian JP (1995) Increased bone mineral density after parathyroidectomy in primary hyperparathyroidism. J Clin Endocrinol Metab 80:729–734. https://doi.org/10.1210/jcem.80.3.7883824
Christiansen P, Steiniche T, Brixen K, Hessov I, Melsen F, Heickendorff L, Mosekilde L (1999) Primary hyperparathyroidism: short-term changes in bone remodeling and bone mineral density following parathyroidectomy. Bone 25:237–244. https://doi.org/10.1016/s8756-3282(99)00150-7
Silverberg SJ, Locker FG, Bilezikian JP (1996) Vertebral osteopenia: a new indication for surgery in primary hyperparathyroidism. J Clin Endocrinol Metab 81:4007–4012. https://doi.org/10.1210/jcem.81.11.8923852
Bala Y, Seeman E (2015) Bone’s material constituents and their contribution to bone strength in health, disease, and treatment. Calcif Tissue Int 97:308–326. https://doi.org/10.1007/s00223-015-9971-y
Seeman E, Martin TJ (2019) Antiresorptive and anabolic agents in the prevention and reversal of bone fragility. Nat Rev Rheumatol 15:225–236. https://doi.org/10.1038/s41584-019-0172-3
Yajima A, Inaba M, Tominaga Y, Ito A (2008) Bone formation by minimodeling is more active than remodeling after parathyroidectomy. Kidney Int 74:775–781. https://doi.org/10.1038/ki.2008.242
Gasser JA, Kneissel M, Thomsen JS, Mosekilde L (2000) PTH and interactions with bisphosphonates. J Musculoskelet Neuronal Interact 1:53–56
Jensen PR, Andersen TL, Chavassieux P, Roux JP, Delaisse JM (2021) Bisphosphonates impair the onset of bone formation at remodeling sites. Bone 145:115850. https://doi.org/10.1016/j.bone.2021.115850
Szymczak J, Bohdanowicz-Pawlak A (2013) Osteoprotegerin, RANKL, and bone turnover in primary hyperparathyroidism: the effect of parathyroidectomy and treatment with alendronate. Horm Metab Res 45:759–764. https://doi.org/10.1055/s-0033-1349842
Miyaoka D, Imanishi Y, Kato E, Toi N, Nagata Y, Kurajoh M, Yamada S, Inaba M, Emoto M (2020) Effects of denosumab as compared with parathyroidectomy regarding calcium, renal, and bone involvement in osteoporotic patients with primary hyperparathyroidism. Endocrine 69:642–649. https://doi.org/10.1007/s12020-020-02401-6
NIH Consensus Development Panel on Osteoporosis Prevention D, Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795. https://doi.org/10.1001/jama.285.6.785
Cusano NE, Rubin MR, Silva BC, Tay YD, Williams JM, Agarwal S, Omeragic B, Guo XE, Bilezikian JP (2018) Skeletal microstructure and estimated bone strength improve following parathyroidectomy in primary hyperparathyroidism. J Clin Endocrinol Metab 103:196–205. https://doi.org/10.1210/jc.2017-01932
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Choe, H.J., Koo, B.K., Yi, K.H. et al. Skeletal effects of combined bisphosphonates treatment and parathyroidectomy in osteoporotic patients with primary hyperparathyroidism. J Bone Miner Metab 40, 292–300 (2022). https://doi.org/10.1007/s00774-021-01279-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-021-01279-2