Abstract
Introduction
In anti-osteoporosis drug trials, vitamin D and calcium (Ca) are common supplements; however, the optimal dose of each is unclear. Using data from the randomized, double-blind, placebo-controlled DIRECT trial, we assessed whether baseline serum 25-hydroxy vitamin D (25[OH]D) level influences the efficacy of denosumab co-administered with vitamin D and Ca.
Materials and methods
In this prespecified sub-analysis, subjects with primary osteoporosis who received denosumab or placebo, plus vitamin D (≥ 400 IU/day) and Ca (≥ 600 mg/day), were classified as 25(OH)D deficient (< 20 ng/mL), insufficient (≥ 20 to < 30 ng/mL), and sufficient (≥ 30 ng/mL). Study endpoints included absolute serum 25(OH)D level at baseline, 12 months, and 24 months; change in serum 25(OH)D and bone mineral density (BMD) status from baseline; and incidence of new vertebral fractures at 24 months.
Results
In 475 denosumab-treated and 481 placebo-treated subjects, proportions with deficient/insufficient/sufficient 25(OH)D at baseline were 53.1%/37.1%/9.9% and 50.9%/42.0%/7.1%, respectively. Supplementation significantly increased mean serum 25(OH)D levels; at 24 months, mean levels were > 30 ng/mL (sufficient) in both treatment groups. Increase in BMD over time was higher in the denosumab group vs. placebo group in all three vitamin D status groups. At month 24, denosumab-treated subjects with deficient/insufficient baseline 25(OH)D had a significantly lower risk of new vertebral fracture vs. placebo-treated subjects.
Conclusion
Among DIRECT trial subjects supplemented with ≥ 400 IU/day of vitamin D and ≥ 600 mg/day of Ca, baseline 25(OH)D sufficiency may not influence the efficacy of denosumab in increasing BMD or preventing vertebral fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D is vital for bone and mineral health [1], and a deficiency/insufficiency of vitamin D is associated with several musculoskeletal clinical conditions [2]; therefore, guidelines for the proper management of serum vitamin D levels have been published worldwide [2,3,4,5,6,7,8]. Moreover, it has been reported that serum 25-hydroxy vitamin D (25[OH]D) levels may be able to influence the effects of anti-osteoporosis treatments, such as bisphosphonates or selective estrogen receptor modulators, with low 25(OH)D associated with inadequate treatment responses [9,10,11,12,13,14].
In many clinical trials for anti-osteoporosis drugs, participants are supplemented with vitamin D and/or calcium (Ca) to achieve sufficient efficacy [15,16,17,18,19,20,21,22,23,24]. However, the optimal dosages for vitamin D and Ca supplementation are unclear, and the amounts used have differed widely between trials: 0–1200 IU/day (vitamin D) and 200–1500 mg/day (Ca) [15,16,17,18,19,20,21,22,23,24].
Denosumab is a fully human monoclonal IgG2 antibody against receptor activator of nuclear factor-kB ligand (RANKL) [25] that prevents the survival and activation of osteoclasts by inhibiting RANK activation. In the FREEDOM trial in postmenopausal women, subjects received denosumab (60 mg every 6 months) or placebo, alongside vitamin D (at least 400–800 IU/day) and Ca (at least 1000 mg/day). Denosumab was found to increase bone mineral density (BMD) and decrease bone turnover markers and fracture risk significantly, compared with placebo [26]. In the Japanese, phase 3 Denosumab Fracture Intervention Randomized Placebo-Controlled (DIRECT trial), denosumab (60 mg every 6 months) was administered alongside vitamin D (at least 400 IU/day) and Ca (at least 600 mg/day), and treatment benefits were observed in subjects with osteoporosis who had prevalent mild or moderate vertebral fractures [27].
Given the various dosages of vitamin D/Ca used between the international and Japanese studies, the optimal dose of these supplements alongside denosumab remains to be determined. It is also unclear whether the doses of vitamin D and Ca need to be adjusted according to the baseline 25(OH)D level. In the FREEDOM trial, vitamin D supplementation varied according to serum 25(OH)D: at least 800 IU/day for subjects with ≤ 20 ng/mL serum 25(OH)D, and at least 400 IU/day for subjects with > 20 ng/mL of serum 25(OH)D [26]; however, in the DIRECT trial, at least 400 IU/day vitamin D was administered regardless of serum 25(OH)D concentration [27]. Ca dosage was not adjusted in either study based on 25(OH)D. Furthermore, whether baseline serum vitamin D levels have an impact on denosumab effects, such as BMD increase and fracture risk reduction, is unknown. Using data from the DIRECT trial, this study assessed the changes in serum 25(OH)D level and the effects of denosumab co-administered with vitamin D and calcium on BMD and fracture risk according to baseline 25(OH)D level.
Materials and methods
Study design
The DIRECT trial (NCT00680953) was a randomized, double-blind, placebo-controlled trial. The complete study methodology has been described previously [27]. In brief, denosumab 60 mg or matching placebo was administered subcutaneously every 6 months during a 24-month period (at 0, 6, 12, and 18 months) in a double-blind manner. All subjects who received denosumab or placebo also received daily supplements containing Ca ≥ 600 mg and vitamin D ≥ 400 IU throughout the study period. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki, the International Conference on Harmonization E6 guideline for Good Clinical Practice, and all applicable national ordinances. Approval was obtained from the Institutional Review Board at each study center, and informed consent was obtained from all individual participants included in the study.
The detailed inclusion and exclusion criteria have been described [27]. Subjects with one to four prevalent vertebral fractures and a BMD T-score of less than − 1.7 (Young Adult Mean in Japan 80%) at the lumbar spine or − 1.6 (Young Adult Mean in Japan 80%) at the total hip by dual-energy X-ray absorptiometry (DXA) based on the diagnostic criteria of primary osteoporosis in Japan [28] were included in the DIRECT trial. Subjects with serum 25(OH)D levels < 12 ng/mL; with more than two moderate (grade 2) and/or any severe (grade 3) vertebral fractures on lateral spine radiographs by semiquantitative grading [29]; or with evidence of conditions such as hyperparathyroidism, hypoparathyroidism, hypercalcemia, hypocalcemia, rheumatoid arthritis, or Paget’s disease of the bone were excluded.
The present report describes a sub-analysis of subjects with primary osteoporosis from the DIRECT trial [27], focusing on serum levels of 25(OH)D at baseline; this analysis was prespecified at the time the DIRECT trial was planned. The subjects in the denosumab and placebo arms in the DIRECT trial were analyzed in this study. Both arms were stratified into three groups based on serum 25(OH)D concentration at baseline, according to current Japanese criteria [2]: deficient (< 20 ng/mL); insufficient (≥ 20 to < 30 ng/mL); and sufficient (≥ 30 ng/mL).
Study measures
The endpoints of this sub-analysis were: absolute serum 25(OH)D level at baseline and after 12 and 24 months of treatment; change in serum 25(OH)D status from baseline; serum 25(OH)D concentrations in the denosumab and placebo groups at the last measurement by baseline levels; percent change in BMD from baseline to 24 months at the lumbar spine (L1–L4), total hip, femoral neck, and distal one-third of the radius by baseline serum 25(OH)D levels; and the incidence of new vertebral fractures at 24 months stratified by baseline serum 25(OH)D levels.
Details of sampling have been described elsewhere [27]. Serum samples were transported to LSI Medience Co., Ltd. (formerly Mitsubishi Chemical Medience Co., Ltd., Tokyo Japan), where the measurement of serum 25(OH)D concentrations was performed by competitive protein binding assay. BMD was evaluated by DXA (QDR® instrument; Hologic Inc., Marlborough, MA, USA) measured at the lumbar spine (L1–L4), total hip, femoral neck, and distal one-third of the radius at baseline, 3 months (except for the distal radius), and 6, 12, 18, and 24 months. Quality control and BMD scan analysis were performed centrally (Synarc Inc., Portland, OR, USA).
As previously reported [27], vertebral fractures were identified from anteroposterior and lateral spine radiographs, taken at baseline and then every 6 months. The definition applied for a new vertebral fracture was an increase of ≥ 1 semiquantitative grading scale in a vertebral body that was normal at baseline, and ≥ 20% loss of height from baseline at the anterior, posterior, or central vertebra.
Statistical analyses
As analysis targets, the safety analysis set (comprising all subjects who received at least one dose of the study drug) was used for the summary of 25(OH)D. The full analysis set (comprising all randomized subjects, with the exception of those who did not have osteoporosis at screening, those who did not receive the study drug or those who had no available efficacy data after the first dose of the study drug) was used for the analysis of BMD and new vertebral fractures. Missing data were not imputed for 25(OH)D, and the last observation carried forward method was used for BMD data. All tests were performed at a two-sided 5% significance level.
The change in 25(OH)D was displayed as a transition chart over time or scatter chart. Student’s t-test was used to compare the percent changes from baseline in BMD at 24 months between the placebo and denosumab groups and among each subgroup stratified by baseline 25(OH)D levels (< 20 ng/mL, ≥ 20 to < 30 ng/mL, or ≥ 30 ng/mL). The incidences of new vertebral fractures at 24 months were displayed as a bar chart and stratified by baseline 25(OH)D levels. A log-rank test was used to compare the placebo and denosumab groups with a hazard ratio (HR) based on the proportional hazards model stratified by baseline 25(OH)D levels. The grouped survival data approach was applied for the log-rank test, and the estimation of the HR was used to statistically analyze new vertebral fracture data as most new vertebral fractures were observed at scheduled visits as previously described [27]. A post hoc analysis was performed using a Student’s t-test to compare 25(OH)D concentrations between baseline and each time point. The software used for statistical analysis was SAS version 9.1.3 (SAS Institute Inc., Cary, NC, USA).
Results
Subject characteristics
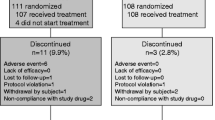
The safety analysis set from the DIRECT trial, which comprised 481 placebo-treated subjects and 475 denosumab-treated subjects, was used for the analyses in this study. Baseline characteristics, according to 25(OH)D levels (deficient, insufficient, and sufficient), are shown in Table 1. The background characteristics at baseline were similar between the placebo and the denosumab groups and across each subgroup except for serum 25(OH)D concentration. These background characteristics are in accordance with the data reported in the main study [27].
Absolute serum 25(OH)D level after 12 and 24 months of treatment
Mean serum 25 (OH)D levels were significantly increased by supplementation in both placebo- and denosumab-treated subjects, even with 400 IU vitamin D supplements. The mean ± standard deviation (SD) serum 25(OH)D concentrations of the placebo group were 20.6 ± 5.9 ng/mL, 32.9 ± 8.9 ng/mL, and 30.9 ± 7.0 ng/mL at baseline, 12 months, and 24 months, respectively. Mean ± SD serum 25(OH)D concentrations of the denosumab group were 21.0 ± 6.1 ng/mL, 32.2 ± 8.9 ng/mL, and 31.0 ± 6.8 ng/mL at baseline, 12 months, and 24 months, respectively.
The serum 25(OH)D concentrations at baseline, 12 months, and 24 months were similar between the two groups (Fig. 1). In both groups, the mean value of serum 25(OH)D concentrations at 12 and 24 months were all ≥ 30 ng/mL. The mean values of serum 25(OH)D concentrations at 12 or 24 months were significantly higher than at baseline in both groups (P < 0.0001). No difference was observed between the 25(OH)D concentrations at 12 and 24 months (Fig. 1).
Changes in serum 25(OH)D status from baseline
In both groups, the majority of subjects (placebo 58.3%, denosumab 57.1%) had sufficient levels of 25(OH)D at 24 months (Fig. 2a, b).
Change in serum 25(OH)D status and concentrations from baseline. Change in serum 25(OH)D in the placebo (a) and denosumab groups (b) stratified by serum 25(OH)D status. Scatter charts illustrate the change in serum 25(OH)D concentrations at the last measurement from baseline in the placebo (c) and denosumab groups (d). 25(OH)D 25-hydroxy vitamin D
At the last measurement, 25(OH)D was increased compared with baseline in 89.6% (395/441) of subjects in the placebo group and 88.0% (387/440) in the denosumab group (Fig. 2c, d). The serum 25(OH)D status at baseline increased from deficient to insufficient or sufficient at the last measurement in 20.4% (90/441) and 26.8% (118/441) of subjects in the placebo group, and 19.3% (85/440) and 29.8% (131/440) of subjects in the denosumab group, respectively (Table 2). The serum 25(OH)D status at baseline increased from insufficient to sufficient at the last measurement in 26.5% (117/441) of subjects in the placebo group and 21.1% (93/440) of subjects in the denosumab group (Table 2).
Changes in BMD from baseline by baseline serum 25(OH)D level
The percent changes in BMD for 24 months by serum 25(OH)D status at baseline (deficient, insufficient, and sufficient) in the denosumab group at three sites were as follows: 9.10%, 9.10%, and 9.29% at the lumbar spine (L1–L4); 4.60%, 4.52%, and 5.19% at the total hip; and 3.93%, 3.66%, and 5.71% at the femoral neck, respectively (Fig. 3a–c). All changes were greater than the corresponding placebo groups (0.27%, − 0.12%, and − 0.13% at the lumbar spine [L1–L4]; − 0.98%, − 1.24%, and − 0.99% at the total hip; and − 0.97%, − 1.36%, and − 0.69% at the femoral neck).
Change in BMD from baseline to 24 months by baseline serum 25(OH)D levels. The percent change in BMD from baseline to 24 months stratified by baseline serum 25(OH)D levels according to site: lumbar spine (a), total hip (b), femoral neck (c), and distal 1/3 radius (d); and difference in percent change from placebo in the denosumab groups at 24 months (e). For panels (a–c), and (d), the bars show 95% CIs of the mean values at each time point. For panel (e), P < 0.0001 for all comparisons vs placebo was based on a Student’s t-test. Bars show 95% CIs of the difference from placebo at 24 months. 25(OH)D 25-hydroxy vitamin D, BMD bone mineral density, CI confidence interval
At the distal one-third of the radius, the percent changes in BMD from baseline to 24 months by serum 25(OH)D status at baseline (deficient, insufficient, and sufficient) in the denosumab groups were 0.60%, 0.46%, and 0.07%, respectively, showing a slight increase in BMD, while decreases were observed in the corresponding placebo groups (− 1.82%, − 1.53%, and − 3.44%) (Fig. 3d).
Figure 3e shows the differences from placebo in mean percent change in BMD from baseline to 24 months in the denosumab group by baseline 25(OH)D levels (deficient, insufficient, and sufficient) as follows: 8.83%, 9.22%, and 9.42% at the lumbar spine (L1–L4); 5.58%, 5.76%, and 6.19% at the total hip; 4.89%, 5.02%, and 6.40% at the femoral neck; and 2.43%, 1.99%, and 3.51% at the distal one-third of the radius, respectively. Compared with placebo, denosumab significantly (all, P < 0.0001) increased bone density regardless of baseline serum 25(OH)D level at the four sites evaluated.
Fracture risk by baseline serum 25(OH)D level
The incidences of new vertebral fractures at 24 months, stratified by baseline 25(OH)D levels (deficient, insufficient, and sufficient), were 1.2%, 3.4%, and 2.2% in the denosumab group and 7.8%, 9.0%, and 2.9% in the placebo group, respectively (Fig. 4). Denosumab-treated subjects with deficient or insufficient 25(OH)D at baseline had a significantly lower risk of a new vertebral fracture compared with placebo-treated subjects (HR 0.149, 95% confidence interval [CI] 0.044–0.504, P = 0.0004, and HR 0.365, 95% CI 0.145–0.919, P = 0.0256, respectively). For subjects with sufficient 25(OH)D at baseline, there was no significant difference observed between denosumab and placebo in the risk of a new vertebral fracture (HR 0.789, 95% CI 0.049–12.629, P = 0.8667).
Discussion
Although the potential influence of serum 25(OH)D levels on treatment responses to anti-osteoporosis treatments are well-recognized [9,10,11,12,13,14], to date, no studies have analyzed the effect of denosumab according to baseline serum 25(OH)D concentration. This study is the first to reveal the effects of denosumab on BMD and fracture prevention stratified by serum 25(OH)D level at baseline.
In this subgroup analysis of the randomized DIRECT trial [27], the impact of denosumab on BMD increase and fracture prevention seemed unaffected by baseline 25(OH)D levels in subjects supplemented with ≥ 400 IU/day vitamin D and ≥ 600 mg/day calcium. According to the present data, there is no need to increase the dose of supplemented vitamin D based on 25(OH)D sufficiency at baseline to obtain the effects of denosumab. Furthermore, the efficacy of denosumab was confirmed in subjects receiving supplementation with just 400 IU/day vitamin D, which is lower than in the FREEDOM trial [26]. Furthermore, in the present study, no difference was observed between the groups even when stratified by the serum 25(OH)D concentration after 24 months (Online Resource 1). In addition, after 24 months, there was no increase in the incidence of new vertebral body fractures in the denosumab group according to the serum 25(OH)D concentration (Online Resource 2). If subjects are supplemented with vitamin D ≥ 400 IU/day and calcium ≥ 600 mg/day, the effect of denosumab is likely to be obtained regardless of the serum 25(OH)D concentration.
Our results are consistent with the results of previous reports evaluating the impact of baseline 25(OH)D on efficacy outcomes with anti-osteoporotic treatment agents plus vitamin D supplementation [30, 31], although it must be remembered that supplementation dosage varied in each trial. The MORE study, which evaluated the effect of raloxifene on BMD and fractures in postmenopausal women with osteoporosis, supplemented subjects with 400–600 IU/day vitamin D and 500 mg/day Ca throughout the study [21, 30]. The FIT study, which evaluated the efficacy of alendronate in women with low BMD, supplemented subjects with 250 IU/day vitamin D and 500 mg/day Ca throughout the study [15, 31]. Both studies showed that baseline 25(OH)D level did not influence the efficacy of raloxifene or alendronate [30, 31]. In contrast, in studies in which no vitamin D supplementation was administered, low baseline levels of 25(OH)D were found to correlate with inadequate response to treatment [9, 10, 12, 14]. In bisphosphonates studies, the effects of treatment have been evaluated without the administration of vitamin D and Ca supplementation. In contrast, no studies, as far as we know, have examined the association between baseline serum 25(OH)D and the effect of denosumab without vitamin D and Ca supplementation. Therefore, while we consider that vitamin D and Ca supplementation may have contributed to the effect of denosumab independent of the baseline serum 25(OH)D concentration, we cannot draw a definitive conclusion based on these findings.
Unlike previous studies such as MORE and FIT, our study also examined the effect of baseline 25(OH)D on the incidence of fractures during the study. We believe this is the first such published analysis, and our data confirm that the number of new vertebral fractures was reduced regardless of baseline vitamin D status. The incidence rate of new vertebral fracture was significantly suppressed in the denosumab group compared with the placebo group in subjects with deficient/insufficient 25(OH)D at baseline. Conversely, there was no significant difference between treatment groups in subjects with sufficient 25(OH)D at baseline; however, this is likely because the number of subjects with sufficient baseline vitamin D who developed fractures was too small to evaluate the difference between the treatment groups properly.
Supplementation with calcium and vitamin D is aimed at preventing hypocalcemia and promoting an adequate response to anti-osteoporosis drugs. In the DIRECT trial, hypocalcemia, as an adverse event, occurred in two subjects (0.4%) in the denosumab group. However, these events were not serious adverse events [27]. Given that in the present study, the 25(OH)D status at baseline was deficient in about half of the subjects, it is considered that supplementation with ≥ 400 IU/day vitamin D and ≥ 600 mg/day calcium effectively reduced the incidence of hypocalcemia.
Reportedly, among elderly Japanese women, subjects with sufficient vitamin D had a lower incidence of limb and vertebral fractures [32]. Furthermore, other studies reported a correlation between vitamin D insufficiency and fracture risk [33,34,35,36]. Similarly, the subjects in the placebo group with sufficient baseline vitamin D in our study tended to have a lower incidence of new vertebral fractures than subjects in the placebo group with deficient or insufficient vitamin D. However, as previously discussed, the number of subjects in the sufficient group was too small to draw any definitive conclusions.
The proportions of subjects with deficient (< 20 ng/mL), insufficient (≥ 20 to < 30 ng/mL), and sufficient (≥ 30 ng/mL) levels of 25(OH)D [2] at baseline in our study were 53.1%, 37.1%, and 9.9%, respectively, in the denosumab group and 50.9%, 42.0%, and 7.1%, respectively, in the placebo group. These proportions are similar to those reported in a recent cohort study of Japanese women aged ≥ 50 years, in which 52% were classified as deficient, 38% as insufficient, and 10% as sufficient [37]. These proportions are also similar to those reported in a Chinese study for postmenopausal women [38]. However, in a US study, the proportion of subjects with a deficient status (< 20 ng/mL) among women ≥ 70 years old was 33.6%, and the combined percentage of subjects who were deficient and insufficient (< 30 ng/mL) was 76.7% [39]. Both of these incidences are lower than those reported in the placebo group in this study (50.9% and 92.9%, respectively).
Although > 90% of subjects in our study were classified as having deficient or insufficient vitamin D levels at baseline, at 24 months, the mean ± SD serum 25(OH)D level in both treatment groups was > 30 ng/mL (30.9 ± 7.0 ng/mL in the placebo group and 31.0 ± 6.8 ng/mL in the denosumab group), which is classed as sufficient vitamin D, according to Japanese guidelines [2]. Although an increase in 25(OH)D was observed, the amounts of vitamin D (≥ 400 IU/day) and Ca (≥ 600 mg/day) supplemented in this study were lower than those used in non-Japanese studies of denosumab [26] and several other anti-osteoporotic agents [17, 20, 22, 23].
Finally, we noted that the BMD of the distal one-third of the radius in the placebo group decreased over 24 months in the subgroup with sufficient 25(OH)D compared with the subgroups with deficient or insufficient 25(OH)D. In the placebo group, the baseline absolute BMD of the distal one-third of the radius was similar among subgroups stratified by baseline serum 25(OH)D level (data not shown). A greater reduction in BMD in the subgroup with sufficient 25(OH)D was seen in this research. However, we cannot draw a definitive conclusion regarding this finding because of the small number of subjects in that subgroup.
The main limitations of this study were the exclusion of subjects who had < 12 ng/mL of serum 25(OH)D and the fact that the study was conducted only in Japanese subjects; thus, the results may not be directly applicable to other ethnicities. Additionally, the DIRECT study was not powered to investigate nonvertebral fractures. As the number of subjects with nonvertebral fractures was extremely small, the efficacy data are not quantifiable and are not described.
In conclusion, in subjects supplemented with vitamin D (at least 400 IU/day) and Ca (at least 600 mg/day), the baseline sufficiency status of serum 25(OH)D may not affect denosumab efficacy outcomes such as BMD increase and fracture prevention.
References
Bikle DD (2014) Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol 21:319–329
Okazaki R, Ozono K, Fukumoto S, Inoue D, Yamauchi M, Minagawa M, Michigami T, Takeuchi Y, Matsumoto T, Sugimoto T (2017) Assessment criteria for vitamin D deficiency/insufficiency in Japan: proposal by an expert panel supported by the Research Program of Intractable Diseases, Ministry of Health, Labour and Welfare, Japan, the Japanese Society for Bone and Mineral Research and the Japan Endocrine Society [Opinion]. J Bone Miner Metab 35:1–5
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium (2011) Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK56070/. Accessed 11 October 2019
Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, Josse RG, Lips P, Morales-Torres J, Yoshimura N (2010) IOF position statement: vitamin D recommendations for older adults. Osteoporos Int 21:1151–1154
Hanley DA, Cranney A, Jones G, Whiting SJ, Leslie WD, Cole DEC, Atkinson SA, Josse RG, Feldman S, Kline GA, Rosen C, Guidelines Committee of the Scientific Advisory Council of Osteoporosis Canada (2010) Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada. CMAJ 182:E610–E618
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, NO Foundation (2014) Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Heaney RP (1709S) Functional indices of vitamin D status and ramifications of vitamin D deficiency. Am J Clin Nutr 80(6 Suppl):1706S–1709S
Ishijima M, Sakamoto Y, Yamanaka M, Tokita A, Kitahara K, Kaneko H, Kurosawa H (2009) Minimum required vitamin D level for optimal increase in bone mineral density with alendronate treatment in osteoporotic women. Calcif Tissue Int 85:398–404
Okazaki R, Muraoka R, Maehara M, Inoue D (2019) Factors associated with inadequate responses to risedronate in Japanese patients with osteoporosis. J Bone Miner Metab 37:185–197
Carmel AS, Shieh A, Bang H, Bockman RS (2012) The 25(OH)D level needed to maintain a favorable bisphosphonate response is ≥33 ng/ml. Osteoporosis Int 23:2479–2487
Adami S, Giannini S, Bianchi G, Sinigaglia L, Di Munno O, Fiore CE, Minisola S, Rossini M (2009) Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int 20:239–244
Peris P, Martínez-Ferrer A, Monegal A, Martínez de Osaba MJ, Muxi A, Guañabens N (2012) 25 hydroxyvitamin D serum levels influence adequate response to bisphosphonate treatment in postmenopausal osteoporosis. Bone 51:54–58
Mawatari T, Muraoka R, Iwamoto Y (2017) Relationship between baseline characteristics and response to risedronate treatment for osteoporosis: data from three Japanese phase III trials. Osteoporos Int 28:1279–1286
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Shiraki M, Kushida K, Fukunaga M, Kishimoto H, Taga M, Nakamura T, Kaneda K, Minaguchi H, Inoue T, Morii H, Tomita A, Yamamoto K, Nagata Y, Nakashima M, Orimo H (1999) A double-masked multicenter comparative study between alendronate and alfacalcidol in Japanese patients with osteoporosis. The Alendronate Phase III Osteoporosis Treatment Research Group. Osteoporos Int 10:183–192
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352
Kushida K, Fukunaga M, Kishimoto H, Shiraki M, Itabashi A, Inoue T, Kaneda K, Morii H, Nawata H, Yamamoto K, Ohashi Y, Orimo H (2004) A comparison of incidences of vertebral fracture in Japanese patients with involutional osteoporosis treated with risedronate and etidronate: a randomized, double-masked trial. J Bone Miner Metab 22:469–478
Cooper C, Emkey RD, McDonald RH, Hawker G, Bianchi G, Wilson K, Schimmer RC (2003) Efficacy and safety of oral weekly ibandronate in the treatment of postmenopausal osteoporosis. J Clin Endocrinol Metab 88:4609–4615
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Glüer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 282:637–645
Silverman SL, Christiansen C, Genant HK, Vukicevic S, Zanchetta JR, de Villiers TJ, Constantine GD, Chines AA (2008) Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo-, and active-controlled clinical trial. J Bone Miner Res 23:1923–1934
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, Zerbini CAF, Milmont CE, Chen L, Maddox J, Meisner PD, Libanati C, Grauer A (2016) Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med 375:1532–1543
Matsumoto T, Hagino H, Shiraki M, Fukunaga M, Nakano T, Takaoka K, Morii H, Ohashi Y, Nakamura T (2009) Effect of daily oral minodronate on vertebral fractures in Japanese postmenopausal women with established osteoporosis: a randomized placebo-controlled double-blind study. Osteoporos Int 20:1429–1437
Bekker PJ, Holloway DL, Rasmussen AS, Murphy R, Martin SW, Leese PT, Holmes GB, Dunstan CR, DePaoli AM (2004) A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res 19:1059–1066
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, FREEDOM Trial (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Nakamura T, Matsumoto T, Sugimoto T, Hosoi T, Miki T, Gorai I, Yoshikawa H, Tanaka Y, Tanaka S, Sone T, Nakano T, Ito M, Matsui S, Yoneda T, Takami H, Watanabe K, Osakabe T, Shiraki M, Fukunaga M (2014) Clinical Trials Express: fracture risk reduction with denosumab in Japanese postmenopausal women and men with osteoporosis: denosumab fracture intervention randomized placebo controlled trial (DIRECT). J Clin Endocrinol Metab 99:2599–2607
Orimo H, Sugioka Y, Fukunaga M, Muto Y, Hotokebuchi T, Gorai I, Nakamura T, Kushida K, Tanaka H, Ikai T, Oh-hashi Y (1998) The Committee of the Japanese Society for Bone and Mineral Research for Development of Diagnostic Criteria of Osteoporosis. Diagnostic criteria of primary osteoporosis. J Bone Miner Metab 16:139–150
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis the Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Antoniucci DM, Vittinghoff E, Blackwell T, Black DM, Sellmeyer DE (2005) Vitamin D insufficiency does not affect bone mineral density response to raloxifene. J Clin Endocrinol Metab 90:4566–4572
Antoniucci DM, Vittinghoff E, Palermo L, Black DM, Sellmeyer DE (2009) Vitamin D insufficiency does not affect response of bone mineral density to alendronate. Osteoporos Int 20:1259–1266
Nakamura K, Saito T, Oyama M, Oshiki R, Kobayashi R, Nishiwaki T, Nashimoto M, Tsuchiya Y (2011) Vitamin D sufficiency is associated with low incidence of limb and vertebral fractures in community-dwelling elderly Japanese women: the Muramatsu Study. Osteoporos Int 22:97–103
Tanaka S, Kuroda T, Yamazaki Y, Shiraki Y, Yoshimura N, Shiraki M (2014) Serum 25-hydroxyvitamin D below 25 ng/mL is a risk factor for long bone fracture comparable to bone mineral density in Japanese postmenopausal women. J Bone Mineral Metab 32:514–523
Cauley JA, Lacroix AZ, Wu L, Horwitz M, Danielson ME, Bauer DC, Lee JS, Jackson RD, Robbins JA, Wu C, Stanczyk FZ, LeBoff MS, Wactawski-Wende J, Sarto G, Ockene J, Cummings SR (2008) Serum 25-hydroxyvitamin D concentrations and risk for hip fractures. Ann Intern Med 149:242–250
Looker AC, Mussolino ME (2008) Serum 25-hydroxyvitamin D and hip fracture risk in older U.S. white adults. J Bone Miner Res 23:143–150
van Schoor NM, Visser M, Pluijm SMF, Kuchuk N, Smit JH, Lips P (2008) Vitamin D deficiency as a risk factor for osteoporotic fractures. Bone 42:260–266
Tamaki J, Iki M, Sato Y, Kajita E, Nishino H, Akiba T, Matsumoto T, Kagamimori S, JPOS Study Group (2017) Total 25-hydroxyvitamin D levels predict fracture risk: results from the 15-year follow-up of the Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos Int 28:1903–1913
Xie Z, Xia W, Zhang Z, Wu W, Lu C, Tao S, Wu L, Gu J, Chandler J, Peter S, Yuan H, Wu T, Liao E (2019) Prevalence of vitamin D inadequacy among Chinese postmenopausal women: a nationwide, multicenter, cross-sectional study. Front Endocrinol (Lausanne) 9:782
Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA (2008) Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000–2004. Am J Clin Nutr 88:1519–1527
Acknowledgements
The authors wish to thank Keyra Martinez Dunn, MD and Sally-Anne Mitchell, PhD of Edanz Medical Writing for providing medical writing support, which was funded by Daiichi Sankyo Co., Ltd., Tokyo, Japan. The study was funded by Daiichi Sankyo Co., Ltd., Tokyo, Japan.
Author information
Authors and Affiliations
Contributions
Conceptualization: TS, TM, TH, MS, MK, NO, HT, and TN; Methodology: TS, MK, NO, HT, and TN; Formal analysis and investigation: NO; Writing—original draft preparation: TS and MK; Writing—review and editing: TS, TM, TH, MS, NO, HT, and TN; Funding acquisition: MK.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. T. Sugimoto has received research grants from Astellas Pharma, Eisai, Daiichi Sankyo Co., Ltd., Chugai Pharmaceutical Co., Ltd., and Eli Lilly Japan, as well as consulting and/or lecture fees from Asahi Kasei Pharma Co., Ltd., and Daiichi Sankyo Co., Ltd. Dr. T. Matsumoto has received consulting fees from Daiichi Sankyo Co., Ltd., Astellas Amgen Biopharma Co. Ltd., Chugai Pharmaceutical Co., Ltd., and Teijin Pharma. Dr. T. Hosoi has received consulting fees from Daiichi Sankyo Co., Ltd. Dr. M. Shiraki has received consulting fees from Daiichi Sankyo Co., Ltd., Chugai Pharmaceutical Co., Ltd., Teijin Pharma, Asahi Kasei Pharma Co., Ltd., and MSD. Dr. M. Kobayashi, Dr. N. Okubo, and Dr. H. Takami are employees of Daiichi Sankyo Co., Ltd., Tokyo, Japan. Dr. T. Nakamura acted as a consultant for Teijin Pharma, Daiichi Sankyo Co., Ltd., Chugai Pharmaceutical Co., Ltd., Asahi Kasei Pharma Co., Ltd., and Amgen Inc.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below are links to the electronic supplementary material.
About this article
Cite this article
Sugimoto, T., Matsumoto, T., Hosoi, T. et al. Efficacy of denosumab co-administered with vitamin D and Ca by baseline vitamin D status. J Bone Miner Metab 38, 848–858 (2020). https://doi.org/10.1007/s00774-020-01119-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-020-01119-9