Abstract
This study aimed to evaluate the association of bone metabolism markers with coronary atherosclerosis and coronary artery disease (CAD) in postmenopausal women. Based on the findings of coronary angiography, 111 women with CAD and 116 women without CAD were recruited. Serum calcium, phosphate, parathyroid hormone (PTH), 25-hydroxyvitamin D (25OHD), osteocalcin, N-terminal propeptide of type I procollagen (P1NP) and C-terminal cross-linked telopeptide of type I collagen (CTX) were measured. The Gensini score was used to assess the severity of coronary atherosclerosis. Compared with women with serum calcium ≤2.29 mmol/L, women with serum calcium >2.29 mmol/L had a 2.63-fold increased risk of CAD after adjusting for multiple cardiovascular risks, PTH and 25OHD [odds ratio (OR) = 2.91, 95% confidence interval (CI) 1.35–6.28]. In the fully adjusted model plus PTH and 25OHD, the risk of CAD increased 1.87-fold with every 1-SD increment of serum calcium (OR = 1.87, 95% CI 1.21–2.88). To further analyze the potential strong confounding effect of albumin, the absolute levels of calcium were replaced by their albumin-corrected values in the regression model. Compared with women with albumin-corrected calcium ≤2.27 mmol/L, women with albumin-corrected calcium >2.27 mmol/L had a 2.36-fold increased risk of CAD in the fully adjusted model plus PTH and 25OHD (OR = 2.36, 95% CI 1.13–4.92). The risk of coronary atherosclerosis as defined by Gensini score >0 increased 1.73-fold with every 1-SD increment of serum calcium in the fully adjusted model plus PTH and 25OHD (OR = 1.73, 95% CI 1.09–2.73). However, albumin-corrected calcium was not associated with coronary atherosclerosis either as a categorical variable or as a continuous variable in all models. No significant association of PTH, 25OHD, osteocalcin, CTX and P1NP with CAD or coronary atherosclerosis was found in this study. Higher serum calcium levels were independently associated with CAD in postmenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, a variety of bone metabolism markers have been shown to be associated with the development of cardiovascular diseases. The components of bone, calcium and phosphate play a critical role in bone metabolism. Maintenance of normal serum calcium and phosphate is also a prerequisite for many important physiologic processes, including intracellular signaling, cardiovascular function and metabolic pathways. Through the mechanism of vascular calcification [1], serum calcium and phosphate have been linked to coronary calcification [2,3,4], coronary artery disease (CAD) [2], myocardial infarction [5], heart failure [6] and all-cause mortality of CAD [7]. Serum calcium also contributes to the development of cardiovascular diseases through its positive association with various cardiovascular risk factors, including blood pressure, cholesterol, triglyceride, glucose and body mass index [8, 9].
Serum calcium and phosphate levels are tightly regulated within a narrow range by a complex interplay of factors, including vitamin D and parathyroid hormone (PTH) [10]. Beyond its role in mineral and bone metabolism, low serum 25-hydroxyvitamin D (25OHD) levels were shown to be associated with the presence and severity of CAD [11, 12], and gender differences may exist underlying this relationship [12]. Similarly, high PTH levels may increase the risk of arterial dysfunction [13], hypertension [14], left ventricle hypertrophy [15], heart failure [16] and atherosclerotic disease [17].
It has been shown that bone turnover markers play a role in atherosclerotic diseases. Osteocalcin is the most abundant non-collagenous bone matrix protein [18], is predominantly expressed by osteoblast and is considered a biomarker of bone turnover [19, 20]. Apart from its skeletal effects, clinical studies reported that osteocalcin is involved in atherosclerosis. Serum osteocalcin concentration was inversely related to carotid intima-media thickness [21], abdominal aortic calcification [22], and the presence and severity of CAD [23,24,25]. In patients with CAD, a large fraction of endothelial progenitor cells express osteocalcin, which may mediate vascular calcification and vascular injury [26, 27]. Type I collagen-derived peptides are also important bone turnover markers. C-terminal cross-linked telopeptide of type I collagen (CTX) was reported to be associated with carotid intima-media thickness [28]. Higher N-terminal propeptide of type I procollagen (P1NP) levels predicted increased risk of myocardial infarction [29].
Taking into consideration the increased risk of osteoporosis and CAD after the menopause and the close relationship between bone metabolism and atherosclerosis, the objective of this study was to evaluate the association of bone metabolism markers with coronary atherosclerosis and CAD in postmenopausal women. As a variety of bone markers have been reported to be associated with CAD and because of the interrelationship between bone markers, we measured a group of bone markers, including serum calcium and phosphate and its regulators PTH and 25OHD, the non-collagenous bone marker osteocalcin, and the collagenous bone markers P1NP and CTX. We aimed to find out the independent association of bone markers with CAD in postmenopausal women.
Materials and methods
Study population
All participants were Chinese postmenopausal women who underwent coronary angiography for suspected CAD at the Cardiology Department of Zhongshan Hospital in Shanghai between October 2015 and January 2016. They were randomly recruited in a consecutive manner. These patients had chest pain or dyspnea symptoms, and were hospitalized for coronary angiography to make a definite diagnosis. Based on the findings of coronary angiography, we recruited 111 women with CAD and 116 women without CAD. The subjects were excluded who were receiving hormone therapy or anti-osteoporotic treatment to reduce external influence on bone metabolism, as well as those who were taking calcium and vitamin D supplements. We also excluded those with metabolic bone diseases, acute illness, severe systemic diseases, abnormal liver function, chronic kidney disease (estimated glomerular filtration rate <60 mL/min/1.73 m2) and malignancy, and those with a history of stroke, myocardial infarction and other thrombotic diseases within the previous 6 months.
This study was approved by the Ethics Committee of Zhongshan Hospital. The study complied with the Declaration of Helsinki and informed consent was obtained from all participants.
Clinical assessment
Baseline information concerning medical history and health-related behaviors was collected. Medication usage including hormones, anti-osteoporotic drugs, calcium and vitamin D supplements and statins was recorded. Smoking habits were also recorded, defined as never smoking, current smoking (smoking regularly in the past 6 months), or ever smoking (cessation of smoking for more than 6 months). Menopause was defined as natural cessation of menstruation for longer than 12 months or cessation by hysterectomy.
Weight and height were measured, and body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Waist circumference was measured midway between the lower rib margin and the iliac crest in a standing position. Blood pressure was measured using a mercury sphygmomanometer after resting for 10 min in a sitting position. Hypertension was defined by the following criteria: diagnosis of hypertension made previously by a physician, or systolic blood pressure ≥140 mmHg, or diastolic blood pressure ≥90 mmHg, or treatment with antihypertensive medications. Diabetes was defined by the following criteria: diagnosis of diabetes made previously by a physician, or fasting plasma glucose ≥7 mmol/L, or 2-h postprandial glucose ≥11.1 mmol/L, or HbA1c ≥6.5%, or use of insulin or oral hypoglycemic agents.
Laboratory assays
Blood samples were obtained after a fasting period of at least 10 h in the morning. Glucose, creatinine, uric acid, calcium, phosphate, albumin and lipid profiles were tested using a Hitachi 7600 biochemistry autoanalyzer (Roche Diagnostics, Basel, Switzerland). HbA1c was measured by high-performance liquid chromatography using a Bio-Rad Variant II analyzer (Bio-Rad Laboratories, Hercules, CA, USA). Estimated glomerular filtration rate (eGFR) was calculated by using the modification of diet in renal disease study equation as the following: 186 × [serum creatinine (mg/dL)]−1.154 × (age)−0.203 × (0.742 if female) [30]. Albumin-corrected calcium serum levels were calculated using a widely used formula: albumin-corrected calcium (mmol/L) = uncorrected calcium (mmol/L) − 0.02 × albumin (g/L) + 0.8 [7, 31]. Total osteocalcin, 25OHD, CTX, P1NP and intact PTH was measured using electrochemiluminescence immunoassay by the Roche Cobas E601 electrochemiluminescence system (Roche Diagnostics). The intra- and inter-batch variation coefficients were 1.2–4.7% and 1.5–5.7%, respectively. High-sensitivity C-reactive protein (hsCRP) concentration was measured by immunonephelometry using a Hitachi 7600 biochemistry autoanalyzer (DiaSys Diagnostics, Shanghai, China).
Angiographic analysis
Two cardiologists who were blinded to the study protocol carried out the angiographic analysis, and a percentage stenosis was given to the major epicardial arteries and sub-branches. Based on the findings of the coronary angiography, patients were diagnosed with CAD (≥50% stenosis in ≥1 coronary vessel) and without CAD. We used the Gensini score [32] to assess the severity of atherosclerosis of coronary arteries: it scores as 1 for 1–25% narrowing, 2 for 26–50%, 4 for 51–75%, 8 for 76–90%, 16 for 91–99% and 32 for a complete occlusion. This score is then multiplied by a factor depending on the functional significance of the coronary artery. The multiplying factor for a left main stem lesion is 5; it is 2.5 for proximal left anterior descending artery (LAD) and left circumflex artery (LCX) lesions, 1.5 for a mid-LAD lesion, and 1 for distal LAD, mid/distal LCX and right coronary artery lesions. The multiplication factor for any other branch is 0.5.
Statistical analyses
Continuous variables are expressed as mean ± SD or median (interquartile range). Comparisons between groups were performed with independent sample t test and χ 2 testing for continuous and categorical variables, respectively. Spearman correlation analysis was performed to examine the correlation between serum calcium and different variables. We tested the association of bone metabolism markers with CAD or the presence of coronary atherosclerosis as defined by Gensini score >0 using multiple logistic regressions. Bone metabolism markers were included in the regression model as continuous variables (divided by their respective SD) or categorical variables (categorized by their respective median). The unadjusted logistic regression model, model adjusted for age and BMI, and model adjusted for all covariates (fully adjusted model) were separately fitted for each bone metabolism marker. To further evaluate the independent effect of calcium and phosphate on CAD or coronary atherosclerosis, we added PTH and 25OHD to the fully adjusted model. Statistical tests were two-sided and P values <0.05 were considered significant. All statistical analyses were performed using SPSS software version 19.0.
Results
The characteristics of the participants are presented in Table 1. Our study recruited 227 postmenopausal women who underwent coronary angiography for suspected CAD, comprising 111 patients with CAD and 116 patients without CAD. Women with CAD were older than women without CAD. Women with CAD had a higher proportion of statin use, a higher HbA1c level and a higher albumin level than women without CAD. For the comparison of bone metabolism markers, only serum calcium levels and albumin corrected calcium levels were significantly higher in women with CAD compared with women without CAD. All other bone metabolism markers, including serum phosphate, PTH, 25OHD, osteocalcin, CTX and P1NP, were not significantly different between the CAD group and non-CAD group. There were 19 patients using diuretics, comprising 10 CAD patients (8 patients used thiazide diuretics and 2 patients used loop diuretics) and 9 non-CAD patients (8 patients used thiazide diuretics and 1 patient used loop diuretics). The use of diuretics was not different between the CAD group and non-CAD group (P = 0.52).
Based on the significant difference in serum calcium concentrations between the CAD group and non-CAD group, we did a correlation analysis of calcium with clinical and laboratory parameters to find the factors influencing serum calcium levels (Table 2). Metabolic parameters such as waist circumference, waist to hip ratio, diastolic blood pressure, fasting blood glucose, 2-h postprandial blood glucose, triglyceride and uric acid were all positively correlated with calcium, and the correlation was mild to moderate. It should be noted that calcium and albumin were highly correlated, with a Spearman correlation coefficient of 0.50. As expected, PTH and 25OHD were significantly correlated with calcium. Interestingly, calcium and Gensini score were positively correlated with each other.
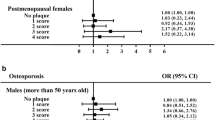
Next, we tested the association of bone metabolism markers with CAD using multiple logistic regression (Table 3). We found that serum calcium was independently associated with CAD. We categorized the participants into two groups by the median of serum calcium (2.29 mmol/L). Compared with women with serum calcium ≤2.29 mmol/L, women with serum calcium >2.29 mmol/L had a 2.63-fold increased risk of CAD in the unadjusted model [odds ratio (OR) = 2.63, 95% confidence interval (CI) 1.45–4.77]. In the model adjusted for age and BMI, this association was still significant (OR = 3.07, 95% CI 1.64–5.75). Taking into consideration the close relationship between serum calcium and a variety of clinical and biochemical parameters, we adjusted for smoking, hypertension, diabetes, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglyceride, estimated glomerular filtration rate, statin use and high-sensitivity C-reactive protein further, and higher serum calcium (>2.29 mmol/L) was still significantly associated with CAD (OR = 2.60, 95% CI 1.25–5.43). Finally, the effect of further adding PTH and 25OHD to the fully adjusted model was evaluated. We found that the result was robust after further adjustment for PTH and 25OHD, and the magnitude of the effect was not diminished (OR = 2.91, 95% CI 1.35–6.28). We also tested serum calcium as a continuous variable by dividing by its SD. Similarly, serum calcium was significantly associated with CAD in the unadjusted model, in the model adjusted for age and BMI, in the fully adjusted model, and also in the fully adjusted model plus PTH and 25OHD. In the fully adjusted model plus PTH and 25OHD, the risk of CAD increased 1.87-fold with every 1-SD increment of serum calcium (OR = 1.87, 95% CI 1.21–2.88). The above results were similar if we further adjusted for the use of diuretics. Other bone metabolism markers, including phosphate, PTH, 25OHD, CTX and P1NP, were not associated with CAD either in the unadjusted model or in the fully adjusted model (Table 3).
To further analyze the potential strong confounding effect of albumin, we replaced the absolute levels of calcium by their albumin-corrected values in the regression model. The results were similar to those of the model using uncorrected calcium levels. Compared with women with albumin-corrected calcium ≤2.27 mmol/L, women with albumin-corrected calcium >2.27 mmol/L had a 2.36-fold increased risk of CAD in the fully adjusted model plus PTH and 25OHD (OR = 2.36, 95% CI 1.13–4.92) (Table 3). When testing albumin-corrected calcium as a continuous variable by dividing by its SD, the association of calcium with CAD was significant in the unadjusted model and the model adjusted for age and BMI, but it became non-significant in the fully adjusted model or fully adjusted model plus PTH and 25OHD (Table 3). The above results were similar if we further adjusted for the use of diuretics.
Bearing in mind on the relationship between serum calcium and CAD, we further examined whether bone metabolism markers were associated with the presence of coronary atherosclerosis as defined by Gensini score >0 (Table 4). Compared with women with serum calcium ≤2.29 mmol/L, women with serum calcium >2.29 mmol/L had a 2.13-fold increased risk of coronary atherosclerosis in the unadjusted model (OR = 2.13, 95% CI 1.10–4.12). In the model adjusted for age and BMI, this association remained significant (OR = 2.61, 95% CI 1.30–5.26). However, in the fully adjusted model and the fully adjusted model plus PTH and 25OHD, the association became non-significant (OR = 2.21, 95% CI 0.96–5.04; OR = 2.23, 95% CI 0.94–5.29). When testing calcium as a continuous variable by dividing by its SD, serum calcium was consistently associated with coronary atherosclerosis in the unadjusted model, the model adjusted for age and BMI, the fully adjusted model and the fully adjusted model plus PTH and 25OHD (OR = 1.60, 95% CI 1.12–2.29; OR = 1.76, 95% CI 1.21–2.56; OR = 1.69, 95% CI 1.09–2.63; OR = 1.73, 95% CI 1.09–2.73, respectively). The above results were similar if we further adjusted for the use of diuretics. Other bone metabolism markers, including phosphate, PTH, 25OHD, CTX and P1NP, were not associated with coronary atherosclerosis either in the unadjusted model or in the fully adjusted model (Table 4). Considering the potential confounding effect of albumin, we replaced the absolute levels of calcium by their albumin-corrected values in the regression model. We found that albumin-corrected calcium was no longer associated with coronary atherosclerosis either as a categorical variable or as a continuous variable in all models (Table 4). The association of albumin-corrected calcium with coronary atherosclerosis remained non-significant if we further adjusted for the use of diuretics.
Discussion
Our study examined the potential role of bone metabolism markers in CAD and coronary atherosclerosis in postmenopausal women. We found that serum calcium was independently associated with the presence of CAD and coronary atherosclerosis in postmenopausal women. A higher serum calcium level carried a higher risk of CAD and coronary atherosclerosis. No significant effect of other bone markers such as serum phosphate, PTH, 25OHD, osteocalcin, CTX and P1NP on CAD or coronary atherosclerosis was found in our study. As serum albumin levels have a profound influence on serum calcium concentration, the relationship between calcium and CAD may be confounded by albumin. We calculated albumin-corrected calcium in order to have a surrogate for ionized calcium. We found that the association of albumin-corrected calcium with CAD remained significant. However, albumin-corrected calcium was no longer associated with coronary atherosclerosis.
Our findings were in line with the previous studies. In the study by Shin et al., higher calcium was significantly associated with coronary artery calcification score >100 and CAD in participants who underwent cardiac computed tomography angiography for a general health evaluation or for evaluating symptoms and signs of cardiac disease [2]. In another study by Kwak et al., they also found that serum calcium was significantly associated with coronary artery calcification score in a population undergoing cardiac computed tomography angiography for a general health checkup [3]. In other studies, higher calcium levels were related to increased risk of myocardial infarction in a population-based cohort [5] and all-cause mortality in patients with CAD [7]. Although the mechanism by which serum calcium is related to CAD remains unclear, vascular calcification resembling bone metabolism, which is now recognized as a marker of atherosclerotic plaque burden, may be an important explanation [1]. Calcium might have a direct effect on vascular calcification. High calcium can induce vascular smooth muscle cells in the vessel wall to change into an osteoblast-like phenotype and cause the mineralization of collagen and non-collagenous proteins in arteries [1, 33].
Besides its influence on vascular calcification, serum calcium may contribute to the development of CAD through its positive association with cardiovascular risk factors such as dyslipidemia, hypertension, elevated glucose level and increased BMI [8, 34]. Consistent with previous findings, we also found that serum calcium level was positively associated with waist circumference, waist to hip ratio, diastolic blood pressure, fasting glucose, 2-h postprandial glucose, triglyceride, apolipoprotein B, apolipoprotein E and uric acid in postmenopausal women. As a result, the association of serum calcium with CAD in our study may contribute to the relationship between higher calcium levels and unfavorable cardiovascular risk profile. However, the association of calcium with CAD remained significant after adjusting for multiple cardiovascular risks in the regression model, and the magnitude of effect did not change much compared with those of the unadjusted and minimally adjusted models. Our results were consistent with previous findings [2, 3], suggesting the independent role of serum calcium in the development of cardiovascular diseases.
The strong correlation of serum calcium with albumin may account for a major confounding effect in the association analysis of calcium with CAD. To avoid collinearity problems and to analyze the potential confounding effect of albumin, we replaced the absolute calcium levels by their albumin-corrected values (a surrogate for ionized calcium) in the regression models. The association of albumin-corrected calcium with CAD remained significant after adjusting for multiple cardiovascular risks and the magnitude of effect diminished only slightly, suggesting the robust relationship between calcium and CAD.
After examining the relationship between serum calcium and CAD, we also analyzed the association of calcium with coronary atherosclerosis as defined by Gensini score >0. The association of calcium with coronary atherosclerosis seemed weaker compared to the association with CAD. Although the association remained significant in all models when testing calcium as a continuous variable, this association became non-significant in the fully adjusted model and fully adjusted model plus PTH and 25OHD when testing calcium as a dichotomous variable. More importantly, albumin-corrected calcium analyzed either as a continuous variable or as a dichotomous variable was not associated with coronary atherosclerosis in all models. We postulate that albumin-corrected calcium increases very slightly in patients with mild coronary atherosclerosis, which may reduce the difference in albumin-corrected calcium between patients with coronary atherosclerosis and patients without coronary atherosclerosis. The difference may become obvious and statistically significant on increasing the sample size, which deserves to be investigated in the future. Another possibility for this negative finding is that we did not use ionized serum calcium in our study, as it is not routinely measured in our hospital. The ionized serum calcium is biologically active and physiologically important for cellular function, so measurement of ionized serum calcium is considered superior to serum total calcium. Usually, albumin-corrected calcium is calculated when ionized calcium is not available, which is based on the assumption that the concentration of ionized serum calcium changed linearly with the concentration of albumin. However, albumin-corrected calcium may not correlate well with ionized calcium, which is also affected by factors besides serum albumin, for example blood pH.
Our study also evaluated the association of several other bone markers, including PTH, 25OHD, osteocalcin, CTX and P1NP, with CAD and coronary atherosclerosis. However, no significant association was found in our study. In fact, the relationships between these bone markers and atherosclerosis were inconsistent in previous studies. Some important issues should be considered when assessing the relationship between these bone markers and atherosclerosis. As PTH and 25OHD are regulators of serum calcium, serum calcium may be a confounding factor in the association of PTH and 25OHD with atherosclerosis. Whether the significant association of PTH and 25OHD with cardiovascular diseases in previous studies was independent of calcium is not clear [11,12,13,14,15]. Other factors may explain the discrepancy between our study and previous studies. Firstly, the inconsistent findings among studies may be associated with the different genetic background of various ethnicities. Secondly, our study only included postmenopausal women, while previous studies included both men and women. It is known that serum 25OHD level is different between men and women. In addition, bone turnover and bone loss is accelerated in postmenopausal women, which is different from men and premenopausal women. Thirdly, the sample size of our study was relatively small, which may be a limitation of the study. Studies with large sample sizes in the Chinese population are needed to further examine the effects of bone metabolic markers on CAD.
Although CTX, P1NP and osteocalcin are bone metabolism markers, they may also be released from atherosclerotic plaques. Type I collagen is a major component of extracellular matrix in atherosclerotic plaques [35, 36]. Cathepsin K degrades type I collagen into CTX, which is used as a marker of matrix degradation [37]. Co-localization of cathepsin-K and CTX was demonstrated in areas of intimal hyperplasia and in advanced plaques [37]. Studies also have shown osteocalcin deposits in calcified atherosclerotic plaques [38]. Besides, a large fraction of endothelial progenitor cells express osteocalcin in atherosclerotic diseases [26, 27]. Therefore, different sources of these bone markers may obscure the relationship between bone markers and atherosclerosis. As CAD and osteoporosis may coexist in postmenopausal women, adjustment of bone mineral density seems to be reasonable when examining the relationship between bone markers and CAD.
There are some advantages to our study. In our study, CAD and the severity of coronary atherosclerosis were evaluated based on coronary angiography. A group of bone markers, including serum calcium and phosphate and its regulators PTH and 25OHD, the non-collagenous bone marker osteocalcin, and the collagenous bone markers P1NP and CTX, were examined for their role in CAD. We focused on a population of postmenopausal women with multiple cardiovascular risks. Our study provided evidence for the independent role of serum calcium in CAD in postmenopausal women. Although calcium supplementation is commonly used in postmenopausal women for the prevention and treatment of osteoporosis, its benefits and risks should be balanced.
Meanwhile, several limitations of our study should be addressed. A causal role for serum calcium cannot be established in our study, and a follow-up study should be conducted. Serum calcium may contribute to CAD through the mechanism of vascular calcification, but coronary calcification was not assessed in our study. Bone mineral density was not adjusted in the analysis, which may confound the association of bone markers with CAD.
In conclusion, our study found that higher serum calcium levels were independently associated with CAD in postmenopausal women. No significant association of PTH, 25OHD, osteocalcin, CTX and P1NP with CAD was found in this study.
References
Giachelli CM (2004) Vascular calcification mechanisms. J Am Soc Nephrol 15:2959–2964
Shin S, Kim KJ, Chang HJ, Cho I, Kim YJ, Choi BW, Rhee Y, Lim SK, Yang WI, Shim CY, Ha JW, Jang Y, Chung N (2012) Impact of serum calcium and phosphate on coronary atherosclerosis detected by cardiac computed tomography. Eur Heart J 33:2873–2881
Kwak SM, Kim JS, Choi Y, Chang Y, Kwon MJ, Jung JG, Jeong C, Ahn J, Kim HS, Shin H, Ryu S (2014) Dietary intake of calcium and phosphorus and serum concentration in relation to the risk of coronary artery calcification in asymptomatic adults. Arterioscler Thromb Vasc Biol 34:1763–1769
Kim WS, Lee DH, Youn HJ (2013) Calcium-phosphorus product concentration is a risk factor of coronary artery disease in metabolic syndrome. Atherosclerosis 229:253–257
Jorde R, Schirmer H, Njolstad I, Lochen ML, Bogeberg Mathiesen E, Kamycheva E, Figenschau Y, Grimnes G (2013) Serum calcium and the calcium-sensing receptor polymorphism rs17251221 in relation to coronary heart disease, type 2 diabetes, cancer and mortality: the Tromso Study. Eur J Epidemiol 28:569–578
Lutsey PL, Alonso A, Michos ED, Loehr LR, Astor BC, Coresh J, Folsom AR (2014) Serum magnesium, phosphorus, and calcium are associated with risk of incident heart failure: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Clin Nutr 100:756–764
Grandi NC, Brenner H, Hahmann H, Wusten B, Marz W, Rothenbacher D, Breitling LP (2012) Calcium, phosphate and the risk of cardiovascular events and all-cause mortality in a population with stable coronary heart disease. Heart 98:926–933
Williams DM, Fraser A, Lawlor DA (2011) Associations of vitamin D, parathyroid hormone and calcium with cardiovascular risk factors in US adolescents. Heart 97:315–320
Gallo L, Faniello MC, Canino G, Tripolino C, Gnasso A, Cuda G, Costanzo FS, Irace C (2016) Serum calcium increase correlates with worsening of lipid profile: an observational study on a large cohort from south Italy. Medicine (Baltimore) 95:e2774
Bergwitz C, Juppner H (2010) Regulation of phosphate homeostasis by PTH, vitamin D, and FGF23. Annu Rev Med 61:91–104
Liew JY, Sasha SR, Ngu PJ, Warren JL, Wark J, Dart AM, Shaw JA (2015) Circulating vitamin D levels are associated with the presence and severity of coronary artery disease but not peripheral arterial disease in patients undergoing coronary angiography. Nutr Metab Cardiovasc Dis 25:274–279
Verdoia M, Schaffer A, Barbieri L, Di Giovine G, Marino P, Suryapranata H, De Luca G, Novara Atherosclerosis Study Group (2015) Impact of gender difference on vitamin D status and its relationship with the extent of coronary artery disease. Nutr Metab Cardiovasc Dis 25:464–470
Bosworth C, Sachs MC, Duprez D, Hoofnagle AN, Ix JH, Jacobs DR Jr, Peralta CA, Siscovick DS, Kestenbaum B, de Boer IH (2013) Parathyroid hormone and arterial dysfunction in the multi-ethnic study of atherosclerosis. Clin Endocrinol (Oxf) 79:429–436
Yao L, Folsom AR, Pankow JS, Selvin E, Michos ED, Alonso A, Tang W, Lutsey PL (2016) Parathyroid hormone and the risk of incident hypertension: the Atherosclerosis Risk in Communities study. J Hypertens 34:196–203
Soares AA, Freitas WM, Japiassu AV, Quaglia LA, Santos SN, Pereira AC, Nadruz Junior W, Sposito AC (2015) Enhanced parathyroid hormone levels are associated with left ventricle hypertrophy in very elderly men and women. J Am Soc Hypertens 9:697–704
Bansal N, Zelnick L, Robinson-Cohen C, Hoofnagle AN, Ix JH, Lima JA, Shoben AB, Peralta CA, Siscovick DS, Kestenbaum B, de Boer IH (2014) Serum parathyroid hormone and 25-hydroxyvitamin D concentrations and risk of incident heart failure: the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc 3:e001278
Hagstrom E, Michaelsson K, Melhus H, Hansen T, Ahlstrom H, Johansson L, Ingelsson E, Sundstrom J, Lind L, Arnlov J (2014) Plasma-parathyroid hormone is associated with subclinical and clinical atherosclerotic disease in 2 community-based cohorts. Arterioscler Thromb Vasc Biol 34:1567–1573
Wolf G (1996) Function of the bone protein osteocalcin: definitive evidence. Nutr Rev 54:332–333
Price PA, Parthemore JG, Deftos LJ (1980) New biochemical marker for bone metabolism. Measurement by radioimmunoassay of bone GLA protein in the plasma of normal subjects and patients with bone disease. J Clin Invest 66:878–883
Ivaska KK, Hentunen TA, Vaaraniemi J, Ylipahkala H, Pettersson K, Vaananen HK (2004) Release of intact and fragmented osteocalcin molecules from bone matrix during bone resorption in vitro. J Biol Chem 279:18361–18369
Yang R, Ma X, Dou J, Wang F, Luo Y, Li D, Zhu J, Bao Y, Jia W (2013) Relationship between serum osteocalcin levels and carotid intima-media thickness in Chinese postmenopausal women. Menopause 20:1194–1199
Ogawa-Furuya N, Yamaguchi T, Yamamoto M, Kanazawa I, Sugimoto T (2013) Serum osteocalcin levels are inversely associated with abdominal aortic calcification in men with type 2 diabetes mellitus. Osteoporos Int 24:2223–2230
Zhang Y, Qi L, Gu W, Yan Q, Dai M, Shi J, Zhai Y, Chen Y, Liu J, Wang W, Ning G, Hong J (2010) Relation of serum osteocalcin level to risk of coronary heart disease in Chinese adults. Am J Cardiol 106:1461–1465
Kim KM, Lim S, Moon JH, Jin H, Jung KY, Shin CS, Park KS, Jang HC, Choi SH (2016) Lower uncarboxylated osteocalcin and higher sclerostin levels are significantly associated with coronary artery disease. Bone 83:178–183
Bao Y, Zhou M, Lu Z, Li H, Wang Y, Sun L, Gao M, Wei M, Jia W (2011) Serum levels of osteocalcin are inversely associated with the metabolic syndrome and the severity of coronary artery disease in Chinese men. Clin Endocrinol (Oxf) 75:196–201
Gossl M, Modder UI, Atkinson EJ, Lerman A, Khosla S (2008) Osteocalcin expression by circulating endothelial progenitor cells in patients with coronary atherosclerosis. J Am Coll Cardiol 52:1314–1325
Flammer AJ, Gossl M, Widmer RJ, Reriani M, Lennon R, Loeffler D, Shonyo S, Simari RD, Lerman LO, Khosla S, Lerman A (2012) Osteocalcin positive CD133+/CD34−/KDR+ progenitor cells as an independent marker for unstable atherosclerosis. Eur Heart J 33:2963–2969
Leli C, Pasqualini L, Vaudo G, Gaggioli S, Scarponi AM, Mannarino E (2010) Carotid intima-media thickness and bone turnover: the role of C-terminal telopeptide of type I collagen. Intern Emerg Med 5:127–134
Yeap BB, Alfonso H, Chubb SA, Byrnes E, Beilby JP, Ebeling PR, Allan CA, Schultz C, Hankey GJ, Golledge J, Flicker L, Norman PE (2015) Proportion of undercarboxylated osteocalcin and serum P1NP predict incidence of myocardial infarction in older men. J Clin Endocrinol Metab 100:3934–3942
Stevens LA, Coresh J, Greene T, Levey AS (2006) Assessing kidney function—measured and estimated glomerular filtration rate. N Engl J Med 354:2473–2483
Dhingra R, Sullivan LM, Fox CS, Wang TJ, D’Agostino RB Sr, Gaziano JM, Vasan RS (2007) Relations of serum phosphorus and calcium levels to the incidence of cardiovascular disease in the community. Arch Intern Med 167:879–885
Gensini GG (1983) A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol 51:606
Mizobuchi M, Towler D, Slatopolsky E (2009) Vascular calcification: the killer of patients with chronic kidney disease. J Am Soc Nephrol 20:1453–1464
Jorde R, Sundsfjord J, Bonaa KH (2001) Determinants of serum calcium in men and women. The Tromso Study. Eur J Epidemiol 17:1117–1123
Heeneman S, Cleutjens JP, Faber BC, Creemers EE, van Suylen RJ, Lutgens E, Cleutjens KB, Daemen MJ (2003) The dynamic extracellular matrix: intervention strategies during heart failure and atherosclerosis. J Pathol 200:516–525
Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W Jr, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW (1995) A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 92:1355–1374
Barascuk N, Skjot-Arkil H, Register TC, Larsen L, Byrjalsen I, Christiansen C, Karsdal MA (2010) Human macrophage foam cells degrade atherosclerotic plaques through cathepsin K mediated processes. BMC Cardiovasc Disord 10:19
Tyson KL, Reynolds JL, McNair R, Zhang Q, Weissberg PL, Shanahan CM (2003) Osteo/chondrocytic transcription factors and their target genes exhibit distinct patterns of expression in human arterial calcification. Arterioscler Thromb Vasc Biol 23:489–494
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
About this article
Cite this article
Ling, Y., Wang, Z., Wu, B. et al. Association of bone metabolism markers with coronary atherosclerosis and coronary artery disease in postmenopausal women. J Bone Miner Metab 36, 352–363 (2018). https://doi.org/10.1007/s00774-017-0841-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-017-0841-8