Abstract
The present landscape of adverse drug reactions (ADRs) cases paints a somber picture, with statistics indicating that a substantial proportion of hospital admissions result from patients experiencing drug side effects. The existing solutions for preventing and monitoring ADRs, however, seem to operate in isolation. Addressing these gaps calls for the creation of a fully integrated platform for preventing and monitoring ADRs. Central to the success of such a platform is understanding user needs. This research focused on identifying functional needs for physicians and patients, along with non-functional requirements from hospital information system providers. This study employs a user-centered design methodology structured around a series of key steps that collectively guide the process of user needs and requirement identification and analysis. For an overarching view of the functional requirements, questionnaires were utilized to engage both physicians and patients. For gathering non-functional requirements interviews were conducted with Hospital Information System Providers. 37 physicians and 40 patients participated in the survey. Physicians favored Drug Information Checker, Drug-to-Drug Interaction Checker, Patient ADR Report history-based drug checker, and other general features. Patients prioritized ADR Reporting, Medication Reminders, and mobile platform accessibility. Additionally, two hospital system experts highlighted non-functional prerequisites, including interoperability, security, usability, availability, and performance. This study focus encompassed three pivotal actors: physicians, patients, and hospital information system providers. Physicians and patients lent insights into functional requirements that mirror their clinical and personal journeys, respectively. Meanwhile, the contributions of hospital information system providers illuminated the non-functional aspects imperative for a seamlessly integrated platform.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Patient safety stands as a paramount concern in the realm of healthcare, with the paramount objective of minimizing adverse drug reactions (ADRs) and medical errors to elevate the overall quality of patients’ lives. The endeavor to achieve this goal underscores the significance of efficient strategies that not only address existing challenges but also pave the way for an advanced healthcare landscape.
The present landscape of ADR cases paints a somber picture, with statistics indicating that a substantial proportion of hospital admissions – ranging from 2.3 to 21.2% – result from patients experiencing drug side effects [1, 2]. However, it’s noteworthy that less than 5% of these cases of drug side effects are reported by patients themselves [3], pointing to an underrepresentation of actual occurrences. Such a discrepancy emphasizes the need for a comprehensive approach to detecting, preventing, and monitoring ADRs.
An end-to-end strategy to effectively address ADRs encompasses several crucial elements. First and foremost, the accurate identification of patients becomes pivotal, such as comprehending patient medication history, genetics, and drug interactions. This foundational data can then be harnessed to create personalized prescriptions tailored to individual needs [3,4,5,6]. Additionally, the strategy entails continuous monitoring of patients, allowing healthcare providers to swiftly ascertain any adverse effects resulting from prescribed drugs [7]. The essence lies not only in observation but also in the ability to predict and intervene. It is imperative that the data collected throughout this process is not only accurate but also meticulously organized to enable seamless observations, analysis, and, ultimately, predictions [8].
The existing solutions for preventing and monitoring ADRs, however, seem to operate in isolation, failing to align with the comprehensive strategy outlined above [9]. For instance, current clinical decision support systems are fragmented, focusing on basic drug information [10, 11], diagnosis-based drug information [12], patient biometric-based drug information [13, 14], and patient medication history-based drug information [12, 15], without integration with patient health monitoring systems. This lack of integration hampers the potential of these solutions to fully support the end-to-end strategy required for effective ADR management. Addressing this gap and fostering a cohesive healthcare ecosystem calls for the creation of a fully integrated platform for preventing and monitoring ADRs.
This study endeavors to grasp user requirements prior to platform development. Understanding user needs is vital, as user acceptance is pivotal for technological advancements [16, 17]. To begin this journey effectively, a thorough understanding of what healthcare providers, patients, and other stakeholders truly need from the platform is essential. This user-centric approach ensures that the platform not only meets the technical criteria but also aligns seamlessly with the practical needs and expectations of those who will interact with it.
2 Literature review and related works
2.1 Adverse drug reactions (ADR)
An adverse drug reaction (ADR) is characterized by the World Health Organization (WHO) as unfavorable and unwanted effects arising from the use of a medication to treat an illness or aid in diagnosis [18]. In a parallel vein, Edward and Aronson [19] offer a more comprehensive definition, describing ADR as a significantly detrimental or unpleasant response stemming from an intervention tied to the utilization of a medicinal product. Such reactions not only serve as indicators of potential future hazards but also necessitate preventative actions, specific treatments, dosage regimen adjustments, or even product withdrawal. In this study, the Edward and Aronson [19] delineation of ADR will be employed. The spectrum of ADR encompasses six distinct categories: those related to dosage (e.g., toxic effects), those unrelated to dosage (e.g., immunological reactions), instances where both dosage and time play roles, time-related responses (e.g., carcinogenesis), withdrawal-related, and scenarios of unexpected treatment failure (e.g., inadequate oral contraceptive dosing).
Prior investigations have delved into strategies for averting ADR occurrences. Fortescue et al. [4] unveiled that amalgamating computerized physician order entry with clinical decision support systems precipitated a notable 72% reduction in the risk of adverse medication events. Furthermore, Coleman and Pontefract [3] propose tailored prescriptions as an ADR prevention strategy, achievable through the integration of clinical decision support systems into clinical contexts. Notably, Yap et al. [7] underscore the value of ongoing patient surveillance, particularly for at-risk patient groups, in thwarting the onset of ADRs. Given the insights gleaned from the preceding data, this research endeavors to assess two distinct categories of IT solutions for ADR prevention: clinical decision support systems and applications designed for monitoring patient health.
2.2 The current state of IT solutions for preventing and monitoring ADR
In the rapidly evolving healthcare landscape, IT solutions for preventing and monitoring ADRs have taken center stage. A comprehensive literature review was conducted to grasp the current state of these solutions, shedding light on key trends and highlighting potential areas for advancement [9].
The review uncovered notable findings. Firstly, research in this domain is concentrated in developed countries, reflecting resource discrepancies. When it comes to Clinical Decision Support Systems (CDSS), Knowledge-based systems stand out, encompassing features like basic [10, 11] and diagnosis-based drug checks [12], biometrics-based assessments [13, 14], and history-based evaluations [12, 15].
Patient Health Monitoring Applications, primarily on smartphones, offer various features including form-based [20, 21] and in-app survey ADR reporting mechanisms [22,23,24], showcasing a versatile means of patient engagement.
However, a distinct pattern emerges: most studies focus on individual IT solutions for either ADR prevention or monitoring, leaving integrated solutions largely unexplored. While standalone solutions have promise, an integrated platfrom could potentially offer a more comprehensive and effective way to address ADRs [8]. Therefore, this research aims to understand user needs prior to platform development.
3 Research methodology
3.1 Requirement gathering
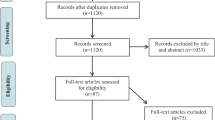
Our study employs a user-centered design methodology. This approach is tailored to ensure that technological solutions are crafted with a deep understanding of user perspectives. The methodology is structured around a series of key steps that collectively guide the process of user needs and requirement identification and analysis [16, 25, 26]. Figure 1 illustrates the step for requirement gathering.
This research was conducted within the dynamic context of Indonesia, a developing nation where research on IT solutions for preventing and monitoring ADRs is notably sparse [9]. To identify the most suitable users and extract their inherent needs, a meticulous data collection process was initiated. This journey began by collecting data from prior projects and research studies, meticulously gleaned from the reported literature [9]. This initial step laid the groundwork for understanding existing knowledge and trends. Furthermore, the insights contributed by physicians from both public and private hospitals in Indonesia proved invaluable. Their expert perspectives, grounded in the country’s healthcare landscape, added depth to our understanding of user requirements.
Step 1: Identification and Selection of Users. The process is composed of two integral sub-steps: User Identification and User Selection. These sub-steps are devised to ensure a comprehensive understanding of the platform’s end users and to tailor the technological solution to their unique needs and expectations.
Sub-Step 1: User Identification. This intricate task entails delineating the various roles within the platform’s ecosystem. In the context of our study, three primary actors were identified, each playing a distinct and significant role in the platform’s functioning. The first actor is Physician. Physician is a pivotal actor responsible for prescribing medications to patients. Their role involves making informed decisions regarding suitable treatments, dosages, and regimens. The second actor is Patient. Patient is another central actor who will ultimately consume the prescribed medication. The last actor is the Provider of Hospital Information Management System. This actor holds a crucial role in maintaining and managing the information systems within the hospital. Integrating new functionalities into the existing Hospital Information Management System is a priority, and understanding this actor’s requirements is essential to ensure a seamless incorporation of the platform into the hospital’s ecosystem.
Sub-Step 2: User Selection. In the intricate process of User Selection, the paramount objective is to curate a representative sample from each of the identified user categories. This ensures that the insights gleaned are robust and reflective of the diverse perspectives within each group. The criteria for selection are thoughtfully tailored to capture the essence of the user group’s characteristics and preferences. To encapsulate the comprehensive spectrum of physician perspectives, specific criteria have been defined for selection. The chosen physicians should: (1) Fall within the age range of 35 to 65, a bracket that encompasses a substantial portion of practicing professionals. Possess a specialist degree, indicating their expertise and specialized knowledge. (2) Work within Class A or B hospitals in Indonesia, where hospital information systems are already implemented, offers an environment for the integration of the platform for preventing and monitoring ADRs at a later stage. (3) Actively engage with and utilize hospital information systems as part of their daily workflow, ensuring that their experiences are closely tied to the platform’s integration.
The selection criteria for patients revolve around ensuring a diverse representation of those who will be consuming the prescribed medication. Emphasis will be placed on assessing the level of smartphone proficiency, as this is essential to ensure that patients can utilize their smartphones effectively for reporting ADRs for monitoring purposes. Chosen patients should: (1) Span an age range of 25 to 65, capturing a broad spectrum of experiences and requirements. (2) Be active users of smartphones, as this technology plays a pivotal role in their interaction with the platform and overall healthcare management.
Finally, for Hospital Information System Provider, the criteria for selection involve: (1) Age criteria spanning from 25 to 65, capturing a range of perspectives and experiences. (2) Holding at least a bachelor’s degree, indicating a certain level of expertise, and understanding of information system integration. (3) Actively participating in the integration and maintenance of the Hospital Information System, as their insights will be integral in understanding the technical requirements and challenges.
Step 2: Interaction with End Users. The second step of our user-centered design methodology involves direct interaction with the end users. This interactive phase is conducted through a combination of interviews and questionnaires, each tailored to extract distinct facets of user requirements.
For an overarching view of the functional requirements, questionnaires were utilized to engage both physicians and patients. Questionnaires offer a structured approach to gather insights into user preferences, behaviors, and expectations, providing a comprehensive understanding of functional needs. These structured surveys probed various dimensions of user needs. The questions themselves were meticulously developed, drawing from the insights derived in the preliminary base of knowledge. These insights were gleaned through literature review and initial interviews conducted with physicians from both public and private hospitals. This ensured that the questions were informed by real-world experiences and industry trends.
Complementing the questionnaire-driven approach, interviews were selected as a dedicated avenue to delve deeper into specific aspects of non-functional requirements. Particularly, interviews were conducted with Hospital Information System Providers to unearth crucial non-functional requirements such as system availability, interoperability, security, and technical specifications. Interviews offer a qualitative depth that allows for nuanced exploration of complex technical considerations, ensuring a thorough understanding of alignment with existing information systems and industry standards. By strategically employing both methods, this research aims to gather a holistic understanding of user and system requirements, laying the foundation for the development of a seamless and user-centric platform.
Step 3: Evaluation. After the completion of data collection from questionnaires and interviews, the evaluation phase will ensue. This phase is dedicated to addressing user needs, which will subsequently inform the formulation of final requirements.
3.2 Requirement analysis
As previously mentioned, we employed questionnaires as a data collection tool to gain insights into the functional requirements from both physicians and patients. These questionnaires employed a Likert scale ranging from 1 to 4, where a score of 1 indicated “very unimportant,” and a score of 4 indicated “very important.” The subsequent analysis of the questionnaires involved the utilization of Descriptive Statistics to assess central tendencies and variabilities. We deemed a particular element as a requirement if the mean score exceeded 3, signifying a consensus among respondents that the functionality was necessary.
The questionnaire for physicians was structured into four distinct categories, each of which delved into specific facets of functional requirements: (1) Drug Checker Features, (2) Result Display Trigger, (3) Alert Display, and (4) General Features. The particulars of the questionnaire items for physicians are elucidated in Table 1. Additionally, to ensure the selection criteria are met for physicians, we employ questions regarding age, education background, frequency of hospital information system usage in a week, and the name of the hospital where the doctor currently works.
Conversely, the patient questionnaire was categorized into three sections: (1) ADR Reporting, (2) Reminder, and (3) Platform. The comprehensive details of the patient questionnaire are outlined in Table 2. Additionaly, to ensure that the selection criteria are fulfilled for patients, we incorporate inquiries concerning age, smartphone ownership, and the frequency of smartphone usage.
In parallel, to collect data pertaining to non-requirements, we conducted semi-structured interviews with hospital information providers. These interviews were focused on the assessment of five software quality attributes: interoperability, security, availability, usability, and performance. The data resulting from these interviews underwent a content analysis to ascertain non-functional requirements. Content analysis involves four stages: (1) decontextualization breaks down interview content into smaller units, labeled with specific codes, (2) recontextualization compares the original content with segmented units for thorough processing, (3) categorization groups segmented content for insight extraction, and (4) compilation documents analysis findings from interviews.
4 Results and discussion
4.1 Physician requirements
The distribution of questionnaires among physicians occurred within the timeframe spanning from July 25th, 2022, to August 25th, 2022, encompassing the participation of 37 physicians holding specialist degrees. Among these respondents, 59.5% were male, while 40.5% were female. Regarding age distribution, 32.4% of respondents fell within the age bracket of 35–40 years, 18.9% were aged between 56 and 60 years, 16.2% were within the 41–45 years age group, and another 16.2% fell within the 51–55 years age category. The remaining respondents were aged between 46 and 50 years. Concerning the hospitals where the physicians worked, 59.5% of respondents were employed at Class B Hospitals, while 40.5% were affiliated with Class A Hospitals.
In terms of professional backgrounds, 37.8% of respondents identified as pediatricians, 10.8% as neurosurgeon specialists, 8.1% as obstetrics and gynecology specialists, 8.1% as heart and blood vessel specialists, and 8.1% as internal medicine specialists. As for their usage patterns of the hospital information system, 51.4% of respondents reported daily utilization, 24.3% used the system three days a week, 13.5% utilized it for two days a week, and the remaining respondents employed the system once a week.
Subsequently, the questionnaire results underwent rigorous analysis employing descriptive statistics. The outcome of this analysis, focusing on central tendency assessment, is elucidated in Table 3.
Additionally, the variability within the questionnaire results was assessed, and Table 4 provides a detailed presentation of the results pertaining to variability measurement.
Based on the assessment result, in the domain of the Drug Information Checker (DC1), it is evident that physicians place considerable importance on the feature enabling access to detailed information about specific medications. The mean score of 3.71 indicates a notably positive perception among respondents, with the majority of them rating this feature highly. Furthermore, the mode and median scores both align at the maximum value of 4, highlighting a consensus among physicians that this functionality is indeed crucial. This convergence of central tendency metrics suggests a robust agreement within the surveyed group regarding the significance of having comprehensive medication information at their disposal. An intriguing aspect of the analysis is the minimal variability observed in this category, as indicated by the low variance (0.32) and standard deviation (0.57) scores. The range of scores, spanning a mere 2 points, underscores a consistent perspective among physicians. The absence of an interquartile range (IQR) further reinforces the notion that respondents exhibited little divergence in their assessments. This consistency may imply a shared professional consensus within the medical community regarding the necessity of accessing detailed medication information, underscoring the stability of this requirement across the surveyed sample. These findings assume heightened significance in the context of developing a Clinical Decision Support System geared toward averting ADR. The strong consensus and minimal variability observed among physicians regarding the importance of accessing comprehensive medication information signal a clear and imperative requirement for the CDSS. This underscores the critical role of robust features for medication data retrieval within the system. Incorporating such features aligns closely with the objective of enhancing clinical decision-making, mitigating the risks associated with ADR, and ultimately advancing patient safety and healthcare quality. The uniformity of opinion among physicians not only highlights the system’s need but also reaffirms the necessity for healthcare technology developers to tailor CDSS solutions precisely to these well-defined requirements, ensuring that they effectively address the challenges and demands of the medical field.
Within the domain of the Drug-to-Drug Interaction Checker (DC2), it is evident that physicians assign a high level of importance to the feature focused on assessing drug interactions. The mean score of 3.82 suggests a robust consensus among respondents, with the majority of them rating this feature quite favorably. Both the mode and median scores, which align at the maximum value of 4, further underscore the unanimous agreement among physicians that this functionality is indispensable. This convergence of central tendency metrics signifies a shared perception within the surveyed group regarding the critical nature of assessing drug interactions in clinical practice. An interesting aspect of the analysis is the minimal variability observed in this category, as indicated by the low variance (0.14) and standard deviation (0.38) scores. The range of scores, spanning just 1 point, highlights a consistent viewpoint among physicians. The absence of an interquartile range (IQR) further reinforces the notion that respondents displayed minimal divergence in their assessments. This consistency underscores a collective professional agreement within the medical community regarding the necessity of assessing drug interactions as an integral aspect of clinical decision support. These findings hold significant implications for the development of a Clinical Decision Support System (CDSS) aimed at preventing ADR, especially concerning drug interactions. The strong consensus among physicians and the minimal variability in their responses emphasize the critical role that robust drug interaction assessment features should play within the CDSS. This alignment with the preferences of medical practitioners reinforces the CDSS’s potential to enhance clinical decision-making, reduce the risks associated with ADR, and ultimately advance patient safety. The consistent viewpoint within the medical community highlights the importance of closely aligning technology solutions with these well-established requirements, ensuring that the CDSS effectively addresses the pressing issue of drug interactions in healthcare practice.
In the realm of the Biometrics-Based Drug Checker (DC3), it is apparent that there exists a notable diversity of perspectives among physicians concerning the feature that assesses medication suitability based on a patient’s genetics. The mean score of 2.71 reflects a range of responses, suggesting a less uniform consensus compared to some other features. The mode and median scores, both at 3, indicate a degree of centrality in the ratings, but the variability in responses is noteworthy. The range of scores, spanning 3 points, highlights the spectrum of opinions among physicians, signifying that while some perceive this feature as moderately important, others may hold different viewpoints. An important facet of the analysis is the considerable variability observed in this category, as indicated by the relatively high variance (1.21) and standard deviation (1.10) scores. The wide range of scores underscores the dispersion of opinions and the presence of both high and low ratings among respondents. The interquartile range (IQR) of 2 further emphasizes the variance in responses. This variation suggests that physicians’ perspectives on the significance of genetics-based medication suitability assessment are more diverse compared to some other requirements, indicating a need for careful consideration and further exploration of this feature in the context of the Clinical Decision Support System (CDSS) development. These findings have noteworthy implications for the development of a Clinical Decision Support System (CDSS), particularly concerning the incorporation of genetics-based medication suitability assessment. The diversity of opinions and the significant variability observed in responses highlight the need for customization and flexibility within the CDSS. While some physicians may consider genetics-based assessment crucial for patient safety, others may have reservations or alternative viewpoints. Therefore, the CDSS should be designed to accommodate a range of preferences and allow for tailored use by medical practitioners. This approach ensures that the CDSS effectively addresses the multifaceted nature of genetics-based medication suitability in clinical practice, providing healthcare professionals with the tools necessary to make informed decisions aligned with their individual perspectives and clinical contexts.
Within the context of the Patient ADR Report History-Based Drug Checker (DC4), it is evident that physicians accord significant importance to the feature that verifies whether patients have reported ADRs to their prescribed medications. The mean score of 3.68 signifies a robust consensus among respondents, indicating a prevailing sentiment that this functionality holds considerable value. Furthermore, both the mode and median scores, at the maximum value of 4, underscore the unanimous agreement among physicians regarding the crucial role of verifying patient-reported ADRs. This convergence of central tendency metrics reflects a shared belief within the surveyed group about the significance of patient ADR reporting in clinical decision support. An interesting aspect of the analysis is the moderate variability observed in this category, as indicated by the variance (0.33) and standard deviation (0.58) scores. The range of scores, spanning 2 points, highlights a degree of diversity in opinions among physicians, albeit not as pronounced as in some other features. The interquartile range (IQR) of 0.5 suggests some dispersion in responses, reflecting varying levels of importance attributed to patient ADR reporting verification. This diversity may indicate that while the majority of physicians view this feature favorably, there exist nuances in how different practitioners perceive its significance. These findings carry significant implications for the development of a Clinical Decision Support System (CDSS), especially concerning the integration of patient ADR report history-based features. The consensus among physicians and the moderate variability in responses emphasize the pivotal role that verifying patient-reported ADRs should play within the CDSS. Such functionality can enhance clinical decision-making, contribute to patient safety, and provide healthcare professionals with valuable insights into medication tolerability. While there is a shared belief in the importance of this feature, the diversity in opinions also calls for flexibility in CDSS design to cater to varying perspectives and clinical contexts. It underscores the need for a customizable approach that allows physicians to leverage patient ADR reporting verification in a manner that aligns with their individual practice and patient care needs.
In the category Generate Recommendation Result by Clicking Multiple Buttons (RD1), it is evident that users express a strong inclination toward this user interface approach. The mean score of 3.65 indicates a notable preference for allowing users to generate results by selecting multiple options. Both the mode and median scores, at 4, underscore the widespread consensus among users in favor of this method. The central tendency metrics reflect a unanimous agreement among respondents that this approach aligns with their expectations of user-friendliness and efficiency. This consensus signifies a shared belief that a multi-option selection process facilitates a more tailored and precise recommendation generation experience within the CDSS. Conversely, in the category Generate Recommendation Result by Clicking Single Button (RD2), users also express a favorable opinion, although slightly less pronounced compared to the multiple buttons option. The mean score of 3.68 suggests that users still view this approach positively. Furthermore, both the mode and median scores align at 4, indicating a consensus among users that generating results with a single button click is an acceptable method. The central tendency metrics in this category demonstrate that this approach is perceived as efficient and convenient by the user base, albeit with slightly less uniform agreement compared to the multiple buttons option. These findings hold substantial implications for the design of the Clinical Decision Support System’s (CDSS) user interface. While both options garner user approval, the preference for generating results by clicking multiple buttons appears to be slightly stronger. However, the minimal variability in scores for both options indicates that either approach can be accommodated within the CDSS without significant user dissatisfaction. The key takeaway is the importance of providing flexibility and choice to users, allowing them to select the interface method that best aligns with their workflow and preferences. Ultimately, this approach ensures that the CDSS caters to a diverse user base and enhances their overall experience by providing a user-friendly and adaptable interface for generating recommendation results.
In the category Passive Alert (AD1), it is evident that users express a notable preference for this style of alert presentation within the CDSS. The mean score of 3.54 signifies a significant preference for integrating alerts into the results, eliminating the need for user-initiated actions. Both the mode and median scores, at 4, highlight a consensus among users that this passive approach is favored. The central tendency metrics reflect a unanimous agreement among respondents that passive alerts align with their expectations of streamlined workflow and efficiency. This consensus suggests that users appreciate an unobtrusive approach where alerts seamlessly blend into the result display, promoting a smooth user experience. In the category Active Alert (AD2), users also express approval, albeit slightly less pronounced compared to passive alerts. The mean score of 3.48 suggests that users still view the active alert approach positively. Furthermore, both the mode and median scores align at 4, indicating a consensus among users that displaying alerts as pop-up notifications is an acceptable method. The central tendency metrics in this category demonstrate that this approach is perceived as effective and informative by the user base, albeit with slightly less uniform agreement compared to passive alerts. These findings have significant implications for the presentation of alerts within the Clinical Decision Support System’s (CDSS) interface. While passive alerts garner stronger user preference, the approval for active alerts is considerable. The minimal variability in scores for both options indicates that either approach can be effectively incorporated into the CDSS without causing user dissatisfaction. The key takeaway is the importance of providing flexibility in alert presentation to cater to diverse user preferences. This approach ensures that the CDSS accommodates varying user needs and workflows, enhancing their overall experience by allowing them to choose the alert style that aligns best with their clinical practice and usability expectations.
Within the realm of Integration with Existing Hospital Information Systems (GF1), it is evident that users place substantial importance on the seamless integration of the CDSS with their current hospital information infrastructure. The mean score of 3.68 signifies a robust consensus among respondents, indicating a prevailing sentiment that integration holds considerable value. Both the mode and median scores, at 4, underscore the unanimous agreement among users regarding the crucial role of integrating the CDSS with their existing systems. These central tendency metrics reflect a shared belief within the surveyed group about the significance of streamlined data flow and interoperability in supporting their clinical decision-making processes. An interesting aspect of the analysis is the moderate variability observed in this category, as indicated by the variance (0.28) and standard deviation (0.53) scores. The range of scores, spanning 2 points, highlights some diversity in opinions among users, although not to a significant extent. The interquartile range (IQR) of 1 suggests that there is a degree of consensus, with most users viewing integration positively. This limited variability indicates that while individual preferences may vary slightly, the majority of users perceive integration as a valuable feature that enhances the functionality and utility of the CDSS. These findings hold significant implications for the development of the Clinical Decision Support System (CDSS) and its integration with hospital information systems. The strong consensus among users and the moderate variability in responses emphasize the pivotal role that seamless integration should play within the CDSS. Such integration can enhance clinical decision-making, data accuracy, and overall healthcare quality. While there may be some nuances in user preferences, the limited variability suggests that the CDSS should prioritize and ensure compatibility with existing hospital information systems. This approach aligns with the expectations and needs of the user base and underscores the importance of delivering a user-friendly, integrated solution that seamlessly supports hospital workflows and facilitates efficient patient care.
Within the domain of Requesting Documentation of Reasons for Not Following System Recommendations (GF2), it is evident that users attach significant importance to this feature. The mean score of 3.42 signifies a noteworthy consensus among respondents, highlighting a prevailing sentiment that requesting documentation holds considerable value. Both the mode and median scores, at 4, underscore the unanimous agreement among users regarding the crucial role of documenting reasons for non-compliance with system recommendations. These central tendency metrics reflect a shared belief within the surveyed group about the significance of transparency and accountability in clinical decision-making processes. An interesting aspect of the analysis is the noticeable variability observed in this category, as indicated by the relatively high variance (0.66) and standard deviation (0.81) scores. The range of scores, spanning 3 points, highlights a degree of diversity in opinions among users. The interquartile range (IQR) of 1 suggests a dispersion in responses, reflecting varying levels of importance attributed to documenting user decisions. This variability indicates that while the majority of users view this feature favorably, there exist nuanced perspectives on the necessity and extent of documentation. These findings have significant implications for the development of the Clinical Decision Support System (CDSS) and its approach to documenting user decisions. The consensus among users and the noticeable variability in responses underscore the importance of providing an option for users to document their reasons for not following system recommendations. Such documentation can enhance transparency, facilitate quality improvement efforts, and promote a culture of accountability in healthcare decision-making. However, the variability in opinions also calls for flexibility in the CDSS design, allowing users to customize the level of documentation to align with their workflow and clinical practice. This approach ensures that the CDSS supports diverse user preferences and effectively balances the need for documentation with the efficiency of the clinical workflow.
In the domain of System Functionality in Offline Mode (GF3), it is evident that users place considerable emphasis on the ability of the system to remain operational when offline and sync data once an online connection is re-established. The mean score of 3.68 signifies a robust consensus among respondents, indicating a prevailing sentiment that this feature holds considerable value. Both the mode and median scores, at 4, underscore the unanimous agreement among users regarding the crucial role of offline functionality and data synchronization. These central tendency metrics reflect a shared belief within the surveyed group about the significance of uninterrupted system access and the secure handling of data, even in offline scenarios. An important aspect of the analysis is the limited variability observed in this category, as indicated by the low variance (0.33) and standard deviation (0.58) scores. The range of scores, spanning 2 points, indicates that users are largely aligned in their opinions, with minimal divergence in responses. The interquartile range (IQR) of 0.5 further reinforces the notion that respondents exhibited little variation in their assessments. This consistency implies a shared professional consensus within the user community about the necessity of offline functionality and data synchronization, highlighting its stability as a requirement for the Clinical Decision Support System (CDSS). These findings bear significant implications for the development of the Clinical Decision Support System (CDSS), particularly concerning its reliability and continuity of service. The strong consensus among users and the limited variability in responses underscore the pivotal role that offline functionality and data synchronization should play within the CDSS. Such features can enhance the system’s reliability, ensure seamless access to critical information even in offline settings, and safeguard against data loss or disruption. The uniformity of opinion among users also emphasizes the importance of aligning technological solutions with their requirements, highlighting the potential for the CDSS to excel in providing continuous, dependable support to healthcare professionals, regardless of their connectivity status.
4.2 Patient requirements
The distribution of questionnaires transpired within a specified temporal range, spanning from August 20th, 2022, to September 8th, 2022, soliciting responses from a cohort of 40 valid participants, with a balanced gender distribution of 50% male and 50% female respondents. The age composition of the respondents exhibited the following distribution: 30% were aged between 61 and 65 years, 30% fell within the 31–35 age bracket, 12.5% were in the 25–30 age group, 7.5% were between 36 and 40 years old, 7.5% represented the 56–60 age category, 5% belonged to the 41–45 age range, while the remainder were distributed among those aged 46–50.
Subsequently, the questionnaire responses underwent a meticulous analysis utilizing descriptive statistical techniques. The findings pertaining to the central tendency assessment are presented in Table 5. Additionally, the measurement of variability within the questionnaire results is delineated in Table 6.
In terms of reporting related features, the analysis of the questionnaire results indicates that patients attach substantial importance to both the In-App Survey and Form-Based Reporting features for reporting ADR within the patient health monitoring application. For the In-App Survey feature (AR1), the central tendency statistics demonstrate a strong consensus, with a mean score of 3.54, a mode of 4, and a median of 4. These values reflect a collective sentiment that this feature is vital for patients to report drug side effects and assess their quality-of-life post-drug consumption. Similarly, for the Form-Based Reporting feature (AR2), the central tendency statistics reveal a high level of importance, with a mean score of 3.63, a mode of 4, and a median of 4, underscoring its significance.
The analysis highlights that both the In-App Survey and Form-Based Reporting features are integral components of the patient health monitoring application for reporting ADR. While patients collectively consider both features as highly important, the variability in perceptions is more pronounced for the In-App Survey. This suggests that the application should offer customizable options and user-centric controls for this feature to accommodate diverse perspectives and preferences. Conversely, the relatively low variability for Form-Based Reporting indicates that patients generally agree on its importance, which could allow for a more standardized implementation. Striking a balance between customization and uniformity will be essential in meeting the varied requirements of patients and enhancing their ability to report and manage ADR effectively.
Regarding reminder related features, the analysis of the questionnaire results underscores the importance of both the Drug Reminder and ADR Assessment Reminder features in the patient health monitoring application for facilitating ADR reporting. For the Drug Reminder feature (RM1), the central tendency statistics reveal a robust consensus, with a mean score of 3.60, a mode of 4, and a median of 4. These values collectively convey that patients place substantial importance on the ability to register and receive reminders for drug consumption schedules. Similarly, for the ADR Assessment Reminder feature (RM2), the central tendency statistics demonstrate a high level of significance, with a mean score of 3.57, a mode of 4, and a median of 4, emphasizing its critical role in ensuring timely ADR assessments.
While both features are perceived as crucial, a closer examination of the measure of variability provides additional insights. Both the Drug Reminder and ADR Assessment Reminder features exhibit a range of 2, indicating some variability in patient perceptions, and the variability metrics—variance and standard deviation—align closely. This suggests that while there is a consensus on the importance of these features, individual preferences and requirements may lead to slight variations in their perceived significance. However, the relatively low variability overall indicates that patients generally agree on the importance of receiving reminders related to drug consumption schedules and ADR assessments.
The analysis highlights the paramount role of both the Drug Reminder and ADR Assessment Reminder features in enhancing patient adherence to ADR reporting. Patients collectively prioritize these features to ensure they do not forget crucial tasks related to their drug consumption and ADR assessments. While there are slight variations in perceptions, the low overall variability suggests a broad consensus among patients regarding their significance. Therefore, the application should ensure the effective implementation of these reminder features, allowing for customization to accommodate individual patient preferences while maintaining a standardized and user-friendly approach to support timely and accurate ADR reporting.
Within the realm of platform for the PHM, the analysis of the questionnaire results regarding the preferred platform for the Patient Health Monitoring application highlights a clear preference among patients for mobile accessibility. The Mobile platform (PL1), which allows the application to be used on smartphones, exhibits robust central tendency statistics with a mean score of 3.57, a mode of 4, and a median of 4. These values collectively convey that patients place significant importance on the ability to access the application via their smartphones. Furthermore, the relatively low variability, as indicated by a range of 2, variance of 0.43, and standard deviation of 0.65, suggests a consistent consensus among patients regarding the desirability of mobile accessibility.
In contrast, while the Desktop platform option (PL2), enabling access via a browser on a PC/Laptop, is still considered important, the statistics indicate a slightly lower level of significance among patients. The central tendency metrics for Desktop reveal a mean score of 3.05, a mode of 3, and a median of 3, indicating a preference but with less intensity compared to the Mobile platform. The range of 2, variance of 0.47, and standard deviation of 0.68 imply a bit more variability in patient perceptions. This suggests that while there is a general agreement on the importance of Desktop accessibility, individual preferences may vary to a slightly greater degree than with the Mobile platform.
Furthermore, the analysis demonstrates that patients prioritize mobile accessibility for the Patient Health Monitoring application, with a clear consensus on its importance. The mobile option aligns closely with patients’ preferences for convenience and on-the-go access. However, the Desktop platform is also valued, albeit to a somewhat lesser extent, indicating the need for a multi-platform approach to accommodate varying patient preferences. The application’s development should prioritize a user-friendly mobile interface while ensuring that the Desktop option remains robust and user-centric to address the diverse requirements of patients who may prefer accessing it via PC or laptop.
4.3 Hospital information system provider requirements
To comprehensively understand the non-functional requirements essential for seamless integration, maintenance, and interoperability of the proposed platform, semi-structured interviews were conducted with two seasoned hospital information system specialists from distinct private hospitals. Boasting over five years of experience in managing and integrating hospital information systems, these interviewees provided invaluable insights into four critical facets: Interoperability, Security, Usability, Availability, and Performance.
In the realm of interoperability, the interviewees highlighted the pivotal role of Application Programming Interfaces (APIs) adhering to the HL7® FHIR® (Fast Healthcare Interoperability Resources) standard. This standard is embraced due to its widespread adoption within the healthcare sector for seamless data exchange. The integration of the proposed platform with existing healthcare software aligns with this widely accepted standard, ensuring unhindered data flow and connectivity.
The paramount importance of information security was emphasized, and the ISO 27,001 standard emerged as a crucial benchmark. ISO/IEC 27,001, an international standard for managing information security, was identified as a prerequisite for the proposed platform. This underlines the commitment to safeguarding patient data and sensitive information, bolstering trust, and ensuring compliance with rigorous security standards.
The usability aspect was approached with sensitivity to operational continuity. The external system’s design must prevent disruptions to the primary physician workflows, ensuring that it seamlessly integrates into the hospital information system without impeding core activities. Furthermore, the external system’s integration was underscored, preventing it from functioning as a standalone entity. Instead, it should merge seamlessly into the hospital information system, fostering a cohesive and unified ecosystem.
Given the critical nature of healthcare operations, the concept of high availability (SLA 99.9%) emerged as a non-negotiable requirement. Recognizing the pivotal role of the platform within healthcare operations, ensuring consistent accessibility and uptime was deemed imperative. This commitment to high availability aligns with the industry’s expectations for uninterrupted and reliable system access.
Performance emerged as a pivotal factor to maintain physician efficiency. Acknowledging that sluggish external systems could potentially hinder patient care, a swift system response time was set as a criterion. A stringent response time threshold of under three seconds was identified to ensure that the external system seamlessly complements physician activities without inducing delays.
5 Conclusion
This study centers on a pivotal endeavor, the identification of user needs essential for the development of an adept platform for preventing and monitoring ADR. Employing a user-centered design methodology, we undertook a rigorous exploration to grasp the fundamental requisites pivotal to the platform’s success.
Delving into the intricate tapestry of healthcare, our focus encompassed three pivotal actors: physicians, patients, and hospital information system providers. With distinct yet interconnected roles, these stakeholders contributed their perspectives on essential functionalities and non-functional prerequisites. Physicians and patients, as end-users, lent insights into functional requirements that mirror their clinical and personal journeys, respectively. Meanwhile, the contributions of hospital information system providers illuminated the non-functional aspects imperative for a seamlessly integrated platform.
These identified requirements collectively serve as the compass guiding the software architecture design for developing a platform for preventing and monitoring ADRs. The next steps of this research involve developing a platform based on service-oriented architecture, where user requirements play a pivotal role in performing service identification.
Acknowledging the scope of this study, it is important to recognize that certain limitations inherent to our research warrant consideration. The physician requirements, while capturing overarching needs, suggest a future avenue of exploration—diving deeper into the specific demands of various specialist fields. Such a nuanced understanding would enable the platform to address unique clinical workflows, fostering tailored care delivery. Besides that, the patient requirements, focusing on manual interactions such as in-app surveys and form submissions, present an opportunity for refinement. Future research could explore innovative ways to minimize manual actions, streamlining patient engagement and data input for a more seamless experience. In analyzing the non-functional requirements from the hospital information system provider perspective, it’s imperative to acknowledge that the interviews predominantly delved into technical aspects. Future analyses should encompass broader considerations, including economic feasibility, to ensure the platform aligns not only with technical standards but also with real-world resource allocation.
Data availability
This study employs data that was meticulously collected by the authors. Questionnaires were disseminated through the Google Forms platform, while interviews were conducted via teleconferencing.
References
Chan SL, Ang X, Sani LL et al (2016) Prevalence and characteristics of adverse drug reactions at admission to hospital: a prospective observational study. Br J Clin Pharmacol 82:1636–1646. https://doi.org/10.1111/bcp.13081
Sendekie AK, Netere AK, Tesfaye S et al (2023) Incidence and patterns of adverse drug reactions among adult patients hospitalized in the University of Gondar comprehensive specialized hospital: a prospective observational follow-up study. PLoS ONE 18:e0282096. https://doi.org/10.1371/journal.pone.0282096
Coleman JJ, Pontefract SK (2016) Adverse drug reactions. Clin Med 16:481–485. https://doi.org/10.7861/clinmedicine.16-5-481
Fortescue EB, Kaushal R, Landrigan CP et al (2003) Prioritizing strategies for preventing medication errors and adverse drug events in Pediatric inpatients. Pediatrics 111:722–729. https://doi.org/10.1542/peds.111.4.722
Vogenberg FR, Isaacson Barash C, Pursel M (2010) Personalized medicine: part 1: evolution and development into theranostics. P T 35:560–576
Welch BM, Kawamoto K (2013) Clinical decision support for genetically guided personalized medicine: a systematic review. J Am Med Inform Assoc 20:388–400. https://doi.org/10.1136/amiajnl-2012-000892
Yap KY-L, Low HX, Koh KS et al (2013) Feasibility and Acceptance of a Pharmacist-Run Tele-Oncology Service for Chemotherapy-Induced nausea and vomiting in Ambulatory Cancer patients. Telemedicine e-Health 19:387–395. https://doi.org/10.1089/tmj.2012.0136
Dorajoo SR, See V, Chan CT et al (2017) Identifying potentially avoidable readmissions: a medication-based 15-Day readmission risk stratification algorithm. Pharmacotherapy: J Hum Pharmacol Drug Therapy 37:268–277. https://doi.org/10.1002/phar.1896
Khalil A-A, Lumban Gaol F, Subirosa Sabarguna B, Prabowo H (2021) IT Solutions for Preventing and Monitoring Adverse Drug Reactions: A Systematic Literature Review. In: 2021 5th International Conference on Computational Biology and Bioinformatics. ACM, New York, NY, USA, pp 56–61
Henshall C, Cipriani A, Ruvolo D et al (2019) Implementing a digital clinical decision support tool for side effects of antipsychotics: a focus group study. Evid Based Mental Health 22:56–60. https://doi.org/10.1136/ebmental-2019-300086
Mulder-Wildemors LGM, Heringa M, Floor-Schreudering A et al (2020) Reducing Inappropriate Drug Use in older patients by Use of clinical decision support in Community Pharmacy: a mixed-methods evaluation. Drugs Aging 37:115–123. https://doi.org/10.1007/s40266-019-00728-y
Shoshi A, Müller U, Shoshi A et al (2017) KALIS - An eHealth System for Biomedical Risk Analysis of Drugs. Stud Health Technol Inf 236:128–135
Roncato R, Dal Cin L, Mezzalira S et al (2019) FARMAPRICE: A Pharmacogenetic Clinical Decision Support System for Precise and Cost-Effective Therapy. Genes (Basel) 10:. https://doi.org/10.3390/genes10040276
Schwartz PJ, Woosley RL (2016) Predicting the unpredictable. J Am Coll Cardiol 67:1639–1650. https://doi.org/10.1016/j.jacc.2015.12.063
Yang C-Y, Lo Y-S, Chen R-J, Liu C-T (2018) A clinical decision support engine based on a National Medication Repository for the detection of potential duplicate medications: design and evaluation. JMIR Med Inf 6:e6. https://doi.org/10.2196/medinform.9064
Bajenaru L, Marinescu IA, Dobre C et al (2020) Towards the development of a personalized healthcare solution for elderly: from user needs to system specifications. In: 2020 12th International Conference on Electronics, Computers and Artificial Intelligence (ECAI). IEEE, pp 1–6
IANCULESCU M, ALEXANDRU A (2016) Silver Digital Patient, a New Emerging Stakeholder in Current Healthcare. ProActiveAgeing: a Case Study. Stud Inf Control 25. https://doi.org/10.24846/v25i4y201607
Sahu RK, Yadav R, Prasad P et al (2014) Adverse drug reactions monitoring: prospects and impending challenges for pharmacovigilance. Springerplus 3:695. https://doi.org/10.1186/2193-1801-3-695
Edwards IR, Aronson JK (2000) Adverse drug reactions: definitions, diagnosis, and management. Lancet 356:1255–1259. https://doi.org/10.1016/S0140-6736(00)02799-9
Charlston S, Siller G (2018) Teledermatologist expert skin advice: a unique model of care for managing skin disorders and adverse drug reactions in hepatitis C patients. Australas J Dermatol 59:315–317. https://doi.org/10.1111/ajd.12803
Copeland AC, Foster MC, Muluneh B et al (2019) The utility of a telemedicine platform to monitor adherence and adverse effects of tyrosine kinase inhibitors. Leuk Lymphoma 60:1842–1844. https://doi.org/10.1080/10428194.2018.1551540
Ithnin M, Mohd Rani MD, Abd Latif Z et al (2017) Mobile App Design, Development, and publication for adverse drug reaction assessments of causality, severity, and preventability. JMIR Mhealth Uhealth 5:e78. https://doi.org/10.2196/mhealth.6261
Jabaley CS, Wolf FA, Lynde GC, O’Reilly-Shah VN (2018) Crowdsourcing sugammadex adverse event rates using an in-app survey: feasibility assessment from an observational study. Ther Adv Drug Saf 9:331–342. https://doi.org/10.1177/2042098618769565
Kulenovic A, Lagumdzija-Kulenovic A (2020) Using PM-TOM for the minimization of adverse drug and Gene Interactions in therapies for common multi-diseases. Stud Health Technol Inf 272:205–208. https://doi.org/10.3233/SHTI200530
Kujala S, Kauppinen M (2004) Identifying and selecting users for user-centered design. In: Proceedings of the third Nordic conference on Human-computer interaction - NordiCHI ’04. ACM Press, New York, New York, USA, pp 297–303
Maguire M, Bevan N (2002) User Requirements Analysis. pp 133–148
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The manuscript was written by AAK. FLG provided a comprehensive review from a computer science standpoint, BSS conducted a thorough review from a healthcare perspective, and HP performed the final evaluation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was not sought for the present study. Due to the content of the questionnaire and the anonymous data processing, no implications could be identified.
Consent to participate
Informed consent was obtained from all interview participants through written communication via email and from questionnaire respondents via survey software. They were explicitly informed that their data would be used solely for research purposes.
Consent for publication
The manuscript doesn’t contain any individual person’s data. Qualitative and quantitative data have been anonymized.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalil, AA., Gaol, F.L., Sabarguna, B.S. et al. Navigating personalized medication: unveiling user needs to forge a cutting-edge platform for proactive prevention and monitoring of adverse drug reactions. Requirements Eng 29, 357–369 (2024). https://doi.org/10.1007/s00766-024-00426-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00766-024-00426-1