Abstract
Purpose
The French Society for Biological Psychiatry and Neuropsychopharmacology and the French-speaking Marcé Society have joined forces to establish expert recommendations on the prescription of psychotropic drugs before, during, and after pregnancy in women with major depressive disorder (MDD) and bipolar disorder (BD).
Methods
To elaborate recommendations, we used the RAND/UCLA Appropriateness Method, which combines scientific evidence and expert clinicians’ opinions.
A written survey was completed by 48 psychiatrists, who have expertise in the management of mood disorders and/or in perinatal psychiatry. Key recommendations are provided by the scientific committee based on data analysis and interpretation of the results of the survey.
Results
The recommendations address the following three areas that are deemed essential in women with mood disorders, with an emphasis on screening, treatment options, and monitoring: (i) management of mood disorders in women of childbearing age, (ii) management during pregnancy, (iii) management during the post-partum period.
As first-line strategies, experts recommend treating mood symptoms during pregnancy and maintaining a pharmacological treatment, even in euthymic or stabilized patients.
First-line options include only medications with no teratogenic risk, and during breastfeeding, only medications without evidence of adverse effects in nursing infants.
Conclusion
The expert consensus guidelines will help facilitate treatment decisions for clinicians in the daily assessment and management of mood disorders in women of childbearing age, during pregnancy, and in the post-partum period.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Major depressive disorders (MDD) and bipolar disorders (BD) are the most severe mood disorders in adulthood. These disorders are frequent (more than 5% of the general population) and affect mainly young people and women, namely women of childbearing age (Kessler et al. 2005).
To achieve remission and prevent relapse of these chronic and often recurrent disorders, multidisciplinary interventions including long-term pharmacological treatments are warranted in most cases.
Considerable efforts have been made to help clinicians in the management of these complex disorders and several national or international scientific societies have produced and regularly updated treatment guidelines (Grunze et al. 2013; Goodwin et al. 2016; MacQueen et al. 2016; Fountoulakis et al. 2017; Yatham et al. 2018; Malhi et al. 2021).
However, treatment recommendations specific to women of childbearing age with mood disorders, as well as during pregnancy and in case of breastfeeding, are rarely included in these treatment guidelines and remain scarce. In addition, a systematic review of treatment options has shown significant heterogeneity across guidelines (Belzeaux et al. 2019). One reason is that for evident ethical reasons, clinical trials involving medication for women in peripartum are very rare. As a consequence, the levels of evidence on the efficacy and safety of medication in this sensitive population are low and are based mainly on retrospective and/or cohort studies or case series.
Although low fecundity has been reported in women suffering from mood disorders and especially BD (Power et al. 2013), most of these patients will experience pregnancy, childbirth, and motherhood. Pregnancy and post-partum are associated with a high risk of relapse in both MDD and BD (Wesseloo et al. 2016) with more than half of the patients undergoing a recurrent mood episode (Stevens et al. 2019). The risk of relapse is even higher in the case of treatment discontinuation during pregnancy. Therefore, the main objective is to stabilize the patient’s mood before pregnancy and to encourage planned pregnancies in women of childbearing age. Overall, mood episodes during pregnancy and post-partum periods are very difficult to manage pharmacologically, as they require to take into account the teratogenic, neonatal, and neurodevelopmental risks associated with some psychotropic medications, the counter-indications for some medications during breastfeeding, and also potential negative side effects with specific consequences in post-partum (e.g., sedation that impairs newborn care) (Sutter-Dallay et al. 2015). These considerations often negatively impact pregnancy planning but also affect treatment adherence before and during pregnancy.
In such a context, it is disconcerting that treatments counter-indicated in women of childbearing age are still prescribed frequently in the large majority of countries. For example, we reported that more than 15% in BD women of childbearing age in the French FACE-BD cohort have received valproate in the last years (Samalin et al. 2020).
Thus, specific recommendations for the treatment of women of childbearing age with mood disorders, including during peripartum, remain an important need. First of all, such recommendations will help clinicians refine the long-term therapeutic management of these patients by rating treatment strategies according to their teratogenic risk. Secondly, it is also necessary to offer guidance to minimize risks through good practices and to fine-tune therapeutic options on the basis of clinical characteristics of mood disorders in the case of planned or desired pregnancy, as well as during pregnancy and breastfeeding. Finally, guidelines may help all health professionals reduce stigma about childbearing in this specific population and improve perinatal health by promoting access to specialized care.
Therefore, the French Society for Biological Psychiatry and Neuropsychopharmacology (AFPBN) and the French-speaking Marcé Society have joined forces to establish expert recommendations on the prescription of psychotropic drugs before, during, and after pregnancy in women with mood disorders.
Materials and methods
MDD and BD share common clinical manifestations and show a comparable risk of relapse during peripartum. We therefore developed recommendations for both pathologies, and we present the corresponding findings here together.
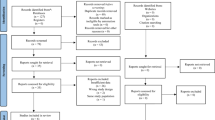
Expert recommendations were determined using the RAND/UCLA Appropriateness Method (for a full description of the task force organization and expert panel, see Supplementary materials). This method combines scientific evidence and expert opinion to assess the appropriateness of medical procedures (Llorca et al. 2010; Bennabi et al. 2019). It involves the following steps: (I) comprehensive review and analysis of the literature with regard to the research question conducted by a scientific committee, (II) elaboration of a questionnaire to collect experts’ opinions for several clinical situations, (III) scoring of the questionnaires, (IV) analysis of the experts’ opinions and drafting of the final report, (V) peer-review phase, (VI) diffusion of the recommendations.
The procedures were approved by an independent national ethics committee (IRB 00013040).
Questionnaire development
First, the scientific committee (RB, FG, LS, ALS, EM, JP, AA, LB) conducted synthesis and analysis of the available data on the management of mood disorders (MDD and BD) in women of childbearing age and at peripartum.
To find all published relevant studies, we performed a literature search in PubMed and EMBASE using the keywords “childbearing age,” “perinatal,” “pregnancy,” “childbirth,” “postpartum,” “breastfeeding,” “major depressive disorder,” “bipolar disorder,” “guidelines,” “pharmacotherapy.” Based on this review, the committee developed a questionnaire consisting of 32 questions that covered 274 therapeutic options; see Supplementary Material. These questions were regrouped into three areas:
-
Management of mood disorders in women of childbearing age: ranking of treatments for the management of mood disorders according to their teratogenic risk (questions 1 to 7), strategies to minimize the risks associated with the use of psychotropic drugs for the treatment of mood disorders (question 8), preconception care: information and advice to share, relevant clinical characteristics of mood disorder to guide therapeutic strategies before a planned pregnancy (questions 10 to 12)
-
Management of mood disorders during pregnancy: screening for a mood disorder, ranking of treatments for the management of mood disorders according to their teratogenic risk, treatment options, treatment monitoring, and follow-up (questions 13 to 25)
Management of mood disorders during post-partum: screening for a mood disorder, information about breastfeeding, ranking of treatments for the management of mood disorders according to their lactation risk (questions 26 to 32)
Our knowledge about the teratogenic risk and lactation risk of medications for the management of mood disorders is constantly improving and the rating of a given drug may change in the future with developing knowledge. Therefore, we chose to develop “sustainable” recommendations based on teratogenic risk categories and lactation risk categories rather than individual drugs. This approach will ensure the usefulness and applicability of these recommendations even if new knowledge or evidence about drug-related risks becomes available in the near future.
A teratogenic risk category was defined for drugs used in pregnancy according to their documented safety information based on the French Reference Centre for Teratogenic Agents (Elefant et al. 2014; CRAT 2023). This categorization applies only to recommended doses.
The classification includes the following:
-
No risk: drugs that have been taken by a large number of pregnant women without any proven increased risk of birth defect (e.g., lamotrigine < 200 mg/j, quetiapine, sertraline)
-
Intermediate risk: drugs that, due to their effects, may cause harm to the fetus or drugs for which human data is lacking (i.e., carbamazepine, lithium, fluvoxamine)
-
High risk: drugs that have caused or may cause birth defects (i.e., valproate)
The lactation risk categories were adapted from the Thomas Hale classification for the breastfeeding safety of medications (Table 1).
Rating scale
The questionnaire was designed to be completed online by experts in mood disorders and/or perinatal psychiatry (see below).
Each expert answered each question according to a rating scale from 0 to 9 derived from a variation of the “Nominal Group” method, developed by the Rand Corporation and the University of California in the USA (“RAND/UCLA appropriateness rating method”), 0 meaning a “total disagreement” or “a formal contraindication” and 9 indicating a “total agreement” or “a formal indication” (Fig. 1).
Expert selection
The Scientific Committee with the support of the AFPBN and the Francophone Marcé Society selected 61 French psychiatrists considered to be experts in the management of mood disorders and/or in perinatal psychiatry.
The selection criteria defined by the Scientific Committee were as follows:
-
Number of years of practice ≥ 5
-
Number of patients currently seen for mood disorders and/or in perinatal period ≥ 30 per month on average or representing more than 30% of the daily clinical activity
-
Participation in research projects and/or publication(s) and/ or communication(s) of research results in the field of mood disorders and/or perinatal psychiatry over the last 5 years
Each expert was invited and consulted individually.
Data analysis
The responses to the different questions or propositions were qualitatively and quantitatively analyzed (number of answers, median, mean, standard deviation, minimum, maximum) (Table 2):
First intention treatment/strategy was defined if at least 50% of the answers to the question were in the zone 7–9 and less than 20% were in the zone 0.
Second intention treatment/strategy was defined if less than 50% of the answers to the question were in the zone 7–9, at least 50% were in the cumulated zones 7–9 and 4–6, and less than 20% were in the zone 0.
Third intention treatment/strategy was defined if less than 50% of the answers to the question were in the cumulated zones 7–9 and 4–6 and less than 20% were in the zone 0.
Contraindication was defined if at least 50% of the answers were in the zone 0.
For all other cases, the answer was considered non-consensual.
Results
Expert panel
Forty-eight experts, representing 79% of those contacted, completed the questionnaire between January 2022 and May 2022. The reasons for the non-participation of the remaining 13 experts were as follows: no response to the invitation, lack of time, failure to start filling out the questionnaire online despite initial positive response.
The sociodemographic data and professional activities of the experts’ panel are presented in Table 3.
Management of mood disorders in women of childbearing age
The following sections summarize the key recommendations established based on data analysis and interpretation of the results by the Scientific Committee (questions and raw data are available in supplementary materials).
Rating strategies for the management of mood disorders in women of childbearing age according to the teratogenic risk of the treatment
In the acute phase, it is recommended to use the following:
-
As first-line (strategy of choice), an effective treatment (i.e., antidepressant in case of MDD or mood stabilizers in case of BD) without teratogenic risk
-
As second-line, an effective treatment with intermediate teratogenic risk
During the maintenance phase, in order to reduce the risk of a recurrent mood episode, it is also recommended to use the following:
-
As first-line (strategy of choice), an effective treatment without teratogenic risk
-
As second-line, an effective treatment with intermediate teratogenic risk
The use of high-risk teratogenic treatment, including in severe clinical situations or during hospitalization, is counter-indicated. It should be noted that, to this date, no approved antidepressant is classified as a high-risk teratogenic treatment whereas certain mood stabilizers, such as valproate and its derivatives, are.
The use of long-acting antipsychotics is recommended as first-line therapy in women who do not plan to be pregnant in the coming months in case of BD with poor adherence but is not recommended in case of planned pregnancy.
Experts did not consider age as a factor in the choice of treatment strategy.
Strategies to minimize the risks associated with the use of psychotropic drugs for the treatment of mood disorders before pregnancy
For all psychotropic drugs used in the treatment of mood disorders (MDD and BD) in women of childbearing age, experts have recommended the following, as first-line (Fig. 2):
-
To establish if a contraceptive method is being used
-
To provide comprehensive information to the patient and—if the patient agrees—to the partner about the teratogenic and neurodevelopmental risks associated with psychotropic medications in case of pregnancy
-
To provide comprehensive information to the patient and—if the patient agrees—to the partner on the importance of planning a pregnancy in order to anticipate possible adaptations of the current treatment and define the most suitable care strategies
-
To ensure regular reassessment of the prescribed treatment
These steps should be followed repeatedly every 12 months minimum to 36 months maximum.
For psychotropic drugs with intermediate teratogenic risk, the above-mentioned recommendations should be repeated every 12 months. In addition, experts have also recommended the following as first-line strategies:
-
To take a pregnancy test before initiation of drug
-
To provide a patient guide booklet for every prescribed drug
For psychotropic drugs with high teratogenic risk, the above-mentioned recommendations should be repeated every 6 to 12 months. In addition, experts recommended the following as first-line strategy:
-
To have an informed consent for medication completed and signed by the patient
Preconception care
Information and advice to share
Experts recommended to provide information and advice about the following:
-
The risk of relapse(s), the suicidal risk during the perinatal period, and how to prevent them (follow-up, monitoring, treatment)
-
The risks associated with addictive behaviors, strategies for their prevention, and the benefits of abstinence in case of addictive comorbidities
-
The desired period of euthymia of at least 6 months before pregnancy to reduce the risk of relapse
-
The option to breastfeed and the putative effects of psychotropic drugs during breastfeeding
-
The diet and lifestyle rules (regarding sleep, physical activities, etc.) that have a positive impact on mental health
-
If and when possible, the involvement of the partner in the planned pregnancy and in decisions concerning the care of the patient and the future baby
Experts also recommended providing information and advice for women with BD about the following:
-
The genetic liability to develop mood disorders
Relevant clinical characteristics of mood disorder for guidance on therapeutic strategies in advance of a planned pregnancy
The relevant characteristics of MDD for guidance on therapeutic strategies in advance of a planned pregnancy were as follows:
-
Residual depressive symptoms
-
Comorbid premenstrual dysphoric disorder
-
History of severe major depressive episode or major depressive episode with peripartum onset
-
History of suicide attempts
-
Comorbid anxiety disorder
-
Adherence to treatment
-
Patient preference
-
Family history of mood episode with peripartum onset and/or BD
The relevant characteristics of BD for guidance on therapeutic strategies in advance of a planned pregnancy, in addition to the above-mentioned characteristics, were as follows:
-
Type of BD
-
Predominant polarity of BD
-
Presence of rapid cycling
Management of mood disorders during pregnancy
Screening
In pregnant women without an established diagnosis of a mood disorder (MDD and BD), it is recommended to systematically search or check for certain signs or symptoms, namely:
-
Suicidal ideation and suicidal risk
-
Depressive and manic symptoms
-
Anxiety disorders
-
Substance use disorders and withdrawal symptoms
If a mood disorder is suspected, the following combined actions are recommended as first-line strategy:
-
To consult a psychiatrist practicing in a perinatal department or maternity ward
-
To cooperate with the gynecologist or midwife in order to develop a monitoring schedule and treatment plan with the patient during pregnancy
-
To meet a social worker if vulnerability factors have been identified (i.e. isolation, precariousness)
Notably, consulting a general psychiatrist or a general practitioner is only recommended as a second-line strategy, i.e., when the above combined first-line actions are not available.
Rating strategies for the management of mood disorders according to the teratogenic risk of the treatment
In the acute phase, it is recommended to use the following:
-
As first-line (strategy of choice), an effective treatment (i.e., antidepressant in case of MDD or mood stabilizers in case of BD) without teratogenic risk whatever the pregnancy trimester.
-
As second-line, an effective treatment with intermediate teratogenic risk only during the second and third trimester.
-
In the case of BD, experts did not reach a consensus for the use or counter-indication of an effective mood stabilizer with intermediate teratogenic during the first trimester.
During the maintenance phase, in order to reduce the risk of a new mood episode, it is also recommended to use the following:
-
As first-line (strategy of choice), an effective treatment without teratogenic risk whatever the pregnancy trimester.
-
As second-line, an effective treatment with intermediate teratogenic risk only during the second and third trimester.
-
In case of BD, experts did not reach a consensus for the use or counter-indication of an effective mood stabilizer with intermediate teratogenic during the first trimester.
The use of a high-risk teratogenic treatment, whatever the clinical situation, including hospitalization, is counter-indicated during all pregnancy trimesters.
In pregnant women with BD, the use of a long-acting antipsychotic formulation is only recommended as second-line therapy, in case of poor adherence and frequent relapses.
Treatment options
During pregnancy, treatment options include continuing medication (with or without adjustment of the dose), switching to an alternative medication associated with lower teratogenic risk or, finally, discontinuing medication and reintroducing it either after the first trimester (e.g., in case of treatment with lithium to avoid cardiac malformation) or immediately after delivery.
In case of discontinuation of treatment before pregnancy, the expert panel recommends the reintroduction of an effective treatment in women with stabilized MDD if one of the following relevant characteristics is present:
-
Patient preference
-
Residual mood symptoms
-
History of severe mood episode
-
History of mood episode with peripartum onset
-
History of suicide attempts
-
Comorbid anxiety disorder
In case of discontinuation of treatment before pregnancy, the expert panel recommends the reintroduction of an effective treatment in women with stabilized BD if one of the following relevant characteristics is present:
-
Patient preference
-
Residual mood symptoms (depressive or manic symptoms)
-
History of severe mood episode
-
History of mood episode with peripartum onset
-
History of suicide attempts
-
Comorbid anxiety disorder
-
Rapid cycling
-
Family history of mood episode with peripartum onset
Experts recommend the use of electroconvulsive therapy in some clinical situations in women with mood disorder during pregnancy:
-
As first-line treatment:
-
Presence of mood episode with catatonic features
-
Previous relapse after discontinuation of electroconvulsive therapy during consolidation or maintenance phases
-
Treatment-resistant depression and treatment-resistant mania (no response to adequate trials of medication)
-
Patient preference
-
Previous positive response to electroconvulsive therapy, but only during the second and third trimester in this specific case
-
As second-line treatment:
-
Presence of mood episode with psychotic features
-
Presence of major depressive episode with melancholic features
-
Presence of a high suicide risk
-
As an alternative therapeutic option to medications with intermediate or high teratogenic risk
Treatment monitoring and follow-up
Maternal physiological changes during pregnancy may require dosing adjustments. The second and early third trimester may require higher or lower doses due to changes in hepatic metabolism, renal clearance, and plasma volume. Conversely, during the weeks before delivery, lower doses could be safer for the newborn.
Therefore, experts also recommend as a first-line strategy to closely monitor women during pregnancy through regular testing of plasma levels of routinely tested psychotropic medications (i.e., lithium, lamotrigine, antidepressants) and to aim towards the minimum effective dose.
Regarding the follow-up and management of women with stabilized mood disorder (MDD and BD) during pregnancy, the experts recommend the following as first-line strategies:
-
To consult a psychiatrist practicing in a perinatal service or a maternity hospital or to continue the follow-up with their psychiatrist with a high frequency (at least once a month) and adapt to the evolution of the patient’s clinical condition
-
To carry out an antenatal consultation with a pediatrician of the maternity hospital
-
To plan a specialized obstetrical follow-up and delivery in a specialized center with permanent pediatric support
-
To prepare a crisis plan involving the patient (discussion of episode-precipitating factors and development of strategies for preventing new episodes)
Management of mood disorders during the post-partum period
Screening
According to the experts, the recommendations established for patients during pregnancy apply similarly for the postpartum period in women without an established diagnosis of a mood disorder or in case of suspected mood disorder (see “Rating strategies for the management of mood disorders in women of childbearing age according to the teratogenic risk of the treatment” section).
Information about breastfeeding
The current recommendation from the WHO clearly favors exclusive breastfeeding for the first 6 months of an infant’s life, while from the age of 6 months and until the age of 2 years children should be eating safe and adequate complementary foods in addition to breastfeeding (WHO 2023). However, for mothers with mood disorders during post-partum, the benefits of breastfeeding should be balanced with the potential risk of the infant being exposed to medication.
Therefore, experts recommend the following as first-line strategies:
-
To provide comprehensive information to the patient and the partner (if the patient agrees) on the risk associated to the exposure to psychotropic medications during lactation and, since most psychotropic medications pass into breastmilk to some extent, to inform for each medication on expected levels in breastmilk, as well as potential adverse effects in breastfed infants.
-
To provide comprehensive information from a pediatrician in the maternity hospital on the benefits and risks of breastfeeding.
-
If breastfeeding is desired, the following information should be provided:
-
The use of a breast pump and the implementation of a feeding schedule shared with one’s partner promote mood stability.
-
To the extent possible, it is preferable to take the medication immediately after a breastfeed and just before a prolonged period of sleep.
-
If formula feeding is desired, the practitioner should support this choice and provide information about the benefit of sharing night feeds with the partner in order to reduce the risk of sleep disruption.
If breastfeeding is chosen, the experts recommend, as a second-line strategy, to monitor the drug levels in breastmilk, if possible.
Rating strategies for the management of mood disorders according to the lactation risk category of the treatment
For women with mood disorder (MDD and BD) in both the acute and the maintenance phase, the experts recommend the following:
-
As first-line (strategy of choice), an effective medication without evidence of adverse effects in nursing infants (L1-L2 Hale’s lactation risk categories of medications, (Hale and Krutsch 2023)
The use of medications with evidence of risk to a nursing infant (L4-L5 Hale’s lactation risk categories of medications) is counter-indicated whatever the clinical situation, including during hospitalization.
No consensus has been reached regarding the use of a medication with mild, non-threatening adverse effects or for which there are no breastfeeding studies (L3 Hale’s lactation risk categories of medications).
Discussion
To the best of our knowledge, we developed here the first consensus-based guidelines for the management of mood disorders (MDD and BD) in women of childbearing age, before pregnancy, during pregnancy, and at post-partum. Women’s mental health is an important issue and its management can be challenging especially at peripartum. While there is a limited amount of evidence-based treatment recommendations for this specific population and at these critical periods, we content that consensus-based guidelines may significantly improve our current knowledge and clinical practice. The painful experience of patients using valproate and other anticonvulsants during pregnancy highlighted the need of guidelines, among other actions, to avoid such dramatic outcomes.
Importantly, experts recommend to treat mood symptoms during pregnancy and to maintain a pharmacological treatment, even in euthymic or stabilized patients. The goal is to counteract the high risk of relapse during pregnancy and post-partum. Relapse can have dramatic consequences, including worse disease prognosis and maternal suicide, alteration of the mother-infant relationship, modification of the behavior of the baby, and familial disturbance (Gressier et al. 2020). Experts’ recommendations define clinical characteristics that help clinicians to decide about treatment maintenance/re-introduction during pregnancy.
However, it is worth noting that first-line options in our recommendations are “conservative” with priority given to safety, even when the literature suggests better safety than expected. For example, the use of electroconvulsive therapy is limited to specific and very severe clinical situations. In contrast, in general clinical practice, it is recommended as a first-line treatment when rapid clinical improvement is required, but also when patient preference is reported or when previous response to ECT is documented (Samalin et al. 2020). In the meanwhile, in the current literature, electroconvulsive therapy is considered safe during pregnancy whatever the trimester (Ward et al. 2018). The case of lithium is also a matter of debate. Lithium could be considered the gold standard of pharmacological treatment for BD (Yatham et al. 2018). Recent publications suggest also a better safety than expected when using during pregnancy, specially at a lower dosage (< 600 mg per day) (Fornaro et al. 2020). Yet international guidelines are contradictory about lithium maintenance during pregnancy (Belzeaux et al. 2019). Some guidelines suggest to maintain lithium while some others advise to stop it, at least during the first trimester, independently of the risk associated with tapering (Yathman et al. 2018; Malhi et al. 2021; Goodwin et al. 2016; Fountoulakis et al. 2017). However, lithium tapering should be done very carefully and in the course of several months due to its high association with relapse and worse prognosis the first year after discontinuation. To date, lithium should be considered an intermediate teratogenic risk drug and it is not recommended as a first-line strategy in women of childbearing age and during pregnancy according to the guidelines presented here. On the other hand, our recommendations do not counter-indicate lithium in these patients. This means that a therapeutic decision based on patient’s preference and risk/benefit balance could lead to lithium prescription and even more importantly maintenance, including during the first trimester of pregnancy. Similarly, if breastfeeding is chosen, it is recommended to prescribe only medication without evidence of adverse effects in nursing infants, while some data suggests that the use of other treatments, including lithium, is possible with appropriate monitoring (Pacchiarotti et al. 2016).
Beyond the use of lithium in women of childbearing age and during pregnancy, similar concerns persist for all medications. Antipsychotics are widely used during pregnancy and are known to this date to have no or low teratogenic risks. This level of risk may change based on future studies or new signal from pharmacovigilance (i.e., risperidone) (Huybrechts et al. 2016). The prescriptions should be based on updated information regarding these risks.
These treatment guidelines have some limitations. First of all, we made the choice to classify treatment according to their teratogenic risk. This classification may be debatable as it does not take into account possible neurodevelopmental abnormalities associated with treatment exposure and overall tolerance of neonates.
Moreover, this classification may lead to low specificity of the information and further drug-by-drug recommendations could be considered useful. However, our classification ensures these guidelines remain applicable even as new evidence about drug-related risk emerges in the near future.
Finally, these recommendations are not exhaustive. The pharmacological treatment recommendations are only one component of the treatment choice, which also encompasses the patient’s preferences, the clinician’s personal knowledge and experience, and the family or social context in which the prescription is proposed.
In conclusion, these consensus-based guidelines allow to bridge the available empirical literature and clinical practice. They are developed based on a pragmatic approach and understanding of the “real world” of clinical practice, based on the experience of prescribers specialized in mood disorders and perinatal psychiatry. Our recommendations will help facilitate treatment decisions for clinicians involved in the daily assessment and management of mood disorders in women of childbearing age, including during pregnancy and post-partum.
Data availability
All data and materials as well as software application or custom code support the published claims and comply with field standards.
References
Belzeaux R, Sanguinetti C, Murru A, Verdolini N, Pacchiarotti I, Hidalgo-Mazzei D, Cohen L, Anmella G, Barbuti M, Vieta E, Llorca PM, Samalin L (2019) Pharmacotherapy for the peripartum management of bipolar disorder. Expert Opin Pharmacother 20(14):1731–1741. https://doi.org/10.1080/14656566.2019.1626826
Bennabi D, Yrondi A, Charpeaud T et al (2019) Clinical guidelines for the management of depression with specific comorbid psychiatric conditions French recommendations from experts (the French Association for Biological Psychiatry and Neuropsychopharmacology and the fondation FondaMental). BMC Psychiatry 19(1):1–9. https://doi.org/10.1186/s12888-019-2025-7
CRAT (2023) Le Centre de Référence sur les Agents Tératogènes. https://www.le-crat.fr/. Accessed 28 July 2023
Elefant E, Vauzelle C, Beghin D (2014) Centre de référence sur les agents tératogènes (CRAT): a pioneer center. Therapie 69:39–45. https://doi.org/10.2515/therapie/2014004
Fornaro M, Maritan E, Ferranti R, Zaninotto L, Miola A, Anastasia A, Murru A, Solé E, Stubbs B, Carvalho AF, Serretti A, Vieta E, Fusar-Poli P, McGuire P, Young AH, Dazzan P, Vigod SN, Correll CU, Solmi M (2020) Lithium exposure during pregnancy and the postpartum period: a systematic review and meta-analysis of safety and efficacy outcomes. Am J Psychiatry 177(1):76–92. https://doi.org/10.1176/appi.ajp.2019.19030228
Fountoulakis KN, Grunze H, Vieta E et al (2017) The International College of Neuro-Psychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 3: the clinical guidelines. Int J Neuropsychopharmacol 20(2):180–195. https://doi.org/10.1093/ijnp/pyw109
Goodwin GM, Haddad PM, Ferrier IN et al (2016) Evidence-based guidelines for treating bipolar disorder: revised third edition recommendations from the British Association for Psychopharmacology. J Psychopharmacol 30(6):495–553 https://doi.org/10.1177/0269881116636545
Gressier F, Letranchant A, Glatigny-Dallay E, Falissard B, Sutter-Dallay AL (2020) Negative impact of maternal antenatal depressive symptoms on neonate’s behavioral characteristics. Eur Child Adolesc Psychiatry 29(4):515–526. https://doi.org/10.1007/s00787-019-01367-9
Grunze H, Vieta E, Goodwin GM et al (2013) The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2012 on the long-term treatment of bipolar disorder. World J Biol Psychiatry 14(3):154–219. https://doi.org/10.3109/15622975.2013.770551
Huybrechts KF, Hernández-Díaz S, Patorno E, Desai RJ, Mogun H, Dejene SZ, Cohen JM, Panchaud A, Cohen L, Bateman BT (2016) Antipsychotic use in pregnancy and the risk for congenital malformations. JAMA Psychiat 73(9):938–946. https://doi.org/10.1001/jamapsychiatry.2016.1520
Kessler RC, Chiu WT, Demler O, Walters EE (2005) Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry 62(6):617–627. https://doi.org/10.1001/archpsyc.62.6.617
Llorca PM, Courtet P, Martin P, Abbar M, Gay C, Meynard JA, Baylé F, Hamon M, Lançon C, Thibaut F, Thomas P, Lancrenon S, Guillaume S, Samalin L (2010) Screening and management of bipolar disorders: methodology. Encephale 36(Suppl 4):S79-85. https://doi.org/10.1016/s0013-7006(10)70036-1
MacQueen GM, Frey BN, Ismail Z, Jaworska N, Steiner M, Lieshout RJ, Kennedy SH, Lam RW, Milev RV, Parikh SV, Ravindran AV; CANMAT Depression Work Group (2016) Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 6. special populations: youth, women, and the elderly. Can J Psychiatry 61(9):588–603. https://doi.org/10.1177/0706743716659276
Malhi GS, Bell E, Bassett D, Boyce P, Bryant R, Hazell P, Hopwood M, Lyndon B, Mulder R, Porter R, Singh AB, Murray G (2021) The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry 55(1):7–117. https://doi.org/10.1177/0004867420979353
Pacchiarotti I, León-Caballero J, Murru A, Verdolini N, Furio MA, Pancheri C, Valentí M, Samalin L, Roigé ES, González-Pinto A, Montes JM, Benabarre A, Crespo JM, de Dios PC, Goikolea JM, Gutiérrez-Rojas L, Carvalho AF, Vieta E (2016) Mood stabilizers and antipsychotics during breastfeeding: focus on bipolar disorder. Eur Neuropsychopharmacol 26(10):1562–1578. https://doi.org/10.1016/j.euroneuro.2016.08.008
Power RA, Kyaga S, Uher R, MacCabe JH, Långström N, Landen M, McGuffin P, Lewis CM, Lichtenstein P, Svensson AC (2013) Fecundity of patients with schizophrenia, autism, bipolar disorder, depression, anorexia nervosa, or substance abuse vs their unaffected siblings. JAMA Psychiat 70(1):22–30. https://doi.org/10.1001/jamapsychiatry.2013.268
Samalin L, Yrondi A, Charpeaud T, Genty JB, Blanc O, Sauvaget A, Stéphan F, Walter M, Bennabi D, Bulteau S, Haesebaert F, D’Amato T, Poulet E, Holtzmann J, Richieri RM, Attal J, Nieto I, El-Hage W, Bellivier F, Schmitt L, Lançon C, Bougerol T, Leboyer M, Aouizerate B, Haffen E, Courtet P, Llorca PM (202AD) Adherence to treatment guidelines in clinical practice for using electroconvulsive therapy in major depressive episode. J Affect Disord 1(264):318–323. https://doi.org/10.1016/j.jad.2020.01.004
Samalin L, Godin O, Olié E, Etain B, Henry C, Pelletier A, Poinso F, Encely L, Mazer N, Roux P, Loftus J, Gard S, Bennabi D, Polosan M, Schwitzer T, Aubin V, Schwan R, Passerieux C, Bougerol T, Dubertret C, Aouizerate B, Haffen E, Courtet P, Bellivier F, Leboyer M, FACE-BD collaborators, Llorca PM, Belzeaux R (2020) Evolution and characteristics of the use of valproate in women of childbearing age with bipolar disorder: Results from the FACE-BD cohort. J Affect Disord 276:963–969. https://doi.org/10.1016/j.jad.2020.07.078
Stevens AWMM, Goossens PJJ, Knoppert-van der Klein EAM, Draisma S, Honig A, Kupka RW (2019) Risk of recurrence of mood disorders during pregnancy and the impact of medication: a systematic review. J Affect Disord 249:96–103. https://doi.org/10.1016/j.jad.2019.02.018
Sutter-Dallay AL, Bales M, Pambrun E, Glangeaud-Freudenthal NM, Wisner KL, Verdoux H (2015) Impact of prenatal exposure to psychotropic drugs on neonatal outcome in infants of mothers with serious psychiatric illnesses. J Clin Psychiatry 76(7):967–973. https://doi.org/10.4088/JCP.14m09070
Ward HB, Fromson JA, Cooper JJ, De Oliveira G, Almeida M (2018) Recommendations for the use of ECT in pregnancy: literature review and proposed clinical protocol. Arch Womens Ment Health 21(6):715–722. https://doi.org/10.1007/s00737-018-0851-0
Wesseloo R, Kamperman AM, Munk-Olsen T, Pop VJ, Kushner SA, Bergink V (2016) Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry 173(2):117–127. https://doi.org/10.1176/appi.ajp.2015.15010124
Yatham LN, Kennedy SH, Parikh SV et al (2018) Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord 20(2):97–170. https://doi.org/10.1111/bdi.12609
Acknowledgements
The authors are grateful to the experts who completed the survey which had allowed the development of these recommendations.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Ludovic Samalin, Ludivine Boudieu, and Raoul Belzeaux. The first draft of the manuscript was written by Ludovic Samalin, Raoul Belzeaux, and Eleni Tzavara, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by an institutional independent national ethics committee (IRB 00013040) and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article (supplementary file).
Competing interests
Ludovic Samalin has received honoraria and served as a consultant for Janssen-Cilag, Lundbeck, Otsuka, Rovi, and Sanofi-Aventis with no financial or other relationship relevant to the subject of this article.
Raoul Belzeaux has received honoraria and served as a consultant for Lundbeck, Otsuka, and Sanofi-Aventis with no financial or other relationship relevant to the subject of this article.
The other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to missing Supplementary Material.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1
(DOC 1.18 MB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Belzeaux, R., Gressier, F., Boudieu, L. et al. French Society for Biological Psychiatry and Neuropsychopharmacology and French-speaking Marcé Society guidelines for the management of mood disorders in women before, during, and after pregnancy. Arch Womens Ment Health 27, 595–605 (2024). https://doi.org/10.1007/s00737-024-01440-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-024-01440-6