Abstract
The COVID-19 pandemic heightened prenatal maternal stress, a risk factor for poorer maternal and infant health. There was substantial variability, however, in the extent to which the stress of pandemic pregnancy influenced maternal mental health. Some of this variability may have been due to the different coping strategies used to manage pandemic stress. In this cross-sectional study of 7,383 pregnant women in the U.S. (M = 25.69 ± 8.71 weeks gestational age) recruited during the first and second U.S. waves of the COVID-19 pandemic, we examined associations of objective stressors, the subjective experience of stress, and the use of four coping strategies with anxiety and depressive symptoms. Spiritual coping, planning/preparation, and avoidant coping were associated with increased subjective and objective stress and with greater mood and anxiety symptoms, whereas coping by positive appraisal was associated with modestly lower subjective stress and with lower mood and anxiety symptoms. We also found small interactions of stress and coping in predicting mood and anxiety symptoms, suggesting that fit between coping strategy and type of stress influences coping outcomes. Specific coping strategy used as well as the fit between coping strategy and stress type may determine whether coping buffers or exacerbates mood and anxiety symptoms. The small magnitude of these associations suggests that individual-level coping may be insufficient in the face of the overwhelming nature of the stress accompanying a global pandemic. This work adds to our understanding of coping with pregnancy stress in the context of population-level stressors (i.e., a pandemic or large-scale disaster).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elevated stress during pregnancy is associated with worse maternal mental and physical health (Biaggi et al. 2016; Ibrahim and Lobel 2020), which may in turn have long-term effects on child health and development (Adamson et al. 2018; Gentile 2017). The COVID-19 pandemic contributed to stress for pregnant women via increased social isolation, financial strain, limited prenatal care access, and infection risk (Barbosa-Leiker et al. 2021; Matvienko-Sikar et al. 2021; Meaney et al. 2021). Women pregnant during the pandemic also reported high levels pregnancy-specific stress (e.g., caring for a child, physical toll of pregnancy/childbirth) and pandemic-specific stress (e.g., infection risk and not feeling prepared for childbirth; Pope et al. 2021; Preis et al. 2020b). High rates of prenatal depression and anxiety have been reported in some studies yet prevalence rates differ widely (Tomfohr-Madsen et al. 2021; Yan et al. 2020). There has also been significant heterogeneity in the observed effects of stress on maternal mental health outcomes (for reviews, see Demissie and Bitew 2021; Fan et al. 2021; Sun et al. 2021). One possible explanation for these findings is that interindividual differences in stress coping may moderate the effect of stressful pandemic conditions on maternal mental health outcomes.
Coping with stress in pregnancy
Coping strategies are cognitive or behavioral responses used to manage stress, but not all strategies are equally effective. Studies of coping in the context of pregnancy-specific stress have commonly examined positive appraisal, planning/preparation, spiritual coping, and avoidance-based coping (Ibrahim et al. 2019; Rehbein et al. under review). Avoidant coping is consistently linked with higher distress (Giurgescu et al. 2006; Guardino and Dunkel Schetter 2014; Hamilton and Lobel 2008), while positive appraisal is linked to lower distress (Giurgescu et al. 2006; Guardino and Dunkel Schetter 2014; Ibrahim et al. 2019). Evidence concerning the efficacy of planning/preparation and spiritual coping is mixed (Dolatian et al. 2017; Lobel et al. 2002; Vitorino et al. 2018). Lobel and colleagues (2002) suggest that spiritual coping may reduce stress when it involves gratitude, mindfulness, or social support, but may be harmful when it involves perseveration on feared outcomes.
The utility of coping strategies may also depend on strategy-situation fit (Cheng et al. 2014; Shing et al. 2016). Effective coping is a tailored response to a specific stressor, and the importance of strategy-situation fit is emphasized by transactional theories of coping (Frydenberg 2014). For example, research examining prenatal coping in the context of the 2011 Queensland, Australia floods found that planning/preparation was associated with greater distress specifically for women with high levels of disaster exposure (Chen et al. 2020). Similarly, planning/preparation did not predict lower distress in a study of women with high-risk pregnancies (Lobel et al. 2002), suggesting that efforts to cope through problem-solving are ineffective or even increase distress when the stressor cannot be easily resolved by the individual.
Coping with prenatal stress during the COVID-19 pandemic
During the COVID-19 pandemic, high reliance on maladaptive coping strategies, including avoidance and poor self-care, has been documented in pregnant women (Werchan et al. 2022). Avoidant coping appears particularly common in women experiencing objective pandemic-related stress—that is, circumstances widely considered stressful such as financial loss and social isolation (Khoury et al. 2021). Avoidance has also been associated with worse mental health during the pandemic while planning/preparation and positive appraisal have been linked with better mental health (Khoury et al. 2021; Penengo et al. 2021; Spinola et al. 2020). The effects of spiritual coping during the pandemic appear mixed with some work suggesting it was generally deleterious (Penengo et al. 2021) and other work suggesting it may only have benefitted certain demographic groups such as African American women (Wheeler et al. 2021). Exploration of multivariate relationships of coping and stress are limited. Khoury and colleagues (2021) found that dysfunctional coping involving avoidance or maladaptive emotion regulation partially mediated the relationship between COVID-19 stress and mental health. Dysfunctional coping was associated with greater stress and worse mental health while emotion-focused coping was associated with lower stress and better mental health.
Despite growing research on stress and coping during pandemic pregnancy, important questions remain. First, whether coping functions as a moderator, rather than a mediator, of the relationship between stress and mental health outcomes has not been explored. That is, stress may predict poor mental health only when pregnant women use maladaptive coping strategies; adaptive coping may mitigate the deleterious impact of stress on mental health. Second, prior studies have largely focused on coping with perceived stress (c.f., Khoury et al. 2021). Effective coping, however, may look different for subjective versus objective stress. Third, because coping's effectiveness depends on strategy-situation fit, it is important to examine the efficacy of coping strategies as stressful pandemic conditions evolved over time.
The current study
We studied associations among stress, coping, and mood and anxiety symptoms in a large sample of pregnant women during the first two waves of the COVID-19 pandemic in the US. We hypothesized that avoidant coping would be linked to more mood and anxiety symptoms and positive appraisal would be linked to less mood and anxiety symptoms. We did not advance hypotheses about spiritual coping and planning/preparation, which have produced mixed results in previous studies. We explored the moderating impact of coping on the connection between stress and mood and anxiety symptoms using two distinct models for objective and subjective stress. We adjusted for sociodemographic and obstetric variables as well as other coping styles. We added wave of recruitment (Wave 1 vs. Wave 2) as a covariate to consider the evolving nature of the pandemic. Moreover, we performed exploratory analyses to determine whether the fit between coping strategy and pandemic circumstances changed throughout the pandemic.
Method
Study design
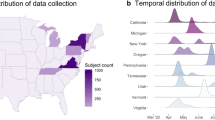
This cross-sectional study examined response data from the baseline surveys of a large longitudinal study, the Stony Brook COVID-19 Pregnancy Experiences (SB-COPE) Study, assessing psychosocial impacts of the COVID-19 pandemic on peripartum women and their offspring. We recruited pregnant women, 18 years or older, who could read in English, through targeted advertisement and pregnancy-related pages on social media sites (e.g., Facebook, Instagram, Reddit). Recruitment occurred in two waves corresponding to the first two waves of the COVID-19 pandemic in the U.S. (Wave 1: N = 4,388 women, April–May, 2020; Wave 2: N = 2,995 women, December, 2020). The cross-sectional analyses included data from baseline surveys of both waves of recruitment (total N = 7,383). Informed consent was obtained and participants completed surveys through Qualtrics. Participants were enrolled in a raffle with a 1/100 chance to win a $100 gift card for each questionnaire completed. The study has been continuously approved since April 21, 2020 by the IRB of Stony Brook University (IRB2020-00227).
Measures
Sociodemographic and Obstetric Factors included as covariates were variables that had previously been associated with mental health in studies of pregnant women during the pandemic (Lobel et al. 2022) and were significantly correlated in this sample with mood and anxiety symptoms. Specifically: maternal age (years), parity (number of births), and high-risk pregnancy status (No/Yes or Unsure). Additionally, we operationalized race as Black/African American versus all other racial groups based on previous literature suggesting that certain coping strategies, such as religious/spiritual coping, function differently among Black/African American vs non-Black individuals (Oates and Goode 2013; Wheeler et al. 2021).
Coping was measured using 14 items from the Revised Prenatal Coping Inventory (NuPCI; Hamilton and Lobel 2008) assessing the frequency of coping over the past month on a 5-point scale ranging from 0 (“Never”) to 4 (“Very Often”). Items assessed 4 different coping strategies (Ibrahim et al. 2019): spiritual coping (3 items, e.g., “Prayed that the birth will go well”), positive appraisal (3 items, e.g.,“ Felt that pregnancy has made life better”), planning/preparation (6 items, e.g.,“ Talked to people about what it is like to raise a child”), and avoidant coping (2 items, e.g.,“ Tried not to think about the birth”). The adapted NuPCI demonstrated mixed internal consistency across subscales (α’s range from 0.57 for avoidant coping to 0.85 for spiritual coping). Factor structure of this version of the NuPCI was assessed using confirmatory factor analysis (CFA; Supplemental Fig. 1).
Subjective Stress was measured using the Revised Prenatal Distress Questionnaire (NuPDQ; Ibrahim and Lobel 2020; Yali and Lobel 1999), and the Pandemic-Related Pregnancy Stress Scale (PREPS; Preis, Mahaffey, & Lobel 2020a, b). The NuPDQ is a 17-item measure assessing whether a respondent is feeling “bothered, upset, or worried” about each stressor (e.g., “changes in weight and body”, “what will happen during labor and delivery”) on a 3-point scale from 0 (“Not at All”) to 2 (“Very Much”). The NuPDQ has strong psychometric properties (Ibrahim and Lobel 2020), including in the current sample (α = 0.81). The PREPS assesses stress related to being pregnant during the COVID-19 pandemic and includes two subscales: 1) preparedness stress (7 items, e.g., “I am concerned that I am not getting enough healthy food or sleep or exercise because of COVID-19 restrictions”) and 2) infection stress (5 items, e.g., “I am worried that I might get COVID-19 when I go to the hospital to deliver”). Responses are on a 5-point scale from 1 (“Very Little”) to 5 (“Very Much”). The PREPS subscales have strong psychometric properties (Preis et al. 2020b) including internal consistency in the current sample (α’s = 0.82 for preparedness stress and 0.85 for infection stress). Z-scores of the NUPDQ and PREPS subscale scores were averaged to create a composite variable of subjective stress.
Objective Stress was measured as a sum of the following variables (range = 0–5): 1) essential worker status (Y/N), 2) “income loss for oneself or for someone on whom the participant depends due to COVID-19” (Y/N), 3) prenatal care appointments cancelled due to pandemic (Y/N), 4) diagnosed or suspected COVID-19 infection (Y/N), and 5) major stressful life event during pregnancy (Y/N). Both diagnosed and suspected cases of COVID-19 infection were included because at the first wave of recruitment (April–May, 2020), COVID-19 testing was not widely available. Among those with diagnosis of COVID-19 infection, n = 24 individuals endorsed being hospitalized as a result.
Mood and Anxiety Symptoms included frequency over the last two weeks of anxiety symptoms as reported on the Generalized Anxiety Disorder-7-item (GAD-7; Spitzer et al. 2006) and depressive symptoms as reported on the Patient Health Questionnaire-2-item (PHQ-2; Kroenke et al. 2003), using a 4-point response scale from 0 (“Not at All”) to 3 (“Nearly Every Day”). The GAD-7 and PHQ-9 are widely used screening measures and have strong psychometric properties (Byrd-Bredbenner et al. 2021; Staples et al. 2019), including in the current sample (GAD-7 α = 0.92; PHQ-2 α = 0.85). Z-scores of these measures were averaged to create a composite variable of mood and anxiety symptoms.
Data analytic plan
Analyses were conducted using SPSS version 28.0 (IBM Corp 2021) and R using the Lavaan package (R Core Team, 2021; Rosseel 2012). Depression and anxiety were highly correlated (r = 0.70, p < 0.001), as were measures of subjective stress (r’s range from 0.41-0.59, p’s < 0.001). Chi-squared and independent samples t-tests were used to compare group means of the Wave 1 and Wave 2 samples on sociodemographic, obstetric, stress, coping, and mood and anxiety variables. Next, collapsing across waves of recruitment, within-subjects ANOVA was used to compare mean levels of the four NuPCI coping strategies. Pearson’s correlations were used to examined bivariate associations among coping (NuPCI), objective stress, subjective stress, and mood and anxiety symptoms as measured using our composite measure of GAD-7 and PHQ-2. Finally, multiple regression was used to examine associations between mood and anxiety symptoms and coping strategies, type of stress, and the interaction of coping and stress factors (i.e., strategy-situation fit). Specifically, we examined two models (theoretical models in Fig. 1), one for objective stress and one for subjective stress, predicting mood and anxiety symptoms (using composite of GAD-7 and PHQ-2). Independent variables were wave of recruitment, sociodemographic and obstetric factors, coping strategies, stress (either subjective or objective), and the interaction of each coping strategy with stress.
Theoretical model of interactive effects of coping subtypes (i.e., spiritual coping, positive appraisal, planning/preparation, and avoidant coping) with stress (i.e., pandemic-related objective stress and pregnancy stress [composite of PREPS and NuPDQ z-scores]) to predict maternal mood and anxiety symptoms (composite of GAD-7 and PHQ-2 z-scores). Separate models were examined for each stress type
Results
7,383 women were recruited (Wave 1: N = 4,388 recruited April–May, 2020; Wave 2: N = 2,995 recruited December, 2020; see Table 1 for demographics). Both samples were majority white, although Wave 2 had fewer white participants (Χ2 = 18.48, p < 0.001) and more Black/African American participants (Χ2 = 24.37, p < 0.001). Both Wave 1 and Wave 2 samples were majority non-Hispanic (90.5% non-Hispanic in both waves of recruitment). Both waves of recruitment were also highly educated (69.0% bachelor’s degree or higher), with the Wave 2 sample reporting relatively higher educational attainment (Χ2 = 555.59, p < 0.001).
Collapsing across waves of recruitment, ANOVA with Greenhouse–Geisser correction for non-sphericity indicated significant differences in mean levels of the four coping strategies (F(2.6, 19188.86) = 2263.35, p < 0.001). Post-hoc pairwise comparisons indicated that positive appraisal (M = 2.42 ± 0.81) was used more than all other coping strategies (p’s < 0.001), and avoidant coping (M = 1.37 ± 0.88) was used less frequently than all other coping strategies (p’s < 0.001). Additionally, planning/preparation (M = 2.19 ± 0.79) was use more than spiritual coping (M = 1.58 ± 1.27, p < 0.001).
Spiritual coping, planning/preparation, and avoidant coping all exhibited small correlations with higher subjective and objective stress and mood and anxiety symptoms (see bivariate associations, Table 2). Positive appraisal also had a small correlation with lower subjective stress and mood and anxiety symptoms, but was not significantly related to objective stress. Objective stress had a small correlation with higher subjective stress and with higher mood and anxiety symptoms; subjective stress exhibited a large association with higher mood and anxiety symptoms.
In both linear regression models (Table 3), higher mood and anxiety symptoms were associated with being in the Wave 1 sample, being younger, higher parity, high-risk pregnancy status, and higher stress (either subjective or objective stress). Spiritual and avoidant coping predicted higher mood and anxiety symptoms in both stress models, while planning/preparation predicted higher mood and anxiety symptoms in the model for objective stress only. Positive appraisal predicted lower mood and anxiety symptoms in both models.
In addition to main effects, several modest interactions were found between coping strategies and stress in both models. Simple slopes of interactive associations are presented in Fig. 2. For both subjective and objective stress, the association between stress and mood and anxiety symptoms was weaker among women who used positive appraisal more frequently (Figs. 2a & 2d; β = -0.06, p < 0.001 and β = -0.03, p < 0.05, respectively). Additionally, women who used planning/preparation coping more experienced fewer mood and anxiety symptoms at low levels of subjective stress, but more symptoms at high levels of stress (Fig. 2b; β = 0.02, p < 0.05). By contrast, for the objective stress model, women who used planning/preparation coping more reported higher mood and anxiety symptoms at both low and high levels of objective stress, and the relationship between objective stress and mood and anxiety symptoms was stronger for women who used planning/preparation more (Fig. 2e; β = 0.04, p < 0.001). Finally, the interaction of avoidant coping with subjective stress was significantly associated with mood and anxiety symptoms. Specifically, among women who used avoidant coping more, the association between subjective stress and higher mood and anxiety symptoms was slightly stronger compared to women who used avoidant coping less (Fig. 2c; β = 0.03, p < 0.01). Additional exploratory hierarchical regression models were conducted, adding a second step to the current models in which we examined three-way interactions among coping, stress, and wave of recruitment. These analyses, presented in Table 3, did not reveal any significant three-way interactions.
Discussion
This study of a large cohort of American pregnant women examined associations of stress, coping, and their interactions with mood and anxiety symptoms during the COVID-19 pandemic. We separately examined associations with objective and subjective stress. We also included cross-sectional data from two samples, recruited respectively in the first and second U.S. waves of the COVID-19 pandemic, to provide a more nuanced understanding of coping with prenatal stress given evolving pandemic conditions. In the Wave 2 sample compared to Wave 1, use of spiritual coping and planning/preparation was modestly higher, and use of avoidant coping was modestly lower. By Wave 2, methods for protecting against the virus (e.g., masking, social distancing) were better understood and vaccines were on the horizon. Thus, decreasing uncertainty distress may have resulted in less reliance on avoidance and greater use of planning/preparation coping. This is consistent with hypothesized models of uncertainty distress regulation during the COVID-19 pandemic (Freeston et al. 2020) and consistent with the modestly lower levels of pandemic-related stress and mood and anxiety symptoms observed at Wave 2 versus Wave 1. These comparisons should be interpreted with caution, however, as the samples at each wave differed in education and racial identification.
Overall, positive appraisal was associated with lower mood and anxiety symptoms whereas avoidant coping was associated with higher mood and anxiety symptoms, consistent with the existing literature on coping in pregnancy (Ibrahim et al. 2019). The likely benefits of positive appraisal and costs of avoidance were also borne out by regression models examining interactions of coping with subjective and objective stress. Although we cannot determine causal relationships in this cross-sectional study, these results suggest that coping by positive appraisal may protect against mood and anxiety symptoms for both objective and subjective stress. Avoidance, by contrast, appears to be specifically detrimental for mental health in the context of high subjective stress.
In general, planning/preparation and spiritual coping were also both associated with higher mood and anxiety symptoms at the bivariate level. Multivariate analyses, however, may shed light on the mixed pattern of findings in prior studies of planning/preparation. Our findings here suggest that planning/preparation may be beneficial to mood and anxiety symptoms when a woman is experiencing low subjective stress but becomes detrimental when subjective stress is high. On the other hand, planning/preparation appeared to be universally deleterious to mental health in presence of objective stress, regardless of stress severity. We did not find any qualifications to the association of spiritual coping with mood and anxiety symptoms, suggesting that – at least during the pandemic – the effectiveness of spiritual coping may not have been affected by the nature of the stress.
The current results are consistent with previous work (Chen et al. 2020; Ibrahim et al. 2019; Khoury et al. 2021), but it should be noted that the associations of coping strategies with mental health variables were modest. This suggests that intervening on coping alone is not sufficient to alleviate distress for many women. Personal context (i.e., stress, mental health history) and social determinants of health should also be considered key targets for intervention (Endres et al. 2023; Guo et al. 2022; Lega et al. 2022; Preis et al. 2020a). The very small bivariate association of spiritual coping or planning/preparation with mood/anxiety symptoms may reflect that these two coping strategies vary in their efficacy across different circumstances and different sociocultural subgroups (for review, see Rehbein et al. under review). Further research is needed to better examine how cultural and situation factors influence the effectiveness of spiritual coping and planning/preparation in the face of major population-level stressors like the pandemic.
Although the present study makes strides towards disentangling the relationship between stress, coping, and mental health in women pregnant during the COVID-19 pandemic, there are several limitations to consider. Much research conducted during the pandemic, such as this, utilized online, self-selected samples recruited via social media. Such recruitment methods may increase risk for sampling bias (Singh and Sagar 2021). This limitation notwithstanding, remote survey administration reduces barriers to research participation for the perinatal population, a group that has historically been difficult to recruit for research (Frew et al. 2014) and was necessary given the abrupt onset of the pandemic and limitations on other face to face recruitment strategies. The self-report nature of our measures also meant that we did not include a formal clinical evaluation of current or lifetime psychopathology, limiting our ability to draw conclusions about changes in mental health functioning as a result of pandemic stress. The mental health screening measures utilized here also do not allow us to draw conclusions about the prevalence of psychological disorders in this sample. Relatedly, the present study is cross-sectional so inferences about causal impacts of coping on mental health are speculative. Within the objective stress composite, we included both SARS-COV-2 infection or suspected infection which may conflate a range of experiences. Due to the lack of reliable surveillance data in the US from early in the pandemic, we were also not able to account for regional variability in infection rates nor local pandemic mitigation policies, each of which may contribute to the variance in pregnancy stress. While we can speculate that increased understanding of SARS-CoV-2 from Wave 1 to Wave 2 may have decreased uncertainty, we did not directly assess these constructs.
The current study benefitted from a large, geographically diverse cohort. However, the sample was not racially, educationally, or economically representative of the US population. Sample demographic composition also varied between waves of recruitment, limiting our ability to separate sociodemographic and time/condition effects. Our research was also limited to examining these relationships in the US. Previous research suggests significant between-country differences in perinatal mental health during the pandemic (Mateus et al. 2022; Motrico et al. 2021). Finally, the present research was conducted in English and, despite efforts to recruit from areas with higher concentrations of minoritized individuals, the sample was majority white and highly educated. The relative efficacy of various coping strategies may differ for minoritized populations and for individuals from different cultural backgrounds (Garcini et al. 2022; Rehbein et al. under review). Similarly, it is likely that perinatal mood and anxiety symptoms differed across sociodemographic groups (Kovacheva et al. 2023). Further investigation is needed to better understand the relationships among stress, coping, and mental health within under-represented groups.
In sum, stress associated with the COVID-19 pandemic stress had modest yet sustained negative effects on mood and anxiety symptoms. Selection of coping strategy and strategy-situation fit may influence whether coping buffers or exacerbates mental health symptoms. The modest magnitude of these effects, however, suggests that an individual’s coping skills alone are not adequate to buffer the overwhelming stressful circumstances created by a global pandemic. Future research should examine geographic/national differences as well as differences among sociodemographic groups in the relationships between stress, coping, and perinatal mental health. Additionally, policy decisions should consider these national and sociodemographic differences in mental health needs when devising recommendations for effective intervention and coping strategies. Experts in infectious disease expect that epidemics/pandemics will increase in their intensity and frequency in the future (Marani et al. 2021). Therefore, it is critical that we learn how best to protect vulnerable populations, including pregnant women, from the adverse consequences of stress related to public health crises.
Data Availability
The data presented in the current manuscript is not available for public use.
References
Adamson B, Letourneau N, Lebel C (2018) Prenatal maternal anxiety and children’s brain structure and function: A systematic review of neuroimaging studies. J Affect Disord 241:117–126. https://doi.org/10.1016/j.jad.2018.08.029
Barbosa-Leiker C, Smith CL, Crespi EJ, Brooks O, Burduli E, Ranjo S, . . . Gartstein MA (2021) Stressors, coping, and resources needed during the covid-19 pandemic in a sample of perinatal women. BMC Pregnancy Childbirth 21(1):1–13. https://doi.org/10.1186/s12884-021-03665-0.
Biaggi A, Conroy S, Pawlby S, Pariante CM (2016) Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord 191:62–77. https://doi.org/10.1016/j.jad.2015.11.014
Byrd-Bredbenner C, Eck K, Quick V (2021) Gad-7, gad-2, and gad-mini: Psychometric properties and norms of university students in the united states. Gen Hosp Psychiatry 69:61–66. https://doi.org/10.1016/j.genhosppsych.2021.01.002
Chen T, Laplante D, Elgbeili G, Brunet A, Simcock G, Kildea S, King S (2020) Coping during pregnancy following exposure to a natural disaster: The qf2011 queensland flood study. J Affect Disord 273:341–349. https://doi.org/10.1016/j.jad.2020.03.165
Cheng C, Lau H-PB, Chan M-PS (2014) Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychol Bull 140(6):1582. https://doi.org/10.1037/a0037913
Demissie DB, Bitew ZW (2021) Mental health effect of covid-19 pandemic among women who are pregnant and/or lactating: A systematic review and meta-analysis. SAGE Open Med 9:20503121211026195. https://doi.org/10.1177/20503121211026195
Dolatian M, Mahmoodi Z, Dilgony T, Shams J, Zaeri F (2017) The structural model of spirituality and psychological well-being for pregnancy-specific stress. J Relig Health 56(6):2267–2275. https://doi.org/10.1007/s10943-017-0395-z
Endres K, Haigler K, Sbrilli M, Jasani S, Laurent H (2023) Social determinants of perinatal mental health during the covid-19 pandemic. General Hospital Psychiatry
Fan S, Guan J, Cao L, Wang M, Zhao H, Chen L, Yan L (2021) Psychological effects caused by covid-19 pandemic on pregnant women: A systematic review with meta-analysis. Asian J Psychiatr 56:102533. https://doi.org/10.1016/j.ajp.2020.102533
Freeston M, Tiplady A, Mawn L, Bottesi G, Thwaites S (2020) Towards a model of uncertainty distress in the context of coronavirus (covid-19). Cogn Behav Ther 13:e31
Frew PM, Saint-Victor DS, Isaacs MB, Kim S, Swamy GK, Sheffield JS, . . . Ault K (2014) Recruitment and retention of pregnant women into clinical research trials: an overview of challenges, facilitators, and best practices. Clin Infect Dis 59(suppl. 7):S400–S407
Frydenberg E (2014) Coping research: Historical background, links with emotion, and new research directions on adaptive processes. Aust J Psychol 66(2):82–92. https://doi.org/10.1111/ajpy.12051
Garcini LM, Rosenfeld J, Kneese G, Bondurant RG, Kanzler KE (2022) Dealing with distress from the covid-19 pandemic: Mental health stressors and coping strategies in vulnerable latinx communities. Health Soc Care Community 30(1):284–294
Gentile S (2017) Untreated depression during pregnancy: Short-and long-term effects in offspring. A systematic review. Neuroscience 342:154–166. https://doi.org/10.1016/j.neuroscience.2015.09.001
Giurgescu C, Penckofer S, Maurer MC, Bryant FB (2006) Impact of uncertainty, social support, and prenatal coping on the psychological well-being of high-risk pregnant women. Nurs Res 55(5):356–365. https://doi.org/10.1097/00006199-200609000-00008
Guardino CM, Dunkel Schetter C (2014) Coping during pregnancy: A systematic review and recommendations. Health Psychol Rev 8(1):70–94. https://doi.org/10.1080/17437199.2012.752659
Guo J, De Carli P, Lodder P, Bakermans-Kranenburg MJ, Riem MM (2022) Maternal mental health during the covid-19 lockdown in china, italy, and the netherlands: A cross-validation study. Psychol Med 52(15):3349–3359
Hamilton JG, Lobel M (2008) Types, patterns, and predictors of coping with stress during pregnancy: Examination of the revised prenatal coping inventory in a diverse sample. J Psychosom Obstet Gynecol 29(2):97–104. https://doi.org/10.1080/01674820701690624
IBM Corp (2021) IBM SPSS Statistics for Windows, Version 28.0. IBM Corp, Armonk, NY
Ibrahim SM, Lobel M (2020) Conceptualization, measurement, and effects of pregnancy-specific stress: Review of research using the original and revised prenatal distress questionnaire. J Behav Med 43(1):16–33. https://doi.org/10.1007/s10865-019-00068-7
Ibrahim SM, Nicoloro-SantaBarbara J, Auerbach MV, Rosenthal L, Kocis C, Busso CE, Lobel M (2019) Pregnancy-specific coping and changes in emotional distress from mid-to late pregnancy. J Reprod Infant Psychol 37(4):397–412. https://doi.org/10.1080/02646838.2019.1578871
Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A (2021) Coping strategies mediate the associations between covid-19 experiences and mental health outcomes in pregnancy. Arch Women Ment Health: 1–11. https://doi.org/10.1007/s00737-021-01135-2
Kovacheva K, Rodríguez-Muñoz MF, Gómez-Baya D, Domínguez-Salas S, Motrico E (2023) The socio-demographic profile associated with perinatal depression during the covid-19 era. BMC Public Health 23(1):786
Kroenke K, Spitzer RL, Williams JB (2003) The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical care 1:1284–92. https://doi.org/10.1097/01.MLR.0000093487.78664.3C
Lega I, Bramante A, Lauria L, Grussu P, Dubini V, Falcieri M, . . . Mignuoli AD (2022) The psychological impact of covid-19 among women accessing family care centers during pregnancy and the postnatal period in italy. Int J Environ Res Public Health 19(4):1983
Lobel M, Yali AM, Zhu W, DeVincent C, Meyer B (2002) Beneficial associations between optimistic disposition and emotional distress in high-risk pregnancy. Psychol Health 17(1):77–95. https://doi.org/10.1080/08870440290001548
Lobel M, Preis H, Mahaffey B, Schaal NK, Yirmiya K, Atzil S, . . . Colli C (2022) Common model of stress, anxiety, and depressive symptoms in pregnant women from seven high-income western countries at the covid-19 pandemic onset. Soc Sci Med 315:115499. https://doi.org/10.1016/j.socscimed.2022.115499
Marani M, Katul GG, Pan WK, Parolari AJ (2021) Intensity and frequency of extreme novel epidemics. Proc Natl Acad Sci 118(35):e2105482118. https://doi.org/10.1073/pnas.2105482118
Mateus V, Cruz S, Costa R, Mesquita A, Christoforou A, Wilson CA, . . . Dominguez-Salas S (2022) Rates of depressive and anxiety symptoms in the perinatal period during the covid-19 pandemic: Comparisons between countries and with pre-pandemic data. J Affect Disord 316:245–253
Matvienko-Sikar K, Pope J, Cremin A, Carr H, Leitao S, Olander EK, Meaney S (2021) Differences in levels of stress, social support, health behaviours, and stress-reduction strategies for women pregnant before and during the covid-19 pandemic, and based on phases of pandemic restrictions, in Ireland. Women Birth 34(5):447–454. https://doi.org/10.1016/j.wombi.2020.10.010
Meaney S, Leitao S, Olander EK, Pope J, Matvienko-Sikar K (2021) The impact of covid-19 on pregnant womens’ experiences and perceptions of antenatal maternity care, social support, and stress-reduction strategies. Women and Birth. https://doi.org/10.1016/j.wombi.2021.04.013
Motrico E, Bina R, Domínguez-Salas S, Mateus V, Contreras-García Y, Carrasco-Portiño M, . . . Dikmen-Yildiz P (2021) Impact of the covid-19 pandemic on perinatal mental health (riseup-ppd-covid-19): Protocol for an international prospective cohort study. BMC Public Health 21(1):1–11
Oates GL, Goode J (2013) Racial differences in effects of religiosity and mastery on psychological distress: Evidence from national longitudinal data. Society and Mental Health 3(1):40–58. https://doi.org/10.1177/215686931245593
Penengo C, Colli C, Cesco M, Croccia V, Degano M, Ferreghini A, . . . Sala A (2021) Stress, coping, and psychiatric symptoms in pregnant women in outpatient care during the 2021 second-wave covid-19 pandemic. Front Psychiatry 12. https://doi.org/10.3389/fpsyt.2021.775585
Pope J, Olander EK, Leitao S, Meaney S, Matvienko-Sikar K (2021) Prenatal stress, health, and health behaviours during the covid-19 pandemic: An international survey. Women Birth. https://doi.org/10.1016/j.wombi.2021.03.007
Preis H, Mahaffey B, Heiselman C, Lobel M (2020) Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM 2(3):100155. https://doi.org/10.1016/j.ajogmf.2020.100155
Preis H, Mahaffey B, Lobel M (2020b) Psychometric properties of the pandemic-related pregnancy stress scale (preps). J Psychosom Obstet Gynecol 41(3):191–197. https://doi.org/10.1080/0167482X.2020.1801625
R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Rehbein E, Moyer A, Lobel M (under review) Ways of coping with stress during pregnancy: Differences revealed through meta-analysis
Rosseel Y (2012) Lavaan: an R package for structural equation modeling. J Stat Softw 48(2):1–36. http://www.jstatsoft.org/v48/i02/
Shing EZ, Jayawickreme E, Waugh CE (2016) Contextual positive coping as a factor contributing to resilience after disasters. J Clin Psychol 72(12):1287–1306. https://doi.org/10.1002/jclp.22327
Singh S, Sagar R (2021) A critical look at online survey or questionnaire-based research studies during covid-19. Asian J Psychiatry 65:102850
Spinola O, Liotti M, Speranza AM, Tambelli R (2020) Effects of covid-19 epidemic lockdown on postpartum depressive symptoms in a sample of italian mothers. Front Psychiatry 11:1177. https://doi.org/10.3389/fpsyt.2020.589916
Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: The gad-7. Arch Intern Med 166(10):1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Staples LG, Dear BF, Gandy M, Fogliati V, Fogliati R, Karin E, Titov N (2019) Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The phq-2, gad-2, and k-6. Gen Hosp Psychiatry 56:13–18. https://doi.org/10.1016/j.genhosppsych.2018.11.003
Sun F, Zhu J, Tao H, Ma Y, Jin W (2021) A systematic review involving 11,187 participants evaluating the impact of covid-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynecol 42(2):91–99. https://doi.org/10.1080/0167482X.2020.1857360
Tomfohr-Madsen LM, Racine N, Giesbrecht GF, Lebel C, Madigan S (2021) Depression and anxiety in pregnancy during covid-19: A rapid review and meta-analysis. Psychiatry Res 300:113912. https://doi.org/10.1016/j.psychres.2021.113912
Vitorino LM, Chiaradia R, Low G, Cruz JP, Pargament KI, Lucchetti AL, Lucchetti G (2018) Association of spiritual/religious coping with depressive symptoms in high-and low-risk pregnant women. J Clin Nurs 27(3–4):e635–e642. https://doi.org/10.1111/jocn.14113
Werchan DM, Hendrix CL, Ablow JC, Amstadter AB, Austin AC, Babineau V, . . . Crowell SE (2022) Behavioral coping phenotypes and associated psychosocial outcomes of pregnant and postpartum women during the covid-19 pandemic. Sci Rep 12(1):1–12. https://doi.org/10.1038/s41598-022-05299-4
Wheeler JM, Misra DP, Giurgescu C (2021) Stress and coping among pregnant black women during the covid-19 pandemic. Public Health Nurs. https://doi.org/10.1111/phn.12909
Yali AM, Lobel M (1999) Coping and distress in pregnancy: An investigation of medically high risk women. J Psychosom Obstet Gynecol 20(1):39–52. https://doi.org/10.3109/01674829909075575
Yan H, Ding Y, Guo W (2020) Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: A systematic review and meta-analysis. Front Psychology 11:617001. https://doi.org/10.3389/fpsyg.2020.617001
Acknowledgements
This study was funded by a Stony Brook University Office of the Vice President for Research and Institute for Engineering-Driven Medicine COVID-19 Seed Grant and by the National Institutes of Health (NIH) Office of the Director Implementing a Maternal health and Pregnancy Outcomes Vision for Everyone (IMPROVE) Initiative (R21DA049827). During their work on this article, Brittain Mahaffey received support The National Institute of Child Health and Human Development (NICHD) K23HD092888. Amanda Levinson received support from a K12 institutional training grant though Stony Brook Medicine and The Long Island Network for Clinical and Translational Science (LINCATS). Finally, both Heidi Preis and Marci Lobel were supported by NIH Grant R21DA049827.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The parent study was conceived and data collected by Heidi Preis, Brittain Mahaffey and Marci Lobel. Material preparation and data analysis were performed by Amanda Levinson and Brittain Mahaffey. The first draft of the manuscript was written by Amanda Levinson and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial conflicts of interest to report.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Levinson, A., Lobel, M., Preis, H. et al. Coping with subjective and objective stress during a pandemic pregnancy: implications for maternal mental health. Arch Womens Ment Health 26, 819–829 (2023). https://doi.org/10.1007/s00737-023-01357-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-023-01357-6