Abstract
Postpartum depression (PPD) is characterized as a depressive episode conditional on childbirth. We examined whether the risk of depression is higher following childbirth than that at a randomly generated time unrelated to childbirth. In a prospective cohort of all women with live singleton births in Sweden, 1997–2008, we first calculated the relative risk (RR) of PPD for mothers with a history of depression compared to mothers without such a history. Next, we repeated the calculations, but now for depression following a computer-generated arbitrary “phantom delivery” date, unrelated to the true date of delivery. For this phantom delivery date, we used the average expected date of delivery for all women of the same age. For the analyses of each group, women were followed for a full calendar year. We fitted Poisson regression and calculated RR and two-sided 95% confidence intervals (CI). Among a total of 707,701 deliveries, there were 4397 PPD cases and 4687 control depression cases. The RR of PPD was 21.0 (CI 19.7–22.4). The RR of depression in the control group was 26.2 (CI 24.7–27.9). We provide evidence that the risk for PPD is no greater following childbirth than following a random date unrelated to childbirth. This finding suggests that the postpartum period may not necessarily represent a time of heightened vulnerability for clinically significant depression and that the well-established observation of depression covarying with childbirth does not necessarily equate to causation, but rather may be a secondary effect of postpartum women representing a medically captured population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postpartum depression (PPD) is often described as one of the most common nonobstetric complications associated with childbearing, reportedly affecting 9–13% of all new mothers (World Health Organization 1992; Gaynes et al. 2005; O’Hara and McCabe 2013). Characterized as a perinatal onset specifier of a unipolar major depressive disorder with the appearance of symptoms within the first four weeks according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5, American Psychiatric Association 2013) or six weeks according to the International Classification of Disease (ICD-10, World Health Organization 1992) after child delivery, PPD is unique among psychiatric disorders in that it is conditionally based on the timing of onset as opposed to having unique symptomatology. To date, scientific evidence supporting PPD as a distinct nosologic entity remains unavailable, and because the time surrounding birth represents a time of heightened stress and vulnerability for most, if not all, new mothers (Guardino and Schetter 2014), the clinical utility of a PPD specifier has recently been questioned (Di Florio and Meltzer-Brody 2015; Hoertel et al. 2015).
A review of the vast literature on PPD reveals that it is often arbitrarily defined, with the majority of studies confounding the distinction between major and minor depression (Gaynes et al. 2005). In fact, most PPD research to date has relied on symptom inventories, such as the widely used Edinburgh Postnatal Depression Scale (Cox et al. 1987), which not only are unable to differentiate between depressive symptomatology and the common discomforts associated with pregnancy and the perinatal period (Gjerdingen and Yawn 2007) but also may suffer from issues of diagnostic sensitivity and specificity (Cox 2017; Myers et al. 2013; Gibson et al. 2009). These screening tools when used independently of a clinical interview not only lack the clinical specificity required for diagnosis, leading to potentially ambiguous conclusions that are of limited use to patients, practitioners, clinical researchers, and epidemiologists, but are also prone to overestimating prevalence (Gaynes et al. 2005; Silverman et al. 2017; Thombs et al. 2018). Indeed, studies of depression relying on symptom screens generally show significantly increased prevalence rates compared to those relying on clinical diagnosis (Silverman et al. 2017; Rasmussen et al. 2017; Thombs et al. 2018).
Interestingly, despite the perinatal period regularly being reported as a time of heightened psychic vulnerability, prevalence studies exploring whether depressive episodes in the postpartum period are higher compared to those at other time points in a woman’s life remain indeterminate (Di Florio and Meltzer-Brody 2015; Wisner et al. 2013; Gavin et al. 2005; Bennett et al. 2004; O’Hara and Swain 1996; O’Hara et al. 1990; Cooper et al. 1988). This disparity may be due in part to the majority of studies relying on clinical rather than epidemiological samples. Epidemiological samples are population based, whereas clinical samples are from care-based clinics and referral centers, and inpatient samples involve patient series, which may not represent the entire population of women with PPD and are subject to varying diagnostic criteria. Only a handful of large-scale epidemiologic studies of PPD risk currently exist. These studies, which rely on nationally inclusive healthcare registries and clinical diagnoses, point not only to significantly lower prevalence rates but also to women with a history of depression as being at significantly greater risk for PPD (Räisänen et al. 2014; Silverman et al. 2017; Rasmussen et al. 2017).
Given the current characterization of unipolar major depression as an often recurrent disorder and epidemiologic research demonstrating that those with a depression history are at greatest risk for PPD (Räisänen et al. 2014; Silverman et al. 2017; Rasmussen et al. 2017), such findings suggest the possibility that depression after childbirth may simply represent the natural recurrence of a depressive episode. Indeed, the diagnostic criteria for a major depressive episode do not differ in the perinatal period as compared to other times (World Health Organization 1992; American Psychiatric Association 2013) and explorations attempting to determine if PPD differs characteristically from other unipolar depressive disorders have proven difficult, with the majority of studies demonstrating that the symptom profile of PPD is congruous with other unipolar depressive disorders that occur across the female lifespan (Howard et al. 2014; Di Florio and Meltzer-Brody 2015; Hoertel et al. 2015). More recent explorations into heritability and familial aggregation have also pointed to PPD as being associated with unipolar depression genetic etiologies nonspecific to childbirth (Forty et al. 2006; Corwin et al. 2010; Viktorin et al. 2015).
The purpose of this study was to empirically test the association between childbirth and depression. Notwithstanding the cited studies, there is a scarcity of analyses exploring the incidence of depression recurrence in the postpartum period in comparison to other times in a woman’s life, none of which are nationally inclusive, ascertain lifetime psychiatric history from clinical medical records, and few of which use clinical diagnoses of depression. Using the largest population-based sample to date, we compared the 12-month incidence of a PPD with the 12-month incidence of depression following a computer-generated, randomly chosen phantom delivery date unrelated to childbirth (see Maust et al. 2015). If the incidence of PPD was significantly higher than the incidence of depression following the random date, the postpartum period may indeed represent a time of heightened vulnerability for women at greatest risk. In contrast, a finding of a comparable incidence of PPD in comparison to the rate of depression observed in the control group will raise additional questions regarding the current characterization of PPD as the most common complication specific to childbirth.
Methods
Study population
Using the nationwide Swedish Medical Birth Register, which includes information on all births in Sweden, we identified a cohort comprising all Swedish-born women who delivered a live singleton infant between January 1, 1997, and December 31, 2008, and had a history of depression. To avoid problems with correlated data and given the power of the sample, we only included information from first births during the study period for each woman. Dates of inclusion were selected to conform to the implementation of the ICD-10th Revision (World Health Organization 1992) diagnostic system by the Swedish health system in 1997.
We defined depression history as a clinical diagnosis of depression any time prior to the delivery date using ICD-9 and ICD-10 codes. Since 1973, the nationwide Swedish National Patient Register has been prospectively capturing admission dates and clinical diagnoses for virtually all psychiatric hospitalizations. Since 2000, hospital outpatient care has been included in the registry as well. Data linkage between the Medical Birth Register and the Swedish National Patient Register was accomplished using the unique national identification number assigned to Swedish residents. The study protocol was approved by Mount Sinai School of Medicine’s Program for the Protection of Human Subjects, the Swedish National Board of Health and Welfare, and the Ethical Review Board at Karolinska Institutet, Stockholm.
Outcomes
Contemporary diagnostic nosology characterizes PPD as a specifier of a major depressive disorder (unipolar) with an onset of symptoms within four or six weeks after delivery (World Health Organization 1992; American Psychiatric Association 2013). However, consistent with prior research (Munk-Olsen et al. 2006; Savitz et al. 2011; Silverman et al. 2017; Rasmussen et al. 2017) and in agreement with recommendations from the Agency for Healthcare Research and Quality (Gaynes et al. 2005), we defined PPD as a depression diagnosis recorded in the medical register within 12 months following delivery. Depression diagnoses included diagnoses of postpartum depression, as well as major depressive disorder (single or recurrent), unspecified episodic mood disorder, or depressive disorder that occurred within the first year postpartum (Table 1). The additional diagnostic codes for unipolar depression reflect the range of classifications used by clinicians who diagnose depression.
Analytic approach; selection of a randomized date
Women were followed from the date of delivery until PPD, death, emigration, or 12 months following the date of delivery, whichever came first. We fitted Poisson regression models censoring for death, emigration, a diagnosis of depression, or end of follow-up, whichever came first. As a primary comparison, we calculated the risk of depression during the 12 months following childbirth, comparing women with a history of depression to women without a history of depression. Relative risk was estimated by the incidence rate ratios obtained from the Poisson regression. Since the relative risk of PPD is conditional on a specific event in time (namely child birth), we wanted to compare this risk estimate with the risk for a depression diagnosis at a randomly generated time point. To accomplish this, we calculated the relative risk for a depression diagnosis beginning follow-up from an artificial date: the population age specific expected date of delivery. In this approach, we selected a random date of follow-up from the distribution of delivery dates of women born the same year. This phantom delivery date is artificial and should presumably not be associated with a causal effect while at the same time be representative of women of the same age. We then calculated the 12-month incidence relative risk of depression adjusted for the true date of delivery from this random date. This methodology will automatically adjust for any seasonal variations and risk associated with age. For both models, we compared women with a history of depression to women without a history of depression, at the start or follow-up for PPD.
For estimated risks, the associated two-sided 95% Wald-type confidence intervals (CI) were calculated, corresponding to a statistical test on the two-sided 5% level of significance. Data management and all statistical models (Poisson regression using PROC GLIMMIX) were conducted using the SAS software version 9.4 64-bit running Debian Linux.
Results
Characteristics of the study cohort
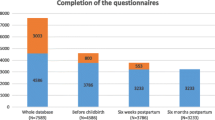
A total of 707,701 unique women with a live singleton birth between 1997 and 2008 were identified, 13,934 of whom had a history of depression. As previously detailed (Silverman et al. 2017), among the 4397 women identified with PPD, 1485 (33.8%) women had a history of depression, adjusted relative risk with 95% confidence intervals (95% CI) = 21.0 (19.7–22.4).
Relative risk of depression diagnosis to a computer-generated randomized date
When we randomly created artificial dates of delivery, 86% of the women were assigned a date later than 3 months after, or more than 12 months before, their actual date of delivery. Beginning follow-up for depression diagnosis following this artificial date of delivery, the adjusted relative risk for women with a history of depression was 26.2 (CI 24.7–27.9).
Discussion
Early maternal depression is often reported to be the most common complication associated with childbirth (Gaynes et al. 2005; Guardino and Schetter 2014; O’Hara and Wisner 2014). Past large-scale epidemiologic explorations have demonstrated that women with a history of depression are at greatest risk for PPD (Fisher et al. 2012; Räisänen et al. 2014; Silverman et al. 2017; Rasmussen et al. 2017). The results of this study suggest that for these women, the risk for depression in the postpartum period is no greater when compared to that at a random time surrounding the same childbearing years. This finding suggests that the postpartum period may not necessarily represent a time of heightened vulnerability (Di Florio and Meltzer-Brody 2015; Hoertel et al. 2015).
Using a nationally inclusive sample, this study represents the largest exploration into whether PPD, a depressive illness uniquely characterized as temporally associated with a specific event, is more common than the incidence of depression at other times during childbearing years. By comparing the incidence of PPD in women presumably at greatest risk to the 12-month incidence of depression following a randomly generated artificial delivery date, we provide the first substantial evidence that the risk of depression following childbirth is no greater than at other times in a woman’s childbearing years and may even be lower.
Comparing the 12-month incidence of a clinical depression diagnosis after each woman’s actual delivery date to an arbitrary and randomly generated phantom delivery date allowed us to observe whether the time surrounding pregnancy and the postpartum is truly a period of higher vulnerability for depression as frequently reported (O’Hara and Swain 1996; Bennett et al. 2004; Fisher et al. 2012). That the relative risk of depression in the postpartum period was not larger compared to that at this randomly generated date is both interesting and surprising given the considerable research attention PPD prevalence has received. While the study methodology purposely excluded psychiatric disorders unassociated with unipolar depression, there is a well-understood first emergence risk in the postpartum for women with other psychiatric disorders, such as bipolar (Bergink et al. 2016), as well as an associated increased readmission rate that are presumed to be biologically based (Wesseloo et al. 2016). Because the incidence and relative risk of unipolar depression in the postpartum were lower than those at a randomly generated arbitrary date, one might posit that the reported incidence of PPD is pathogenically unrelated to child delivery. Second, consistent with the hypothesis that depression following pregnancy may, for women with a history of depression, simply represent the natural reemergence of a recurrent depressive disorder, these results also point to the possibility that for a considerably smaller subgroup, namely those without a depression history who develop PPD, there may be an alternative underlying cause. Indeed, this finding is consistent with the possibility that depression in the perinatal period is a complex and heterogeneous disorder (Postpartum Depression: Action Towards Causes and Treatment (PACT) Consortium 2015) occurring via multiple pathways (O’Hara and Wisner 2014; Di Florio and Meltzer-Brody 2015). While the intent of this study was to test the association between childbirth and depression in new mothers, because of the repeatedly observed rarity of clinically ascertained PPD absent of a depression history (Fisher et al. 2012; Räisänen et al. 2014; Silverman et al. 2017; Rasmussen et al. 2017), future studies should consider the possibility that PPD in women with and without a depression history may in fact represent different phenotypes of depression (Navarro et al. 2008; Silverman et al. 2011; Altemus et al. 2012).
Although these findings are of considerable clinical importance, we do recognize some possible study limitations. First, we only explored PPD following first births. This methodology was chosen to avoid the problem of correlated observations between successive births and was the clearest approach given the sample size and high power available using first births. However, because it is possible that some women did not display clinically significant symptomatology until subsequent births (Cooper and Murray 1995), we may have underestimated the overall incidence of PPD. Similarly, because our findings are reliant on registry-based, clinically captured depression rates, we may have underestimated the true association of depression history and depression at any of the observed time points. That is, registry observations may not be fully representative of case prevalence and some numbers of mild depression cases may have fallen below the threshold of clinician detection or diagnostic certainty. This is a well-understood limitation of registry resolution and diagnostic sensitivity in general. While it is difficult to estimate whether incomplete sensitivity would lead to an estimation error, we believe it is far less likely that noncases would be coded incorrectly by clinicians as cases, and if an error was made, it is more likely one of underestimation.
Certainly, a problem universal to all health registry-based studies is the fact that outcome variables may represent treatment-seeking behavior as opposed to actual incidence. While it would seem intuitive that women with a depression history would be more aware of early depression symptomatology, because pregnant and postpartum women represent a medically captured population combined with Sweden’s nationwide universal perinatal mental health initiatives, the observed registry rates for postpartum depression more likely represent treatment-capture as opposed to self-initiated treatment-seeking behavior. More specifically, all postpartum women in Sweden benefit from an in-home healthcare visit after child delivery. This visit is conducted by a healthcare professional, most often a nurse, who is experienced in perinatal mental health. During these visits, secondary to health policy, all new mothers are screened for depressive symptomatology and, if necessary, a structured clinical assessment is provided and/or a referral is made. This therefore underscores an additional strength of the Swedish Health Resources—that is, because the Swedish heathcare services universally screen for treatment need in the postpartum period, they presumably provide the closest approximation of postpartum depression incidence. This, coupled with the possibility that a woman with a history of depression is also more likely to be given a re-diagnosis because she is likely being monitored more closely by clinicians for these symptoms compared to women with no prior depression treatment, further reduces the possibility of depression incidence underestimation. In comparison to pregnant and postpartum women currently receiving regular medical attention, the incidence of depression to the computer-generated, randomized date more likely represents self-initiated, treatment-seeking, behaviors. However, even if this were the case, the incidence of depression within 12 months of the phantom delivery date would therefore have been underestimated, as opposed to overestimated, thereby reducing the relative risk estimate. Finally, because the phantom delivery date was randomly generated, it is likely that a very small number of women will be randomized to their actual delivery date. In other words, it is possible that for a small number of cases we would be assessing the same depression event. However, given the nationally inclusive sample size, it is unlikely this occurrence would have resulted in producing a considerably different risk estimate.
In summary, because maternal depression can result in negative personal, family, and child developmental outcomes (Surkan et al. 2012), it is a serious public health concern. However, the classification of a mood disorder temporally associated with a specific event is unique and whether the nosology of PPD warrants a diagnostic specifier remains controversial. Given the compelling evidence supporting the chronicity of depression throughout the female life span (Kessler 2003) and that the observed risk of clinically relevant depression in the postpartum period was not higher compared to that at an arbitrarily selected date for the subgroup of women with a history of depression, our data provides compelling evidence supporting the possibility that PPD may represent a diagnostic illusory correlation (Borrell-Carrio and Epstein 2004, Klein 2005). That is, the well-established observation of depression covarying with childbirth may not necessarily equate to causation, but rather may be a secondary effect of postpartum women being regularly screened during this time. Indeed, while this finding may seem initially counterintuitive and even controversial, suicidal ideation while closely associated with depression is also understood to occur at lower rates during the perinatal and the postpartum period than in the general population (Healey et al. 2013). Together, these findings raise important questions: firstly, whether the inclusion of the postpartum onset specifier for a major depressive disorder, a psychiatric disorder based on timing of onset as opposed to unique symptomatology, and for which treatment is undifferentiated, remains diagnostically useful and, secondly, whether screening for depression history and antepartum mood screenings would be equally beneficial during prenatal care visits and before delivery.
References
Altemus M, Neeb CC, Davis A, Occhiogrosso M, Nguyen T, Bleiberg KL (2012) Phenotypic differences between pregnancy-onset and postpartum-onset major depressive disorder. J Clin Psychiatry 73(12):e1485–e1491
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. APA Press, Arlington
Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR (2004) Prevalence of depression during pregnancy: systematic review. Obstet Gynecol 103(4):698–709
Bergink V, Rasgon N, Wisner KL (2016) Postpartum psychosis: madness, mania, and melancholia in motherhood. Am J Psychiatry 173(12):1179–1188
Borrell-Carrio F, Epstein RM (2004) Preventing errors in clinical practice: a call for self-awareness. Ann Fam Med 2(4):310–316
Cooper PJ, Murray L (1995) Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. Br J Psychiatry 166(2):191–195
Cooper PJ, Campbell EA, Day A, Kennerley H, Bond A (1988) Non-psychotic psychiatric disorder after childbirth. A prospective study of prevalence, incidence, course and nature. Br J Psychiatry 152:799–806
Corwin EJ, Kohen R, Jarrett M, Stafford B (2010) The heritability of postpartum depression. Biol Res Nurs 12(1):73–83
Cox J (2017) Use and misuse of the Edinburgh Postnatal Depression Scale (EPDS): a ten point ‘survival analysis’. Arch Womens Ment Health 20(6):789–790
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150:782–786
Di Florio A, Meltzer-Brody S (2015) Is postpartum depression a distinct disorder? Curr Psychiatry Rep 17(10):76–82
Fisher J, de Mello MC, Patel V, Rahman A, Tran T, Holton S, Holmes W (2012) Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ 90:139–149
Forty L, Jones L, Macgregor S, Caesar S, Cooper C, Hough A, Dean L, Dave S, Farmer A, McGuffin P, Brewster S, Craddock N, Jones I (2006) Familiality of postpartum depression in unipolar disorder: results of a family study. Am J Psychiatry 163(9):1549–1553
Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T (2005) Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 106:1071–1083
Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC (2005). Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evidence Report/Technology Assessment No. 119. (Prepared by the RTI-University of North Carolina Evidence-based Practice Center, under Contract No. 290–02-0016.) AHRQ Publication No. 05-E006–2. Rockville, MD: Agency for Healthcare Research and Quality
Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R (2009) A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand 119(5):350–364
Gjerdingen DK, Yawn BP (2007) Postpartum depression screening: importance, methods, barriers, and recommendations for practice. J Am Board Fam Med 20(3):280–288
Guardino CM, Schetter CD (2014) Coping during pregnancy: a systematic review and recommendations. Health Psychol Rev 8(1):70–94
Healey C, Morriss R, Henshaw C, Wadoo O, Sajjad A, Scholefield H, Kinderman P (2013) Self-harm in postpartum depression and referrals to a perinatal mental health team: an audit study. Arch Womens Ment Health 16(3):237–245
Hoertel N, López S, Peyre H, Wall MM, González-Pinto A, Limosin F, Blanco C (2015) Are symptom features of depression during pregnancy, the postpartum period and outside the peripartum period distinct? Results from a nationally representative sample using item response theory (IRT). Depress Anxiety 32(2):129–140
Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J (2014) Non-psychotic mental disorders in the perinatal period. Lancet 384(9956):1775–1788
Kessler RC (2003) Epidemiology of women and depression. J Affect Disord 74(1):5–13
Klein JG (2005) Five pitfalls in decisions about diagnosis and prescribing. BMJ 330(7494):781–783
Maust DT, Kim HM, Seyfried LS, Chiang C, Kavanagh J, Schneider LS, Kales HC (2015) Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiatry 72(5):438–445
Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB (2006) New parents and mental disorders: a population-based register study. JAMA 296(21):2582–2589
Myers ER, Aubuchon-Endsley N, Bastian LA, Gierisch JM, Kemper AR, Swamy GK et al (2013) Efficacy and safety of screening for postpartum depression. Comparative Effectiveness Review 106. AHRQ Publication No. 13-EHC064-EF. Agency for Healthcare Research and Quality, Rockville
Navarro P, García-Esteve L, Ascaso C, Aguado J, Gelabert E, Martín-Santos R (2008 Jul) Non-psychotic psychiatric disorders after childbirth: prevalence and comorbidity in a community sample. J Affect Disord 109(1–2):171–176
O’Hara MW, McCabe JE (2013) Postpartum depression: current status and future directions. Annu Rev Clin Psychol 9:379–407
O’Hara MW, Swain AM (1996) Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry 8:37–54
O’Hara MW, Wisner KL (2014) Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol 28(1):3–12
O’Hara MW, Zekoski EM, Philipps LH, Wright EJ (1990) Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 99:3–15
Postpartum Depression: Action Towards Causes and Treatment (PACT) Consortium (2015) Heterogeneity of postpartum depression: a latent class analysis. Lancet Psychiatry 2(1):59–67
Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S (2014) Risk factors for and perinatal outcomes of major depression during pregnancy: a population-based analysis during 2002-2010 in Finland. BMJ Open 4(11):e004883
Rasmussen MH, Strøm M, Wohlfahrt J, Videbech P, Melbye M (2017 Sep 26) Risk, treatment duration, and recurrence risk of postpartum affective disorder in women with no prior psychiatric history: a population-based cohort study. PLoS Med 14(9):e1002392
Savitz D, Stein C, Yee F, Kellerman L, Silverman ME (2011) The epidemiology of hospitalized postpartum depression in New York State, 1995–2004. Ann Epidemiol 21(6):399–406
Silverman ME, Loudon H, Liu X, Mauro C, Leiter G, Goldstein MA (2011) The neural processing of negative emotion postpartum: a preliminary study of amygdala function in postpartum depression. Arch Womens Ment Health 14(4):355–359
Silverman ME, Reichenberg A, Savitz DA, Cnattingius S, Lichtenstein P, Hultman CM, Larsson H, Sandin S (2017) The risk factors for postpartum depression: a population-based study. Depress Anxiety 34(2):178–187
Surkan PJ, Ettinger AK, Ahmed S, Minkovitz CS, Strobino D (2012) Impact of maternal depressive symptoms on growth of preschool- and school-aged children. Pediatrics 130(4):847–855
Thombs BD, Kwakkenbos L, Levis AW, Benedetti A (2018) Addressing overestimation of the prevalence of depression based on self-report screening questionnaires. CMAJ 190(2):E44–E49
Viktorin A, Meltzer-Brody S, Kuja-Halkola R, Sullivan PF, Landén M, Lichtenstein P, Magnusson PK (2015) Heritability of perinatal depression and genetic overlap with nonperinatal depression. Am J Psychiatry 173(2):158–165
Wesseloo R, Kamperman AM, Munk-Olsen T, Pop VJ, Kushner SA, Bergink V (2016) Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry 173(2):117–127
Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH (2013) Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 70(5):490–498
World Health Organization (1992) International statistical classification of diseases and related health problems, 10th revision (ICD-10). WHO, Geneva
Funding
This study was supported by a grant to Michael E. Silverman from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; Grant number: R21HD073010.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Rights and permissions
About this article
Cite this article
Silverman, M.E., Reichenberg, A., Lichtenstein, P. et al. Is depression more likely following childbirth? A population-based study. Arch Womens Ment Health 22, 253–258 (2019). https://doi.org/10.1007/s00737-018-0891-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-018-0891-5