Abstract
It is well established that a subgroup of women are particularly vulnerable to affective dysregulation during times of hormonal fluctuation. One underrecognized reproductive transition may be late-onset postpartum depression (PPD) in the context of weaning from breastfeeding and the resumption of menstruation. The goal of this review is to propose a biologically plausible mechanism for affective dysregulation during these transitions. The relationship between affective symptoms and neurohormonal changes associated with weaning will be investigated through a hypothesis-driven review of relevant literature. Neurosteroids, like allopregnanolone (ALLO), are widely recognized for augmenting GABAergic inhibition and having a powerful anxiolytic effect (Belelli D and Lambert JL, Nature Reviews Neuroscience 6:565-575, 2005). However, when ALLO is administered after prolonged withdrawal, there may be a paradoxical anxiogenic effect (Smith et al., Psychopharmacology 186:323–333, 2006; Shen et al., Nat Neurosci 10:469–477, 2007). Weaning from breastfeeding is a physiologic example of fluctuating levels of ALLO after prolonged withdrawal. We propose that the complex hormonal milieu during weaning and resumption of menstruation may modify GABAA receptors such that ALLO may contribute to rather than ameliorate depressive symptoms in vulnerable individuals. The proposed model provides an initial step for understanding the mechanisms by which the changing hormonal environment during weaning and resumption of menstruation may contribute to an increased risk of depression in a subgroup of women who are hormonally sensitive. Future research investigating this model would be valuable both to identify women at increased risk for developing mood symptoms late in postpartum and to inform treatment for this and related reproductive depressive disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women who have mood symptoms in the context of gonadal hormone changes may have a distinct type of depression compared with women who have non-reproductive-related mood symptoms (Cooper and Murray 1995; Payne et al. 2009; Viktorin et al. 2016). This hormonal sensitivity to depression has been referred to as “reproductive depression” and includes menarche, perinatal depression, premenstrual dysphoric disorder (PMDD), and depression in the perimenopausal period (Payne et al. 2009).
We hypothesize that depression at the time of weaning, which may be a proxy for resumption of menstruation, is an additional example of a reproductive depression that may be underappreciated due to limitations in the current definition of perinatal depression. The DSM-5 (https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596) defines perinatal depression with the specifier “with peripartum onset”: a major depressive episode beginning during pregnancy or within 4 weeks of delivery. The first month postpartum is a period of elevated risk for perinatal depression, and genetic studies have suggested that women presenting with depression during this time period may have a distinct clinical phenotype (Forty et al. 2006). However, the clustering of risk in the first postnatal month may be more attributable to bipolar disorder than major depressive disorder (Jones and Cantwell 2010). While rates of symptom onset for unipolar depression have been consistently shown to be highest in the first 6 to 8 weeks postpartum, multiple studies have now demonstrated that risk for symptom onset extends far beyond this (Stowe et al. 2004; Munk-Olsen et al. 2006; Gjerdingen et al. 2011; Kothari et al. 2016). A retrospective study of women with postpartum onset of major depression showed that only 54% of cases occurred within the first month postpartum (Altemus et al. 2012). This suggests that a substantial proportion of depression associated with the postpartum remains poorly characterized and poorly explained.
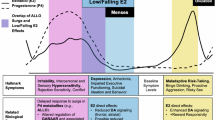
Research on mood changes associated with weaning is scarce. As illustrated in Fig. 1, this period is difficult to study due to multiple complicating factors such as variation in return to ovulation and menstrual cycling postpartum, variable use of hormonal contraceptives in the postpartum, variation in infant feeding patterns, and broad psychosocial stressors associated with or co-occurring with weaning. Rare case reports have been published. Susman and Katz (1988) presented four cases of mothers with depression starting within 2 weeks of weaning, and Sharma and Corpse (2008) presented a case of a woman who developed depression after completing weaning with each of her three infants, despite stopping breastfeeding after variable durations with each child. Epidemiologic studies suggest that this phenomenon is likely underrepresented by the scarcity of these cases in the literature. In fact, Misri et al. (1997) found that 17% of postpartum depression cases emerged after the time of weaning.
Sources of variation that complicate investigation of late-onset postpartum depression in breastfeeding women. Potential complicating factors that affect ALLO and GABA-A regulation in the postpartum are illustrated in the figure. Each bar represents a period of individual variation for a typical postpartum event, informed by American Academy of Pediatrics (AAP) and American College of Obstetrics and Gynecology (ACOG) recommendations as well as the Family and Medical Leave Act (FMLA). Individual variability in each of these domains may challenge identification of a late-onset postpartum depression phenotype even if unifying neurohormonal mechanisms exist
Despite the complicated neurohormonal milieu specific to the postpartum, multiple neurohormonal similarities to other periods of reproductive transition such as menarche and menopause do exist and may be a useful starting point for understanding the etiology of late-onset postpartum depression. For this review, we will begin with an examination of research on the role of gonadal steroids in reproductive depressions and then focus in on the role of allopregnanolone (ALLO) in particular. We will borrow from research on ALLO-associated depression at other reproductive transition points in the female life cycle in order to better understand weaning-associated symptoms. Though other mechanisms related to lactation-associated depression are likely to exist, we believe that there is robust evidence to support ALLO’s role in late-onset postpartum depression associated with weaning and/or resumption of menses postpartum and that prior research on this mechanism maintains validity when applied to this transition as well.
Gonadal steroids and perinatal depression
Estrogen and progesterone circulate at supraphysiologic levels during pregnancy and precipitously decline at parturition (Bloch et al. 2003). The onset of affective symptoms during these dramatic hormonal shifts in the early postpartum has generated interest in gonadal steroids in the pathophysiology of postnatal depression. However, gonadal hormone studies of postnatal depression have not revealed demonstrable differences in the physiology of estrogen and progesterone between affected and unaffected women. Women who develop postnatal depression do not have more rapid postpartum hormone withdrawal, greater reductions in hormone levels from pregnancy to the postpartum period, or lower absolute concentrations of estradiol and progesterone compared to healthy controls (Schiller et al. 2014).
In response, some researchers have hypothesized that there is a vulnerable subpopulation of women that are more sensitive to the same hormonal changes than the general population (Schiller et al. 2015). This hypothesis has since been supported in a number of small studies. Schmidt et al. (1998) successfully eliminated menstrual-related depressive symptoms in patients with a history of PMDD using a GnRH agonist, while hormone add-back caused symptom return. This same hormone manipulation had no effect on mood in control patients. Similarly, in a study by Bloch et al. (2000), euthymic women were given high doses of estradiol and progesterone during ovarian suppression with a GnRH agonist to mimic antepartum levels, and then, both steroids were abruptly withdrawn. Women with a history of postnatal depression reported increased depressive symptoms during both hormone add-back and hormone withdrawal, but no mood changes were observed in control patients. This study design removed confounding biological and psychological stressors associated with childbirth and again provided evidence that a subpopulation of women, those with a history of postnatal depression, were particularly susceptible to rapid changes in reproductive hormones independent from pregnancy (Schiller et al. 2015).
ALLO and depression
In an effort to better characterize a reproductive depression phenotype, there has been increased attention to the role of ALLO. ALLO is a neurosteroid metabolite of progesterone, which is known to modulate GABAA receptors. There is evidence that ALLO plays a role in depression outside of reproductive transitions. However, the nature of ALLO’s role in affective illness is complex, as some studies have implicated inadequate ALLO levels while others have implicated changing ALLO levels, and it is unclear the extent to which ALLO’s effect on mood may differ in the presence or absence of fluctuating gonadal steroid levels or between men and women. ALLO levels have been found to be low in major depressive disorder and to elevate with antidepressant treatment (Uzunova et al. 1998; Romeo et al. 1998; Ströhle et al. 1999; Schüle et al. 2006, 2007; Eser et al. 2006). Furthermore, circulating levels of ALLO are correlated with progesterone levels in women and fluctuate during the menstrual cycle, pregnancy, and postpartum (Gilbert Evans et al. 2005; Schiller et al. 2014). The relationship between ALLO levels and contraceptive agents is complex, although ALLO levels do appear to correlate with some synthetic progestins (those that are not 19-nor derivatives) and estrogens used in some contraceptives appear to stimulate ALLO synthesis (Bernardi et al. 2003). During lactation, the hypothalamic-pituitary-ovarian (HPO) axis is suppressed and therefore ALLO levels remain low. With resumption of menstrual cycling in the later postpartum, ALLO fluctuations resume with mid-luteal peaks (Wang et al. 1996; Genazzani et al. 1998; Luisi et al. 2000). The combination of ALLO’s known association with depression as well as physiologic fluctuations in ALLO during periods of risk for reproductive depression makes ALLO an attractive candidate for study in regard to the pathophysiology of the reproductive depression phenotype.
Depending on the context, ALLO can be either anxiolytic or anxiogenic (Backstrom et al. 2014). ALLO is well known for its anxiolytic property, which has been replicated in multiple rodent models (Akwa et al. 1999; Wieland et al. 1991; Schüle et al. 2014). In a small study of panic disorder in humans, ALLO levels have been shown to acutely decrease in response to sodium lactate or CCK-4-induced panic, but only in subjects with previously diagnosed panic disorder (Ströhle et al. 2003). More recent research has focused on anxiolytic and antidepressant effects of ALLO specifically in peripartum populations. In one study, infusion of intravenous brexanolone, which is a synthetic analog of ALLO now in development as a pharmaceutical, resulted in reduction in severe postnatal depression compared to placebo (Kanes et al. 2017). In addition, a recent study by Osborne et al. 2017 suggested that blunted ALLO levels during pregnancy predicted postnatal depression in a linear fashion. Taken together, this line of research implies that raising ALLO levels in women at risk for or affected by perinatal depression may be a reasonable strategy for treatment or even prevention.
However, in other contexts, ALLO appears to be paradoxically anxiogenic. For example, women with PMDD often develop mood symptoms in the mid-luteal phase of the menstrual cycle and some women with perinatal depression begin to develop mood symptoms during pregnancy, both of which are periods when ALLO levels rise (Gotlib et al. 1989; Pearlstein et al. 2005). In addition, two studies have demonstrated that administering progesterone in the postnatal period increased affective symptoms in women with a history of perinatal depression (Lawrie et al. 1998; Bloch et al. 2000). Furthermore, in a study by Schmidt et al. (1998), women with premenstrual syndrome (PMS) whose symptoms remitted with a GnRH agonist demonstrated mood worsening with progesterone add-back. Interestingly, this study also demonstrated mood worsening with estradiol add-back, which remains poorly understood although may also relate to anxiogenic effects of ALLO. Estrogens have been shown to increase ALLO levels in postmenopausal women undergoing hormone replacement treatment (HRT), possibly via modulation of enzymes involved in ALLO biosynthesis (Bernardi et al. 2003).
Reconciling the seemingly conflicting data on ALLO’s effect on mood has been a challenge for the field of reproductive psychiatry. For the purpose of our review, we will focus on the explanatory effect of fluctuating ALLO levels on GABAA physiology. There are several additional possible explanations, some tangentially related to ALLO’s effect on GABAA physiology, that are worthwhile avenues for further study but beyond the scope of this review. The first is that, given the complex hormonal milieu during periods of reproductive transition, there may be other mitigating or enhancing factors that influence ALLO’s effects on mood such as estrogen, lactogens, inflammation, and alterations in the stress-response system (Bloch et al. 2003; Brunton et al. 2015; Kimmel et al. 2016; Roomruangwong et al. 2018). Second, there may be subpopulations of women with reproductive depression that have different affective responses to different ALLO levels, possibly in the fashion of a U-shaped curve (Backstrom et al. 2014). Third, there may be differential metabolism of progesterone in affected women such that ratios of progesterone to allopregnanolone are altered in women with depression (Girdler et al. 2001; Klatzkin et al. 2006). Last, ALLO’s effect on mood may depend on other contextual factors such as the presence of stress and/or the reactivity of the stress-response system (Smith et al. 2006).
Changes in rather than levels of ALLO dysregulate affective state in susceptible individuals
It has been widely hypothesized that the change in ALLO levels rather than the absolute concentration of those levels may be responsible for mood changes in sensitive individuals. Similar to studies of gonadal steroids, which have failed to consistently show an association between PMDD and postnatal depression symptoms and absolute concentrations of estrogen and progesterone, abnormal plasma levels of ALLO have not been consistently observed in PMDD and postnatal depression (Schmidt et al. 1994; Wang et al. 1996; Rapkin et al. 1997; Monteleone et al. 2000; Epperson et al. 2002; Lombardi et al. 2004; Deligiannidis et al. 2013; Hellgren et al. 2014; Crowley et al. 2016; Deligiannidis et al. 2016). In fact, both increases and decreases in ALLO have been shown to produce anxiogenic behavior (Gulinello et al. 2001, Gulinello and Smith 2003; Shen et al. 2005). In a recent study by Schiller et al. (2014), they reexamined data from previous studies of ovarian suppression with a GnRH agonist and subsequent progesterone add-back in women with a history of PMDD and postnatal depression. In both groups, change in ALLO after progesterone add-back was negatively correlated with depressive symptoms in patients with a history of PMDD or postnatal depression, but the effect was absent in controls. Furthermore, Martinez et al. (2016) stabilized ALLO levels from the follicular to the luteal phase of the menstrual cycle by administering a 5α-reductase competitive inhibiter to patients with a history of PMDD and healthy controls. They observed a significant reduction in PMDD symptoms in patients and no mood changes in controls. Both studies support the hypothesis that changes in ALLO levels may serve as an “affective switch” in a subset of vulnerable women (Schiller et al. 2014).
Mechanism of ALLO’s effect on mood in vulnerable populations
The effect of changing ALLO levels on depressive symptoms in vulnerable women is likely related to GABAergic functioning, which we propose is particularly relevant to weaning-induced depressions. There are multiple GABAA modulators known to have a biphasic effect at the receptor, including ALLO (Wang 2011). The GABAA receptor is composed of various subunits, which can greatly influence its sensitivity to neurosteroids like ALLO (MacKenzie and Maguire 2014). For example, during pregnancy, when levels of progesterone and ALLO are extremely elevated, the expression of the δ subunits is downregulated in multiple areas of the brain, which reduces receptor sensitivity to elevated ALLO levels (Maguire and Mody 2008). Furthermore, the GABAA receptor is extremely plastic, and its subunit composition can change during fluctuations in ALLO levels (Gordon et al. 2015). Gulinello et al. (2001; 2003) have demonstrated that either increases or decreases in ALLO can trigger changes in the α4 subunit of the GABAA receptor enough to trigger anxiogenic behavior. Smith et al. (2006) demonstrated that ALLO withdrawal increased the expression of GABAA receptor α4 subunit in the mouse CA1 hippocampus. After an extended period of withdrawal, when ALLO was reintroduced in combination with an aversive stimulus, this triggered hippocampal excitability rather than inhibition in mice. Based on these findings, they hypothesized that prolonged ALLO withdrawal may modify GABA receptors such that reintroduction of ALLO produces an anxiogenic effect rather than an anxiolytic effect.
Studies of ALLO physiology during puberty have demonstrated that it is anxiogenic during this reproductive transition as well and that this effect may be related to ALLO having a paradoxical modulation of GABAA receptors. Shen et al. (2007) studied the interaction between ALLO, GABAA receptor subunits, and anxiety during puberty and proposed that the anxiogenic effect of ALLO is due to a particular configuration of subunits (α4β2δ) of GABAA receptors. This particular subunit configuration is induced by prolonged withdrawal of ALLO in pubertal mice, and it reverses GABA-gated current, inhibiting it instead of enhancing it. We suggest that this reversal of GABA-gated current may also occur in women resuming menstruation in the puerperum.
The role of prolonged ALLO withdrawal in triggering a paradoxical effect of ALLO on GABAA responsivity makes this mechanism particularly relevant to late-onset postnatal depression. After parturition, there is a precipitous decline in progesterone and, therefore ALLO, followed by static low levels until menstrual cycling returns. Breastfeeding further extends the period of ALLO withdrawal since lactation delays the resumption of menstrual cycling. Therefore, weaning, which represents a physiologic example of reintroduction of ALLO after a period of withdrawal, could contribute to the pathophysiology of late-onset postnatal depression.
If GABAergic dysregulation is involved in reproductive depression, then genes coding for GABAA receptor subunits may predispose certain individuals to respond to changes in ALLO maladaptively (Gordon et al. 2015). It has already been established that GABAA receptor subunit polymorphisms are associated with an increased risk of other psychiatric disorders including major depressive disorder, bipolar disorder, schizophrenia, and alcohol dependence (Soyka et al. 2008; Fatemi et al. 2013). In an animal model, Maguire and Mody (2008) demonstrated that GABAA receptor δ-subunit knock-out mice exhibit behavioral abnormalities consistent with PPD. These mice are behaviorally silent until exposed to pregnancy and the postpartum state, at which time they demonstrate depressive symptoms and cannibalize their young. This model demonstrates that reproductive events may provoke affective dysregulation in genetically susceptible individuals.
Linking depressive symptoms associated with ALLO fluctuation across the reproductive life cycle
ALLO fluctuations, at least in a subset of vulnerable women, are relevant triggers for depressive symptoms throughout the female reproductive lifespan (Gordon et al. 2015). Better characterizing ALLO physiology during multiple periods of reproductive transition is likely to facilitate the study of this mechanism as well as to better specify the vulnerable phenotype by illuminating similarities and differences within this complex neurohormonal system. Table 1 summarizes knowledge to date on ALLO physiology, as well as related HPO and hypothalamic-pituitary-adrenal (HPA) physiology, across five points of reproductive transition.
We believe that menarche is particularly similar to postpartum resumption of menstruation in that both are a period of transition out of physiologic hypogonadotropic hypogonadism, with GnRH neurons being quiescent prior to menarche and suppressed during the puerperum (Strauss and Barbieri 2014). The erratic nature of LH pulsatility and therefore ovulation frequency in both menarche and the late postpartum would result in irregular ALLO fluctuations and challenge the plasticity of GABAA receptors. Additionally, lactation prolongs the period of hypogonadotropic hypogonadism to varying degrees, which may contribute to increased sensitization of the GABAA receptor to ALLO. We propose that the variable LH pulse patterns, which results in erratic hormone fluctuations, including changes in ALLO levels, likely cause an increased susceptibility to mood dysregulation both in puberty and during menstrual resumption postnatally.
Other authors including Gordon et al. (2015) have proposed that similar GABAergic mechanisms may govern other reproductive transitions such as the perimenopause. The HPO axis during perimenopause has many similarities to menarche and the puerperal resumption of menstruation, including erratic LH pulsatility, erratic ovulatory patterns, and irregular ALLO fluctuations. However, differences also exist and data examining GABAergic functioning in both the perimenopause and puerperal resumption of menstruation are lacking. This characterization of the reproductive phenotype across the female lifecycle is an important next step for research.
Future directions
Despite mood symptoms with weaning and resumption of menstruation being commonly encountered clinically, it has unfortunately been studied little. We propose that there are two primary reasons for this. First, there is tremendous variability in the natural course of postpartum ALLO fluctuations related to variability in menses, variable use of hormonal contraceptive agents, and variability in infant feeding patterns both in relation to breastfeeding as well as in relation to the introduction of and reliance upon solid foods for nutritional sustenance. Such variability along multiple relevant constructs makes it challenging to identify a consistent phenotype for study. Nonetheless, in regard to ALLO, there may be a unifying etiologic explanation for depressive symptoms across the female reproductive lifespan, which would demand a different conceptualization of the phenotype: one relying on mechanisms rather than timing of symptoms or specific reproductive triggers for neurosteroid fluctuation. In order to accomplish this, more research is needed to characterize ALLO physiology during and around each major reproductive transition point. For example, what are ALLO fluctuation patterns in relation not only to parturition, but also to resumption of menstruation, use of hormonal contraceptives in the postpartum, and infant feeding patterns? For women with known vulnerability to reproductive depressions, what are the relationships between ALLO fluctuations and their symptoms?
The second reason we believe that late-onset postnatal depression has been neglected in the literature has been the complexity of this neurohormonal system overall. There are multiple neurohormonal systems that are likely relevant to depressive symptoms in the late postpartum including not only ALLO but also resumption of fluctuating estrogens, withdrawal of lactogens, inflammation and aberrant immune functioning, changes in the stress-response system, and possibly others. Therefore, simplifying an explanatory model is sufficiently enough for study risks neglecting multiple important contributing factors. We believe that one strategy for overcoming this is to start with mechanisms that may be similar across multiple risk periods for depression in the female reproductive lifespan. Clarifying these central mechanisms would provide an important framework that could allow for more effective study of modulating factors specific to a particular risk period as well as minimize confounding from psychosocial variables. We believe that the role of fluctuating ALLO levels on GABAergic functioning is a prime candidate for this study.
Conclusion
We hypothesize that late-onset postnatal depression that is associated with weaning and resumption of menstrual cycling may be largely attributable to GABAA dysregulation by ALLO after a period of prolonged withdrawal. Similar patterns of changes in ALLO are observed at other time points of reproductive transition throughout the female reproductive life cycle, and better understanding these similarities is likely to be helpful in facilitating the study of late-onset postnatal depression. Further research is warranted to confirm this hypothesis as well as to better understand how it might interface with other relevant systems (see Fig. 2) including the HPA axis (via changes in adrenal metabolism or oxytocin effects), HPO axis (via estrogen modulation and/or progesterone metabolism), immunologic functioning (via GABAergic modulation of the adaptive immune system) (Bhat et al. 2010), and lactogenic hormones (via oxytocin modulation of GABAA receptors) (Smith et al. 2016).
References
Akwa Y, Purdy RH, Koob GF, Britton KT (1999) The amygdala mediates the anxiolytic-like effect of the neurosteroid allopregnanolone in rat. Behav Brain Res 106:119–125
Altemus M, Neeb CC, Davis A, Occhiogrosso M, Nguyen T, Bleiberg KL (2012) Phenotypic differences between pregnancy-onset and postpartum-onset major depressive disorder. J Clin Psychiatry 73(12):1485–1491
Backstrom T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G, Savic I, Strömberg J, Timby E, van Broekhoven F, van Wingen G (2014) Allopregnanolone and mood disorders. Prog Neurobiol 113:88–94
Bernardi F, Pieri M, Stomati M, Luisi S, Palumbo M, Pluchino N, Ceccarelli C, Genazzani AR (2003) Effect of different hormonal replacement therapies on circulating allopregnanolone and dehydroepiandrosterone levels in postmenopausal women. Gynecol Endocrinol 17(1):65–77
Bhat R, Axtell R, Mitra A, Miranda M, Lock C, Tsien RW, Steinman L (2010) Inhibitory role for GABA in autoimmune inflammation. PNAS 107(6):2580–2585
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR (2000) Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry 157(6):924–930
Bloch M, Daly RC, Rubinow DR (2003) Endocrine factors in the etiology of postpartum depression. Compr Psychiatry 44:234–246
Brunton PJ, Donadio MV, Yao ST, Greenwood M, Seckl JR, Murphy D, Russell JA (2015) 5α-Reduced neurosteroids sex-dependently reverse central prenatal programming of neuroendocrine stress responses in rats. J Neurosci 35(2):666–677
Cooper P, Murray L (1995) Course and recurrence of postnatal depression: evidence for the specificity of the diagnostic concept. Br J Psychiatry 166:191–195
Cox EQ, Stuebe A, Pearson B, Grewen K, Rubinow D, Meltzer-Brody S (2015) Oxytocin and HPA stress axis reactivity in postpartum women. Psychoneuroendocrinology 55:164–172
Crowley SK, O’Buckley TK, Schiller CE, Stuebe A, Morrow AL, Girdler SS (2016) Blunted neuroactive steroid and HPA axis responses to stress are associated with reduced sleep quality and negative affect in pregnancy: a pilot study. Psychopharmacology 233(7):1299–1310
Deligiannidis KM, Sikoglu EM, Shaffer SA, Frederick B, Svenson AE, Kopoyan A, Kosma CA, Rothschild AJ, Moore CM (2013) GABAergic neuroactive steroids and resting-state functional connectivity in postpartum depression: a preliminary study. J Psychistr Res 47(6):816–828
Deligiannidis KM, Kroll-Desrosiers AR, Mo S, Nguyen HP, Svenson A, Jaitly N, Hall JE, Barton BA, Rothschild AJ, Shaffer SA (2016) Peripartum neuroactive steroid and γ-aminobutyric acid profiles in women at-risk for postpartum depression. Psychoneuroendocrinology 70:98–107
Epperson CN, Haga K, Mason GF, Sellers E, Gueorguieva R, Zhang W, Weiss E, Rothman DL, Krystal JH (2002) Cortical γ-aminobutyric acid levels across menstrual cycle in healthy women and those with premenstrual dysphoric disorder: a proton magnetic resonance spectroscopy study. Arch Gen Psychiatry 59(9):851–858
Eser D, Schule C, Baghai TC, Romeo E, Rupprecht R (2006) Neuroactive steroids in depression and anxiety disorders: clinical studies. Neuroendocrinology 84(4):244–254
Fatemi SH, Folsom TD, Rooney RJ, Thuras PD (2013) Expression of GABAA a2-, b1- and ε-receptors are altered significantly in the lateral cerebellum of subjects with schizophrenia, major depression and bipolar disorder. Transl Psychiatry 3:e303
Forty L, Jones L, Jones I, Caesar S, Cooper C, Hough A, Dean L, Dave S, Farmer A, McGuffin P, Brewster S, Craddock N, Jones I (2006) Familiality of postpartum depression in unipolar disorder: results of a family study. Am J Psychiatry 163(9):1549–1553
Genazzani AD, Petraglia F, Bernardi F, Casarosa E, Salvestroni C, Tonetti A, Nappi RE, Luisi S, Palumbo M, Purdy RH, Luisi M (1998) Circulating levels of allopregnanolone in humans: gender, age and endocrine influences. J Clin Endocrinol Metab 83(6):2099–2103
Gilbert Evans SE, Ross LE, Sellers EM, Purdy RH, Romach MK (2005) 3alpha-reduced neuroactive steroids and their precursors during pregnancy and the postpartum period. Gynecol Endocrinol 21(5):268–279
Girdler SS, Straneva PA, Light KC, Pedersen CA, Morrow AL (2001) Allopregnanolone levels and reactivity to mental stress in premenstrual dysphoric disorder. Biol Psychiatry 49(9):788–797
Gjerdingen D, Crow S, McGovern P, Miner M, Center B (2011) Changes in depressive symptoms over 0–9 months postpartum. J Women's Health 20(3):381–386
Gordon JL, Girdler SS, Meltzer-Brody SE, Stika CS, Thurston RC, Clark CT, Prairie BA, Moses-Kolko E, Joffe H, Wisner KL (2015) Ovarian hormone fluctuation, neurosteroids, and HPA axis dysregulation in perimenopausal depression: a novel heuristic model. Am J Psychiatry 172(3):227–236
Gotlib IH, Whiffen VE, Mount JH, Cordy NI (1989) Prevalence rates and demographic characteristics associated with depression in pregnancy and postpartum. J Consult Clin Psychol 57(2):269–274
Gulinello M, Smith SS (2003) Anxiogenic effects of neurosteroid exposure: sex differences and altered GABAA receptor pharmacology in adult rats. J Pharmacol Exp Ther 305(2):541–548
Gulinello M, Gong QH, Li X, Smith SS (2001) Short-term exposure to a neuroactive steroid increases α4 GABAA receptor subunit levels in association with increased anxiety in the female rat. Brain Res 910:55–66
Hellgren C, Akerud H, Skalkidou A, Bäckström T, Sundström-Poromaa I (2014) Low serum allopregnanolone is associated with symptoms of depression in late pregnancy. Neuropsychobiology 69(3):147–153
Howie PW, McNeilly AS (1982) Breastfeeding and postpartum ovulation. IPPF Med Bull 16(2):1–3
Hoyt LT, Falconi A (2015) Puberty and perimenopause: reproductive transitions and their implications for women’s health. Soc Sci Med 132:103–112
Jones I, Cantwell R (2010) The classification of perinatal mood disorders—suggestions for DSMV and ICD11. Arch Womens Ment Health 13:33–36
Kanes S, Colquhoun H, Gunduz-Bruce H, Raines S, Arnold R, Schacterle A, Doherty J, Epperson CN, Deligiannidis KM, Riesenberg R, Hoffmann E, Rubinow D, Jonas J, Paul S, Meltzer-Brody S (2017) Brexanolone (SAGE-547 injection) in post-partum depression: a randomised controlled trial. Lancet 390:480–489
Kimmel M, Clive M, Gispen F, Guintivano J, Brown T, Cox O, Beckmann MW, Kornhuber J, Fasching PA, Osborne LM, Binder E, Payne JL, Kaminsky Z (2016) Oxytocin receptor DNA methylation in postpartum depression. Psychoneuroendocrinology 69:150–160
Klatzkin RR, Morrow AL, Light KC, Pedersen CA, Girdler SS (2006) Associations of histories of depression and PMDD diagnosis with allopregnanolone concentrations following the oral administration of micronized progesterone. Psychoneuroendocrinology 31(10):1208–1219
Kothari C, Wiley J, Moe A, Liepman MR, Tareen RS, Curtis A (2016) Maternal depression is not just a problem early on. Public Health 137:154–161
Lawrie TA, Hofmeyr GJ, De Jager M, Berk M, Paiker J, Viljoen E (1998) A double-blind randomized placebo controlled trial of postnatal norethisterone enanthate: the effect on postnatal depression and serum hormones. Br J Obstet Gynecol 105(10):1082–1090
Lombardi I, Luisi S, Quirici B, Monteleone P, Bernardi F, Liut M, Casarosa E, Palumbo M, Petraglia F, Genazzani AR (2004) Adrenal response to adrenocorticotropic hormone stimulation in patients with premenstrual syndrome. Gynecol Endocrinol 18(2):79–87
Luisi S, Petraglia F, Benedetto C, Nappi RE, Bernardi F, Fadalti M, Reis FM, Luisi M, Genazzani AR (2000) Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients. J Clin Endocrinol Metab 85(7):2429–2433
MacKenzie G, Maguire J (2014) The role of ovarian hormone-derived neurosteroids on the regulation of GABAA receptors in affective disorders. Psychopharmacology 231(17):3333–3342
Maguire J, Mody I (2008) GABA(A)R plasticity during pregnancy: relevance to postpartum depression. Neuron 59(2):207–213
Martinez PE, Rubinow DR, Nieman LK, Koziol DE, Morrow AL, Schiller CE, Cintron D, Thompson KD, Khine KK, Schmidt PJ (2016) 5α-Reductase inhibition prevents the luteal phase increase in plasma allopregnanolone levels and mitigates symptoms in women with premenstrual dysphoric disorder. Neuropsychopharmacology 41(4):1093–1102
Melon LC, Hooper A, Yang X, Moss SJ, Maguire J (2017) Inability to suppress the stress-induced activation of the HPA axis during the peripartum period engenders deficits in postpartum period engenders deficits in postpartum behaviors in mice. Psychoneuroendocrinology 12:003
Misri S, Sinclair D, Kuan A (1997) Breast-feeding and postpartum depression: is there a relationship? Can J Psychiatr 42(10):1061–1065
Monteleone P, Luisi S, Tonetti A, Bernardi F, Genazzani AD, Luisi M, Petraglia F, Genazzani AR (2000) Allopregnanolone concentrations and premenstrual syndrome. Eur J Endocrinol 142(3):269–273
Munk-Olsen T, Munk Laursen T, Bøcker Pedersen C, Mors O, Bo Mortensen P (2006) New parents and mental disorders; a population-based register study. JAMA 296(21):2582–2589
Osborne LM, Gispen F, Sanyal A, Yenokyan G, Meilman S, Payne JL (2017) Lower allopregnanolone during pregnancy predicts postpartum depression: an exploratory study. Psychoneuroendocrinology 79:116–121
Payne J, Palmer JT, Joffe H (2009) A reproductive subtype of depression: conceptualizing models and moving toward etiology. Harv Rev Psychiatry 17(2):72–86
Pearlstein T, Yonkers KA, Fayyad R, Gillespie JA (2005) Pretreatment pattern of symptom expression in premenstrual dysphoric disorder. J Affect Disord 85(3):275–282
Rapkin AJ, Morgan M, Goldman L, Brann DW, Simone D, Mahesh VB (1997) Progesterone metabolite allopregnanolone in women with premenstrual syndrome. Obstet Gynecol 90(5):709–714
Romeo E, Strohle A, Spalletta G, di Michele F, Hermann B, Holsboer F, Pasini A, Rupprecht R (1998) Effects of antidepressant treatment on neuroactive steroids in major depression. Am J Psychiatry 155(7):901–913
Roomruangwong C, Anderson G, Berk M, Stoyanov D, Carvalho AF, Maes M (2018) A neuro-immune, neuro-oxidative and neuro-nitrosative model of prenatal and postpartum depression. Prog Neuro-Psychopharmacol Biol Psychiatry 81:262–274
Schiller CE, Schmidt PJ, Rubinow DR (2014) Allopregnanolone as a mediator of affective switching in reproductive mood disorders. Psychopharmacology 231(17):3557–3567
Schiller CE, Meltzer-Brody S, Rubinow DR (2015) The role of reproductive hormones in postpartum depression. CNS Spectr 20(1):48–59
Schmidt PJ, Purdy RH, Moore PH Jr, Paul SM, Rubinow DR (1994) Circulating levels of anxiolytic steroids in the luteal phase in women with premenstrual syndrome in control subjects. J Clin Endocrinol Metab 79(5):1256–1260
Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR (1998) Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med 338(4):209–216
Schüle C, Romeo E, Uzunov DP, Eser D, di Michele F, Baghai TC, Pasini A, Schwarz M, Kempter H, Rupprecht R (2006) Influence of mirtazapine on plasma concentrations of neuroactive steroids in major depression and on 3α-hydroxysteroid dehydrogenase activity. Mol Psychiatry 11(3):261–272
Schüle C, Baghai TC, di Michele F, Eser D, Pasini A, Schwarz M, Rupprecht R, Romeo E (2007) Effects of combination treatment with mood stabilizers and mirtazapine on plasma concentrations of neuroactive steroids in depressed patients. Psychoneuroendocrinology 32(6):669–680
Schüle C, Nothdurfter C, Rupprecht R (2014) The role of allopregnanolone in depression and anxiety. Prog Neurobiol 113:79–87
Shaaban MM, Sayed GH, Ghaneimah SA (1987) The recovery of ovarian function during breastfeeding. J Steroid Biochem 27(4–6):1043–1052
Sharma V, Corpse C (2008) Case study revisiting the association between breastfeeding and postpartum depression. J Hum Lact 24(1):77–79
Shen H, Gong QH, Yuan M, Smith SS (2005) Short-term steroid treatment increases delta GABAA receptor subunit expression in rat CA1 hippocampus: pharmacological and behavioral effects. Neuropharmacology 49(5):573–586
Shen H, Gong QH, Aoki C, Yuan M, Ruderman Y, Dattilo M, Williams K, Smith SS (2007) Reversal of neurosteroid effects at α4β2δ GABAA receptors triggers anxiety at puberty. Nat Neurosci 10(4):469–477
Smith SS, Ruderman Y, Frye C, Homanics G, Yuan M (2006) Steroid withdrawal in the mouse results in anxiogenic effects of 3alpha,5beta-THP: a possible model of premenstrual dysphoric disorder. Psychopharmacology 186(3):323–333
Smith AS, Tabbaa M, Lei K, Eastham P, Butler MJ, Linton L, Altshuler R, Liu Y, Wang Z (2016) Local oxytocin tempers anxiety by activating GABAA receptors in the hypothalamic paraventricular nucleus. Psychoneuroendocrinology 63:50–58
Soyka M, Preuss UW, Hesselbrock V, Zill P, Koller G, Bondy B (2008) GABA-A2 receptor subunit gene (GABRA2) polymorphisms and risk for alcohol dependence. J Psychiatr Res 42(3):184–191
Stowe ZN, Hostetter AL, Newport DJ (2004) The onset of postpartum depression: implications for clinical screening in obstetrical and primary care. Am J Obstet Gynecol 192(2):522–526
Strauss JF, Barbieri RL (eds) (2014) Yen & Jaffe’s reproductive endocrinology: physiology, pathophysiology, and clinical management. Elsevier/Saunders, Philadelphia
Ströhle A, Romeo E, Hermann B, Pasini A, Spalletta G, di Michele F, Holsboer F, Rupprecht R (1999) Concentrations of 3α-reduced neuroactive steroids and their precursors in plasma of patients with major depression and after clinical recovery. Biol Psychiatry 45(3):274–277
Ströhle A, Romeo E, diMichele F et al (2003) Induced panic attacks shift gamma-aminobutyric acid type A receptor modulatory neuroactive steroid composition in patients with panic disorder: preliminary results. Arch Gen Psychiatry 60:161–168
Susman V, Katz J (1988) Weaning and depression: another postpartum complication. Am J Psychiatr 145(4):498–501
Uzunova V, Sheline Y, Davis JM, Rasmusson A, Uzunov DP, Costa E, Guidotti A (1998) Increase in the cerebrospinal fluid content of neurosteroids in patients with unipolar major depression who are receiving fluoxetine or fluvoxamine. Proc Natl Acad Sci 95(6):3239–3244
Viktorin A, Meltzer-Brody S, Kuja-Halkola R, Sullivan PF, Landén M, Lichtenstein P, Magnusson PK (2016) Heritability of perinatal depression and genetic overlap with nonperinatal depression. Am J Psychiatr 173(2):158–165
Wang M (2011) Neurosteroids and GABA-A receptor function. Front Endocrinol (Lausanne) 2:44
Wang M, Seippel L, Purdy RH, Backstrom T (1996) Relationship between symptom severity and steroid variation in women with premenstrual syndrome: study on serum pregnenolone, pregnenolone sulfate, 5α-pregnane-3,20-dione and 3α-hydroxy-5α-pregnan-20-one. J Clin Endocrinol Metab 81(3):1076–1082
Wieland S, Lan NC, Mirasedeghi S, Gee KW (1991) Anxiolytic activity of the progesterone metabolite 5β-pregnan-3α-ol-20-one. Brain Res 565(2):263–268
Windle RJ, Wood SA, Kershaw YM, Lightman SL, Ingram CD (2013) Adaptive changes in basal and stress-induced HPA activity in lactating and post-lactating female rats. Endocrinology 154(2):749–761
Zhang K, Pollack S, Ghods A, Dicken C, Isaac B, Adel G, Zeitlan G, Santoro N (2008) Onset of ovulation after menarche in girls: a longitudinal study. J Clin Endocrinol Metab 93(4):1186–1194
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Burke, C.S., Susser, L.C. & Hermann, A.D. GABAA dysregulation as an explanatory model for late-onset postpartum depression associated with weaning and resumption of menstruation. Arch Womens Ment Health 22, 55–63 (2019). https://doi.org/10.1007/s00737-018-0871-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-018-0871-9