Abstract
Women’s lack of knowledge on symptoms of perinatal depression and treatment resources is a barrier to receiving care. We sought to estimate the prevalence and predictors of discussing depression with a prenatal care provider. We used the 2011 population-based data from 24 sites participating in the Pregnancy Risk Assessment Monitoring System (n = 32,827 women with recent live births) to examine associations between maternal characteristics and report that a prenatal care provider discussed with her what to do if feeling depressed during or after pregnancy. Overall, 71.9 % of women reported discussing perinatal depression with their prenatal care provider (range 60.7 % in New York City to 85.6 % in Maine). Women were more likely to report a discussion on perinatal depression with their provider if they they were 18-29years of age than over 35 years of age compared to older (adjusted prevalence ratio [aPR] 18 to 19 y = 1.08, 20 to 24 y = 1.10, 25 to 29 y = 1.09), unmarried (aPR = 1.07) compared to married, had <12 years of education (aPR = 1.05) compared to >12 years, and had no previous live births (aPR = 1.03) compared to ≥1 live births. Research is needed on effective ways to educate women about perinatal depression and whether increased knowledge on perinatal depression results in higher rates of treatment and shorter duration of symptoms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prenatal and postpartum depression affects approximately 8–14 % of US women (Gaynes et al. 2005; Ko et al. 2012; Wisner et al. 2013). However, fewer than half of these women receive treatment for their depressive symptoms (Ko et al. 2012). US women experience many barriers to the diagnosis and treatment of perinatal depression, one of which is the lack of knowledge about the signs and symptoms of depression and when and where to seek help (Byatt et al. 2013; Flynn et al. 2010; Ko et al. 2012). To reduce barriers related to knowledge, five US states (VA 2003, TX 2003/2005, NJ 2006, MN 2010/2012, OR 2011) have enacted mandates on education for prenatal and postpartum depression, either alone or in conjunction with awareness campaigns and mandates on universal screening for perinatal depression (Rhodes and Segre 2013). The educational mandates require providers who care for pregnant or postpartum women to provide information about depression to their patients. In the USA, approximately 71 % of pregnant women receive early and adequate prenatal care, allowing for multiple opportunities for prenatal education on depression (http://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives?topicId=26).
Pregnant and postpartum women desire information on how to gauge the severity of their symptoms and when and where to seek treatment (Byatt et al. 2013; Flynn et al. 2010). Discussion of depression and treatment options with a health care provider may facilitate earlier entry into care and continuity of treatment (Byatt et al. 2012). However, little is known about how often these discussions occur and whether clinicians provide universal education to their patients or target specific women with risk factors for depression. A survey conducted among obstetric nurse managers in 87 Ohio hospitals found that approximately 90 % of participating hospitals educate women about postpartum depression at the delivery hospitalization (Garg et al. 2005). The authors also reported that first-time mothers and those with more risk factors for depression were more likely to receive education on postpartum depression. However, to our knowledge, there are no population-based estimates from other states on the percentage of women who receive prenatal education on depression from their provider and how those estimates differ by maternal characteristics. This information is needed to determine the unmet need for education on perinatal depression, especially as more states enact educational mandates. Therefore, using population-based data from US women with recent live births, we examined the self-reported prevalence of receipt of prenatal education on depression from a prenatal care provider and whether prevalence differs by maternal characteristics.
Materials and methods
Data source
We used the 2011 data from the Pregnancy Risk Assessment Monitoring System (PRAMS), a surveillance project of US state and New York Cityhealth departments and the Centers for Disease Control and Prevention (www.cdc.gov/PRAMS). Annually, a stratified sample of women with recent live births is mailed a questionnaire about their experiences before, during, and after pregnancy. Survey data are linked to birth certificate records and weighted to produce population-based estimates. More information on the PRAMS methodology can be found online (http://www.cdc.gov/prams/methodology.htm). In 2011, 24 sites participated in PRAMS and had response rates ≥65 %, the PRAMS threshold for reporting data.
Measures
To assess prevalence of receipt of prenatal education on depression, all PRAMS participants were asked, “During any of your prenatal care visits, did a doctor, nurse, or other health care worker talk with you about what to do if you feel depressed during your pregnancy or after your baby is born?” The question assessed active education (a discussion with a health care provider), as opposed to passive education (receipt of written materials). The question does not ascertain information on who initiated the discussion.
To examine what subgroups of women may be more likely to receive prenatal education on depression, we assessed prevalence of receipt of such education by maternal demographic characteristics, Medicaid insurance for prenatal care and/or delivery, number of prenatal care visits attended, number of prenatal stressful life events, smoking status during pregnancy, and state/site of residence. The number of prenatal stressful life events was based on women’s responses to 13 questions assessing stressful experiences in the 12 months before delivery, such as separation or divorce, job loss, and homelessness. PRAMS also assesses women’s postpartum depressive symptoms by asking women if they have felt (1) down, depressed, or sad; (2) hopeless; or (3) slowed down since their new baby was born. Possible responses (and associated numerical values) were never (1), rarely (2), sometimes (3), often (4), or always (5). The values of the three responses were summed. Women with scores of ≥10 were considered to have postpartum depressive symptoms; this algorithm has a sensitivity of 57 % and specificity of 87 % compared to a structured clinical interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (O’Hara et al. 2012).
Procedures
Initially, we examined maternal characteristics for the entire sample. We examined prevalence of receipt of active prenatal education on depression overall and by site. We also used the average marginal prediction approach to logistic regression (Bieler et al. 2010) to generate adjusted prevalence ratios (aPRs) and 95 % confidence intervals (CIs) of women’s report that their prenatal care provider discussed depression with them, by each maternal characteristic. In addition, we calculated receipt of prenatal education on depression by women’s report of postpartum depressive symptoms. All survey participants receive information about the surveillance system and provide their consent before completing the survey. The Centers for Disease Control and Prevention’s Institutional Review Board has approved the PRAMS protocol and use of de-identified data by investigators for secondary analyses. All analyses were conducted in SUDAAN (RTI International, Research Triangle Park, NC) to account for sampling design, and appropriate weights were used to generate population estimates.
Results
Sample
In 2011, 33,715 US women participated in PRAMS from the 24 sites (23 states and New York City) that met the PRAMS response threshold for reporting data. Of these women, 32,827 (97.4 %) had information on receipt of prenatal education on depression, 27,907 (85.0 %) of whom had information on all other maternal characteristics and were included in the multivariable model. The largest percentage of women excluded from the multivariable model (5.5 %) were missing data on Medicaid insurance (publicly funded insurance based on poverty level) during prenatal care or delivery. Women excluded from the multivariable model were more likely to be younger than 18 years, non-Hispanic black or Hispanic, and unmarried and have less than 12 years of education and fewer than nine prenatal care visits (p < 0.05 for all).
The majority of women in our analytic sample were between 20 and 34 years of age, were white, were married, had more than a high school education, had more than one previous live birth, had nine or more prenatal care visits, experienced two or fewer stressful life events during pregnancy, and were nonsmokers (Table 1). Approximately half (49.2 %) were Medicaid recipients.
Prevalence
Overall, 71.9 % of women reported that their prenatal care provider discussed with them what to do if they felt depressed during pregnancy or after their child was born. However, prevalence varied significantly by site and ranged from 60.7 % in New York City to 85.6 % in Maine (Table 2). Prevalence of receipt of prenatal education on depression was 81.6 % in MN, 69.5 % in NJ, and 79.3 % in OR, three of the five states with educational mandates.
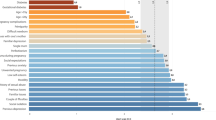
Prevalence of receipt of prenatal education on depression varied significantly by all maternal characteristics examined (chi-square p < 0.05 for all), except number of stressful life events experienced during pregnancy (Table 3). However, in all subgroups examined, prevalence estimates were above 60 %, and the differences between subgroups were not large (range 63.1 to 78.8 %). Women with the highest point prevalence of reporting that their prenatal care provider discussed perinatal depression with them were 18 to 19 years old (78.8 %), unmarried (76.9 %), and younger than 18 years of age (75.7 %). Women with the lowest point prevalence of reporting a discussion with their provider on perinatal depression were Asians/Pacific Islanders (63.1 %), 35 years or older (65.4 %), and not covered by Medicaid insurance (68.7 %). In the multivariable model, women aged 18 to 19 (adjusted prevalence ratio [aPR] = 1.08), 20 to 24 (aPR = 1.10), and 25 to 29 (aPR = 1.09), compared to women aged 35 years or older, were more likely to report a discussion on perinatal depression with their provider. Additionally, unmarried women (aPR = 1.07) compared to married women, those with less than 12 years of education (aPR = 1.05) compared with more than 12 years, and women with no previous live births (aPR = 1.03) compared to one or more previous live births were more likely to report a discussion on perinatal depression with their provider. Asians/Pacific Islanders (aPR = 0.91), compared to non-Hispanic white women, and women with eight or fewer prenatal care visits (aPR = 0.95), compared with 12 or more visits, were less likely to report a discussion on perinatal depression with their provider. Additionally, of women who screened positive for postpartum depressive symptoms, 67.5 % reported that their prenatal care provider discussed perinatal depression with them (Fig. 1). Rates of postpartum depressive symptoms ranged from 8.0 to 13.5 % for all subgroups of women (data not shown).
Discussion and conclusion
We found that nearly three quarters of women reported that their prenatal care providers discussed with them what to do if they feel depressed during or after pregnancy. A slightly higher percentage of younger age, unmarried, less-educated, nulliparous women reported that their prenatal care provider discussed depression with them. Older women, Asians/Pacific Islanders, married women, those with more education, and those with a previous live birth were slightly less likely to report discussing perinatal depression with their provider. We also found that, of women who screened positive for postpartum depressive symptoms, approximately one third reported that their prenatal care provider did not discuss perinatal depression with them.
It is difficult to compare our results to other published reports due to the small number of studies on the topic and different methodologies. To our knowledge, only three published studies have assessed prevalence of patient education on perinatal depression (Farr et al. 2014; Garg et al. 2005; Logsdon et al. 2010). Dates of data collection were not reported for two studies (Garg et al. 2005; Logsdon et al. 2010). One study among obstetric nurse managers at Ohio hospitals reported that 90 % of hospitals provided education on postpartum depression, most commonly at hospitalization after delivery (Garg et al. 2005). The nursing staff and attending obstetricians most commonly educated women on postpartum depression. However, only 28 % of hospitals reported direct education (provider communication), as opposed to 55 % reporting passive education (distribution of written materials). Similar to our findings, women with signs of depression and those with more risk factors were more likely to receive education on depression. Another study among 43 hospital-based perinatal nurses from a single suburban hospital in the southern USA found that 25 % of the sample reported teaching new mothers about postpartum depression always or most of the time (Logsdon et al. 2010). However, the response rate was only 29 %. The third study was an analysis of the 2009–2010 New Jersey PRAMS data from hospitals providing depression screening results to the New Jersey Department of Health (Farr et al. 2014). Among women with depression screening results, 67 % reported discussing depression with their prenatal care provider.
Three states in our analysis have mandates to educate women on perinatal depression (Rhodes and Segre 2013). New Jersey’s law was passed in 2006 and mandated that “professionals providing prenatal care to women shall provide education to women and their families about postpartum depression.” The Minnesota law was passed in 2010 to develop educational materials on postpartum depression; in 2012, the legislature amended the bill to require dissemination of the materials to pregnant women. Oregon’s law, enacted in 2011, requires the development of training and informational materials on postpartum depression and their dissemination to new mothers before hospital discharge. Our data are from 2011, and the PRAMS survey question specifically asks about a prenatal care provider discussing depression with the woman, rather than educating the woman in other ways (e.g., written materials). Therefore, the results reported here cannot be used to evaluate baseline levels or implementation of these laws, although it is possible that these laws may increase direct communication about perinatal depression between patients and providers.
Based on our results, clinicians may be targeting discussions on perinatal depression toward new mothers and those who may be disadvantaged (younger, unmarried, and less-educated women). Approximately a third of women who were over 35 years of age, Asians/Pacific Islanders, married, with more education, and with a previous live birth reported not discussing perinatal depression with their provider. Although these women have a slightly lower risk of experiencing postpartum depression than their counterparts, 8 to 10 % reported postpartum depressive symptoms. While clinical judgment is an important tool, all women may benefit from understanding the signs and symptoms of depression and where to seek care, when needed.
Studies have shown that lack of patient education about perinatal depression and where to seek care is a barrier to women’s engagement in mental health treatment (Byatt et al. 2013; Ko et al. 2012). Pregnant and postpartum women desire information on how to gauge severity of their symptoms and when and where to seek treatment (Flynn et al. 2010). Discussion of depression and treatment options with a health care provider may facilitate earlier entry into care and continuity of treatment (Byatt et al. 2012). However, providers may not discuss perinatal depression with their patients because of lack of time, knowledge, or resources or because of a perception that women do not want help (Byatt et al. 2013; Byatt et al. 2012). Provider training on perinatal depression assessment, diagnosis, and treatment options, along with educational resources for women, may encourage more patient-provider dialogue. More knowledge about perinatal depression, coupled with other effective interventions, may increase treatment for women in need.
Our study has several limitations. We do not know whether women received information about perinatal depression in other formats or from someone other than their prenatal care provider. We also do not know whether the provider or the woman initiated the conversation or when during prenatal care it occurred (e.g., if it occurred after screening positive for depression). Women are surveyed at 2 to 9 months postpartum and may not accurately recall the discussions they had with their prenatal care provider. Additionally, we excluded from the multivariable model 888 women with missing information on whether the woman’s provider discussed depression with her and an additional 4920 women with missing data on other variables of interest. Included and excluded women differed with respect to maternal characteristics; however, similar percentages reported that their prenatal care provider discussed depression with them (included 72 %, excluded 71 %). Because of the sensitivity and specificity of 57 and 87 %, respectively, for the PRAMS algorithm on postpartum depressive symptoms, a positive screen cannot be interpreted as a clinical diagnosis of postpartum depression. Despite these limitations, this is the first population-based study to examine prevalence of receipt of prenatal education on depression in multiple states and New York City and how prevalence differs by site and maternal characteristics.
In summary, we found that most women with recent live births from 23 states and New York City reported that their prenatal care provider discussed what to do if they felt depressed during pregnancy or after delivery. However, almost one third of women with postpartum depressive symptoms did not report such a discussion. Research is needed to understand whether educating pregnant and postpartum women about perinatal depression and where to seek care increases treatment rates and decreases symptom duration. To that end, prenatal care providers may need further training about the signs and symptoms of depression and information about local mental health resources, so that they can provide complete information to their patients.
References
Bieler GS, Brown GG, Williams RL, Brogan DJ (2010) Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol 171:618–623
Byatt N, Biebel K, Lundquist RS, Moore Simas TA, Debordes-Jackson G, Allison J, Ziedonis D (2012) Patient, provider, and system-level barriers and facilitators to addressing perinatal depression. J Reprod Infant Psychol 30:436–449
Byatt N, Biebel K, Friedman L, Debordes-Jackson G, Ziedonis D, Pbert L (2013) Patient’s views on depression care in obstetric settings: how do they compare to the views of perinatal health care professionals? Gen Hosp Psychiatry 35:598–604
Farr SL, Denk CE, Dahms EW, Dietz PM (2014) Evaluating universal education and screening for postpartum depression using population-based data. J Women’s Health (Larchmt) 23:657–663
Flynn HA, Henshaw E, O’Mahen H, Forman J (2010) Patient perspectives on improving the depression referral processes in obstetrics settings: a qualitative study. Gen Hosp Psychiatry 32:9–16
Garg A, Morton S, Heneghan A (2005) A hospital survey of postpartum depression education at the time of delivery. J Obstet Gynecol Neonatal Nurs 34:587–594
Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC (2005) Perinatal depression: prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ)1-8
Ko JY, Farr SL, Dietz PM, Robbins CL (2012) Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health (Larchmt) 21:830–836
Logsdon MC, Foltz MP, Scheetz J, Myers JA (2010) Self-efficacy and postpartum depression teaching behaviors of hospital-based perinatal nurses. J Perinat Educ 19:10–16
O’Hara MW, Stuart S, Watson D, Dietz PM, Farr SL, D’Angelo D (2012) Brief scales to detect postpartum depression and anxiety symptoms. J Women’s Health (Larchmt) 21:1237–1243
Rhodes AM, Segre LS (2013) Perinatal depression: a review of US legislation and law. Arch Womens Ment Health 16:259–270
Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH (2013) Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 70:490–498
Conflict of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Farr, S.L., Ko, J.Y., Burley, K. et al. Provider communication on perinatal depression: a population-based study. Arch Womens Ment Health 19, 35–40 (2016). https://doi.org/10.1007/s00737-014-0493-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-014-0493-9