Abstract
l-Arginine (Arg) is the enzymatic precursor of nitric oxide (NO) which has multiple biological functions. Asymmetric dimethylarginine (ADMA) and symmetric dimethylarginine (SDMA) are endogenous inhibitors of NO. We hypothesized that the ADMA and SDMA have additional biological functions in pregnancy, beyond NO synthesis, and may play a role in the regulation of birthweight (BW). To investigate this issue, we measured the plasma concentration of ADMA, SDMA, Arg and the NO metabolites nitrite and nitrate, at 23–25 weeks of gestation in women with normal placental function (Group 1) and in women with impaired placental perfusion; 19 of these women had normal outcome (Group 2), 14 had a fetus that was growth restricted (Group 3), and 10 women eventually developed preeclampsia (Group 4). BW percentile was found to inversely correlate with maternal plasma ADMA concentration in Group 3 (r = − 0.872, P < 0.001) and in Group 4 (r = − 0.800, P < 0.05). But, BW percentile did not correlate with the maternal plasma concentration of Arg, SDMA, nitrate or nitrite. Our results suggest that maternal plasma ADMA concentration is an important indicator of fetal growth restriction in women with impaired placental perfusion independent of NO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
l-Arginine (Arg) is the physiological substrate of nitric oxide (NO) synthase (NOS), whereas asymmetric dimethylarginine (ADMA) and symmetric dimethylarginine (SDMA) are endogenous inhibitors of NOS activity (Tsikas et al. 2000a, b). The increased generation of the potent vasodilator NO by the maternal endothelium is considered a major player in pregnancy (Williams et al. 1997). Failure of normal trophoblastic invasion and re-modeling of the uterine spiral arteries is thought to lead to a high-resistance utero-placental circulation. This abnormal placental function can lead to the development of PE and fetal growth restriction (FGR), that can be detected non-invasively by a Doppler examination of the maternal uterine arteries at 23–25 weeks’ gestation (Albaiges et al. 2000). A deficiency of maternal NO is considered important in the development of PE (Cockell and Poston 1997).
Most studies reported elevated maternal concentrations of ADMA, but not of SDMA, in women that are destined to develop preeclampsia (PE) later on in the pregnancy (Savvidou et al. 2003; Speer et al. 2008; Laskowska et al. 2011, 2015; Khalil et al. 2013; López-Alarcón et al. 2015; Gumus et al. 2016; Yuan et al. 2017). Furthermore, maternal plasma concentration of ADMA, but not of SDMA, correlated inversely with maternal endothelial function, as assessed by brachial flow-mediated dilation (FMD), suggesting ADMA as a possible causative factor for PE (Savvidou et al. 2003). Even after 10 years following the pregnancy complicated by PE, maternal levels of ADMA were found to be elevated in women that had PE together with a small for gestational age (SGA) offspring (Sandvik et al. 2013). Some studies investigated the relationship between umbilical cord ADMA levels and neonatal birthweight (BW) and found that circulating ADMA was significantly higher in SGA and large for gestational age (LGA) compared to the appropriate for gestational age (AGA) neonates (Chiavaroli et al. 2014). Yet, correlations between circulating ADMA concentration and BW in SGA, LGA or AGA neonates have not been reported in that study. More recently, a relationship was found between BW and umbilical cord plasma ADMA which followed a U-shape curve (Takaya et al. 2017). With respect to preterm neonates, currently there is no consensus regarding the relationship between circulating ADMA, SDMA, Arg concentrations and BW (Richir et al. 2008; Moonen et al. 2014; Vida et al. 2009; Buck et al. 2017). Interestingly, in young adults (age 17–29 years) born preterm at extremely low birth weight (< 1000 g), plasma ADMA concentration was found to correlate inversely with their BW (Bassareo et al. 2012).
ADMA and SDMA are cardiovascular risk factors/markers in adults (Schlesinger et al. 2016; Emrich et al. 2017; Zobel et al. 2017). ADMA’s cardiovascular risk is generally considered to be due to its inhibitory action of endothelial NOS (eNOS) activity. However, the half-maximal inhibitory concentration (IC50) of ADMA towards eNOS is almost 25 times higher compared to plasmatic and cellular ADMA concentrations (Tsikas 2017). Furthermore, SDMA is even less potent than ADMA towards NOS activity (Tsikas et al. 2000a). Therefore, the cardiovascular risks arising from ADMA and notably from SDMA are hard to be explained by their inhibitory action of NOS and point out to the additional, NO-independent, not yet recognized activities of ADMA and SDMA. Circulating ADMA and SDMA are considered to derive exclusively from the Arg residues in certain proteins which are methylated on their guanidine (N G) group by protein arginine methyltransferases (PRMT) (Morales et al. 2016). Proteolysis of such N G-methylarginine proteins is thought to release ADMA and/or SDMA which can inhibit NOS activity in endothelial cells, thus leading to cardiovascular disease, in other types of cells such as in neurons, thus contributing to other types of disease. The biological activities of N G-methylarginine proteins have been poorly investigated until now. We have hypothesized that ADMA, SDMA, Arg and N G-methylarginine proteins may be involved in fetal growth in a manner independent of NO.
In the present study, we addressed this hypothesis and re-examined the data reported in a previous study on women with normal or impaired placental function (Savvidou et al. 2003). We especially tested the potential correlations between maternal plasma ADMA, SDMA and Arg concentrations at mid-pregnancy and neonatal BW percentile. From the same population, we also reported the maternal plasma nitrate and nitrite levels.
Materials and methods
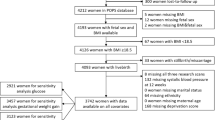
The original population of the study has been described in our previous publication (Savvidou et al. 2003) (Table 1). In summary, we had included 43 pregnant women with normal placental perfusion, as assessed by uterine artery Doppler examination (Group 1) and 43 women with abnormal placental perfusion, as defined by the presence of early diastolic notch bilaterally in the uterine artery Doppler waveforms, at 23–25 weeks of gestation. None of the women in Group 1 developed PE and all of them delivered a phenotypically normal, appropriate for gestational age neonate. The latter group was subdivided into three subgroups; Group 2 consisted of 19 women with abnormal placental perfusion but normal outcome, Group 3 comprised 14 women with abnormal uterine artery Doppler examination who subsequently delivered a growth restricted baby. Group 4 consisted of ten women who had abnormal uterine artery Doppler waveform and subsequently developed PE (Davey and MacGillivray 1988). The study was approved by the King’s College Hospital (London, UK) Ethics Committee (98-306), and all the patients gave written informed consent. BW percentiles were calculated after adjustment for gestational age at delivery (Poon et al. 2012). Amino acids were analyzed simultaneously in 0.5-mL plasma aliquots by HPLC with fluorescence detection as o-phthaldialdehyde derivatives (Tsikas et al. 1998). Nitrite and nitrate in maternal plasma were measured by GC–MS (Tsikas 2000).
Data distribution was evaluated by the D’Agostino and Pearson omnibus K2 normality tests. The non-parametric Mann–Whitney test was used for the not normally distributed variables and these data are presented as median [interquartile range]. Normally distributed variables were analyzed by Student’s unpaired t test and these data are reported as mean ± standard deviation. Correlation of circulating biochemical parameters with other parameters was assessed using the Pearson (normally distributed variables) or Spearman (not normally distributed variables) correlation coefficients. GraphPad Prism 5 was used for statistical analyses and preparation of figures. Two-tailed P values < 0.05 were considered as statistically significant.
Results
Maternal plasma concentrations of biomarkers and pregnancy outcomes
The clinical characteristics of pregnant women and their ADMA, SDMA, Arg, nitrite and nitrate plasma concentrations are summarized in Table 1 (Savvidou et al. 2003).
As expected, the BW percentile of the women who developed PE or had a small baby (i.e., Groups 3 and 4) was lower compared to the women with normal outcome (i.e., Groups 1 and 2). Women who had a small baby had to be delivered earlier than all the other groups. In Group 1, BW percentile differed between women who delivered female babies and women who delivered male babies (41.8 ± 27.5 vs. 57.0 ± 24.2, P = 0.043) (Table 2).
Table 1 shows that maternal Arg plasma concentration was higher in Groups 3 and 4 compared to Groups 1 and 2. ADMA and the ADMA/SDMA molar ratio plasma levels were significantly higher in Groups 2, 3 and 4 compared to Group 1. The highest ADMA plasma concentration was measured in the mothers of Group 3 with FGR (Table 1). In Group 1, ADMA plasma concentration was higher in women who delivered female babies [0.89 (0.69–1.09) vs. 0.59 (0.45–0.86) µM, P = 0.032] (Table 2). SDMA plasma concentration did not differ between the groups. In Group 1, SDMA plasma concentration was borderline higher in women who delivered female babies (0.66 ± 0.23 vs. 0.50 ± 0.27 µM, P = 0.062) (Table 2).
The Arg/ADMA molar ratio in the circulation is generally considered as a capacity measure of the Arg/NO pathway to generate NO. The lowest Arg/ADMA molar ratio was found in Group 3 (Table 1). These observations indicate that the Arg/NO pathway is severely altered in pregnant women with abnormal placental perfusion. The greatest alterations seem to occur in the Groups 3 and 4.
Under certain circumstances such as low nitrate/nitrite cost and overnight fasting (Tsikas 2015), circulating nitrite is a useful measure of endothelium-derived NO and endothelial dysfunction in humans (Kleinbongard et al. 2003, 2006). In Group 1, maternal nitrite plasma concentration was higher than in Groups 2, 3 and 4 (Table 1). In Group 1, nitrite plasma concentration was lower in women who delivered female babies [2.08 (1.91–2.28) vs. 2.70 (2.05–3.33) µM, P = 0.009] (Table 2). In Group 2, nitrite plasma concentration was higher in women who delivered female babies (1.99 ± 0.28 vs. 1.72 ± 0.10 µM, P = 0.020) (Table 2). Maternal nitrate plasma concentration did not differ between the groups, (Table 1) irrespective of the gender of the babies (Table 2).
Correlations between maternal plasma concentrations of biochemical and clinical parameters
The results of the correlations between BW percentile, the amino acids, nitrite and nitrate are summarized in Table 3 for the individual and combined groups.
In the healthy women of Group 1 and in the women of Group 2 with placental hypofusion, BW percentile did not correlate with maternal plasma concentration of Arg, ADMA, SDMA, nitrite or nitrate (Table 3). In contrast, in Group 3 with evident FGR and in Group 4 with PE, BW percentile correlated strongly and inversely (r = − 0.872, P < 0.001 for Group 3; r = − 0.800, P < 0.05 for Group 4) with the maternal ADMA plasma concentration. From the corresponding linear regression equations, it is seen that the effect of ADMA on BW percentile is much higher in Group 4 (y = 78 − 23x) than in Group 3 (y = 4.3 − 0.9x) (Fig. 1). In Group 3, BW percentile correlated positively with the Arg/ADMA molar ratio (r = 0.724, P < 0.05), suggesting that fetal growth in the pregnant women with the highest concentration of circulating ADMA (i.e., Group 3) is severely restricted. In all the study groups, SDMA and Arg maternal plasma concentrations did not correlate with BW percentile (Table 3).
In Group 1, maternal plasma ADMA and SDMA concentrations correlated positively with each other (r = 0.517, P < 0.001), as well as with the plasma concentration of their common precursor Arg (r = 0.359 and r = 0.368, respectively, P < 0.05 each; Table 3). In Group 2, maternal plasma ADMA and SDMA concentrations did not correlate with each other, whereas Arg correlated with SDMA (r = 0.741, P < 0.001) but not with ADMA (Table 3). Such correlations did not exist in the Groups 3 and 4. These observations indicate altered metabolism of Arg to ADMA and SDMA in the women of the Groups 3 and 4.
In Group 1, maternal plasma concentrations of nitrite correlated inversely with ADMA (r = − 0.525, P = 0.001) and SDMA (r = − 0.400, P = 0.013) (Table 3). This observation suggests a well-functioning endothelial Arg/NO system in the healthy pregnant women of the Group 1. In Group 2, maternal plasma concentration of nitrite correlated positively with ADMA (r = 0.490, P = 0.05). In contrast, in the Groups 3 and 4, maternal plasma nitrite concentration did not correlate with ADMA or SDMA plasma concentration. These findings suggest a dysfunctional endothelial Arg/NO pathway (Kleinbongard et al. 2003, 2006). In all the groups, plasma nitrate did not correlate with ADMA or SDMA. In Groups 3 and 4, the correlation between maternal plasma concentrations of nitrate and SDMA failed statistical significance (each P = 0.06) (Table 3).
In Group 1, plasma Arg, but not plasma ADMA or plasma SDMA concentration correlated positively both with diastolic blood pressure (DBP; r = 0.388, P = 0.016) and systolic blood pressure (SBP; r = 0.371, P = 0.022). This was not the case for the Groups 2, 3 and 4.
Discussion
In humans, the imino group (–C=NH) of the guanidine amino group of l-arginine (Arg) is enzymatically oxidized to NO with concomitant formation of l-citrulline. Although only about 0.1% of Arg is metabolized by NOS isoforms virtually in all the cell types of the body, the extremely potent vasodilatory effect of Arg-derived NO in endothelial cells is considered central to the regulation of blood flow and blood pressure in concert with other vasoactive compounds. The Arg/NO pathway plays an important role in health, disease and other conditions including pregnancy, both for the expectant mother and the fetus (Böger et al. 2010; Khalil et al. 2013, 2015). Previously, we found impaired endothelial function and elevated ADMA plasma concentrations in pregnant women who eventually developed PE (Savvidou et al. 2003). In that study, we found a strong inverse correlation between brachial FMD, which is NO-dependent, and plasma ADMA concentration only in the group of women who developed PE, i.e., in Group 4. The FMD levels in women who eventually developed PE (Group 4) were almost half of those in women with normal pregnancy outcome (Savvidou et al. 2003). This observation suggests that the endothelial dysfunction observed in women who subsequently developed PE is attributable, at least in part, to elevated ADMA levels which may reduce endothelial NOS activity and thus NO bioavailability in the cardiovascular system. However, ADMA is a very weak NOS inhibitor (IC50 ≈ 12 µM for eNOS; Kielstein et al. 2007; Tsikas 2017) (Fig. 2). Inhibition of NO-dependent effects in humans by exogenous ADMA has been observed at much higher ADMA plasma concentrations such as 10 µM (Kielstein et al. 2004; Tsikas 2017). It is, therefore, questionable whether the elevated ADMA concentrations measured in the Groups 3 and 4 of our study, can alone inhibit NOS activity to such a degree that NO-related activities including FMD and growth in the fetuses are severely impaired. It is possible that other factors can also play a role (Fig. 2).
Schematic of the proposed mechanisms illustrating the effects of ADMA and cis-EpOA on growth. NOS catalyzes the formation of NO from Arg. NO stimulates growth. Certain proteins rich in Arg (Protein-Arg) can also stimulate growth, in part by oxidizing polyunsaturated fatty acids (PUFAs). Protein–Arg epoxidize oleic acid to cis-EpOA which depresses growth. Protein–Arg are methylated on the guanidine group to form Protein–ADMA and Protein–SDMA by protein–arginine methyltransferases (PRMT) using S-adenosyl methionine (SAM) as the cofactor. Testosterone and IGF-1 inhibit this reaction. Proteolysis of Protein–ADMA and Protein–SDMA releases ADMA and SDMA, respectively, which are both NOS activity inhibitors; ADMA is more potent than SDMA. By this action, ADMA inhibits NO-dependent growth. ADMA (by 20%), SDMA (by 100%) are excreted unchanged in the urine. ADMA is hydrolyzed to l-citrulline and dimethylamine (DMA) by dimethylarginine dimethylaminohydrolase (DDAH). DMA and the NO metabolites nitrite and nitrate are excreted by the kidneys. l-Homoarginine (hArg) is synthesized from Arg and Gly by arginine: glycine amidinotransferase (AGAT) and promotes growth
This is the first study that assessed the association between maternal ADMA plasma concentration, at mid-pregnancy, and BW percentile. In the Groups 3 and 4 of our study, the BW percentiles were considerably lower than in the pregnant women of the Groups 1 and 2. Despite closely comparable maternal plasma concentrations of Arg, ADMA and SDMA in Groups 3 and 4, FGR was more evident in Group 3. We, therefore, examined correlations between the BW percentiles and maternal plasma concentrations of the key amino acids of the Arg/NO pathway, i.e., the NOS substrate Arg, and the NOS inhibitors ADMA and SDMA (Tsikas et al. 2000a, b; Tsikas 2017). We found strong inverse correlations between maternal ADMA plasma concentration and BW percentile in Groups 3 and 4.
A possible explanation for these observations could be that the fetuses of the women in Groups 3 and 4 were exposed to higher levels of ADMA than the fetuses of the women in Groups 1 and 2. The lack of correlation between ADMA and nitrite, the autoxidation product of endothelium-derived NO (Kleinbongard et al. 2003, 2006; Tsikas 2015), in the maternal plasma of the women of the Groups 3 and 4 suggests that ADMA may depress fetal growth mainly by mechanisms independent of NO. Such a mechanism could be inhibition of growth hormone (GH) factors including insulin-like growth factor-1 (IGF-1) by the low-molecular-mass amino acid ADMA and/or certain proteins/peptides that contain one or more ADMA residues (Fig. 2). Several studies reported that intrauterine growth restriction (IUGR) fetuses have placental dysfunction and low circulating levels of insulin, IGF-1, IGF-2 and IGF-binding proteins. Thus, IGF-deficiency in gestational state may be one of the major causes of growth restriction (reviewed by Martín-Estal et al. 2016). IUGR is associated with the male sexual hormone testosterone (Intapad et al. 2017). Further, it is worth mentioning that in nondiabetic ankylosing spondylitis patients, circulating ADMA and IGF-1 levels were found to be inversely correlated (Genre et al. 2014). In men with primary hypogonadism, we found elevated plasma ADMA concentrations which were significantly reduced after a 24-week treatment with testosterone (Tsikas and Kinzel 2017). In acromegaly men and women, who also suffer from cardiovascular disease, ADMA and IGF-1 were also found to be involved (Yaron et al. 2016). In acromegaly men and women with active disease, we found lower circulating concentrations of ADMA compared to acromegaly patients with controlled diseases. In these patients, circulating levels of both, IGF-1 and GH, behaved in the opposite direction than ADMA (data not shown). The close association between plasma nitrite and nitrate concentrations in active and controlled disease suggests that the ADMA changes are not associated with Arg/NOS-derived NO.
In children with growth hormone deficiency (GHD), we found higher plasma ADMA concentrations than in age-matched children (mean age 10 and 9 years, respectively) without GHD (Langen et al. 2015). In young adults with GHD, GH replacement was found to decrease serum ADMA concentration (by 9%), to increase plasma cGMP (by 40%), yet with no changes in plasma nitrite + nitrate and serum ADMA concentrations, SBP and DBP (Setola et al. 2008). The decrease in serum ADMA concentration correlated with the increase of serum IGF-1, whereas the increase in plasma cGMP correlated with the increase of serum IGF-1 (Setola et al. 2008). The results of the above mentioned study suggest that the effects of GH treatment are independent of NO. However, in healthy middle-aged subjects, short-term GH treatment reduced circulating ADMA concentrations, increased plasma nitrite and nitrate concentrations indicating NO involvement (Thum et al. 2007a, b, c). Insulin and IGF-1 have been reported to cause vasodilation in human vessels independent of NO, possibly involving potassium channels (McKay and Hester 1996; Hasdai et al. 1998; Izhar et al. 2000).
Proteins and peptides rich in Arg and/or l-lysine, such as melittin, were found to enhance indirect formation of endothelium-derived NO and endothelium-dependent relaxation (Förstermann and Neufang 1985; Thomas et al. 1986; Ignarro et al. 1989). Such polycationic biomolecules can also induce formation of oxidized fatty. Previously, we found that the maternal plasma cis-9,10-epoxystearic acid (cis-EpOA) concentration did not differ between the four groups of our study (Tsikas and Savvidou 2017). In the Group 4 of our study, maternal plasma ADMA concentration did not correlate with maternal plasma cis-EpOA, however, cis-EpOA correlated inversely with BW percentile (Tsikas and Savvidou 2017). Whether cis-EpOA formation is modulated by polycationic peptides/proteins in pregnancy remains to be demonstrated (Fig. 2).
The physiological significance of ADMA-containing proteins and peptides has not been studied in the context of NO formation from Arg, thus far. However, reported studies indicate important physiological roles of ADMA-containing proteins in growth. Thus, physiological high molecular weight forms of fibroblast growth factor-2 have been reported to contain 5 to 7 ADMA residues (Klein et al. 2000). Insulin is a 51-amino acid protein and contains a single Arg residue. Insulin has been shown to modulate methylation of guanidinoacetate, an l-arginine metabolite (Tsikas and Wu 2015), in liver homogenate (De Barbieri and Benassi 1950). In rats, maternal deficiency of folate, a vitamin contributing to methyl groups, was associated with lower fetal growth, lower maternal serum IGF-1 and IGFBP3, and lower IGFBP-3 in fetal brain and liver compared to control rats (no folate deficiency) (Wu et al. 2017). IGF-1 and IGF-2 receptors and several IGFBP were found to be more abundantly methylated in fetal brain and liver compared to the fetuses of the control rats. In addition, the methylation degree of the IGF-2 gene was found to be lower in the folate deficient group (Wu et al. 2017). Yet, whether Arg residues of the IGF system had been methylated in that study has not been reported. The number of Arg residues is 6 in IGF-1 (70 amino acids) and 8 in IGF-2 (67 amino acids), i.e., relatively high. The methylation degree of IGF-1 and IGF-2 in pregnancy without and with abnormal placental hypofusion and its potential association with ADMA remains to be investigated.
We have hypothesized that ADMA represses growth in children mainly by mechanisms independent of NO (Langen et al. 2015). Extension of this hypothesis to pregnancy would mean that the maternal ADMA is a major repressor of the fetal growth, with high plasma ADMA concentrations disproving the placenta function through its interaction with insulin-like growth factors and/or their binding proteins (BP) and receptors (Martín-Estal et al. 2016). In the study’s Groups 3 and 4, the maternal ADMA plasma concentrations were highest and the BW percentiles were lowest. In both the groups, BW percentile decreased with increasing maternal ADMA plasma concentration, but the negative effect of ADMA on BW was stronger in Group 4, although these babies were larger than in Group 3. This remarkable difference may suggest that in women who eventually developed PE additional, not yet known factors have affected fetuses’ growth and/or maternal physiology resulting in earlier delivery (by 4 weeks compared to Group 3). These factors are likely to be involved in maternal hypertension observed in women of the Group 4 (by 11 mmHg compared to Group 3) and may include vasoactive substances such as endothelin-1 and thromboxane (Possomato-Vieira and Khalil 2016; Saleh et al. 2016). Plasma concentrations of l-homoarginine, another l-arginine metabolite (Tsikas and Wu 2015), at 11–13 weeks’ gestation are lower in early PE than in healthy pregnancy (Khalil et al. 2013, 2015). In the cardiovascular system, hArg seems to counteract the negative effects of ADMA (Tsikas and Kayacelebi 2014; Langen et al. 2015). Unlike ADMA, hArg does not occur as a residue in proteins. Thus, only the free amino acid hArg can exert biological effects. As we had not measured circulating hArg concentrations in the present study, its antagonistic effect on ADMA’s NO-independent actions in the study’s groups is expectable but still elusive (Fig. 2).
In conclusion, we found a significant inverse correlation between birthweight percentile and maternal ADMA plasma concentration, measured at mid-pregnancy, in women with abnormal placental perfusion who also delivered a FGR baby or developed PE. But, BW percentile did not correlate with the maternal plasma concentration of Arg, SDMA, nitrate or nitrite. Maternal plasma ADMA concentration is an important indicator of fetal growth restriction in women with impaired placental perfusion independent of NO. The underlying mechanisms are elusive and further studies are required.
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine
- AGA:
-
Appropriate for gestational age
- BW:
-
Birthweight
- FGR:
-
Fetal growth restriction
- FMD:
-
Flow-mediated dilatation
- GA:
-
Gestational age
- GH:
-
Growth hormone
- GHD:
-
Growth hormone deficiency
- IGF-1:
-
Insulin-like growth factor-1
- IUGR:
-
Intrauterine growth restriction
- LGA:
-
Large for gestational age
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- eNOS:
-
Endothelial NOS
- PE:
-
Preeclampsia
- PRMT:
-
Protein arginine methyltransferase
- SDMA:
-
Symmetric dimethylarginine
- SGA:
-
Small for gestational age
References
Albaiges G, Missfelder-Lobos H, Lees C, Parra M, Nicolaides KH (2000) One-stage screening for pregnancy complications by color Doppler assessment of the uterine arteries at 23 weeks’ gestation. Obstet Gynecol 96:559–564
Bassareo PP, Puddu M, Flore G, Deidda M, Manconi E, Melis A, Fanos V, Mercuro G (2012) Could ADMA levels in young adults born preterm predict an early endothelial dysfunction? Int J Cardiol 159:217–219
Böger RH, Diemert A, Schwedhlm E, Lüneburg N, Maas R, Hecher K (2010) The role of nitric oxide synthase inhibition by asymmetric dimethylarginine in the pathophysiology of preeclampsia. Gynecol Obstet Investig 69:1–13
Buck A, Kayacelebi AA, Chobanyan-Jürgens K, Illsinger S, Bohnhorst B, Beckmann B, Hanff E, Das AM, Tsikas D, Lücke T (2017) Comprehensive analysis of the l-arginine/l-homoarginine/nitric oxide pathway in preterm neonates: potential roles for homoarginine and asymmetric dimethylarginine in foetal growth. Amino Acids 49:783–794
Chiavaroli V, Diesse L, de Giorgis T, Giannini C, Marcovecchio ML, Chiarelli F, Mohn A (2014) Is asymmetric dimethylarginine associated with being born small and large for gestational age? Antioxid Redox Signal 20:2317–2322
Cockell AP, Poston L (1997) Flow-mediated vasodilatation is enhanced in normal pregnancy but reduced in preeclampsia. Hypertension 30:247–251
Davey DA, MacGillivray I (1988) The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol 158:892–898
De Barbieri A, Benassi C (1950) Action of insulin on methylation of guanidoacetic acid in liver homogenates. Boll Soc Ital Biol Sper 26:1435–1436
Emrich IE, Zawada AM, Martens-Lobenhoffer J, Fliser D, Wagenpfeil S, Heine GH, Bode-Böger SM (2017) Symmetric dimethylarginine (SDMA) outperforms asymmetric dimethylarginine (ADMA) and other methylarginines as a predictor of renal and cardiovascular outcome in non-dialysis chronic kidney disease. Clin Res Cardiol. https://doi.org/10.1007/s00392-017-1172-4
Förstermann U, Neufang B (1985) Endothelium-dependent vasodilation by melittin: are lipoxygenase products involved? Am J Physiol 249:H14–H19
Genre F, López-Mejías R, Rueda-Gotor J, Miranda-Filloy JA, Ubilla B, Villar-Bonet A, Carnero-López B, Gómez-Acebo I, Blanco R, Pina T, González-Juanatey C, Llorca J, González-Gay MA (2014) IGF-1 and ADMA levels are inversely correlated in nondiabetic ankylosing spondylitis patients undergoing anti-TNF-alpha therapy. Biomed Res Int 2014:671061
Gumus E, Atalay MA, Cetinkaya Demir B, Sahin Gunes E (2016) Possible role of asymmetric dimethylarginine (ADMA) in prediction of perinatal outcome in preeclampsia and fetal growth retardation related to preeclampsia. J Matern Fetal Neonatal Med 29:3806–3811
Hasdai D, Rizza RA, Holmes DR Jr, Richardson DM, Cohen P, Lerman A (1998) Insulin and insulin-like growth factor-I cause coronary vasorelaxation in vitro. Hypertension 32:228–234
Ignarro LJ, Gold ME, Buga GM, Byrns RE, Wood KS, Chaudhuri G, Frank G (1989) Basic polyamino acids rich in arginine, lysine, or ornithine cause both enhancement of and refractoriness to formation of endothelium-derived nitric oxide in pulmonary artery and vein. Circ Res 64:315–329
Intapad S, Dasinger JH, Fahling JM, Backstrom MA, Alexander BT (2017) Testosterone is protective against impaired glucose metabolism in male intrauterine growth-restricted offspring. PLoS One 12:e0187843
Izhar U, Hasdai D, Richardson DM, Cohen P, Lerman A (2000) Insulin and insulin-like growth factor-I cause vasorelaxation in human vessels in vitro. Coron Artery Dis 11:69–76
Khalil AA, Tsikas D, Akolekar R, Jordan J, Nicolaides KH (2013) Asymmetric dimethylarginine, arginine and homoarginine at 11-13 weeks’ gestation and preeclampsia: a case-control study. J Hum Hypertens 27:38–43
Khalil A, Hardman L, O Brien P (2015) The role of arginine, homoarginine and nitric oxide in pregnancy. Amino Acids 47:1715–1727
Kielstein JT, Impraim B, Simmel S, Bode-Böger SM, Tsikas D, Frölich JC, Hoeper MM, Haller H, Fliser D (2004) Cardiovascular effects of systemic nitric oxide synthase inhibition with asymmetrical dimethylarginine in humans. Circulation 109:172–177
Kielstein A, Tsikas D, Galloway GP, Mendelson JE (2007) Asymmetric dimethylarginine (ADMA)—a modulator of nociception in opiate tolerance and addiction? Nitric Oxide 17:55–59
Klein S, Carroll JA, Chen Y, Henry MF, Henry PA, Ortonowski IE, Pintucci G, Beavis RC, Burgess WH, Rifkin DB (2000) Biochemical analysis of the arginine methylation of high molecular weight fibroblast growth factor-2. J Biol Chem 275:3150–3157
Kleinbongard P, Dejam A, Lauer T, Rassaf T, Schindler A, Picker O et al (2003) Plasma nitrite reflects constitutive nitric oxide synthase activity in mammals. Free Radic Biol Med 35:790–796
Kleinbongard P, Dejam A, Lauer T, Jax T, Kerber S, Gharini P et al (2006) Plasma nitrite concentrations reflect the degree of endothelial dysfunction in humans. Free Radic Biol Med 40:295–302
Langen J, Kayacelebi AA, Beckmann B, Weigt-Usinger K, Carmann C, Hörster I, Lilienthal E, Richter-Unruh A, Tsikas D, Lücke T (2015) Homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in short stature children without and with growth hormone deficiency: hArg and ADMA are involved differently in growth in the childhood. Amino Acids 47:1875–1883
Laskowska M, Laskowska K, Leszczyńska-Gorzelak B, Oleszczuk J (2011) Asymmetric dimethylarginine in normotensive pregnant women with isolated fetal intrauterine growth restriction: a comparison with preeclamptic women with and without intrauterine growth restriction. J Matern Fetal Neonatal Med 24:936–942
Laskowska M, Laskowska K, Oleszczuk J (2015) The relation of maternal serum eNOS, NOSTRIN and ADMA levels with aetiopathogenesis of preeclampsia and/or intrauterine fetal growth restriction. J Matern Fetal Neonatal Med 28:26–32
López-Alarcón M, Montalvo-Velarde I, Vital-Reyes VS, Hinojosa-Cruz JC, Leaños-Miranda A, Martínez-Basila A (2015) Serial determinations of asymmetric dimethylarginine and homocysteine during pregnancy to predict pre-eclampsia: a longitudinal study. BJOG 122:1586–1592
Martín-Estal I, de la Garza RG, Castilla-Cortázar I (2016) Intrauterine growth retardation (IUGR) as a novel condition of insulin-like growth factor-1 (IGF-1) deficiency. Rev Physiol Biochem Pharmacol 170:1–35
McKay MK, Hester RL (1996) Role of nitric oxide, adenosine, and ATP-sensitive potassium channels in insulin-induced vasodilation. Hypertension 28:202–208
Moonen RM, Huizing MJ, Cavallaro G, González-Luis GE, Bas-Suárez P, Bakker JA, Villamor E (2014) Plasma levels of dimethylarginines in preterm very low birth weight neonates: its relation with perinatal factors and short-term outcome. Int J Mol Sci 16:19–39
Morales Y, Cáceres T, May K, Hevel JM (2016) Biochemistry and regulation of the protein arginine methyltransferases (PRMTs). Arch Biochem Biophys 590:138–152
Poon LC, Volpe N, Muto B, Syngelaki A, Nicolaides KH (2012) Birthweight with gestation and maternal characteristics in live births and stillbirths. Fetal Diagn Ther 32:156–165
Possomato-Vieira JS, Khalil RA (2016) Mechanisms of endothelial dysfunction in hypertensive pregnancy and preeclampsia. Adv Pharmacol 77:361–431
Richir MC, van Leeuwen PA, van den Berg A, Wessels R, Twisk JW, Rauwerda JA, Teerlink T, de Vries TP, van Elburg RM (2008) Plasma ADMA concentrations at birth and mechanical ventilation in preterm infants: a prospective pilot study. Pediatr Pulmonol 43:1161–1166
Saleh L, Verdonk K, Visser W, van den Meiracker AH, Danser AH (2016) The emerging role of endothelin-1 in the pathogenesis of pre-eclampsia. Ther Adv Cardiovasc Dis 10:282–293
Sandvik MK, Leirgul E, Nygård O, Ueland PM, Berg A, Svarstad E, Vikse BE (2013) Preeclampsia in healthy women and endothelial dysfunction 10 years later. Am J Obstet Gynecol 209:569.e1–569.e10
Savvidou MD, Hingorani AD, Tsikas D, Frölich JC, Vallance P, Nicolaides KH (2003) Endothelial dysfunction and raised plasma concentrations of asymmetric dimethylarginine in pregnant women who subsequently develop pre-eclampsia. Lancet 361:1511–1517
Schlesinger S, Sonntag SR, Lieb W, Mass R (2016) Asymmetric and symmetric dimethylarginine as risk markers for total mortality and cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. PLoS One 11:e0165811
Setola E, Monti LD, Lanzi R, Lucotti P, Losa M, Gatti E, Galluccio E, Oldani M, Fermo I, Giovannelli M, Bosi E, Piatti P (2008) Effects of growth hormone treatment on arginine to asymmetric dimethylarginine ratio and endothelial function in patients with growth hormone deficiency. Metabolism 57:1685–1690
Speer PD, Powers RW, Frank MP, Harger G, Markovic N (2008) Roberts JM (2008) Elevated asymmetric dimethylarginine concentrations precede clinical preeclampsia, but not pregnancies with small-for-gestational-age infants. Am J Obstet Gynecol 198:112.e1–112.e7
Takaya J, Tanabe Y, Kuroyanagi Y, Kaneko K (2017) Relationship between asymmetric dimethylarginine in umbilical cord plasma and birth weight follows a U-shaped curve. Endocr J 64:431–436
Thomas G, Mostaghim R, Ramwell PW (1986) Endothelium dependent vascular relaxation by arginine containing polypeptides. Biochem Biophys Res Commun 141:446–451
Thum T, Fleissner F, Klink I, Tsikas D, Jakob M, Bauersachs J, Stichtenoth DO (2007a) Growth hormone treatment improves markers of systemic nitric oxide bioavailability via insulin-like growth factor-I. J Clin Endocrinol Metab 92:4172–4179
Thum T, Hoeber S, Froese S, Klink I, Stichtenoth DO, Galuppo P, Jakob M, Tsikas D, Anker SD, Poole-Wilson PA, Borlak J, Ertl G, Bauersachs J (2007b) Age-dependent impairment of endothelial progenitor cells is corrected by growth-hormone-mediated increase of insulin-like growth-factor-1. Circ Res 100:434–443
Thum T, Fleissner F, Klink I, Tsikas D, Stichtenoth D, Ertl G, Bauersachs J (2007c) Growth hormone treatment improves markers of systemic nitric oxide bioavailability via the insulin-like growth factor-1. Importance for endothelial progenitor cells. J Stem Cells Regen Med 2:115–116 (eCollection 2007)
Tsikas D (2000) Simultaneous derivatization and quantification of the nitric oxide metabolites nitrite and nitrate in biological fluids by gas chromatography/mass spectrometry. Anal Chem 72:4064–4072
Tsikas D (2015) Circulating and excretory nitrite and nitrate: their value as measures of nitric oxide synthesis, bioavailability and activity is inherently limited. Nitric Oxide 45:1–3
Tsikas D (2017) Does the inhibitory action of asymmetric dimethylarginine (ADMA) on the endothelial nitric oxide synthase activity explain its importance in the cardiovascular system? The ADMA paradox. J Controv Biomed Res 3:16–22
Tsikas D, Kayacelebi AA (2014) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78:2094–2095
Tsikas D, Kinzel M (2017) Associations between asymmetric dimethylarginine (ADMA), nitrite-dependent renal carbonic anhydrase activity and plasma testosterone levels in hypogonadal men. Hell J Cardiol. https://doi.org/10.1016/j.hjc.2017.10.004
Tsikas D, Savvidou M (2017) Plasma oleic acid oxide in women at risk of preeclampsia correlates inversely with birthweight percentile. JSM Biochem Mol Biol 4:1028
Tsikas D, Wu G (2015) Homoarginine, arginine, and relatives: analysis, metabolism, transport, physiology, and pathology. Amino Acids 47:1697–1702
Tsikas D, Junker W, Frölich JC (1998) Determination of dimethylated arginines in human plasma by high-performance liquid chromatography. J Chromatogr B 705:174–176
Tsikas D, Sandmann J, Savva A, Luessen P, Böger RH, Gutzki FM, Mayer B, Frölich JC (2000a) Assessment of nitric oxide synthase activity in vitro and in vivo by gas chromatography–mass spectrometry. J Chromatogr B 742:143–153
Tsikas D, Böger RH, Sandmann J, Bode-Böger SM, Frölich JC (2000b) Endogenous nitric oxide synthase inhibitors are responsible for the l-arginine paradox. FEBS Lett 478:1–3
Vida G, Sulyok E, Lakatos O, Ertl T, Martens-Lobenhoffer J, Bode-Böger SM (2009) Plasma levels of asymmetric dimethylarginine in premature neonates: its possible involvement in developmental programming of chronic diseases. Acta Paediatr 98:437–441
Williams DJ, Vallance PJ, Neild GH, Spencer JA, Imms FJ (1997) Nitric oxide-mediated vasodilation in human pregnancy. Am J Physiol 272:H748–H752
Wu MM, Yang F, Qu Y, Mu DZ (2017) Effects of maternal folate deficiency on the methylation of insulin-like growth factor system in the offspring rats. Zhongguo Dang Dai Er Ke Za Zhi 19:470–474
Yaron M, Izkhakov E, Sack J, Azzam I, Osher E, Tordjman K, Stern N, Greenman Y (2016) Arterial properties in acromegaly: relation to disease activity and associated cardiovascular risk factors. Pituitary 19:322–331
Yuan J, Wang X, Xie Y, Wang Y, Dong L, Li H, Zhu T (2017) Circulating asymmetric dimethylarginine and the risk of preeclampsia: a meta-analysis based on 1338 participants. Oncotarget 8:43944–43952
Zobel EH, von Scholten BJ, Reinhard H, Persson F, Teerlink T, Hansen TW et al (2017) Symmetric and asymmetric dimethylarginine as risk markers of cardiovascular disease, all-cause mortality and deterioration in kidney function in persons with type 2 diabetes and microalbuminuria. Cardiovasc Diabetol 16:88
Acknowledgements
The initial study was supported by The Fetal Medicine Foundation (UK Registered Charity number: 1037116).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
The study was approved by the Local REC and all the patients gave written informed consent.
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
Additional information
Handling Editor: J. Marshal.
Rights and permissions
About this article
Cite this article
Tsikas, D., Bollenbach, A. & Savvidou, M.D. Inverse correlation between maternal plasma asymmetric dimethylarginine (ADMA) and birthweight percentile in women with impaired placental perfusion: circulating ADMA as an NO-independent indicator of fetal growth restriction?. Amino Acids 50, 341–351 (2018). https://doi.org/10.1007/s00726-017-2522-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-017-2522-2