Abstract
Calciphylaxis is severe condition with 45–55 % mortality occurring in chronic dialysis patients. Sporadically, the disease may develop in the patients with normal renal function, for example, in the presence of chronic renal inflammation. Sodium thiosulfate (STS) therapy is a treatment modality of calciphylaxis, but mechanism of its action is unknown. We report four cases of calciphylaxis treated with STS, illustrating that its therapeutic effect is not associated with decreased serum calcium or phosphorus concentration. Therapy with intravenous STS was safe and led to subjective improvement, due to pain reduction, and lesions healing in three of four patients. In one patient, complications of diabetes and other co-morbidities led to unfavorable outcome. STS can be considered promising drug in the treatment of calciphylaxis.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare but severe condition occurring in 1–4 % of chronic dialysis patients [1]. This life-threatening state is characterized by vascular calcification and cutaneous necrosis associated with painful progressive ulcerations. The ulcers are typically localized on the skin of the lower extremities and abdomen [2, 3]. Sporadically, the disease may develop in the patients with normal renal function, for example, in the presence of chronic renal inflammation [3]. The highest incidence of the disease is in the fifth decade of life. In females, calciphylaxis occurs two times more frequently than in males [4, 5].
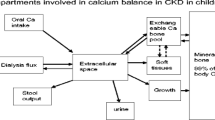
The mortality rate is associated with the localization and type of lesions and reaches 45–55 %. Mortality is higher in the patients with proximal calciphylaxis [6]. The most frequent cause of death is sepsis [4, 6]. The pathogenesis of calciphylaxis is not well understood, probably due to its multifactorial character [2–6]. In the patients with end-stage renal insufficiency and hyperphosphatemia, high serum phosphorus concentration activates the parathyroid glands, and higher concentrations of parathyroid hormone cause hypercalcemia [7].
The diagnosis of calciphylaxis is established clinically: predispositions, risk factors, extreme pain, and livid skin nodules. Induration, typical localization and the configuration of skin ischemia and necrosis are generally sufficient for the diagnosis [8]. Although biopsy provides a direct proof of the diagnosis, it is associated with risk of ulcerations, infection, further progression of the lesions, hemorrhages, and necrosis [9]. The main benefits of biopsy consist of morphological confirmation of the diagnosis and exclusion of other conditions that can mimic calciphylaxis. A punch or telescoping biopsy from lesion margin or deep incisional wedge skin biopsy is likely to have best yield. Punch biopsy is safer and is a preferred approach over an incisional biopsy. In general, biopsy at the center of the ulcer or necrotic area is of low diagnostic yield [10]. Histological findings associated with calciphylaxis include arterial media calcification, microthromboses, fibrointimal hyperplasia, and septal panniculitis [11].
There is no consensus regarding the treatment of calciphylaxis [12]. In uremic patients with calciphylaxis, therapy is focused primarily on the normalization of calcium and phosphorus metabolism, for example, daily dialysis with low calcium dialysate and high doses of calcium-free phosphate binders [13, 14]. Furthermore, the reduction or discontinuation of vitamin D and the administration of receptor activators, calcium binders, and coumarins are applied. There are several proteins important for the process of inhibition of calcification. One of them, matrix gla protein (MGP), requires posttranslational vitamin K dependent carboxylation for activation [12]. Finally, parathyroidectomy and calcimimetic administration should be considered in patients with confirmed hyperparathyroidism [12–14]. The other treatment modalities include local wound care, antibiotics, analgesics, and hyperbaric oxygen therapy [15].
Sodium thiosulfate (STS) intravenous administration is one of the treatment modalities that have been used to treat patients with calciphylaxis since 2004 [16]. STS is typically applied as an antidote for the treatment of cyanide poisoning [17]. Its mechanism of action in calciphylaxis is still unclear. It is known that calcium thiosulfate salts are 250–100,000 times more water soluble than other calcium salts and can be removed by dialysis [18].
The typical empirical dose of STS is 25 g diluted in 100 cm3 of saline, administered intravenously three times per week during the last 30 min of a hemodialysis session. Administration at the end of a hemodialysis session can reduce the risk of adverse effects, because STS is dialyzable [6]. The possible adverse effects of STS administration are hypernatremia, acidemia, gastric hemorrhage, seizures, nausea, vomiting, and peripheral edema [5]. Adverse effects can be attributed to medication errors during the treatment, for example if the initial dose of STS is too big [19, 20]. After dose reduction, the adverse effects usually disappear. The positive effect of STS mediated by the inhibition of vascular calcification has a negative side: the inhibition of bone calcification and hydroxyapatite formation [21].
Although STS had been demonstrated to be effective in the therapy of calciphylaxis, the literature on the problem is still scarce, consisting of several case reports with insufficient clinical data. There is no consensus with regard to the regimen and dosage of STS administration or with regard to the duration of therapy. In this study, we present a case series of four patients with calciphylaxis treated with STS administration and discuss the optimal treatment modality based on a literature review.
Results and discussion
Case 1
A 65-year-old female was treated at the hemodialysis unit with chronic renal insufficiency that developed as a complication of lupus nephritis in 2009. The patient had several co-morbidities: autoimmune hemolytic anemia, hypertension, atrial fibrillation, protein malnutrition, and secondary hyperparathyroidism.
During the period from September to December 2014, the patient was hospitalized repeatedly due to progressive pain in the lower extremities with the subsequent development of ulcerative and necrotic lesions. In January 2015, the diagnosis of calciphylaxis was confirmed by biopsy. From March 2015, the patient was administered STS in the dose of 25 g three times per week during the last 30 minutes of hemodialysis sessions. The patient had been discharged in June, but the therapy with STS still continued.
No significant reduction of serum calcium or phosphorus occurred during treatment. Phosphorus levels actually increased slightly (Fig. 1). The serum parathyroid hormone level increased during the period from February to June 2015 (12.0–35.0 pmol dm−3, reference range is 10.0–55.0 pmol dm−3). Other laboratory parameters are presented in Table 1. The administration of vitamin D and phosphate-binder sevelamer was added to the therapy. Due to abnormal nutritional parameters (decreased serum albumin, total protein, and cholesterol), nutritional support was applied. Hemodialysis continued without complications. After 4 months of hospitalization, a significant reduction in the severity of ulcerative regions was registered, and the general condition of the patient was stabilized. The patient was discharged with a recommendation for further outpatient observation and treatment.
Case 2
A 71-year-old female with poorly controlled diabetes mellitus type II (according to the data from the diabetic profile, repeatedly high glycaemia was registered: 11.0–13.3–7.9–8.2 mmol dm−3) and obesity was included in the regular hemodialysis program because of diabetic and hypertensive nephropathy since November 2013. The additional co-morbidities were arterial hypertension, secondary hyperparathyroidism, and anemia. On February 11, 2014 calciphylaxis was diagnosed, and the treatment was started. The patient had hyperglycemia (11 mmol dm−3) and elevated inflammatory parameters: C-reactive protein (CRP) 39.8 mg dm−3, leukocytes 12.9 × 109 dm−3. A lesion of 4.6 × 2.2 cm with ulceration and 0.5 cm central depression was found in the right hypogastrium, and a lesion without ulceration was present in the left hypogastrium. The patient developed superficial thrombophlebitis on the medial side of the right thigh, which indicated the development of an additional calciphylaxis lesion.
Hemodialysis was performed every second day and followed by the intravenous administration of sodium thiosulfate. The dose was gradually increased from 5 to 10 and further to 15 g. The treatment with STS was well tolerated, without adverse reactions, and led to considerable relief to the patient, pain reduction, and significant regression of the local pathologic findings. During the treatment with STS, serum calcium and phosphorus concentrations did not decrease; actually, mild elevation of the serum concentrations was observed (Fig. 2). The serum parathyroid hormone level slightly decreased from 48 to 45 pmol dm−3 during the period of hospitalization from February to July. Further therapy included regular local treatment of abdominal wall defects and antibiotics administration (Augmentin and Amikacin).
The treatment with STS and dialysis led to healing of the skin defects, pain reduction, and decreased inflammation. No complications occurred. The patient was discharged to outpatient care in July 2014 with the recommendation of dialysis sessions three times per week, infusion therapy, and local treatment of healing skin defects (Table 2).
Case 3
A 62-year-old female with diabetes mellitus type I and coronary artery disease was hospitalized at the dialysis department in September 2014. The indication for hemodialysis was acute renal failure after a complicated cardiac operation and chronic nephrosclerosis.
The calciphylaxis was diagnosed at the end of January 2015, and the treatment with STS was started immediately. STS was administered at a dose of 25 g three times per week during the last hour of hemodialysis sessions. The patient was administered antibiotics (vancomycin, metronidazole) and non-calcium phosphate binders. Serum levels of calcium and phosphorus were within physiological ranges during the treatment with STS.
The calciphylaxis was of the central (proximal) type, with the gradual progression of extensive necrosis in the abdominal region (Fig. 3a). Surgical necrectomies were performed with further daily local care and one hyperbaric oxygenation (HBO) session. The HBO was indicated because of ischemic ulcers and defects persisting despite the treatment provided.
During the hospitalization, the gynecological malignant tumor was diagnosed, but the operation was contraindicated due to the patient’s general state and unhealed lesions in the abdominal region. In April 2015, the patient was discharged from the hospital in a stabilized state (Fig. 3b) with the recommendation of further outpatient local treatment and observation.
According to the medical records and information from relatives, the patient’s condition improved gradually after discharge. Nevertheless, on June 15, the patient was admitted to the hospital with decompensation of diabetes, elevation of inflammatory parameters, increase of tumor markers, and deterioration of her general condition. In the abdominal region, another focus of ulceration and necrosis appeared next to the site of the original lesion, which was nearly healed (Fig. 3c).
On June 21, cardiac and respiratory arrest occurred. The patient was resuscitated, intubated, and transferred to the ICU, where exitus letalis occurred shortly after the transfer (Table 3).
Case 4
A 62-year-old male with diabetes treated with insulin (Novorapid 6–6–8 units subcutaneously and Levemir 8 units subcutaneously before sleeping) had been in the care of the dialysis department from April 2013 with chronic renal failure due to diabetic nephropathy. The diabetes was complicated by diabetic neuropathy of the lower extremities. The co-morbidities included ischemic heart disease and peripheral arterial disease. Calciphylaxis lesions on both legs were diagnosed in October 2014. Sodium thiosulfate therapy was started immediately with three ampoules of STS 10 % 10 cm3/1 g administered intravenously three times a week during the last hour of hemodialysis sessions. In total, the patient received 40 g of STS. Despite this therapy, the defects on the patient’s lower extremities progressed. A below-knee amputation of both legs was recommended, but the patient repeatedly refused it. Due to severe pain in the legs, an epidural catheter was introduced for opiate administration. For further care, the patient was hospitalized in hospice. In November 2014, the patient developed sepsis and died despite antibiotic treatment in early December 2015.
Calciphylaxis remains a life-threatening condition with only 50 % survival during the first 3.3 months after the start of treatment [6]. In our case series study, the administration of STS resulted in the survival of 75 % of patients with documented complete or partial remission of the disease. Therefore, treatment with massive doses of STS (25 g per dialysis session) led to favorable short-term and long-term outcomes in most cases.
STS has a small molecular weight (248) and short elimination half-life (15 min) in patients with normal renal function. The toxicity of STS is low, because it is rapidly excreted by the kidneys and biliary secretion; side effects are rare and usually disappear after the dose reduction [21]. Its administration leads to increased osmolality. The calcium salt of thiosulfuric acid is water soluble and well removable by hemodialysis [1]. The adverse effects of STS administration include hypernatremia, metabolic acidosis with increased anion gap, nausea, peripheral edemas, gastrointestinal bleeding, rhinorrhea, headaches and mild phlebitis [5, 22].
The mechanism of STS action in calciphylaxis is still unknown. Our data confirmed that its effect is not associated with a significant decrease in serum calcium or phosphate concentrations or any decrease in parathyroid hormone level. During the intravenous administration of STS, only insignificant and temporal decreases in calcium and phosphate occurred, and concentrations remained at levels much higher than recommended. Our data are consistent with animal models, where a short decrease in serum calcium occurred within the first 15 min. after thiosulfate administration, but later no significant decrease was recorded [23].
According to previous studies, STS has vasodilator and antioxidant properties [24]. These properties can lead, as observed in our study, to pain relief due to the improvement of endothelial dysfunction present in patients with calciphylaxis [25, 26]. Recent studies suggest that STS prevents calcium crystal formation and binds iron ions participating in the pathogenesis of calciphylaxis. The losses of serum iron are not significant; therefore, the supplementary therapy is not necessary [27, 28].
Over the course of 12 years of STS application in the context of calciphylaxis therapy, different thiosulfate administration schemes have been suggested. The optimal regimen and dosage for thiosulfate administration have not yet been established [19]. In the study by Zitt et al., weekly doses ranged from 30 to 125 grams, with 81 % of patients receiving 75 g of STS per week, while children received 25 g per 1.73 m2 of body surface area per week [6].
Two of our patients were administered STS during the last hour of the hemodialysis session. The other two patients received doses during the last 30 min of hemodialysis. Single doses from 5 to 25 g were administered three to four times per week. The course of treatment lasted several months. Except for the last case, partial or total healing of skin lesion defects, pain relief, and decreased inflammation were observed. No adverse effects were noted during STS administration.
Conclusion
The long-term prognosis in the patients treated with STS depends on several factors: extent of the lesions, severity of the disease, patient’s general condition, age, co-morbidities, and so on. The largest clinical study performed in the field with 27 patients treated with STS confirmed a positive effect of STS administration as part of complex therapy. In 70 % of cases, partial or complete remission was observed. Nevertheless, 52 % of patients died within 101 days. The mortality was highest in the group of elderly patients and in the cases of proximal calciphylaxis [6].
The empirical single dose we recommend for the treatment of calciphylaxis is 25 g of STS administered intravenously three times a week for 30–60 min at the end of hemodialysis sessions. It was shown that the administration of STS during the last hour of dialysis prevents adverse effects and should be preferred to administration after the hemodialysis session [6]. After the first week of therapy, the dose can be reduced to 12.5 g to avoid adverse effects.
Experimental
Patients and laboratory investigations
Four patients with confirmed diagnosis of calciphylaxis were treated in the following hospitals: General University Hospital in Prague, Hospital Decin, and Hospital Nachod in the Czech Republic.
The discharge reports of hospitalized patients with a confirmed diagnosis and the results of laboratory measurements on admission, during hospitalization, and on discharge were collected and analyzed. Laboratory analyses were performed on admission and during hospitalization. All patients were treated with hemodialysis and sodium thiosulfate according to previously published treatment protocols. Sodium thiosulfate solution was given intravenously either before, or during/at the end of hemodialysis sessions. Antibiotics and non-calcium phosphate binders were administered according to the indications and treatment schemes.
Serum sodium, potassium, phosphorus were measured on admission, before the treatment initiation, and during hospital treatment. Other laboratory analyses included liver enzymes (AST, ALT), blood cell count, urea, creatinine, and other clinical biochemical parameters.
References
Musso CG, Enz P, Vidal F, Gelman R, Lizarraga A, Di Giuseppe L, Kowalczuk A, Garfi L, Galimberti R, Algranati L (2009) Saudi J Kidney Dis Transpl 20:1065
Brandenburg VM, Cozzolino M, Ketteler M (2011) J Nephrol 24:142
Weenig RH (2008) J Am Acad Dermatol 58:458
Nigwekar SU, Kroshinsky D, Nazarian RM, Goverman J, Malhotra R, Jackson VA, Kamdar MM, Steele DJ, Thadhani RI (2015) Am J Kidney Dis 66:133
Salmhofer H, Franzen M, Hitzl W, Koller J, Kreymann B, Fend F, Hauser-Kronberger C, Heemann U, Berr F, Schmaderer C (2013) Kidney Blood Press Res 37:346
Zitt E, König M, Vychytil A, Auinger M, Wallner M, Lingenhel G, Schilcher G, Rudnicki M, Salmhofer H, Lhotta K (2013) Nephrol Dial Transpl 28:1232
Zakharov S, Pelclova D, Navratil T, Belacek J, Kurcova I, Komzak O, Salek T, Latta J, Turek R, Bocek R, Kucera C, Hubacek JA, Fenclova Z, Petrik V, Cermak M, Hovda KE (2014) Kidney Int 86:199
Guldbakke KK, Khachemoune A (2007) Int J Dermatol 46:231
Daudén E, Oñate MJ (2008) Dermatol Clin 26:557
Rees JK, Coles GA (1969) Br Med J 2:670
Selye H, Gentile G, Prioreschi P (1961) Science 134:1876
Ketteler M, Biggar HP, Brandenburg VM, Schlieper G, Westenfeld R, Floege J (2007) Dtsch Arztebl 104:3481
Lipsker D, Chosidow O, Martinez F, Challier E, Francès C (1997) Arch Dermatol 133:798
Russell R, Brookshire MA, Zekonis M, Moe SM (2002) Clin Nephrol 58:238
Alikadic N, Kovac D, Krasna M, Lindic J, Sabovic M, Tomazic J, Jeras M, Smrke D (2009) Clin Transpl 23:968
Cicone JS, Petronis JB, Embert CD, Spector DA (2004) Am J Kidney Dis 43:1104
Zakharov S, Vaneckova M, Seidl Z, Diblik P, Kuthan P, Urban P, Navratil T, Pelclova D (2015) Basic Clin Pharmacol Toxicol 117:209
Yatzidis H (1985) Clin Nephrol 23:63
Zakharov S, Navratil T, Pelclova D (2012) Basic Clin Pharmacol Toxicol 110:427
Zakharov S, Navratil T, Pelclova D (2012) Ups J Med Sci 117:309
Yu Z, Gu L, Pang H, Fang Y, Yan H, Fang W (2015) Case Rep Nephrol Dial 5:77
Bryson DP (1996) Comprehensive reviews in toxicology: for emergency clinicians. CRC Press, p 361
Araya CE, Fennell RS, Neiberger RE, Dharnidharka VR (2006) Clin J Am Soc Nephrol 1:1161
Pasch A, Schaffner T, Huynh-Do U, Frey BM, Frey FJ, Farese S (2008) Kidney Int 74:1444
Hayden MR, Goldsmith DJ (2010) Sodium thiosulfate: new hope for the treatment of calciphylaxis. In: Seminars in dialysis, p 258
New N, Mohandas J, John GT, Ratanjee S, Healy H, Francis L, Ranganathan D (2011) Int J Nephrol ID 982854
Adirekkiat S, Sumethkul V, Ingsathit A, Domrongkitchaiporn S, Phakdeekitcharoen B, Kantachuvesiri S, Kitiyakara C, Klyprayong P, Disthabanchong S (2010) Nephrol Dial Transplant 25:1923
Farah M, Crawford RI, Levin A, Yan CC (2011) Nephrol Dial Transplant 26:191
Acknowledgments
The authors acknowledge the financial support of the Projects of the Charles University in Prague P25/1LF/2 and P28/1LF/6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
The study was approved by the General University Hospital Ethics Committee in Prague, Czech Republic.
Rights and permissions
About this article
Cite this article
Hlusicka, J., Veisova, E., Ullrych, M. et al. Serum calcium and phosphorus concentrations and the outcome of calciphylaxis treatment with sodium thiosulfate. Monatsh Chem 148, 435–440 (2017). https://doi.org/10.1007/s00706-016-1850-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00706-016-1850-3