Abstract
Crimean-Congo hemorrhagic fever (CCHF) is a tick-borne disease with a mortality rate of up to 50% in humans. To avoid safety concerns associated with the use of live virus in virus neutralization assays and to detect human serum neutralizing antibodies, we prepared lentiviral particles containing the CCHF glycoprotein (lenti-CCHFV-GP). Incorporation of the GP into the lentiviral particle was confirmed by electron microscopy and Western blotting. Lenti-CCHFV-GP was found to be able to infect a wide range of cell lines, including BHK-21, HeLa, HepG2, and AsPC-1 cells. In addition, lenti-CCHFV-GP was successfully used as an alternative to CCHFV for the detection of neutralizing antibodies. Sera collected from CCHF survivors neutralized lenti-CCHFV-GP particles in a dose-dependent manner. Our results suggest that the lenti-CCHFV-GP pseudovirus can be used as a safe tool for neutralization assays in low-containment laboratories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crimean-Congo hemorrhagic fever (CCHF) is a serious public health concern because of its high mortality rate (50%), its potential for person-to-person transmission, and the lack of specific therapies or licensed vaccines [2, 15]. Since the first description of CCHF in 1944 in Crimea, this disease has been reported in more than 31 countries in Africa, Asia, and Europe, making it the most widespread tick-borne viral infection in humans around the world [12, 21]. Recently, the World Health Organization (WHO) has categorized CCHF as one of the epidemic-prone emerging infectious diseases, prioritized by the Research and Development Blueprint [32].
CCHF virus (CCHFV) is an enveloped RNA virus belonging to the genus Orthonairovirus, family Nairoviridae [20]. Its genome comprises of three RNA segments, small (S), medium (M), and large (L), encoding a nucleoprotein (NP), viral glycoproteins (GN and GC), and an RNA-dependent RNA polymerase, respectively [34]. Phylogenetically, seven genotypes of CCHFV, including Africa-1, Africa-2, Africa-3, Asia-1, Asia-2, Europe-1, and Europe-2, have been identified [22]. The Africa 1-3 genotypes are mainly confined to African countries, while the Europe 1-2 genotypes are dominant in southeastern Europe. Asia-1 and Asia-2 are the most common genotypes in the Middle East and Central Asia, respectively [5].
Although virus neutralization assays are not routinely performed for the laboratory diagnosis of CCHFV infection, such assays can be beneficial for vaccine studies and epidemiological investigations [8, 13]. Neutralizing antibodies can be valuable indicators of vaccine efficacy as well as cross-reactivity between the vaccine and other CCHFV strains [29]. As one of the most specific serological tests, the virus neutralization assay can be used as a confirmatory method for ruling out false-positive results in enzyme-linked immunosorbent assay (ELISA) or immunofluorescence assay (IFA) due to possible cross-reactivity between CCHFV and other nairoviruses [10, 19, 30]. Moreover, a virus neutralization test is required for evaluating the potency and cross-strain neutralizing activity of monoclonal antibodies as a potential therapy against the virus [35].
CCHFV neutralization is commonly carried out using the plaque reduction neutralization test (PRNT), which relies on working with live infectious virus [6]. However, this test can be challenging for several reasons. Since CCHFV is classified as a hazard group 4 agent [31], all assays that require handling live virus, such as PRNT, must be performed in a biosafety level 4 (BSL4) laboratory, which is not available in most CCHF-endemic areas. In addition, PRNT depends on the visual examination of the cytopathic effect (CPE), and CCHFV may produce little or no CPE [6]. Furthermore, PRNT is a time-consuming technique, as it may take up to seven days to obtain the results. These limitations highlight the need to develop alternative methods for quantification of neutralizing antibodies.
A suitable alternative to PRNT is the neutralization assay using non-proliferative and safe CCHFV pseudotyped viral particles. This approach can be employed in a BSL-2 laboratory and is less time-consuming than PRNT [9]. Pseudovirus-based neutralization assays have been developed for a number of highly pathogenic viruses, such as Andes virus, Ebola virus, Japanese encephalitis virus, and Rift Valley fever virus [17, 18, 25, 27]. To develop a neutralization assay for CCHFV, Suda et al. [28] constructed a pseudotyped vesicular stomatitis virus (VSV) bearing the CCHFV glycoprotein (GP). They demonstrated that this pseudovirus could be used as a suitable alternative to conventional neutralization assays with live virus.
Lentiviral vectors (LVs) are used as a research tool because of their great packaging capacity, gene transfer efficiency, and persistent transgenic expression [27]. Pseudotyped Ebola virus (EBOV), hantavirus (HNTV), and Marburg virus (MARV) have been applied for receptor binding and entry assays as well as neutralization assays [7, 11, 14]. In the present study, generated a pseudotyped LV bearing CCHFV GP and evaluated its applicability as a tool for neutralization assays.
Materials and methods
Cells
Eight cell lines, including Lenti-X 293T (human embryonic kidney), HeLa (human cervical adenocarcinoma), A549 (human alveolar adenocarcinoma), AsPC-1 (human pancreas adenocarcinoma), MDCK (Madin-Darby canine kidney), Vero (African green monkey kidney), BHK-21 (baby hamster kidney), and HepG2 (human liver carcinoma) cells were used in this study. The cell lines were purchased from either the Iranian Biological Resources Center (IBRC, Iran) or the Pasteur Institute of Iran. All cells were cultivated in Dulbecco’s modified Eagle medium (DMEM; Gibco, USA) supplemented with 10% fetal bovine serum (FBS; Gibco, USA), 1% L-glutamine (Gibco, USA), 100 U of penicillin per mL, and 100 μg of streptomycin per mL at 37 °C in a 5% CO2 atmosphere.
Antibodies and inactivated CCHFV
CCHFV hyperimmune mouse ascitic fluid (HMAF) and inactivated CCHFV were generously provided by Dr. Amadou Sall (Institut Pasteur de Dakar, Senegal). Other antibodies used in this study included a mouse anti-HIV p24 antibody (Alpha Diagnostic Intl Inc., USA), a mouse anti-β-actin antibody (Sigma-Aldrich, USA), a rabbit anti-mouse horseradish peroxidase (HRP)-conjugated antibody (Merck Millipore, USA), an anti-mouse FITC-conjugated antibody (Santa Cruz Biotechnology, USA), and an anti-mouse IgG gold-conjugated antibody (Sigma-Aldrich, USA).
Plasmids
The codon-optimized cDNA of the CCHFV GP gene (Asia-1 genotype, strain Matin, GenBank accession no. AF467769.2) was synthesized and cloned into pcDNA3.1 (Invitrogen, USA) between the EcoRI and XbaI restriction enzyme sites (Biomatik, Canada). To increase the efficiency of protein expression, a Kozak consensus sequence (GCCGCCATGG) was inserted before the start codon. Finally, the constructed pcDNA3.1/CCHFV-GP plasmid was confirmed by enzyme digestion and sequencing (data not shown). In addition, pLOX-CWgfp (Addgene plasmid 12241, UK), the VSV-G-expressing envelope plasmid pMD2.G (Addgene plasmid 12259, Cambridge, MA, USA), and the lentivirus packaging vector psPAX2, encoding HIV-1 Gag-Pol (Addgene plasmid 12260, Cambridge, MA, USA) were purchased. The pLenti-III-mir-GFP and pLenti-III-GFP-C plasmids were purchased from ABM Inc. (USA). All plasmids were confirmed by enzyme digestion and sequencing (data not shown) and introduced into Escherichia coli DH5α strain by transformation. The plasmids used for transfection were extracted using a NucleoBond® Xtra Maxi Kit (MN, Germany) according to the manufacturer’s instructions.
Production and titration of CCHFV-GP-pseudotyped LV
To generate the CCHFV-GP-pseudotyped LV (lenti-CCHFV-GP), Lenti-X 293T cells grown in 10-cm culture plates were co-transfected with 12 µg of pLOX-CWgfp, pLenti-III-mir-GFP, or pLenti-III-GFP-C, 6 µg of psPAX2, and 6 µg of pcDNA3.1/CCHFV-GP, using Lipofectamine LTX Reagent (Invitrogen, USA). Three different reporter-encoding LVs (pLOX-CWgfp, pLenti-III-mir-GFP, and pLenti-III-GFP-C) were used in parallel to determine which LV was most efficient for pseudovirus production. Pseudovirus production was carried out on Vero and HeLa cells. The pMD2.G vector was also co-transfected with LVs and psPAX2 to generate the VSV-G pseudotype as a control. The culture medium was replaced with fresh medium after four hours. Supernatants were harvested at 48 and 72 hours post-transfection and filtered through a 0.45-µm filter.
For titration of lenti-CCHFV-GP particles, 100 µL of a tenfold serial dilution of the culture supernatant was used to transduce Lenti-X 293T, Vero, and HeLa cell lines (1 × 105 cells/well). The cells were monitored for 48 to 72 hours, trypsinized, resuspended in 1% paraformaldehyde (PFA), and titrated using a flow cytometer (Attune, Life Technologies, USA). The following formula was used to calculate the infectious titer [3]:
To normalize the viruses for experiments with different cell lines, the p24 content of each LV stock was measured using an HIV-1 P24 Antigen ELISA Kit (Xpressbio, USA) (Supplementary Table 1), and the virus was stored at -80 °C. In addition, a VSV-G-pseudotyped LV was generated and used as the control for LV production.
Immunofluorescence staining
To confirm the expression of pcDNA3.1/CCHFV-GP in Lenti-X 293T cells, an indirect immunofluorescence assay was conducted. Twenty-four hours after transfection, the cells were fixed by treatment with methanol for 10 minutes at ambient temperature. Next, they were incubated with HMAF (1:600 dilution) for one hour at 37 °C, followed by three washing steps with PBS, and then incubated with goat anti-mouse IgG conjugated with fluorescein isothiocyanate (FITC; 1:200 dilution). The slides were stained with 4′,6-diamidino-2-phenylindole (DAPI; Sigma, USA) and visualized under a fluorescence microscope (Zeiss, Germany). Untransfected 293T cells and cells transfected with the pcDNA3.1 empty vector were used as negative controls.
Western blotting
In order to examine the expression of CCHFV GP, lenti-CCHFV-GP particles and inactivated CCHFV (positive control) were denatured in a sample buffer with 10% 2-mercaptoethanol and sodium dodecyl sulfate (SDS) and incubated at 95 °C for five minutes. The Lenti-X 293T and Vero cells were lysed in a lysis buffer (50 mM Tris-HCl, pH 7.5, 150 mM NaCl, 0.5% Nonidet P-40, 50 mM NaF, 1 mM Na3VO4, 5 mM β-glycerophosphate, 1 mM dithiothreitol, and 1 mM phenylmethylsulfonyl fluoride), supplemented with a protease inhibitor cocktail (Sigma, USA), on ice. The lysates were cleared by centrifugation at 14,000g for 20 minutes and inactivated by heating with sample buffer at 95 °C for 15 minutes. Next, the heat-inactivated samples were resolved by 10-12% SDS-polyacrylamide gel electrophoresis (SDS-PAGE), and the proteins were transferred to polyvinylidene difluoride (PVDF) membranes (Sigma, USA).
Western blotting was performed using a standard method. CCHFV HMAF fluid (1:600 dilution) and HRP-conjugated anti-IgG (1:5000 dilution) were used as the primary and secondary antibody, respectively. The same method was applied to detect the expression of HIV p24 protein and β-actin, except that the primary antibody was replaced with a 1:1000 dilution of anti-p24 and anti-β-actin mouse monoclonal antibodies, and the secondary antibody was replaced with a 1:5000 dilution of HRP-labeled rabbit anti-mouse IgG antibody. Following the washing step, antibody binding was visualized using DAB reagent (Sigma, USA) according to the manufacturer’s instructions.
Immuno-transmission electron microscopy (ITEM)
Electron microscopy was performed to confirm the expression of CCHFV GP on the surface of recombinant lentivirus. The grids were covered with 15 µL of lenti-CCHFV-GP for 30 minutes and then incubated with HMAF fluid (1:1000 dilution) for two hours. After washing with PBS, the grids were incubated with a gold-conjugated anti-mouse IgG antibody (1:1000 dilution) for 30 minutes in the dark. After washing, the grids were negatively stained with 1% uranyl acetate (Sigma, USA) for 10 minutes at ambient temperature. The grids were then washed and examined using a LEO 906 electron microscope, (Zeiss, Germany).
Transduction of cells with lenti-CCHFV-GP particles
To test the capacity of CCHFV envelope proteins to infect Lenti-X 293T, HeLa, A549, AsPC-1, MDCK, HepG2, BHK-21, and Vero cells, a transduction experiment was carried out. To standardize the test and provide accurate measurements of the effect of viral packaging on the viral titer in different cells, 100 µL of lenti-CCHFV-GP and lenti-VSV-G particles at a concentration of 130 ng p24/100 µL were used to determine the relative transduction efficiency by flow cytometry. One day before infection, 1 × 105 cells/well were seeded, and 100 µL of serially diluted lenti-CCHFV-GP or lenti-VSV G particles (10−1, 10−2, 10−3, 10−4, 10−5, 10−6, 10−7, and 10−8) was added and gently mixed. After overnight incubation, the supernatant was replaced with fresh medium, and the cells were incubated for 48 hours at 37 °C. The transduction efficiency was quantified by flow cytometry. Lenti-VSV-G particles served as a positive control.
Pseudovirus infection inhibition assay
This assay was carried out to evaluate whether the infectivity of lenti-CCHFV-GP particles could be inhibited by HMAF. Twofold serial dilutions of HMAF were incubated with lenti-CCHFV-GP (100,000 TU/mL) for one hour at 37 °C. This antibody and lenti-VSV-G particles were also mixed in 96-well plates as a control. After 72 hours, the cells in each well with positive fluorescence were examined using fluorescence microscopy (Zeiss, Germany) and flow cytometry.
Assay for measuring neutralization of lenti-CCHFV-GP particles by HMAF and clinical serum samples
Three convalescent sera (sera 1-3), collected from three CCHF-recovered individuals, were used for the neutralization assay. Sera 1, 2, and 3 were collected six months, eight months, and 10 years after the onset of the disease, respectively. Before the neutralization assay, CCHFV-NP-specific IgG antibodies were quantified using a Human Crimean-Congo Hemorrhagic Fever Virus-Nucleoprotein Protein (CCHFV-NP) IgG ELISA Kit (Alpha Diagnostic, USA) according to the manufacturer’s instructions.
For the neutralization assay, serum samples and HMAF were heat-inactivated at 56 °C for 30 minutes. A twofold serial dilution of each serum and HMAF was prepared and mixed with 100,000 TU/mL of lenti-CCHFV-GP particles. After incubation for one hour, the pseudotyped virus-serum mixtures were transferred to Lenti-X 293T cells in 96-well plates (1 × 105 cells/well). After 24 hours, the cells were analyzed by flow cytometry. Neutralization efficiency was also calculated using the following formula:
The reciprocal of the dilution resulting in a 50% reduction in pseudovirus infection versus the virus without the serum was recorded as the 50% neutralizing titer (NT50). For samples without neutralization activity, such as the serum of naive individuals, NT50 was set to the lowest value obtained. In each run, a naive individual’s serum and lenti-VSV-G particles were used as controls.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 6.0 (GraphPad Software, La Jolla, CA). A one-way ANOVA test was used to compare the transduction efficiency between different LVs. A P-value less than 0.05 was considered statistically significant.
Results
Study overview
An overview of the study is presented in Figure 1. To produce lenti-CCHFV-GP particles, cells were transfected with three lentivirus-based GFP reporter constructs (pLOX-CWgfp, pLenti-III-mir-GFP, and pLenti-III-GFP-C) together with packaging and pcDNA3.1/CCHFV-GP plasmids. First, the expression of CCHFV GP was detected by immunofluorescence staining, and then, the lenti-CCHFV-GP particles were characterized by Western blotting and ITEM. The transduction efficiency of the collected lenti-CCHFV-GP particles was tested in different cell lines, using flow cytometry to assess GFP expression. Finally, an entry inhibition test was established for lenti-CCHFV-GP particles, and a neutralization assay was performed to evaluate whether the infectivity of lenti-CCHFV-GP particles could be inhibited by the HMAF and the patients’ serum samples.
Schematic representation of the study design. Lenti-X 293T cells were transfected with a plasmid expressing CCHFV Gp, the packaging plasmid and the three LV vectors. Lenti-CCHFV-Gp particles were titrated, and the transduction efficiency was tested in different cell lines. Finally, entry inhibition and neutralization assays based on lenti-CCHFV-Gp particles were performed
Analysis of CCHF Gp expression
An immunofluorescence assay was performed to assess the expression of CCHFV GP in the Lenti-X 293T cell line. For this purpose, Lenti-X 293T cells were transfected with pcDNA3.1/CCHFV-GP or the empty vector alone. Next, the cells were incubated with HMAF and stained with an anti-mouse FITC-conjugated antibody to detect the expression of CCHFV GP (Fig. 2). The assay indicated strong in vitro expression of CCHFV GP, confirming the expression of GP in the cell line producing lenti-CCHFV-GP particles (Lenti-X 293T).
Indirect immunofluorescence staining to detect expression of CCHFV Gp. Mock: Lenti-X 293T cells were transfected with empty pcDNA3.1 and stained with anti-mouse FITC-conjugated secondary antibody, and nuclei were stained with DAPI (blue, for nuclear localization). CCHFV GPC: Cells were treated with HMAF and then stained with anti-mouse FITC-conjugated secondary antibody and DAPI. Un-transfected control: Untransfected cells were incubated with HMAF and stained with anti-mouse FITC-conjugated secondary antibody and DAPI. Merge: DAPI + FITC. DAPI, diamidino-2-phenylindole; FITC, fluorescein isothiocyanate; HMAF, hyperimmune mouse ascitic fluid
Characterization of lenti-CCHFV Gp particles
CCHFV GP incorporation into the lenti-CCHFV-GP particle was examined using Western blot analysis. Western blotting was performed on lenti-CCHFV-GP particles, as well as inactivated CCHFV (positive control) (Fig. 3). In the Western blot, bands at 57 kDa (CCHFV-NP), 72 kDa (CCHFV-GC), and approximately 28 kDa (CCHFV-GN) were observed for the CCHF virion (Fig. 3A, lane 2). On the other hand, two bands at approximately 72 kDa and 28 kDa were observed for the lenti-CCHFV GP particle (Fig. 3A, lane 3). In addition, the p24 capsid protein of HIV-1 was detectable in the lenti-CCHFV-GP particle, while no p24 band was observable in the CCHFV virion (Fig. 3B, lanes 2 and 3). As expected, there were quality-control bands (Fig. 3C, lanes 2 and 3), but there was no sign of specific bands related to CCHFV GP in the two mock-infected cells (Fig. 3D, lanes 2 and 3).
Detection of CCHFV Gp in pseudovirus-containing supernatants. Samples containing lenti-CCHFV-Gp particles and supernatants from mock-transfected cells were separated on a SDS–10% polyacrylamide gel and then blotted onto a PVDF membrane. Blots were cut into strips and probed with specific antibodies. (A) Lanes 2 and 3 were probed with a specific antibody against CCHFV and lenti-CCHFV Gp particles. (B) Lanes 2 (CCHFV) and 3 (lenti-CCHFV-Gp particles) were probed with a monoclonal antibody against p24 lentivirus capsid protein. (C) Lanes 2 and 3 were probed with a specific antibody against β-actin. (D) Lanes 2 and 3 were probed with a specific antibody against CCHFV. Lane 1, protein ladder with sizes shown in kilodaltons (kDa)
ITEM of lenti-CCHFV-GP particles revealed spherical particles with a core structure and diameter of 80-120 nm. The results of ITEM demonstrated labeling of CCHFV GP on the surface of the lenti-CCHFV-GP particles (Fig. 4).
Comparison of LV titer pseudotyped with CCHFV GP
The transduction efficiency of three LVs was compared in Lenti-X 293T, Vero, and HeLa cells. All LVs (130 ng/100µL of p24) transduced Lenti-X 293T cells more efficiently than Vero or HeLa cells (Fig. 5). The transduction efficiency of pLOX-CWgfp LV was significantly higher than that of pLenti-III-GFP-C and pLenti-III-mir-GFP vectors in Lenti-X 293T cells (p < 0.0001). A similar pattern was also observed in Vero and HeLa cells. Consequently, we selected the pLOX-CWgfp LV for producing lenti-CCHFV GP particles and for further analysis.
Transduction efficiencies of lentiviral vectors. Lenti-X 293T, Vero, and HeLa cells were transduced by three LVs. The transduction efficiency of the pLOX-CWgfp lentivector was significantly higher than that of the pLenti-III-GFP-C vector and pLenti-III-mir-GFP vector in Lenti-X 293T cells. A similar pattern was observed in Vero and HeLa cells. The assay was performed in duplicate and was repeated at least two times for each cell line. LVs, lentiviral vectors, (****: p < 0.0001)
Susceptibility of cells to lenti-CCHFV GP particles
To measure viral infectivity, different cell lines were infected with lenti-CCHFV-GP and lenti-VSV-G particles at a concentration of 130 ng p24/100 µL. The infection rate was determined based on the percentage of cells expressing GFP, using flow cytometry (Fig. 6). First, to evaluate the linearity of lenti-CCHFV-GP particle infection, the cells were infected with tenfold dilutions of lenti-CCHFV-GP and lenti-VSV-G particles. The infection signal showed a proper linear range after 24 hours (Fig. 6A). The results showed that all eight cell monolayers emitted green fluorescence to some extent (Supplementary Fig. 1).
(A) CCHFV and VSV pseudovirion infection. Lenti-CCHFV-Gp and lenti-VSV-G particles (130 ng p24/100 µL) were serially diluted before incubation with Lenti-X 293T cells. (B and C) Comparison of lenti-VSV-G (B) and lenti-CCHFV-Gp particle (C) titers in different cell lines. Transduction titers of lenti-VSV-G and lenti-CCHFV-Gp particles were measured by FACS analysis. The most efficient transduction using 130 ng of p24 of lenti-VSV-G particles per 100 µL was observed in Vero, Lenti-X 293T and AsPC-1 cells (B). The most efficient transduction using of lenti-CCHFV-Gp particles 130 ng of p24 per100 µL was observed in Lenti-X 293T, BHK-21 and HepG2 cells (Fig. 6C). VSV, vesicular stomatitis virus; FACS, fluorescence-activated cell sorting; BHK, baby hamster kidney
The most efficient transduction with lenti-VSV-G particles was observed in Vero (1.4 × 107 TU/mL), Lenti-X 293T (1.3 × 107 TU/mL), and AsPC-1 (1.25 × 107 TU/mL) cells. HepG2 (5.4 × 106 TU/mL) and A549 (1.2 × 105 TU/mL) cells showed low transduction efficiency (Fig. 6B). The most efficient transduction with the lenti-CCHFV-GP particle was observed in Lenti-X 293T (1.4 × 107 TU/mL), BHK-21 (5.1 × 106 TU/mL), HepG2 (4 × 106 TU/mL), and HeLa (3.1 × 106 TU/mL) cells. AsPC-1 (4 × 105 TU/mL) and A549 (3 × 105 TU/mL) cells showed relatively low transduction, and lenti-CCHFV Gp particles could not transduce MDCK cells (Fig. 6C).
Pseudovirus infection inhibition assay and neutralization with HMAF and patients’ serum samples
To evaluate the functionality of lenti-CCHFV-GP particles for the neutralization assay, pseudovirions were pretreated with CCHFV HMAF. As shown in Fig. 7A-C, lenti-CCHFV-GP particle could not effectively infect Lenti-X 293T cells after incubation with CCHFV HMAF, while the lenti-VSV-G particle led to infection in Lenti-X 293T cells. Our results showed that an HMAF dilution of 1:1024 could completely inhibit lenti-CCHFV-GP particle infection in Lenti-X 293T cells (Fig. 7D).
Inhibition of infection by lenti-CCHFV-Gp particles. (A) Expression of fluorescence in Lenti-X 293T cells after incubation with lenti-CCHFV-Gp particles and naive serum reaction mixture. (B) Expression of fluorescence in Lenti-X 293T cells after incubation with lenti-VSV-G particles and HMAF reaction mixture. (C) No expression of fluorescence in Lenti-X 293T cells after incubation with lenti-CCHFV-Gp particles and HMAF reaction mixture. (D) HMAF at a dilution of 1:1024 was able to inhibit lenti-CCHFV-Gp particles completely, but not lenti-VSV-G particles, in Lenti-X 293T cells. Merge, FITC + bright field; HMAF, hyperimmune mouse ascitic fluid
The antigenicity of the lenti-CCHFV-GP particles was analyzed using sera obtained from CCHFV-infected patients. To monitor the neutralization of lenti-CCHFV-GP particles, 1 × 105 TU of the pseudovirus per mL was incubated with the patients’ serum samples, and the mixture was used to transduce Lenti-X 293T cells. Samples from different convalescent phases of CCHFV infection were tested by both CCHFV-NP-specific quantitative IgG ELISA and neutralization assay. According to the results of ELISA the IgG titers of sera 1-3 (collected six months, eight months, and 10 years after disease onset) were 1220, 608.2, and 519 U/mL, respectively.
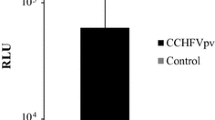
The neutralization assay showed that the three sera exhibited inhibitory activity in a dose-dependent manner despite having different NT50 titers. The NT50 titers of sera 1, 2, and 3 were 1:16, 1:8, and 1:4, respectively. The neutralization activity decreased with serum dilution, as some sera reduced the pseudovirus infection by 80% or more (Fig. 8A). The neutralization efficiency was in good agreement with the ELISA IgG titer, as the highest neutralization efficiency was observed in the serum sample with the highest IgG titer. However, no inhibition was observed when lenti-VSV-G particles were treated with the same panel of CCHFV patients’ sera, confirming the specificity of the responses (Fig. 8B). The NT50 titer of HMAF was 1:32, although no neutralization was observed when lenti-VSV-G particle was treated with HMAF, confirming the response specificity (Fig. 8C).
Neutralization of the infectivity of lenti-CCHFV-Gp particles by sera from CCHFV-infected patients. Sera against CCHFV and a naive serum were serially diluted twofold with DMEM. One hundred µL of lenti-CCHFV-Gp or lenti-VSV-G particles was mixed with anti-CCHFV serum. (A) Neutralization of lenti-CCHFV-Gp particles by serum samples from three anti-CCHFV-positive patients and naive serum. (B) Infection by lenti-VSV-G particles was not neutralized by the three CCHFV patients’ sera or naive serum. (C) Infection by lenti-CCHFV-Gp particles was neutralized by HMAF, but infection by lenti-VSV-G particles was not neutralized by HMAF. The percent neutralization was calculated relative to naive serum (mock, as naive control) (duplicate experiments, mean ± S.D.). DMEM, Dulbecco’s modified Eagle medium; HMAF, hyperimmune mouse ascitic fluid
Discussion
In the present study, we successfully produced lenti-CCHFV-GP particles. We tested LVs (pLOX-CWgfp, pLenti-III-mir-GFP, and pLenti-III-GFP-C) and found that the pLOX-CWgfp vector gave the highest pseudovirus titer, which is similar to the results published by Ahani et al. [1].
In our study, Western blotting and ITEM confirmed the incorporation of CCHFV GP on the surface of the pseudoviruses. In a Western blot, the sizes of the pseudovirus GN and GC proteins were similar to those of CCHFV GP (control). While the size of GC was similar to the estimated size of mature GC (75 KD), the GN band was approximately 28 kDa rather than 37 kDa; this difference was observed in both lenti-CCHFV-GP particles and CCHFV (positive control). Therefore, this observation might have been due to technical issues related to sample preparation for SDS-PAGE. In a recent study in which the aim was to develop a VSV-based vaccine against the CCHF envelope, Western blotting and electron microscopy were used to confirm the presence of CCHFV GP on the surface of recombinant virions [26]. In a study by Rodriguez et al. [26], differences were also observed in the expression patterns of glycoproteins in recombinant viruses and wild-type viruses. In their study, the size of GC was nearly 80 kDa, and no significant GN band was observed.
Our findings showed that lenti-CCHFV-GP particles could infect different human cell lines from various tissues, including the liver, pancreas, cervix, and lungs, with different transduction efficiencies. It is worth mentioning that no transduction was observed in MDCK cells, which are a non-human cell line with a kidney tissue origin. The highest infectivity rate was observed in cells originating from liver and kidney tissues, i.e., Lenti-X 293T and HepG2 cells. This observation is consistent with the finding that CCHFV causes a systemic infection and can replicate in various organs, including the liver, spleen, kidney, lung, and brain [23]. Also, pathogenesis studies of CCHFV have shown that the major replication sites of the virus are phagocytes, hepatocytes, and epithelial cells [23, 34].
The results of the present study suggest for the first time the possibility of CCHFV infection in the pancreas, as lenti-CCHFV-GP particles were able to infect a pancreatic cell line (AsPC-1). Although there is no evidence of CCHFV replication in pancreatic tissues, there have been clinical findings of involvement of the pancreas in CCHF. In this regard, a case of CCHF with acute pancreatitis (amylase level, 1740 U/L; lipase level, 583 U/L) was reported in Turkey [4].
The applicability of lenti-CCHFV-GP particles for neutralization tests was confirmed using both HMAF and convalescent human serum samples, which neutralized these particles in a dose-dependent manner. These results suggest that lenti-CCHFV-GP particles can be used as a safe and effective alternative to PRNT, especially in countries without access to BSL-4 facilities. In a similar study by Suda et al. [29], the applicability of a previously generated VSV-based CCHFV pseudovirus [28] in a neutralization assay was confirmed using clinical samples. Similar to our study, these authors succeeded in producing high titers of pseudovirus; however, they achieved this using a CCHFV GP with a truncated carboxyl terminus [28]. It is noteworthy that truncating the carboxyl terminus of a viral envelope protein could give rise to changes in the native folding of the surface domain and, consequently, the functional and antigenic characteristics of the pseudovirus [16]. Furthermore, they did not characterize their pseudovirus by EM or WB to confirm the incorporation of GP into the pseudotype envelope.
In the present study, serum samples with different time intervals between disease onset and sampling (serum 1, six months; serum 2, eight months; serum 3, 10 years) were used for the neutralization assay. As expected, serum 3 had the lowest neutralizing antibody titer. The other samples had neutralizing antibody titers twice and four times as high, respectively, as sample 3. The neutralization results were in agreement with the ELISA results, as the highest neutralization efficiency was seen in the serum sample with the highest IgG titer.
Generally, IgG antibody against CCHFV tends to remain at detectable levels for up to five years after the onset of disease. Our results, along with the findings of other studies from Iran and India, indicated that CCHF IgG antibody could be detected for more than five years [24, 33]. In the present study, IgG antibody was detected in a serum sample collected 10 years after the onset of disease. Similarly, Mostafavi et al. [24] detected CCHF IgG antibody almost nine years after infection with CCHFV. These findings suggest that more information is needed about the kinetics of immune responses to CCHFV.
In conclusion, the results of the present study showed that lenti-CCHFV-GP particles are a possible alternative to CCHFV for use in virus neutralization assays in BSL-2 laboratories. This system could potentially also be useful for studies investigating attachment and fusion studies of the virus. Additionally, our findings revealed that CCHF IgG and neutralizing antibodies might be detectable for at least 10 years after infection.
References
Ahani R, Roohvand F, Cohan RA, Etemadzadeh MH, Mohajel N, Behdani M, Shahosseini Z, Madani N, Azadmanesh K (2016) Sindbis virus-pseudotyped lentiviral vectors carrying VEGFR2-specific nanobody for potential transductional targeting of tumor vasculature. Mol Biotechnol 58:738–747
Al Abaidani I, Fazlalipour M, Mostafavi E, Leblebicioglu H (2017) Current status of Crimean-Congo hemorrhagic fever in WHO Eastern Mediterranean Region: issues, challenges and future directions. Int J Infect Dis 58:82–89
Barde I, Salmon P, Trono D (2010) Production and titration of lentiviral vectors. Curr Protoc Neurosci 53:21–24
Bastug A, Kayaaslan B, But A, Aslaner H, Sertcelik A, Akinci E, Onguru P, Yetkin MA, Bodur H (2014) A case of Crimean-Congo hemorrhagic fever complicated with acute pancreatitis. Vector Borne Zoonotic Dis 14:827–829
Bente DA, Forrester NL, Watts DM, McAuley AJ, Whitehouse CA, Bray M (2013) Crimean-Congo hemorrhagic fever: history, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antiviral Res 100:159–189
Berber E, Canakoglu N, Yoruk MD, Tonbak S, Aktas M, Ertek M, Bolat Y, Kalkan A, Ozdarendeli A (2013) Application of the pseudo-plaque assay for detection and titration of Crimean-Congo hemorrhagic fever virus. J Virol Methods 187:26–31
Brindley MA, Hunt CL, Kondratowicz AS, Bowman J, Sinn PL, McCray PB Jr, Quinn K, Weller ML, Chiorini JA, Maury W (2011) Tyrosine kinase receptor Axl enhances entry of Zaire ebolavirus without direct interactions with the viral glycoprotein. Virology 415:83–89
Canakoglu N, Berber E, Tonbak S, Ertek M, Sozdutmaz I, Aktas M, Kalkan A, Ozdarendeli A (2015) Immunization of knock-out α/β interferon receptor mice against high lethal dose of Crimean-Congo hemorrhagic fever virus with a cell culture based vaccine. PLoS Negl Trop Dis 9:e0003579
Carnell GW, Ferrara F, Grehan K, Thompson CP, Temperton NJ (2015) Pseudotype-based neutralization assays for influenza: a systematic analysis. Front Immunol 6:161
Casals J, Tignor GH (1980) The Nairovirus genus: serological relationships. Intervirology 14:144–147
Cifuentes-Muñoz N, Darlix J-L, Tischler ND (2010) Development of a lentiviral vector system to study the role of the Andes virus glycoproteins. Virus Res 153:29–35
Hoogstraal H (1979) The epidemiology of tick-borne Crimean-Congo hemorrhagic fever in Asia, Europe, and Africa. J Med Entomol 15:307–417
Klimov A, Balish A, Veguilla V, Sun H, Schiffer J, Lu X, Katz JM, Hancock K (2012) Influenza virus titration, antigenic characterization, and serological methods for antibody detection. Methods Mol Biol 865:25–51
Kondratowicz AS, Lennemann NJ, Sinn PL, Davey RA, Hunt CL, Moller-Tank S, Meyerholz DK, Rennert P, Mullins RF, Brindley MJ (2011) T-cell immunoglobulin and mucin domain 1 (TIM-1) is a receptor for Zaire ebolavirus and Lake Victoria Marburgvirus. Proc Natl Acad Sci USA 108(8426–843):8431
Leblebicioglu H (2010) Crimean-Congo haemorrhagic fever in Eurasia. Int J Antimicrob Agents 36:S43–S46
Li Qianqian, Liu Qiang, Huang Weijin, Li Xuguang, Wang Youchun (2018) Current status on the development of pseudoviruses for enveloped viruses. Rev Med Virol 28:e1963
Li Y, Zhao Y, Wang C, Zheng X, Wang H, Gai W, Jin H, Yan F, Qiu B, Gao Y (2018) Packaging of Rift Valley fever virus pseudoviruses and establishment of a neutralization assay method. J Vet sci 19:200–206
Liu H, Wu R, Yuan L, Tian G, Huang X, Wen Y, Ma X, Huang Y, Yan Q, Zhao Q (2017) Introducing a cleavable signal peptide enhances the packaging efficiency of lentiviral vectors pseudotyped with Japanese encephalitis virus envelope proteins. Virus Res 229:9–16
Marriott AC, Polyzoni T, Antoniadis A, Nuttall PA (1994) Detection of human antibodies to Crimean-Congo haemorrhagic fever virus using expressed viral nucleocapsid protein. J Gen Virol 75:2157–2161
Mazzola LT, Kelly-Cirino C (2019) Diagnostic tests for Crimean-Congo haemorrhagic fever: a widespread tick borne disease. BMJ Glob Health 4:e001114
Messina JP, Pigott DM, Golding N, Duda KA, Brownstein JS, Weiss DJ, Gibson H, Robinson TP, Gilbert M, William Wint G (2015) The global distribution of Crimean-Congo hemorrhagic fever. Trans R Soc Trop Med Hyg 109:503–513
Mild M, Simon M, Albert J, Mirazimi A (2010) Towards an understanding of the migration of Crimean-Congo hemorrhagic fever virus. J Gen Virol 91:199–207
Ergonul O (2007) clinical and pathologic features of Crimean-Congo hemorrhagic fever. In: Ergonul O, Whitehouse CA (eds) Crimean-Congo hemorrhagic fever, vol 8. Springer, Dordrecht, pp 123–124
Mostafavi E, Pourhossein B, Esmaeili S, Amiri FB, Khakifirouz S, Shah-Hosseini N, Tabatabaei SM (2017) Seroepidemiology and risk factors of Crimean-Congo hemorrhagic fever among butchers and slaughterhouse workers in southeastern Iran. Int J Infect Dis 64:85–89
Ray N, Whidby J, Stewart S, Hooper JW, Bertolotti-Ciarlet A (2010) Study of Andes virus entry and neutralization using a pseudovirion system. J Virol Methods 163:416–423
Rodriguez SE, Cross RW, Fenton KA, Bente DA, Mire CE, Geisbert TW (2019) Vesicular stomatitis virus-based vaccine protects mice against Crimean-Congo hemorrhagic fever. Sci Rep 9:7755
Sinn PL, Coffin JE, Ayithan N, Holt KH, Maury W (2017) Lentiviral vectors pseudotyped with filoviral glycoproteins. Methods Mol Biol 1628:65–78
Suda Y, Fukushi S, Tani H, Murakami S, Saijo M, Horimoto T, Shimojima M (2016) Analysis of the entry mechanism of Crimean-Congo hemorrhagic fever virus, using a vesicular stomatitis virus pseudotyping system. Arch Virol 161:1447–1454
Suda Y, Chamberlain J, Dowall S, Saijo M, Horimoto T, Hewson R, Shimojima M (2018) The development of a novel diagnostic assay that uses a pseudotyped vesicular stomatitis virus for the detection of neutralising activity to Crimean-Congo haemorrhagic fever virus. Jpn J Infect Dis 2017:2354
Ward VK, Marriott AC, Polyzoni T, El-Ghorr AA, Antoniadis A, Nuttall PA (1992) Expression of the nucleocapsid protein of Dugbe virus and antigenic cross-reactions with other nairoviruses. Virus Res 24:223–229
Weidmann M, Avsic-Zupanc T, Bino S, Bouloy M, Burt F, Chinikar S, Christova I, Dedushaj I, El-Sanousi A, Elaldi N (2016) Biosafety standards for working with Crimean-Congo haemorrhagic fever virus. J Gene Virol 97:2799–2808
WHO (2017) R&D Blueprint for action to prevent epidemics. http://www.who.int/blueprint/en/ . Accessed 12 Sep 2017
Yadav PD, Pardeshi PG, Patil DY, Shete AM, Mourya DT, Joi J, Health P (2019) Persistence of IgG antibodies in survivors of Crimean Congo hemorrhagic fever virus infection, India. J Infect Public Health 12:598–599
Zivcec M, Scholte F, Spiropoulou C, Spengler J, Bergeron É (2016) Molecular insights into Crimean-Congo hemorrhagic fever virus. Viruses 8:106
Zivcec M, Guerrero LI, Albariño CG, Bergeron É, Nichol ST, Spiropoulou CF (2017) Identification of broadly neutralizing monoclonal antibodies against Crimean-Congo hemorrhagic fever virus. Antiviral Res 146:112–120
Acknowledgements
The authors wish to thank all colleagues in the Department of Arboviruses and Viral Hemorrhagic Fevers at the Pasteur Institute of Iran for cooperation and excellent technical assistance. We gratefully acknowledge Gary Kobinger for scientific comments during manuscript preparation.
Funding
This research was part of a PhD thesis supported by Tehran University of Medical Sciences (Grant no. 96-04-27-36866).
Author information
Authors and Affiliations
Contributions
AAV and MSV designed and organized the study. AAV, KA, AN, MHP, MMG and MP contributed to the planning, designing and analysis of the experiments, and data collection. AAV performed the statistical analysis. AAV, SS and MSV provided materials and analysis tools. AAV, MSV, KA and SS wrote and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures involving human patients were performed in accordance with the ethical standards of the Ethical Committee of Tehran University of Medical Science (Ethical Code No: 96-04-27-36866).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Handling Editor: Hideki Ebihara.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vasmehjani, A.A., Salehi-Vaziri, M., Azadmanesh, K. et al. Efficient production of a lentiviral system for displaying Crimean-Congo hemorrhagic fever virus glycoproteins reveals a broad range of cellular susceptibility and neutralization ability. Arch Virol 165, 1109–1120 (2020). https://doi.org/10.1007/s00705-020-04576-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-020-04576-9