Abstract
The use of opioids for the relief of pain and headache disorders has been studied for years. Nowadays, particularly because of its ability to produce analgesia in various pain models, delta opioid receptor (DOPr) emerges as a promising target for the development of new pain therapies. Indeed, their potential to avoid the unwanted effects commonly observed with clinically used opioids acting at the mu opioid receptor (MOPr) suggests that DOPr agonists could be a therapeutic option. In this review, we discuss the use of opioids in the management of pain in addition to describing the evidence of the analgesic potency of DOPr agonists in animal models.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Opioids are extensively used for the treatment of moderate to severe pain. Opioid compounds, as well as endogenous opioid peptides, produce their effects on neurotransmission through the activation of opioid receptors (Bodnar 2019). There are three different opioid receptors named mu (MOPr), delta (DOPr) and kappa (KOPr) (Kieffer and Gaveriaux-Ruff 2002). While the MOPr is the major target of commonly used opioids, its activation by morphine or other opioids induces important adverse effects (Al-Hasani and Bruchas 2011; McQuay 1999). In this review, we briefly describe the major pain pathways and the distribution of DOPr along those pathways. Finally, an overview of the analgesic effects of DOPr agonists in different preclinical models is provided, together with the conclusion of clinical trials investigating the role of DOPr agonists for pain.
Pain
The International Association for the Study of Pain (IASP) qualifies pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” Pain is a complex and subjective process experienced at an individual level. Nowadays, numerous medications such as NSAID (Non-Steroidal Anti-Inflammatory Drugs) and opioids are used to alleviate acute and chronic pain. Despite their important analgesic potency, opioids are not always well tolerated by their users and often not suitable for a given pain condition. A combination of analgesics is sometimes required, further exacerbating unwanted effects (McQuay 1999). Most opioids currently used in the clinic bind MOPr (Smith and Peppin 2014). However, the activation of this receptor is also responsible for the common unwanted effects associated with opioids. Indeed, the most important adverse effects of opioids are constipation, tolerance, addiction, respiratory depression and sedation (Bailey and Connor 2005). Those effects are particularly debilitating and therefore restrain the usefulness of MOPr agonists under chronic pain conditions. On the other hand, DOPr agonists produce antinociception with less unwanted effects than the currently used opioids (Bodnar 2019; Gaveriaux-Ruff and Kieffer 2011; Gendron et al. 2015). Most importantly, it is generally accepted that DOPr agonists do not produce abuse potential (Negus et al. 1998).
Pain pathways
Pain transmission involves two major pathways (for reviews see Basbaum et al. 2009 and Yam et al. 2018). The first, known as the ascending pain pathway, is characterized by a neuronal circuit capable of integrating signals generated by a wide variety of noxious stimuli. More specifically, the ascending pathway is activated when stimuli from thermal, mechanical or chemical sources activate a first-order neuron known as nociceptor. Activated nociceptors relay the noxious signals to the spinal cord by releasing excitatory neurotransmitters on second-order neurons. The latter, called projection neurons, are then activated and transmit the information to the thalamus which in turn signals to the somatosensory cortex, the insula, and the cingulate cortex.
The second pathway implicated in pain processing is the descending pain pathway. This pathway is known to play a modulatory role. Indeed, a phenomenon best known as “diffuse noxious inhibitory controls” (DNIC) previously described by Le Bars plays a major role in the modulation of pain (Le Bars et al. 1992). DNIC, now termed conditioned-pain modulation (CPM) in human, involves specific supraspinal structures such as subnucleus reticularis dorsalis (SRD) (Le Bars et al. 1992). Besides SRD, other structures in the CNS such as the hypothalamus, the amygdala, the periaqueductal gray (PAG) and the rostro-ventral medulla (RVM) play a role in the modulation of noxious stimuli through their projections to the spinal cord. Interestingly, all three opioid receptors (MOPr, DOPr and KOPr) and their endogenous peptides are present at different levels along these pain pathways where they can participate in the modulation of pain (Al-Hasani and Bruchas 2011).
Another important pain circuit is the trigeminal pain pathway (Bicanic et al. 2019). The trigeminal system innervates the head and is therefore responsible for sensing mechanical, thermal and chemical stimuli applied to the head/face. When compared to the ascending pain pathway described above, this specific pathway takes a different path to the thalamus. To begin, noxious stimuli are perceived by trigeminal ganglia neurons. These neurons have projections in the brainstem, to the spinal trigeminal nucleus (Sp5) in the medulla. From there, a second-order neuron relays the information to the thalamus.
Distribution and trafficking of DOPr in the CNS
As opioid peptides and their specific receptors play a critical role in the relief of pain, it is not surprising that MOPr, DOPr and KOPr are expressed in the CNS, along the pain pathways. For the purpose of this review, the distribution of DOPr will be further discussed. However, one may refer to a recently published interactive MOPr and DOPr brain atlas (Erbs et al. 2015). DOPr is highly expressed in the forebrain in regions such as the amygdala, the cortex, the striatum and the olfactory bulb (Mansour et al. 1994). Furthermore, some structures implicated in pain transmission such as the rostro-ventral medulla (RVM), the parabrachial nucleus, the hypothalamus, the thalamus and the periaqueductal gray area (PAG) contain DOPr (Erbs et al. 2015; Mansour et al. 1994). Interspecies differences in the distribution of DOPr were however observed. Indeed, autoradiography studies revealed that in mice and rats, DOPr is expressed throughout the spinal cord gray matter. Interestingly, in monkeys and humans, DOPr is mainly located in the superficial lamina (laminae I-II) (Mennicken et al. 2003).
If the presence of DOPr in various regions of the brain and in the ascending and descending pain pathways has been well documented (Cahill et al. 2001a; Mansour et al. 1995, 1994; Mennicken et al. 2003), the identity of DRG neurons expressing this receptor remains controversial. At first, DOPr was found in all types of DRG neurons (Dado et al. 1993; Gendron et al. 2006; Mansour et al. 1994; Mennicken et al. 2003). Using a genetically engineered mouse model, Scherrer and colleagues rather observed that a fluorescent DOPr chimera (DOPr-eGFP) was mainly expressed in large myelinated, non-nociceptive neurons (Bardoni et al. 2014; Scherrer et al. 2006). This is in sharp contrast with what was observed by others. Indeed, DOPr was found in large dense core vesicles (LDCV), associated with preprotachykinin A (Guan et al. 2005), as well as in substance P-containing terminals (Riedl et al. 2009). DOPr was also found to regulate substance P release from primary afferents (Beaudry et al. 2011; Kouchek et al. 2013; Normandin et al. 2013) and to synergize with the α2A-adrenergic receptors in peptidergic neurons (Schuster et al. 2013). Using the DOPr-eGFP mouse model, a very low level of coexpression between DOPr with substance P, CGRP or TRPV1 was observed (Scherrer et al. 2009). Absence of DOPr in small DRG neurons is also supported by single-cell RNA-sequencing of mouse sensory neurons (Usoskin et al. 2015). Nowadays, it remains unclear if this discrepancy comes from interspecies differences, lack of specificity in the approaches, or an artifact from the eGFP-tagged receptor.
Although DOPr is highly expressed in the CNS, its subcellular localization is atypical when compared to other class A G protein-coupled receptors (GPCRs). Indeed, various experimental approaches revealed that DOPr is mainly located in the cytoplasm, associated with various membrane structures and organelles, with a very low level of receptors being associated with the plasma membrane (Cahill et al. 2001a; Cheng et al. 1995; Gendron et al. 2006; Pasquini et al. 1992; Zhang et al. 1998). This particular location makes it harder to target DOPr and might explain why selective DOPr agonists show only weak antinociceptive effects under normal conditions (Cahill et al. 2007; Zhang et al. 2010). We and others have however shown that the level of DOPr at the cell surface can be increased with a chronic treatment with morphine or under chronic pain conditions (Cahill et al. 2001a, b, 2003; Gendron et al. 2006; Lucido et al. 2005; Morinville et al. 2003, 2004). Most interestingly, this increase in DOPr at the cell surface is paralleled by an improvement of the analgesic effects of DOPr agonists (Cahill et al. 2001b, 2003; Gendron et al. 2007a, b; Morinville et al. 2003) as well as by an increase in DOPr functions (Hack et al. 2005; Pradhan et al. 2013a). Finding ways to improve the delivery of DOPr at the cell surface could therefore help identify novel analgesic compounds with reduced unwanted effects. Admittedly, increasing DOPr at the cell surface, including in chronic pain models, may as well reveal unwanted effects and reinforcement. In the context of chronic pain, measuring reinforcement of drugs is however challenging. Indeed, because pain is aversive, non-addictive drugs effectively produce place preference in chronic pain models (King et al. 2009).
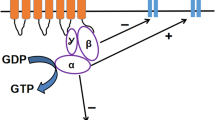
Because they do not reach the brain, peripherally restricted agonists are devoid of centrally mediated unwanted effects affecting mood and emotions. As for central DOPr, peripheral DOPr appears to be incompetent and, to be effective, peripherally restricted DOPr agonists need some sort of priming (Gaveriaux-Ruff et al. 2008; Patwardhan et al. 2005, 2006; Pettinger et al. 2013; Rowan et al. 2009; Stein et al. 1989). In fact, although DOPr is present at the plasma membrane of peripheral sensory neurons, it is weakly activated following agonist binding (Brackley et al. 2016, 2017). Bradykinin (BK) is known to play an important role in the awakening of DOPr functionality in peripheral sensory neurons. In these neurons, GRK2 was found to constitutively associate with DOPr at the plasma membrane through a mechanism involving PKA and AKAP (Brackley et al. 2017). The GRK2–DOPr interaction prevents the association between DOPr and the Gβ subunit, and by way of consequence the agonist efficacy. Interestingly, BK was found to promote the dissociation of GRK2 and DOPr and to increase its association with Raf kinase inhibitory protein (RKIP). The protein kinase C (PKC)-dependent phosphorylation of RKIP sequesters GRK2, restoring the functionality of DOPr in peripheral sensory neurons (Brackley et al. 2016).
DOPr in pain conditions
DOPr agonists represent a great alternative to commonly used opioids to treat acute and chronic pain, because they produce fewer and milder unwanted effects. DOPr agonists also have anxiolytic and anti-depressive effects (Broom et al. 2002b, c; Chu Sin Chung and Kieffer 2013), two important comorbidities of chronic pain (Goldenberg 2010a, b). As stated above (but see also the next section), DOPr agonists have no or very weak antinociceptive effects in acute pain models. In addition, DOPr was not found to participate in the endogenous analgesic tone in normal animals submitted to acute pain tests (Filliol et al. 2000; Zhu et al. 1999). Interestingly, DOPr-KO mice are more sensitive to noxious stimuli in models of chronic inflammatory and neuropathic pain (Gaveriaux-Ruff et al. 2008; Nadal et al. 2006). Together, these observations suggest that DOPr plays an important role in modulating chronic pain, but is less effective against acute pain. The exact reasons why DOPr is more competent in chronic pain models than in acute pain models remain unclear. As mentioned above, the intracellular localization of the receptor in a naive state is one of the current working hypotheses. It is thought that under chronic pain conditions, DOPr expressed in neurons of the CNS can escape the maturation process more efficiently, increasing the density of membrane receptors (Gendron et al. 2016). Chronic pain may modify the interaction of DOPr with various proteins (kinases, chaperones, etc.) to promote this process (Beaudry et al. 2015b; Shiwarski et al. 2019; St-Louis et al. 2017; Xie et al. 2009). In the periphery, DOPr appears to stand incompetent at the plasma membrane of sensory neurons. Inflammation (this is to say chronic inflammatory pain) acts as a “priming” signal to reinstate the functions of DOPr and agonists efficacy. The mechanisms involved in this process have recently been reviewed elsewhere (Jeske 2019).
DOPr in acute pain models
Evidence for DOPr-mediated antinociceptive effects in acute pain tests are shown in Table 1.
Thermal pain
Thermal pain is usually used to test the acute reaction to a warm/hot stimulus such as hot water, radiant heat or a hot plate. Comparison of the latency to tail withdrawal is made before and after the administration of an analgesic compound. Generally speaking, MOPr agonists are known to produce more profound analgesia than DOPr agonists in such experimental settings. As an example, pioneer studies showed that the administration of the MOPr agonist DAMGO (H-Tyr-d-Ala-Gly-MePhe-Gly-ol) produces a more potent analgesia than the DOPr agonist [D-Pen2,5]-Enkephalin (DPDPE) in the hot plate test (Porreca et al. 1984). In the tail flick test, central or systemic administration of SNC80 (a delta-selective agonist) produced a time- and dose-dependent antinociceptive effect (Bilsky et al. 1995). The antinociceptive effect peaked at 10 min following the i.c.v. and i.t. administration and 30 min after the i.p. injection of SNC80. SNC80 also produces antinociception in the hot plate test following i.c.v. administration, an effect that was blocked by the selective DOPr antagonist naltrindole (Bilsky et al. 1995). The antinociceptive effects of the peptidic DOPr-selective agonist deltorphin II was also described in various pain assays, including tail flick, hot plate and Hargreaves plantar tests (Cahill et al. 2001b; Dubois and Gendron 2010; Fraser et al. 2000a; Rossi et al. 1994).
Mechanical pain
Mechanical pain is often described as a sensitivity to mechanical stimuli. To test the acute mechanical pain, tests such as von Frey and paw pressure (Randall-Selitto test) can be used. A pioneer study showed that the i.c.v administration of either deltorphin II or SNC80 in rats produced a peak antinociceptive effect in the paw pressure test 15 min after the injection (Fraser et al. 2000b). Interestingly, the effects were similar in amplitude as the antinociception produced by i.c.v. DAMGO; this is to say that all three agonists were able to reduce the nociception by 80%, suggesting that both DOPr or MOPr produce equivalent analgesia in this model. By contrast, the effect of i.p. SNC80 in naïve mice and in CFA-treated mice assessed with the von Frey test revealed no effect of SNC80 in the naïve mice, but a significant antinociceptive effect was noted in CFA-injected mice (Pradhan et al. 2013a).
Chemical pain (acute inflammatory pain)
Even if, as described above, DOPr agonists produce weak antinociceptive effects in acute pain models, they were found to potently relieve acute inflammatory pain. Indeed, numerous groups confirmed the analgesic effects of delta agonists in both the capsaicin and the formalin tests. Deltorphin II was found to significantly reduce nocifensive behaviors induced by capsaicin and formalin in rodents (Beaudry et al. 2011; Bilsky et al. 1996a; Cahill et al. 2001b; Kabli and Cahill 2007; Morinville et al. 2003; Pradhan et al. 2006). The analgesic effects of SNC80 was also tested for chemical pain using different routes of administration (s.c., i.pl., i.v. and i.t.) and in various species. This agonist reduces pain-like behaviors induced by capsaicin and formalin (Barn et al. 2001; Brandt et al. 2001; Kouchek et al. 2013; Obara et al. 2009). Two groups have shown that the activation of DOPr produced an inhibition of substance P release as well as a decrease in c-fos expression within the spinal cord, suggesting that DOPr agonists are able to block noxious stimuli-induced spinal neurons activation (Beaudry et al. 2011; Kouchek et al. 2013).
DOPr in chronic pain models
DOPr agonists are known to produce robust antinociceptive effects in chronic pain models, possibly because the density of the receptor at the cell surface is increased under such conditions (Gendron et al. 2016). Indeed, DOPr agonists effectively alleviate pain in animal models of inflammatory, cancer, neuropathic and migraine pain. The effects of DOPr agonists in chronic pain models are summarized in Table 2.
Chronic inflammatory pain models: complete Freund’s adjuvant (CFA) and carrageenan
Complete Freund’s adjuvant (CFA) and carrageenan are often used as chronic inflammatory pain models. Although they do not perfectly mimic the human disease, they are often used as animal models of arthritis. In rat and mouse CFA models of inflammation, the i.t. injection of deltorphin II produced a time- and dose-dependent antihyperalgesic effects in the Hargreaves plantar test (Beaudry et al. 2009; Dubois and Gendron 2010; Gendron et al. 2007a). Deltorphin II also produced a dose-dependent, DOPr-mediated analgesic effect in the rat CFA model assessed for mechanical hypersensitivity with the von Frey test (Otis et al. 2011). Others have shown the efficacy of deltorphin II in this model using different routes of administration (Fraser et al. 2000a; Qiu et al. 2000). Another DOPr agonist derived from codeine was tested in the rat CFA model of inflammation using the plantar test. Subcutaneous injection of SB-235863 had a significant antihyperalgesic effect when compared to the vehicle group (Beaudry et al. 2009). SNC80 was also used in the plantar and the von Frey tests in the mouse CFA model. Both i.p. and s.c. injections of SNC80 produced antihyperalgesic and antiallodynic effects that were absent in DOPr-KO mice, supporting a specific role for DOPr (Gaveriaux-Ruff et al. 2008; Pradhan et al. 2013b). Similarly, i.c.v. and s.c. SNC80 induced antihyperalgesic effects in the rat CFA model of inflammation (Fraser et al. 2000a; Gallantine and Meert 2005). Interestingly, this small molecule agonist further produced analgesia in monkeys when administrated s.c. (Brandt et al. 2001). Finally, DPDPE injected i.t. or i.pl. produced analgesia in these models as well (Hervera et al. 2009; Qiu et al. 2000; Zhu et al. 1998).
Using carrageenan as the inflammatory agent, the four agonists mentioned above (Delt II, SB-235863, SNC80 and DPDPE) were also effective in reducing the thermal hyperalgesia and allodynia in rats following i.t. and p.o. administration (Kouchek et al. 2013; Petrillo et al. 2003; Stewart and Hammond 1994).
Cancer pain
Bone cancer-induced pain shares commonalities with both inflammatory and mechanical pain states. However, we know that it has its own characteristics and should therefore be considered in a different category (Honore et al. 2000). The putative analgesic effects of DOPr agonists were assessed in this paradigm by several groups. Following s.c. peritumoral injections of DPDPE 4 weeks after the inoculation of cancer cells (NCTC 2472) in mice, a dose-dependent analgesia was observed in the unilateral hot plate test (Baamonde et al. 2005). Using a different mouse model of bone cancer-induced pain, Brainin-Mattos and colleagues found that an intraperitoneal injection of [dVal(L)2,Ala(L)5]E was effective in reducing allodynia (Brainin-Mattos et al. 2006). Interestingly, the maximal effect produced by this DOPr agonist was comparable to the effects observed following morphine injection (Brainin-Mattos et al. 2006). Calculation of the ED50 for morphine (5.29 ± 1.91 mg/kg) and [dVal(L)2,Ala(L)5]E (1.34 ± 0.31 mg/kg) confirmed the high potency of the DOPr agonist in this model (Brainin-Mattos et al. 2006). In other studies, i.pl. SNC80 and i.t. deltorphin II were also able to reduce the mechanical pain induced by von Frey hairs in mouse and rat models of cancer pain (Otis et al. 2011; Ye et al. 2012).
Neuropathic pain
Preclinical models of neuropathic pain were used to test the effects of DOPr agonists in this specific condition. Using a model of sciatic nerve injury in Wistar rats, deltorphin II and DPDPE injected intrathecally produced an antiallodynic effect in thermal pain tests (Mika et al. 2001). The effects of deltorphin II was also assessed in a model of chronic constriction injury with the thermal pain test (cold) and the von Frey test (Holdridge and Cahill 2007). Deltorphin II was found to produce anti-hyperalgesia and an anti-allodynic effects 14 days after the injury (Holdridge and Cahill 2007). Other DOPr agonists such as DSLET, SNC80 and SB-235863 proved to be potent in preclinical models of neuropathic pain in rats (Obara et al. 2009; Petrillo et al. 2003).
Migraine pain
Drugs such as triptans (sumatriptan) are often used for the treatment of migraine, but in some case patients remain unresponsive. In some instance, such as the severity of migraine, MOPr agonists can be used (Bigal and Lipton 2009; Buse et al. 2012; Thorlund et al. 2016). However, a phenomenon called opioid-induced hyperalgesia (OIH) can appear in patients using opioids repeatedly for migraine headaches. In fact, the use of morphine is only rarely devoid of undesired effects. When used to treat migraine, opioids were found to play a key role in the transition from episodic to chronic migraine problems (Bigal and Lipton 2009; Buse et al. 2012; Thorlund et al. 2016). If the use of MOPr agonists is worrisome at a time when we face a major opioid crisis, the difference in DOPr and MOPr expression in the trigeminal complex could lean toward DOPr as a great alternative. Using [125I]-deltorphin II, Mennicken and colleagues revealed the distribution of DOPr in the Sp5 of rats and humans (Mennicken et al. 2003). They also described the distribution of DOPr mRNA in the Sp5 of rats and humans. A recent review by Charles and Pradhan summarized these observations and discussed the potential of DOPr agonists for the treatment of migraine (Charles and Pradhan 2016). In recent years, several groups have developed preclinical models of rodents to test new migraine therapies. Among these models, nitroglycerin (NTG) and isosorbide dinitrate (ISDN), two nitric oxide donors, were used to mimic migraine headaches (Dallel et al. 2018; Pradhan et al. 2014). Using the NTG model, Pradhan and colleagues showed the effectiveness of SNC80 to produce an antiallodynic effect similar to the one seen with sumatriptan (the most used treatment for migraine) (Moye et al. 2019a, b). SNC80 was able to reduce the thermal and mechanical hyperalgesia induced by NTG (Pradhan et al. 2014). In addition, at 10 mg/kg, the DOPr agonist injected i.p. reversed the conditioned place aversion caused by the NTG administration (Pradhan et al. 2014). Cortical spreading depression (CSD), which is a migraine symptom often correlated with migraine accompanied by aura, was also inhibited by SNC80 as measured by electrophysiological procedures (Pradhan et al. 2014). Using the ISDN model, a cephalic and extracephalic mechanical hypersensitivity was observed and correlated with a migraine progression depending on the number of doses of ISDN given to rodents (Dallel et al. 2018). Treatments usually prescribed for migraine therapy such as olcegepant, sumatriptan and propranolol were also tested in this second migraine model. All three treatments showed analgesic efficacy, but only under specific conditions. For example, olcegepant significantly reduces the cephalic allodynia after a single and after repeated injections of ISDN (10 mg/kg, i.p.), but sumatriptan only alleviates the cephalic allodynia after a single injection of ISDN (Dallel et al. 2018). Propranolol, known as the preventive therapy for migraine treatment, significantly reduced the cephalic allodynia only after repeated doses of ISDN (Dallel et al. 2018). These interesting results provide a new migraine model similar to the NTG one and may be another model on which the analgesic potential of delta agonists could be investigated. In parallel, studying these two models will also provide a better understanding of the migraine mechanisms.
Development of analgesic tolerance to DOPr agonists
Because a large body of evidence showed a great efficacy of DOPr agonists in different pain models (see above), their potential as alternative therapeutics is of considerable interest. However, a possible problem that arises from the use of such molecules is the fact that tolerance can rapidly develop making them less adapted to the treatment of chronic pain. Indeed, it was found that the high-internalizing agonist SNC80 results in the desensitization of DOPr and produces analgesic tolerance (Pradhan et al. 2016). Arrestin 2 was found to play an essential role in this process, since in KO mice drug potency and duration of action are increased, while acute tolerance to the antihyperalgesic effects of SNC80 is reduced (Vicente-Sanchez et al. 2018). However, low-internalizing agonists ARM390 and JNJ20788560 do not produce tolerance unless arrestin 3 is depleted (Pradhan et al. 2016). Absence of tolerance in animal models of pain was also observed with another low-internalizing agonist, SB-235863 (Beaudry et al. 2009; Petrillo et al. 2003). More recently, it was observed that agonists supporting recycling of DOPr produce minimal tolerance (Audet et al. 2012; Charfi et al. 2018). The fact that the development of analgesic tolerance is agonist dependent raises the possibility of developing a drug with minimal risk of tolerance.
DOPr in clinical trials
As described above, DOPr agonists represent a tempting target for the treatment of chronic, inflammatory, neuropathic and migraine pain. As DOPr produces less respiratory depression, tolerance and constipation than MOPr agonists, its activation represents a promising alternative to commonly used opioids. One of the major problems with DOPr agonists is their propensity to induce nonlethal convulsions (Broom et al. 2002a, d; Chung et al. 2015). This adverse effect makes it difficult to bring such molecules to the clinic. Nonetheless, DOPr agonists have reached clinical trials for the treatment of various pathologies and conditions, including pain (Spahn and Stein 2017). Two compounds, ADL5747 and ADL5859, were tested in clinical trials for pain problems (Le Bourdonnec et al. 2008, 2009). In phase I clinical trial, ADL5859 did not induce the adverse events often seen with DOPr agonists (convulsions and locomotor alterations) even with doses as high as 1000 mg/kg. Unfortunatley, ADL5859 showed no better effect than the placebo and ibuprofen after dental surgery. Following this result, three other studies used the DOPr agonist for inflammatory rheumatoid arthritis, diabetes-induced peripheral neuropathy and osteoarthritic pain. No significant findings emerged from these trials. Again, a lack of efficacy over placebo was reported. Two phase II clinical trials looking at the therapeutic effects of ADL5747 in osteoarthritic pain and postherpetic neuralgia were also performed. As for ADL5859, in these trials the parent compound ADL5747 was not more effective than the placebo. The exact reasons why these compounds failed to produce significant analgesic effects in these trials remain unknown. One can argue that the design of the trial was not optimal. Indeed, it is worth mentioning that oxycodone, used as a positive control, also failed to produce a better analgesic effect than the placebo. New trials are certainly needed before we can conclude on the potential therapeutic effects of DOPr agonists.
Conclusion
As described in this review, targeting DOPr represents a promising alternative to develop novel therapies for the treatment of chronic inflammatory, neuropathic, cancer and migraine pain. Despite the current evidence for the analgesic effects of DOPr agonists under each condition, more research is needed to better understand the mechanisms involved in DOPr trafficking, but also to better describe its role in modulating pain.
References
Al-Hasani R, Bruchas MR (2011) Molecular mechanisms of opioid receptor-dependent signaling and behavior. Anesthesiology 115:1363–1381. https://doi.org/10.1097/ALN.0b013e318238bba6
Audet N et al (2012) Differential association of receptor-Gbetagamma complexes with beta-arrestin2 determines recycling bias and potential for tolerance of delta opioid receptor agonists. J Neurosci 32:4827–4840. https://doi.org/10.1523/JNEUROSCI.3734-11.2012
Baamonde A, Lastra A, Juarez L, Garcia V, Hidalgo A, Menendez L (2005) Effects of the local administration of selective mu-, delta-and kappa-opioid receptor agonists on osteosarcoma-induced hyperalgesia Naunyn Schmiedebergs. Arch Pharmacol 372:213–219. https://doi.org/10.1007/s00210-005-0013-6
Bailey CP, Connor M (2005) Opioids: cellular mechanisms of tolerance and physical dependence. Curr Opin Pharmacol 5:60–68. https://doi.org/10.1016/j.coph.2004.08.012
Bardoni R et al (2014) Delta opioid receptors presynaptically regulate cutaneous mechanosensory neuron input to the spinal cord dorsal horn. Neuron 81:1312–1327. https://doi.org/10.1016/j.neuron.2014.01.044
Barn DR, Caulfield WL, Cottney J, McGurk K, Morphy JR, Rankovic Z, Roberts B (2001) Parallel synthesis and biological activity of a new class of high affinity and selective delta-opioid ligand. Bioorg Med Chem 9:2609–2624. https://doi.org/10.1016/s0968-0896(01)00017-7
Basbaum AI, Bautista DM, Scherrer G, Julius D (2009) Cellular and molecular mechanisms of pain. Cell 139:267–284. https://doi.org/10.1016/j.cell.2009.09.028
Beaudry H, Dubois D, Gendron L (2011) Activation of spinal mu- and delta-opioid receptors potently inhibits substance P release induced by peripheral noxious stimuli. J Neurosci 31:13068–13077. https://doi.org/10.1523/JNEUROSCI.1817-11.2011
Beaudry H, Gendron L, Moron JA (2015a) Implication of delta opioid receptor subtype 2 but not delta opioid receptor subtype 1 in the development of morphine analgesic tolerance in a rat model of chronic inflammatory pain. Eur J Neurosci 41:901–907. https://doi.org/10.1111/ejn.12829
Beaudry H, Mercier-Blais AA, Delaygue C, Lavoie C, Parent JL, Neugebauer W, Gendron L (2015b) Regulation of mu and delta opioid receptor functions: involvement of cyclin-dependent kinase 5. Br J Pharmacol 172:2573–2587. https://doi.org/10.1111/bph.13088
Beaudry H, Proteau-Gagne A, Li S, Dory Y, Chavkin C, Gendron L (2009) Differential noxious and motor tolerance of chronic delta opioid receptor agonists in rodents. Neuroscience 161:381–391. https://doi.org/10.1016/j.neuroscience.2009.03.053
Bicanic I, Hladnik A, Dzaja D, Petanjek Z (2019) The anatomy of orofacial innervation. Acta Clin Croat 58:35–42. https://doi.org/10.20471/acc.2019.58.s1.05
Bigal ME, Lipton RB (2009) Overuse of acute migraine medications and migraine chronification. Curr Pain Headache Rep 13:301–307. https://doi.org/10.1007/s11916-009-0048-3
Bilsky EJ, Bernstein RN, Hruby VJ, Rothman RB, Lai J, Porreca F (1996a) Characterization of antinociception to opioid receptor selective agonists after antisense oligodeoxynucleotide-mediated "knock-down" of opioid receptor in vivo. J Pharmacol Exp Ther 277:491–501
Bilsky EJ et al (1995) SNC 80, a selective, nonpeptidic and systemically active opioid delta agonist. J Pharmacol Exp Ther 273:359–366
Bilsky EJ, Wang T, Lai J, Porreca F (1996b) Selective blockade of peripheral delta opioid agonist induced antinociception by intrathecal administration of delta receptor antisense oligodeoxynucleotide. Neurosci Lett 220:155–158. https://doi.org/10.1016/s0304-3940(96)13262-6
Bodnar RJ (2019) Endogenous opiates and behavior: 2017. Peptides. https://doi.org/10.1016/j.peptides.2019.170223
Brackley AD, Gomez R, Akopian AN, Henry MA, Jeske NA (2016) GRK2 constitutively governs peripheral delta opioid receptor activity. Cell Rep 16:2686–2698. https://doi.org/10.1016/j.celrep.2016.07.084
Brackley AD, Sarrami S, Gomez R, Guerrero KA, Jeske NA (2017) Identification of a signaling cascade that maintains constitutive delta-opioid receptor incompetence in peripheral sensory neurons. J Biol Chem 292:8762–8772. https://doi.org/10.1074/jbc.M117.776799
Brainin-Mattos J, Smith ND, Malkmus S, Rew Y, Goodman M, Taulane J, Yaksh TL (2006) Cancer-related bone pain is attenuated by a systemically available delta-opioid receptor agonist. Pain 122:174–181. https://doi.org/10.1016/j.pain.2006.01.032
Brandt MR, Furness MS, Mello NK, Rice KC, Negus SS (2001) Antinociceptive effects of delta-opioid agonists in Rhesus monkeys: effects on chemically induced thermal hypersensitivity. J Pharmacol Exp Ther 296:939–946
Broom DC, Jutkiewicz EM, Folk JE, Traynor JR, Rice KC, Woods JH (2002a) Convulsant activity of a non-peptidic delta-opioid receptor agonist is not required for its antidepressant-like effects in Sprague-Dawley rats. Psychopharmacology 164:42–48
Broom DC, Jutkiewicz EM, Folk JE, Traynor JR, Rice KC, Woods JH (2002b) Nonpeptidic delta-opioid receptor agonists reduce immobility in the forced swim assay in rats. Neuropsychopharmacology 26:744–755
Broom DC, Jutkiewicz EM, Rice KC, Traynor JR, Woods JH (2002c) Behavioral effects of delta-opioid receptor agonists: potential antidepressants? Jpn J Pharmacol 90:1–6
Broom DC, Nitsche JF, Pintar JE, Rice KC, Woods JH, Traynor JR (2002d) Comparison of receptor mechanisms and efficacy requirements for delta-agonist-induced convulsive activity and antinociception in mice. J Pharmacol Exp Ther 303:723–729
Buse DC, Pearlman SH, Reed ML, Serrano D, Ng-Mak DS, Lipton RB (2012) Opioid use and dependence among persons with migraine: results of the AMPP study. Headache 52:18–36. https://doi.org/10.1111/j.1526-4610.2011.02050.x
Cahill CM, Holdridge SV, Morinville A (2007) Trafficking of delta-opioid receptors and other G-protein-coupled receptors: implications for pain and analgesia. Trends Pharmacol Sci 28:23–31. https://doi.org/10.1016/j.tips.2006.11.003
Cahill CM, McClellan KA, Morinville A, Hoffert C, Hubatsch D, O'Donnell D, Beaudet A (2001a) Immunohistochemical distribution of delta opioid receptors in the rat central nervous system: evidence for somatodendritic labeling and antigen-specific cellular compartmentalization. J Comp Neurol 440:65–84. https://doi.org/10.1002/cne.1370
Cahill CM, Morinville A, Hoffert C, O'Donnell D, Beaudet A (2003) Up-regulation and trafficking of delta opioid receptor in a model of chronic inflammation: implications for pain control. Pain 101:199–208
Cahill CM, Morinville A, Lee MC, Vincent JP, Collier B, Beaudet A (2001b) Prolonged morphine treatment targets delta opioid receptors to neuronal plasma membranes and enhances delta-mediated antinociception. J Neurosci 21:7598–7607
Charfi I, Abdallah K, Gendron L, Pineyro G (2018) Delta opioid receptors recycle to the membrane after sorting to the degradation path. Cell Mol Life Sci 75:2257–2271. https://doi.org/10.1007/s00018-017-2732-5
Charles A, Pradhan AA (2016) Delta-opioid receptors as targets for migraine therapy. Curr Opin Neurol 29:314–319. https://doi.org/10.1097/WCO.0000000000000311
Cheng PY et al (1995) Ultrastructural immunolabeling shows prominent presynaptic vesicular localization of delta-opioid receptor within both enkephalin- and nonenkephalin-containing axon terminals in the superficial layers of the rat cervical spinal cord. J Neurosci 15:5976–5988
Chung PCS, Kieffer BL (2013) Delta opioid receptors in brain function and diseases. Pharmacol Ther 140:112–120. https://doi.org/10.1016/j.pharmthera.2013.06.003
Chung PC et al (2015) Delta opioid receptors expressed in forebrain GABAergic neurons are responsible for SNC80-induced seizures. Behav Brain Res 278:429–434. https://doi.org/10.1016/j.bbr.2014.10.029
Dado RJ, Law PY, Loh HH, Elde R (1993) Immunofluorescent identification of a delta (delta)-opioid receptor on primary afferent nerve terminals. NeuroReport 5:341–344
Dallel R, Descheemaeker A, Luccarini P (2018) Recurrent administration of the nitric oxide donor, isosorbide dinitrate, induces a persistent cephalic cutaneous hypersensitivity: a model for migraine progression. Cephalalgia 38:776–785. https://doi.org/10.1177/0333102417714032
Desmeules JA, Kayser V, Gacel G, Guilbaud G, Roques BP (1993) The highly selective delta agonist BUBU induces an analgesic effect in normal and arthritic rat and this action is not affected by repeated administration of low doses of morphine. Brain Res 611:243–248
Dubois D, Gendron L (2010) Delta opioid receptor-mediated analgesia is not altered in preprotachykinin A knockout mice. Eur J Neurosci 32:1921–1929. https://doi.org/10.1111/j.1460-9568.2010.07466.x
Erbs E et al (2015) A mu-delta opioid receptor brain atlas reveals neuronal co-occurrence in subcortical networks. Brain Struct Funct 220:677–702. https://doi.org/10.1007/s00429-014-0717-9
Filliol D et al (2000) Mice deficient for delta- and mu-opioid receptors exhibit opposing alterations of emotional responses. Nat Genet 25:195–200. https://doi.org/10.1038/76061
Fraser GL, Gaudreau GA, Clarke PB, Menard DP, Perkins MN (2000a) Antihyperalgesic effects of delta opioid agonists in a rat model of chronic inflammation. Br J Pharmacol 129:1668–1672. https://doi.org/10.1038/sj.bjp.0703248
Fraser GL, Holmgren J, Clarke PB, Wahlestedt C (2000b) Antisense inhibition of delta-opioid receptor gene function in vivo by peptide nucleic acids. Mol Pharmacol 57:725–731. https://doi.org/10.1124/mol.57.4.725
Gallantine EL, Meert TF (2005) A comparison of the antinociceptive and adverse effects of the mu-opioid agonist morphine and the delta-opioid agonist SNC80. Basic Clin Pharmacol Toxicol 97:39–51. https://doi.org/10.1111/j.1742-7843.2005.pto_07.x
Gaveriaux-Ruff C, Karchewski LA, Hever X, Matifas A, Kieffer BL (2008) Inflammatory pain is enhanced in delta opioid receptor-knockout mice. Eur J Neurosci 27:2558–2567. https://doi.org/10.1111/j.1460-9568.2008.06223.x
Gaveriaux-Ruff C, Kieffer BL (2011) Delta opioid receptor analgesia: recent contributions from pharmacology and molecular approaches. Behav Pharmacol 22:405–414. https://doi.org/10.1097/FBP.0b013e32834a1f2c
Gendron L, Cahill CM, von Zastrow M, Schiller PW, Pineyro G (2016) Molecular pharmacology of delta-opioid receptors. Pharmacol Rev 68:631–700. https://doi.org/10.1124/pr.114.008979
Gendron L et al (2007a) Morphine priming in rats with chronic inflammation reveals a dichotomy between antihyperalgesic and antinociceptive properties of deltorphin. Neuroscience 144:263–274. https://doi.org/10.1016/j.neuroscience.2006.08.077
Gendron L, Lucido AL, Mennicken F, O'Donnell D, Vincent JP, Stroh T, Beaudet A (2006) Morphine and pain-related stimuli enhance cell surface availability of somatic delta-opioid receptors in rat dorsal root ganglia. J Neurosci 26:953–962. https://doi.org/10.1523/JNEUROSCI.3598-05.2006
Gendron L, Mittal N, Beaudry H, Walwyn W (2015) Recent advances on the δ opioid receptor: from trafficking to function. Br J Pharmacol. https://doi.org/10.1111/bph.2015.172.issue-2
Gendron L, Pintar JE, Chavkin C (2007b) Essential role of mu opioid receptor in the regulation of delta opioid receptor-mediated antihyperalgesia. Neuroscience 150:807–817. https://doi.org/10.1016/j.neuroscience.2007.09.060
Goldenberg DL (2010a) The interface of pain and mood disturbances in the rheumatic diseases. Semin Arthritis Rheum 40:15–31. https://doi.org/10.1016/j.semarthrit.2008.11.005
Goldenberg DL (2010b) Pain/Depression dyad: a key to a better understanding and treatment of functional somatic syndromes. Am J Med 123:675–682. https://doi.org/10.1016/j.amjmed.2010.01.014
Guan JS et al (2005) Interaction with vesicle luminal protachykinin regulates surface expression of delta-opioid receptors and opioid analgesia. Cell 122:619–631. https://doi.org/10.1016/j.cell.2005.06.010
Hack SP, Bagley EE, Chieng BC, Christie MJ (2005) Induction of delta-opioid receptor function in the midbrain after chronic morphine treatment. J Neurosci 25:3192–3198
Hervera A, Leanez S, Negrete R, Pol O (2009) The peripheral administration of a nitric oxide donor potentiates the local antinociceptive effects of a DOR agonist during chronic inflammatory pain in mice. Naunyn Schmiedebergs Arch Pharmacol 380:345–352. https://doi.org/10.1007/s00210-009-0436-6
Holdridge SV, Cahill CM (2007) Spinal administration of a delta opioid receptor agonist attenuates hyperalgesia and allodynia in a rat model of neuropathic pain. Eur J Pain 11:685–693. https://doi.org/10.1016/j.ejpain.2006.10.008
Honore P et al (2000) Murine models of inflammatory, neuropathic and cancer pain each generates a unique set of neurochemical changes in the spinal cord and sensory neurons. Neuroscience 98:585–598
Jeske NA (2019) Dynamic opioid receptor regulation in the periphery. Mol Pharmacol 95:463–467. https://doi.org/10.1124/mol.118.114637
Kabli N, Cahill CM (2007) Anti-allodynic effects of peripheral delta opioid receptors in neuropathic pain. Pain 127:84–93. https://doi.org/10.1016/j.pain.2006.08.003
Kamei J, Kashiwazaki T, Hitosugi H, Nagase H (1997a) The role of spinal delta1-opioid receptors in inhibiting the formalin-induced nociceptive response in diabetic mice. Eur J Pharmacol 326:31–36
Kamei J et al (1997b) Supraspinal delta 1-opioid receptor-mediated antinociceptive properties of (-)-TAN-67 in diabetic mice. Eur J Pharmacol 322:27–30
Kieffer BL, Gaveriaux-Ruff C (2002) Exploring the opioid system by gene knockout. Prog Neurobiol 66:285–306
King T et al (2009) Unmasking the tonic-aversive state in neuropathic pain. Nat Neurosci 12:1364–1366. https://doi.org/10.1038/nn.2407
Kouchek M, Takasusuki T, Terashima T, Yaksh TL, Xu Q (2013) Effects of intrathecal SNC80, a delta receptor ligand, on nociceptive threshold and dorsal horn substance p release. J Pharmacol Exp Ther 347:258–264. https://doi.org/10.1124/jpet.113.206573
Le Bars D, Villanueva L, Bouhassira D, Willer JC (1992) Diffuse noxious inhibitory controls (DNIC) in animals and in man. Patol Fiziol Eksp Ter, 55–65
Le Bourdonnec B et al (2008) Potent, orally bioavailable delta opioid receptor agonists for the treatment of pain: discovery of N, N-diethyl-4-(5-hydroxyspiro[chromene-2,4'-piperidine]-4-yl)benzamide (ADL5859). J Med Chem 51:5893–5896. https://doi.org/10.1021/jm8008986
Le Bourdonnec B et al (2009) Spirocyclic delta opioid receptor agonists for the treatment of pain: discovery of N, N-diethyl-3-hydroxy-4-(spiro[chromene-2,4'-piperidine]-4-yl) benzamide (ADL5747). J Med Chem 52:5685–5702. https://doi.org/10.1021/jm900773n
Lucido AL, Morinville A, Gendron L, Stroh T, Beaudet A (2005) Prolonged morphine treatment selectively increases membrane recruitment of delta-opioid receptors in mouse basal ganglia. J Mol Neurosci 25:207–214. https://doi.org/10.1385/JMN:25:3:207
Mansour A, Fox CA, Akil H, Watson SJ (1995) Opioid-receptor mRNA expression in the rat CNS: anatomical and functional implications. Trends Neurosci 18:22–29
Mansour A, Fox CA, Burke S, Meng F, Thompson RC, Akil H, Watson SJ (1994) Mu, delta, and kappa opioid receptor mRNA expression in the rat CNS: an in situ hybridization study. J Comp Neurol 350:412–438. https://doi.org/10.1002/cne.903500307
McQuay H (1999) Opioids in pain management. Lancet 353:2229–2232. https://doi.org/10.1016/S0140-6736(99)03528-X
Mennicken F, Zhang J, Hoffert C, Ahmad S, Beaudet A, O'Donnell D (2003) Phylogenetic changes in the expression of delta opioid receptors in spinal cord and dorsal root ganglia. J Comp Neurol 465:349–360. https://doi.org/10.1002/cne.10839
Mika J, Przewlocki R, Przewlocka B (2001) The role of delta-opioid receptor subtypes in neuropathic pain. Eur J Pharmacol 415:31–37
Morinville A et al (2004) Morphine-induced changes in delta opioid receptor trafficking are linked to somatosensory processing in the rat spinal cord. J Neurosci 24:5549–5559. https://doi.org/10.1523/JNEUROSCI.2719-03.2004
Morinville A, Cahill CM, Esdaile MJ, Aibak H, Collier B, Kieffer BL, Beaudet A (2003) Regulation of delta-opioid receptor trafficking via mu-opioid receptor stimulation: evidence from mu-opioid receptor knock-out mice. J Neurosci 23:4888–4898
Moye LS, Novack ML, Tipton AF, Krishnan H, Pandey SC, Pradhan AA (2019a) The development of a mouse model of mTBI-induced post-traumatic migraine, and identification of the delta opioid receptor as a novel therapeutic target. Cephalalgia 39:77–90. https://doi.org/10.1177/0333102418777507
Moye LS, Tipton AF, Dripps I, Sheets Z, Crombie A, Violin JD, Pradhan AA (2019b) Delta opioid receptor agonists are effective for multiple types of headache disorders. Neuropharmacology 148:77–86. https://doi.org/10.1016/j.neuropharm.2018.12.017
Nadal X, Banos JE, Kieffer BL, Maldonado R (2006) Neuropathic pain is enhanced in delta-opioid receptor knockout mice. Eur J Neurosci 23:830–834
Negus SS, Gatch MB, Mello NK, Zhang X, Rice K (1998) Behavioral effects of the delta-selective opioid agonist SNC80 and related compounds in rhesus monkeys. J Pharmacol Exp Ther 286:362–375
Normandin A, Luccarini P, Molat JL, Gendron L, Dallel R (2013) Spinal mu and delta opioids inhibit both thermal and mechanical pain in rats. J Neurosci 33:11703–11714. https://doi.org/10.1523/JNEUROSCI.1631-13.2013
Obara I, Parkitna JR, Korostynski M, Makuch W, Kaminska D, Przewlocka B, Przewlocki R (2009) Local peripheral opioid effects and expression of opioid genes in the spinal cord and dorsal root ganglia in neuropathic and inflammatory pain. Pain 141:283–291. https://doi.org/10.1016/j.pain.2008.12.006
Otis V, Sarret P, Gendron L (2011) Spinal activation of delta opioid receptors alleviates cancer-related bone pain. Neuroscience 183:221–229. https://doi.org/10.1016/j.neuroscience.2011.03.052
Pasquini F, Bochet P, Garbay-Jaureguiberry C, Roques BP, Rossier J, Beaudet A (1992) Electron microscopic localization of photoaffinity-labelled delta opioid receptors in the neostriatum of the rat. J Comp Neurol 326:229–244. https://doi.org/10.1002/cne.903260206
Patwardhan AM, Berg KA, Akopain AN, Jeske NA, Gamper N, Clarke WP, Hargreaves KM (2005) Bradykinin-induced functional competence and trafficking of the delta-opioid receptor in trigeminal nociceptors. J Neurosci 25:8825–8832. https://doi.org/10.1523/JNEUROSCI.0160-05.2005
Patwardhan AM, Diogenes A, Berg KA, Fehrenbacher JC, Clarke WP, Akopian AN, Hargreaves KM (2006) PAR-2 agonists activate trigeminal nociceptors and induce functional competence in the delta opioid receptor. Pain 125:114–124. https://doi.org/10.1016/j.pain.2006.05.007
Petrillo P et al (2003) Evidence for a selective role of the delta-opioid agonist [8R-(4bS*,8aalpha,8abeta, 12bbeta)]7,10-Dimethyl-1-methoxy-11-(2-methylpropyl)oxycarbonyl 5,6,7,8,12,12b-hexahydro-(9H)-4,8-methanobenzofuro[3,2-e]pyrrolo[2,3-g]isoquinoli ne hydrochloride (SB-235863) in blocking hyperalgesia associated with inflammatory and neuropathic pain responses. J Pharmacol Exp Ther 307:1079–1089. https://doi.org/10.1124/jpet.103.055590
Pettinger L, Gigout S, Linley JE, Gamper N (2013) Bradykinin controls pool size of sensory neurons expressing functional delta-opioid receptors. J Neurosci 33:10762–10771. https://doi.org/10.1523/JNEUROSCI.0123-13.2013
Porreca F, Mosberg HI, Hurst R, Hruby VJ, Burks TF (1984) Roles of mu, delta and kappa opioid receptors in spinal and supraspinal mediation of gastrointestinal transit effects and hot-plate analgesia in the mouse. J Pharmacol Exp Ther 230:341–348
Pradhan A, Smith M, McGuire B, Evans C, Walwyn W (2013a) Chronic inflammatory injury results in increased coupling of delta opioid receptors to voltage-gated Ca2+ channels. Mol Pain 9:8. https://doi.org/10.1186/1744-8069-9-8
Pradhan AA et al (2016) Agonist-specific recruitment of arrestin isoforms differentially modify delta opioid receptor function. J Neurosci 36:3541–3551. https://doi.org/10.1523/JNEUROSCI.4124-15.2016
Pradhan AA, Siau C, Constantin A, Clarke PB (2006) Chronic morphine administration results in tolerance to delta opioid receptor-mediated antinociception. Neuroscience 141:947–954
Pradhan AA, Smith ML, McGuire B, Tarash I, Evans CJ, Charles A (2014) Characterization of a novel model of chronic migraine. Pain 155:269–274. https://doi.org/10.1016/j.pain.2013.10.004
Pradhan MR, Ranjan P, Rao RN, Chipde SS, Pradhan K, Kapoor R (2013b) Inflammatory myofibroblastic tumor of the urinary bladder managed by laparoscopic partial cystectomy Korean. J Urol 54:797–800. https://doi.org/10.4111/kju.2013.54.11.797
Qiu C, Sora I, Ren K, Uhl G, Dubner R (2000) Enhanced delta-opioid receptor-mediated antinociception in mu-opioid receptor-deficient mice. Eur J Pharmacol 387:163–169
Riedl MS et al (2009) Coexpression of alpha 2A-adrenergic and delta-opioid receptors in substance P-containing terminals in rat dorsal horn. J Comp Neurol 513:385–398
Rossi GC, Pasternak GW, Bodnar RJ (1994) Mu and delta opioid synergy between the periaqueductal gray and the rostro-ventral medulla. Brain Res 665:85–93. https://doi.org/10.1016/0006-8993(94)91155-x
Rowan MP, Ruparel NB, Patwardhan AM, Berg KA, Clarke WP, Hargreaves KM (2009) Peripheral delta opioid receptors require priming for functional competence in vivo. Eur J Pharmacol 602:283–287. https://doi.org/10.1016/j.ejphar.2008.11.028
Saitoh A et al (2011) The novel delta opioid receptor agonist KNT-127 produces antidepressant-like and antinociceptive effects in mice without producing convulsions. Behav Brain Res 223:271–279
Saloman JL, Niu KY, Ro JY (2011) Activation of peripheral delta-opioid receptors leads to anti-hyperalgesic responses in the masseter muscle of male and female rats. Neuroscience 190:379–385. https://doi.org/10.1016/j.neuroscience.2011.05.062
Scherrer G et al (2009) Dissociation of the opioid receptor mechanisms that control mechanical and heat pain. Cell 137:1148–1159. https://doi.org/10.1016/j.cell.2009.04.019
Scherrer G et al (2006) Knockin mice expressing fluorescent delta-opioid receptors uncover G protein-coupled receptor dynamics in vivo. Proc Natl Acad Sci USA 103:9691–9696. https://doi.org/10.1073/pnas.0603359103
Schuster DJ, Kitto KF, Overland AC, Messing RO, Stone LS, Fairbanks CA, Wilcox GL (2013) Protein kinase Cepsilon is required for spinal analgesic synergy between delta opioid and alpha-2A adrenergic receptor agonist pairs. J Neurosci 33:13538–13546. https://doi.org/10.1523/JNEUROSCI.4013-12.2013
Shiwarski DJ, Crilly SE, Dates A, Puthenveedu MA (2019) Dual RXR motifs regulate nerve growth factor-mediated intracellular retention of the delta opioid receptor. Mol Biol Cell 30:680–690. https://doi.org/10.1091/mbc.E18-05-0292
Smith HS, Peppin JF (2014) Toward a systematic approach to opioid rotation. J Pain Res 7:589–608. https://doi.org/10.2147/JPR.S55782
Sohn JH, Lee BH, Park SH, Ryu JW, Kim BO, Park YG (2000) Microinjection of opiates into the periaqueductal gray matter attenuates neuropathic pain symptoms in rats. NeuroReport 11:1413–1416
Spahn V, Stein C (2017) Targeting delta opioid receptors for pain treatment: drugs in phase I and II clinical development. Expert Opin Investig Drugs 26:155–160. https://doi.org/10.1080/13543784.2017.1275562
St-Louis E et al (2017) Involvement of the coatomer protein complex I in the intracellular traffic of the delta opioid receptor. Mol Cell Neurosci 79:53–63. https://doi.org/10.1016/j.mcn.2016.12.005
Stein C, Millan MJ, Shippenberg TS, Peter K, Herz A (1989) Peripheral opioid receptors mediating antinociception in inflammation. Evidence for involvement of mu, delta and kappa receptors. J Pharmacol Exp Ther 248:1269–1275
Stewart PE, Hammond DL (1994) Activation of spinal delta-1 or delta-2 opioid receptors reduces carrageenan-induced hyperalgesia in the rat. J Pharmacol Exp Ther 268:701–708
Thorlund K et al (2016) Risk of medication overuse headache across classes of treatments for acute migraine. J Headache Pain 17:107. https://doi.org/10.1186/s10194-016-0696-8
Usoskin D et al (2015) Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing. Nat Neurosci 18:145–153. https://doi.org/10.1038/nn.3881
Vicente-Sanchez A, Dripps IJ, Tipton AF, Akbari H, Akbari A, Jutkiewicz EM, Pradhan AA (2018) Tolerance to high-internalizing delta opioid receptor agonist is critically mediated by arrestin 2. Br J Pharmacol 175:3050–3059. https://doi.org/10.1111/bph.14353
Xie WY, He Y, Yang YR, Li YF, Kang K, Xing BM, Wang Y (2009) Disruption of Cdk5-associated phosphorylation of residue threonine-161 of the delta-opioid receptor: impaired receptor function and attenuated morphine antinociceptive tolerance. J Neurosci 29:3551–3564. https://doi.org/10.1523/JNEUROSCI.0415-09.2009
Yam MF, Loh YC, Tan CS, Khadijah Adam S, Abdul Manan N, Basir R (2018) General pathways of pain sensation and the major neurotransmitters involved in pain regulation. Int J Mol Sci. https://doi.org/10.3390/ijms19082164
Ye Y, Dang D, Viet CT, Dolan JC, Schmidt BL (2012) Analgesia targeting IB4-positive neurons in cancer-induced mechanical hypersensitivity. J Pain 13:524–531. https://doi.org/10.1016/j.jpain.2012.01.006
Zhang X, Bao L, Arvidsson U, Elde R, Hokfelt T (1998) Localization and regulation of the delta-opioid receptor in dorsal root ganglia and spinal cord of the rat and monkey: evidence for association with the membrane of large dense-core vesicles. Neuroscience 82:1225–1242
Zhang X, Bao L, Ma GQ (2010) Sorting of neuropeptides and neuropeptide receptors into secretory pathways. Prog Neurobiol 90:276–283. https://doi.org/10.1016/j.pneurobio.2009.10.011
Zhou L, Zhang Q, Stein C, Schafer M (1998) Contribution of opioid receptors on primary afferent versus sympathetic neurons to peripheral opioid analgesia. J Pharmacol Exp Ther 286:1000–1006
Zhu Y, Hsu MS, Pintar JE (1998) Developmental expression of the mu, kappa, and delta opioid receptor mRNAs in mouse. J Neurosci 18:2538–2549
Zhu Y et al (1999) Retention of supraspinal delta-like analgesia and loss of morphine tolerance in delta opioid receptor knockout mice. Neuron 24:243–252
Acknowledgements
This work was supported by Canadian Institutes of Health Research (CIHR) grants to LG (MOP-136871 and PJT-162103) and a pilot project grant from the Fonds de la Recherche du Québec-Santé (FRQ-S)-funded Quebec Pain Reseach Network (QPRN) (Grant No. 30851). LG is the recipient of a Chercheur-boursier Senior salary support from the FRQ-S.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berthiaume, S., Abdallah, K., Blais, V. et al. Alleviating pain with delta opioid receptor agonists: evidence from experimental models. J Neural Transm 127, 661–672 (2020). https://doi.org/10.1007/s00702-020-02172-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-020-02172-4