Abstract
l-DOPA induced dyskinesias (LIDs) may affect up to 40% of Parkinson’s disease (PD) and impact negatively health-related quality of life. Amantadine has demonstrated significant antidyskinetic effects in animal PD models and in randomized double-blind placebo-controlled trials (RCTs) in patients with PD. These effects are thought to be related to the blockade of NMDA receptors modulating cortico-striatal glutamatergic–dopaminergic interactions involved in the genesis of LIDs. There are three pharmaceutical forms of amantadine currently available in the market: an oral immediate-release (IR) formulation, which is widely available; an extended-release (ER) formulation (ADS-5102) which has been recently developed and approved by the FDA; and an intravenous infusion (IV) solution, which is not commonly used in clinical practice. RCTs with amantadine IR or ER, involving more than 650 patients have shown consistent and long-lasting reductions in LIDs. Interestingly, ADS-5102 not only reduced LIDs, but also reduced significantly at the same time the duration of daily OFF-time, a unique finding compared with other antiparkinsonian medications that usually reduce time spent OFF at the cost of worsening of LIDs. Amantadine IR might also have possible effects on other PD symptoms such as apathy or fatigue. The most common adverse reactions with amantadine are constipation, cardiovascular dysfunction including QT prolongation, orthostatic hypotension and edema, neuropsychiatric symptoms such as hallucinations, confusion and delirium, nausea and livedo reticularis. Corneal degeneration is rare but critical. In summary, amantadine immediate and extended-release are effective and safe for the treatment of LIDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative disorder affecting about 1 person every 1000 in the fifth decade and 19 every 1000 above 80 years old (Pringsheim et al. 2014). Core motor symptoms are bradykinesia, rigidity, tremor and postural abnormalities (Hughes et al. 1992). Patients are also affected by secondary motor symptoms such as gait abnormalities, micrographia and speech problems, (Lang and Lozano 1998). Non-motor features, including cognitive and behavior dysfunction, sleep abnormalities, pain or autonomic disturbances, among others, are frequent and disabling (Chaudhuri and Schapira 2009).
l-DOPA remains the “gold standard” treatment for Parkinson’s disease (PD) motor symptoms since its introduction in the 60s (Birkmayer and Hornykiewicz 1998). As documented in the placebo-controlled l-DOPA study in early PD (ELLDOPA), although l-DOPA clearly improves parkinsonism with a dose-related response, a 600 mg daily dose may also induce LIDs in 17% of patients after only 40 weeks of treatment (Fahn et al. 2004), while this figure attained 40% in other studies (Ahlskog and Muenter 2001). A post hoc study of the STRIDE-PD study showed that, in addition to l-DOPA dose, young age at onset, low body weight, North American geographic region, treatment with entacapone, female gender, and more severe Unified Parkinson’s Disease Rating Scale (UPDRS) Part II score predicted the 4-year risk of developing LIDs (Olanow et al. 2013). Several studies suggest that LIDs impact negatively on health-related quality of life (Pèchevis et al. 2005; Damiano et al. 2000; Montel et al. 2009; Reuther et al. 2007; Perez-Lloret et al. 2017).
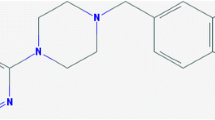
Motor complications remain a major unmet need for the management of PD. Many drugs have been developed to manage OFF episodes, including dopamine agonists, MAO-B and COMT inhibitors, but these drugs usually reduce time spent OFF at the cost of worsening of LIDs (Reichmann and Emre 2012). Up to now, amantadine is the only drug that has been considered “clinically useful” for the treatment of LIDs in the last evidence-based review from the Movement Disorders Society is amantadine (Fox et al. 2011). Amantadine is a synthetic tricyclic amine that belongs to the class of aminoadamantanes (Deleu et al. 2002). It was originally found to have inhibitory effects against several strains of the influenza virus during the 60s (Hubsher et al. 2012). Poskanzer and Schwab reported in 1969 the case of a 58-year parkinsonian woman who claimed an improvement in rigidity, tremor, and akinesia while taking amantadine for flu. The symptoms worsened upon stopping the medication. These effects were then tested in a sample of ten PD patients, of whom seven improved, followed by a 6-month trial in which 163 patients with PD added amantadine to their anti-PD therapy regimens. Results showed improvement in symptoms in 66% of patients with PD. These results were confirmed by forthcoming small uncontrolled trials.
The first “modern” data on the antidyskinetic effect of amantadine were published in the late 90s, closely following the reports on the antiglutamatergic properties of the drug and its potential role in LIDs (Goetz 1998). The objective of this review is to discuss the action mechanism, clinical pharmacokinetics, efficacy and safety of amantadine for LIDs. We searched PubMed with the string “Parkinson’s disease AND amantadine”, between 1980 and 2017. Amantadine’s antiparkinsonian and potential neuroprotective effects will not be covered.
Mechanisms of amantadine antidyskinetic effect
The pathophysiological mechanisms of LIDs are covered in other articles of this Special Supplement and this section will focus on the molecular mechanisms that can explain the antidyskinetic effects of amantadine. Both mechanisms of LIDs and mechanisms of action of amantadine being not fully understood, it is not possible to propose a simple straightforward explanation. LID appears to be a complex set of phenomena. This complexity explains why, despite extensive preclinical and clinical research, few agents have successfully been shown to reduce dyskinesia or to successfully translate from preclinical to clinical settings. One reason has been that the majority of researches have focused on peak dose (high l-DOPA dose) dyskinesia, while many PD subjects may experience a mixture of peak and diphasic dyskinesia. Moreover, there is evidence for abnormalities in several neurotransmitter systems in LIDs and the traditional approaches, which usually focus on a single target, may not be appropriate and may account for failures in clinical translation (see Huot et al. 2013). Amantadine effects in the central nervous system are multiple, complex and not fully understood. Basically, the drug is known to exert antagonistic effects at the glutamate NMDA receptors and cholinergic muscarinic receptors. It is also known to increase dopamine synthesis and/or release and reduce dopamine reuptake.
Amantadine exerts a non-competitive antagonism with low-affinity of the N-methyl-d-aspartate (NMDA)-glutamate receptor subtype at the phencyclidine binding site, which is localized inside and at the sigma 1-binding site localized outside the cation channel (Kornhuber et al. 1991). Several pieces of evidence suggest that it is amantadine NMDA-blocking properties that are the most important to explain its antidyskinetic effects (Stoof et al. 1992; Lupp et al. 1992; Parsons et al. 1996). This is consistent with the observation that glutamate and NMDA receptors play a key role in the genesis of LIDs (Chase and Oh 2000; Huot et al. 2013). Several pieces of evidences suggest that LIDs are linked to loss of long-term depression and depotentiation at corticospinal synapses (Calabresi et al. 2015, 2016). Loss of depotentiation might destabilize neuronal circuits in the basal ganglia, thus generating LIDs. According to recent data, D1 overexcitation resulting from chronic exposure to l-DOPA might induce phosphorylation of the DARPP-32 protein, which in turn increases the levels of phosphorylated NMDA receptors, which is thought to be related to the loss of depotentiation (Calabresi et al. 2016). Another factor influencing the generation of LIDs is the molecular composition of NMDA receptors. Indeed, some studies have shown that dyskinetic rats show higher levels of GluN2A subunit and lower levels of GluN2B subunit (Calabresi et al. 2015). These alterations are associated with changes in the association between NMDA receptors and scaffolding elements, i.e., members of the membrane-associated guanylate kinase (MAGUK) protein family, such as postsynaptic density-95, synapse-associated protein-97 and synapse-associated protein-102.
This is indeed for its NMDA antagonistic effects that Chase and his colleagues chose amantadine in the 90s as a candidate for testing the “NMDA hypothesis” of LIDs in animals and in humans. In normal subjects, the effect of amantadine on human motor cortex excitability was assessed using transcranial magnetic stimulation that modulates human motor cortex excitability. Amantadine decreased intracortical facilitation and increased late inhibition, reflecting glutamatergic modulation or a polysynaptic interaction of glutamatergic and GABAergic circuits (Reis et al. 2006).
Blockade of NMDA receptor by amantadine induces neuronal currents that may lead to a stabilization of other channels closed states (Blanpied et al. 2005). Therefore, by stabilizing the channel associated with the nicotinic receptor, ACh release from striatal interneurons is reduced, as shown in vitro (Stoof et al. 1992; Matsubayashi et al. 1997). Increased cholinergic tone has been considered as a factor associated with the genesis of LIDs (Perez-Lloret and Barrantes 2016). Thus, the effects of amantadine on cholinergic systems might contribute to its effects on LIDs. Clinically, amantadine induces antimuscarinic-like adverse reactions (dry mouth, dysuria and constipation). However, no benefit of antiparkinsonian antimuscarinic medications such as biperiden has been reported in dyskinetic PD patients, thus reinforcing the potential importance of nicotinic contributions to the antidyskinetic effect of amantadine.
Amantadine also affects dopamine synthesis and uptake. The relevance of such mechanisms to account for its clinical antidyskinetic effect remains, however, unclear, and would indeed better fit for accounting for its antiparkinsonian rather than antidyskinetic properties. In rats, amantadine 40 mg/kg significantly increased the activity of the aromatic l-amino acid decarboxylase (AADC) in the striatum and substantia nigra (Fisher et al. 1998). Similar results were obtained in healthy subjects receiving amantadine for 3 days at 100 mg daily dose by assessment of the decarboxylation rate of 6-[18F]fluoro-l-DOPA (FDOPA), which is an exogenous substrate for AADC (Deep et al. 1999). Regarding dopamine uptake, amantadine 1 mM applied by microdialysis to the striatum of Wistar rats caused a significant increase of 50% in extracellular dopamine levels (Mizoguchi et al. 1994). This effect was might be mediated by inhibition of dopamine uptake caused by blockade of NMDA receptors, as non-competitive antagonists of NMDA receptor increase dopamine biosynthesis, turnover and synaptic release from striatal dopaminergic neuronal terminals in vitro (Heikkila and Cohen 1972; Jackisch et al. 1992) and in vivo (Takahashi et al. 1996).
Intuitively, it is difficult to reconcile in a simple way the fact that a drug that increases dopamine synaptic availability can reduce LIDs, as greater doses of dopaminergic medications increase LIDs consistently in animals and in humans. However, it is conceptually possible to argue that the manner dopamine is released in the synapse (pulsatile vs continuous) plays a key role in the genesis of the synaptic plastic abnormalities leading to LIDs, and that a drug that modifies dopamine release/uptake could therefore reduce LIDs (Grace 2008). The fact that the antidyskinetic effects of amantadine occur and disappear clinically quite rapidly, within a couple of days, might not fit well, however, with the concept that long-term plasticity is an important phenomenon involved in LIDs pathophysiology.
The same is true regarding amantadine effects on dopamine receptor functioning. In one study, the effects of amantadine treatments on the expression of dopamine receptors and the functional coupling to G proteins in rat striatal membranes homogenates were investigated (Peeters et al. 2002). This was done by measuring dopamine-induced stimulation of guanosine 5′-O-(gamma-[35S]thio)triphosphate (GTPgS), which has been shown to reflect activation of D2 receptors. Results showed a transient enhancement of dopamine-induced stimulation of GTPgS after a 4-day amantadine treatment. This effect was not related to changes in dopamine receptor availability. Furthermore, amantadine-treated animals exhibited hypersensitive dopamine transmission, as shown by exacerbated responses to a single apomorphine doses. Results of a binding study in rats confirmed that amantadine induced 10% increases in D2 receptor availability (Hesselink et al. 1999). Results with [11C]raclopride Positron Emission Tomography (PET), which is a marker of D2 receptor availability, showed coherent results (Moresco et al. 2002; Volonte et al. 2001). The relevancy for such finding to explain the antidyskinetic effect of amantadine is difficult to assess, but it might point out the importance of the activation of the D2 “indirect” striatopallidal pathway.
Amantadine effect on basal ganglia circuitry functioning has been assessed in some experiments. It has been shown that amantadine-reduced synaptic excitation of rat striatal slices containing medium spiny neurons, as measured by recording evoked excitatory postsynaptic potentials after electrical stimulation of the slices (Rohrbacher et al. 1994). In addition to the striatum, both the subthalamic nucleus and the GPi contain NMDA receptors (Obeso et al. 2008). Theoretically, amantadine should reduce subthalamic activity and output by inhibiting their activation. Notwithstanding, when amantadine effect on subthalamic neural activity was studied in intact or 6-hydroxydopamine (6OHDA)-lesioned rats, it increased significantly subthalamic firing rates (Allers et al. 2005). Amantadine was given intravenously, and thus these results might reflect the combined action of the drug on NMDA receptor at the subthalamic nucleus and elsewhere. Amantadine effect on striatofugal pathways was studied by dual probe microdialysis in 6OHDA hemi-lesioned dyskinetic mice and rats (Bido et al. 2011). l-DOPA caused increased GABA release in substantia nigra Pars reticulata, but not in the Globus Pallidus, which coincided with LIDs. Pretreatment with amantadine (40 mg/kg i.p.) prevented GABA rise and LIDs.
In summary, although amantadine has undisputable antidyskinetic properties that are consistently documented in animal models and PD patients (see below), the intimate mechanisms explaining such a property remain rather mysterious. Non-competitive antagonism at the NMDA receptors probably plays an important role. It is more difficult to link the known effects of the drug on dopaminergic mechanisms (release, synthesis and receptors) with its effects on LIDs. The impact of different doses and duration of exposure having been insufficiently explored, any conclusion on that matter can only be speculative at the moment, and further studies should be strongly encouraged. Moreover, other yet unknown effects on other transmitters or other mechanisms cannot be excluded.
Antidyskinetic effects of amantadine in vivo in animal models of PD with LIDs
Amantadine antidyskinetic effects have now been extensively studied in vivo in different rodent and primate parkinsonian models combining nigro-striatal denervation and l-DOPA exposure. Generally, such experiments have aimed at measuring behavioral changes considered to mimic the so-called “peak-dose” LIDs. A summary of such studies can be found in Table 1.
The antidyskinetic properties of amantadine have been assessed in 6OHDA-lesioned rodents, both in the rat and the mice. In a recent study by Bortolanza and colleagues, amantadine single doses of 10, 20 or 40 mg/kg were administered to lesioned rats with LIDs after 21 days of treatment with l-DOPA 20 mg/kg (Bortolanza et al. 2016). Amantadine dose-dependently reduced of global AIMs score over 180 min post-l-DOPA administration. The 20 mg/kg dose displayed significant antidyskinetic effect only during the first 60 min after l-DOPA. As shown in Table 1, other studies in rats and mice have yielded essentially similar results.
Chase and colleagues were pioneers in proposing in the 90s that the NMDA antagonistic properties of amantadine might be beneficial for the treatment of LIDs. They were also among the first to test this hypothesis in a non-human primate model of LIDs. In this experiment, four MPTP-lesioned monkeys under l-DOPA therapy received the drug in two different regimens: 1.25 or 2.5 mg/kg s.c. twice daily for 3–6 days (Blanchet et al. 1998). l-DOPA was also given at two different effective “low” and “high” doses (i.e., mean doses of 47.5 and 110 mg, respectively). When amantadine was co-administered with low doses of l-DOPA, it suppressed almost completely LIDs, but when its dose attained 2.5 mg/kg, l-DOPA antiparkinsonian effect was also compromised. Conversely, amantadine did not affect l-DOPA antiparkinsonian effect when the latter was administered at higher doses, while it reduced LIDs only at 2.5 mg/kg dose. These authors were not able to offer a convincing explanation for the reduction of antiparkinsonian l-DOPA effects at low doses. Amantadine was also shown to reduce LIDs caused by D1- or D2 agonists in MPTP-lesioned animals (Bibbiani et al. 2005), and its antidyskinetic effect in non-human primates has been repetitively and consistently confirmed in subsequent experiments (see Table 1). For example, amantadine has also been used as a “positive” comparator in animal studies assessing primarily the antidyskinetic effect of other drugs, including IRC-082451, a multi-targeting hybrid molecule with sodium channel blocking, antioxidant and cyclooxygenase inhibiting effects (Aron Badin et al. 2013), eltoprazine, a 5-HT1A/1B-receptor agonist (Bezard et al. 2013), or TC-8831, an agonist at nicotinic acetylcholine receptors (Johnston et al. 2013). In all these experiments, LIDs were reduced when monkeys received amantadine. Amantadine has also been used for the validation of novel LIDs animal models (Dekundy et al. 2007; Lundblad et al. 2005), and for the assessment of new rating scales of LIDs in animals (Sebastianutto et al. 2016). This demonstrates the reliability of its antidyskinetic response and illustrates the fact that the drug is now considered as a referential agent for the evaluation of LIDs in animal models.
Finally, other studies have shown that amantadine antidyskinetic effect can be potentiated by other medications such as levetiracetam (Hill et al. 2004), topiramate (Kobylecki et al. 2011) or fenobam (Ko et al. 2014). Only the combination of topiramate and amantadine has been assessed for LIDs in clinical trials, with negative results (Goetz et al. 2017).
Clinical pharmacokinetics
In healthy elderly subjects, amantadine IR is absorbed slowly and variably from the gastrointestinal tract after oral administration (Deleu et al. 2002). Bioavailability of the IR form is 85–90% (Aoki and Sitar 1988). The drug is extensively bound to tissues, and its apparent volume of distribution is inversely related to dose (Aoki and Sitar 1988). It has been hypothesized that this inverse relationship accounted, at least in part, for disproportionately high amantadine serum concentrations associated with neurotoxic side effects, at least in healthy young adults (Aoki and Sitar 1988). Plasmatic half life is 10–45 h, and steady-state concentrations are usually reached within 4–7 days in healthy elderly and parkinsonian subjects (Deleu et al. 2002). The drug is almost entirely eliminated by renal clearance, particularly renal tubular secretion.
Usual amantadine IR dose to achieve antidyskinetic effects is 100–300 mg (Alliance Pharmaceuticals 2010). Dose should be reduced in patients with renal insufficiency (Horadam et al. 1981). Hemodialysis only removed negligible amounts of the drug. Metabolism by acetylation affects 5–15% of each dose (Koppel and Tenczer 1985; Deleu et al. 2002). In cases of overdose, metabolites can be identified in plasma (Koppel and Tenczer 1985). There are many generics of the IR formulation available in the market. To the best of our knowledge, there are no published bioequivalence studies on them.
In a small study, plasmatic concentrations after oral 600 mg doses of the IR form to parkinsonian patients were 1500–1700 mcg/ml (Brenner et al. 1989). Serum and CSF concentrations were essentially similar. In another study, plasmatic steady-state concentrations were assessed in 78 patients (Nishikawa et al. 2009). Mean daily dose of amantadine was 135.1 ± 62.3 mg/day (range 50–300 mg/day). Mean plasma amantadine concentration ranged from 91 to 4400 ng/ml (mean 812.5 ± 839.5 ng/ml). Interestingly, plasma amantadine concentration of 3000 ng/ml or more was observed in four patients, out of whom three showed neuropsychiatric adverse reactions, thus suggesting that this might be the upper limit of the “therapeutic window”.
The pharmacokinetic profile of Amantadine extended-release (ADS-5102, Gocovri®) has been designed to exhibit an initially slow rate of rise in amantadine levels during sleep and high levels in the morning and throughout the waking hours when given at bedtime (Oertel et al. 2017). According to Gocovri’s Summary of Product Characteristics, median Tmax for plasma amantadine after oral administration was around 12 h (range 6–20 h) (Adamas Pharmaceuticals 2017). Furthermore, accumulation ratio after repeated doses was 1.2–1.3, which is negligible and might contribute to reduced toxicity.
Clinical efficacy
Amantadine is the only drug with solid clinical evidence of an antidyskinetic effect in PD patients (Fox et al. 2011). There are currently three pharmaceutical forms available in the market, the oral immediate- (IR) or extended-release (ER) tablets and the intravenous infusion (IV) formulation. The IR tables are widely available, while the ER ones (ADS-5102) have been recently developed and approved in FDA, but still not in Europe. Finally, the IV solution is not commonly used in the clinical practice and is available in a minority of countries.
In this section, the most important clinical trials of the amantadine will be briefly reviewed. A summary of all trials can be found in Table 2.
Immediate-release oral formulation
Verhagen Metman and colleagues conducted one of the first double-blind trials with amantadine in the late 90s (Verhagen Metman et al. 1998a, b). In a randomized, double-blind, placebo-controlled, cross-over study 18 advanced PD patients received amantadine or placebo for 3 weeks. At the end of each study arm, patients received an intravenous l-DOPA infusion and were assessed. The primary outcome was the modified Abnormal Involuntary Movement Scale (AIMS) and an abbreviated Unified Parkinson’s Disease Rating Scale (UPDRS part III, items 20, 22, 23, 26, 29, and 31, describing tremor, rigidity, finger taps, leg agility, gait, and body bradykinesia). Amantadine dose averaged 350 ± 15 mg in the 14 patients who finished the trial. Dyskinesia scores during steady-state l-DOPA infusions were 60% lower with amantadine (p < 0.001). Abbreviated UPDRS III scores were non-significantly lower in patients on amantadine. UPDRS IV score was also lower with amantadine. Interestingly, amantadine plasmatic levels correlated significantly with the change in AIMS score (r2 = 0.57, p < 0.01), suggesting a good dose–response relationship. Patients from this study were followed for up to 1 year (Metman et al. 1999) in a double-blind fashion. AIMS scores were 56% with amantadine at the end of follow-up. This suggested that amantadine effect was long lasting.
In a multi-center, double-blind, randomized, placebo-controlled, cross-over trial, 36 patients with PD and LIDs received amantadine (300 mg/day) or placebo treatment for 27 days with a 15-days wash-out in between (Sawada et al. 2010). Rush Dyskinesia Rating Scale, the primary outcome, improved in 64 and 16% of patients treated with amantadine or placebo, respectively (adjusted odds ratio for improvement by amantadine 6.7, 95% confidence interval 1.4–31.5, p < 0.01). Amantadine positive effects have also been observed in other studies, employing several dyskinesia scale as outcomes, including the Rush scale (Snow et al. 2000; Paci et al. 2001), UPDRS IV Items 32 + 33 (da Silva-Junior et al. 2005; Luginger et al. 2000; Wolf et al. 2010), or the UDysRS (Goetz et al. 2013). The characteristics and main results from these trials are summarized in Table 2.
In the study from Paci and colleagues, including 20 PD patients, the antidyskinetic effect of amantadine was reported to last less than 8 months (Paci et al. 2001), which conflicted with the results from Verhagen Metman et al. (1999). This fueled a controversy on the duration of amantadine antidyskinetic effect. This topic was revisited in a double-blind placebo-controlled trial (Thomas et al. 2004). Forty advanced PD patients received amantadine 300 mg/day or placebo. Investigators retained the patients into the study until there was clear evidence that the treatment administered (i.e., either amantadine or placebo) was devoid of efficacy. After 15 days of amantadine treatment, there was a reduction by 45% in the total dyskinesia scores, vs < 1% in the placebo group. Notwithstanding, the improvements disappeared 3–8 months later both in placebo- or amantadine-treated patients.
The controversy about the possibly waning antidyskinetic effect of amantadine on the long-term has been revisited using the wash-out design, where PD patients treated with amantadine for LIDs were randomly switched to placebo or remained on amantadine in double-blind conditions. A first study failed to find significant between-group differences, probably due to insufficient power, while LIDs worsened in patients switched to placebo and they did not change in those who were maintained on amantadine (Wolf et al. 2010). The AMANDYSK trial conducted by the French NS-Park/F-CRIN network, and then clearly showed that amantadine kept significant antidyskinetic properties in patients who had been treated with amantadine for LIDs for 3 years on average (Ory-Magne et al. 2014). AMANDYSK was a 3-month, multi-center, randomized, double-blind, placebo-controlled, parallel-group, wash-out study conducted in 57 amantadine-treated (mean daily dose of 250 mg/day for 3 years) dyskinetic patients with PD. The primary endpoint was the change from baseline to last visit of a dyskinesia UPDRS part IV score (items 32 + 33, i.e., LIDs “duration” and “disability”). The UPDRS items 32 + 33 score increased more in the “discontinuing” group (those who were switched to placebo) [+ 1.7; 95% confidence interval (CI) 0.9/2.4] than in the “continuing” group (those who remained on amantadine unchanged) (+ 0.2; 95% CI − 0.4/0.8), with a significant between-group difference (p < 0.003). This finding supports the fact that in such a population, the beneficial effect of amantadine on dyskinesia was still present on the long term. Interestingly, apathy (as measured by caregivers) and fatigue scores tended to worsen more in patients randomized to placebo than amantadine, suggesting potential non-motor effects of the drug.
Extended-release oral formulation
Results from three randomized, double-blind, placebo-controlled studies with ADS-5102, i.e., the EASED, EASE LID and EASE LID 3 studies, have been recently published (Pahwa et al. 2015, 2017; Oertel et al. 2017).
In the Phase II EASED study, 83 PD patients with troublesome LIDs were assigned to placebo or one of three doses of amantadine (260, 340, 420 mg) administered daily at bedtime for 8 weeks (Pahwa et al. 2015). LIDs, as measured by the Unified Dyskinesia Rating Scale (UDysRS), improved significantly with the 340 mg [least-square (LS) mean treatment difference = − 11.3 (95% CI − 19.1, − 3.5), p < 0.005] and 420 mg [LS mean treatment difference = − 10.0 (95% CI − 17.8, − 2.2), p < 0.013] doses. The duration of ON time without troublesome dyskinesia, as measured by home diaries, increased with all doses. MDS-UPDRS item measuring the functional impact of LIDs also improved with all doses. Finally, Clinical Global Impression of Change (CGI-C) scores were significantly better with ADS-5102 340 mg.
The EASE LID was a phase III trial, in which 126 patients were randomized to ADS-5102 274-mg (equivalent to amantadine hydrochloride 340 mg/day) or placebo (Pahwa et al. 2017). At week 12, the least-squares mean (SE) change in the Unified Dyskinesia Rating Scale score—UDysRS—(i.e., the primary endpoint) was − 15.9 ± 1.6 for amantadine ER and − 8.0 ± 1.6 for placebo (treatment difference, − 7.9; 95% CI − 12.5 to − 3.3; p < 0.001). Improvements persisted throughout the 24-weeks follow-up period. UDysRS scores were also improved by − 4.5 points (95% CI − 7.4 to − 1.6, p < 0.003) and − 4.2 (− 7.8 to − 0.7, p < 0.02) at weeks 12 and 24. MDS-UPDRS IV functional impact of dyskinesia scores was also lower with amantadine both at week 12 and 24. Finally, and interestingly, OFF time decreased significantly on amantadine ER by − 0.9 h (− 1.6 to − 0.2; p = 0.02) at week 12 and − 0.8 (− 1.6 to − 0.0, p < 0.04) at week 24. This is the first time that a drug demonstrated that it could improve concomitantly parkinsonism (OFF time) and LIDs, while in general, interventions that improve OFF time do so at the cost of worsening of LIDs.
The EASE LID 3 trial was a confirmatory Phase III study, including 73 PD patients with ≥ 1 h of troublesome dyskinesia and at least mild functional impact were randomized to placebo or ADS-5102 once daily at bedtime for 13 weeks (Oertel et al. 2017). At week 12, least-squares mean change in the UDysRS was − 20.7 (standard error 2.2) for ADS-5102 and − 6.3 (standard error 2.1) for placebo (treatment difference − 14.4, 95% confidence interval − 20.4 to − 8.3, p < 0.0001). OFF time decreased 0.5 h (standard error 0.3) for ADS-5102 from a baseline mean of 2.6 h and increased 0.6 h (standard error 0.3) for placebo from a baseline mean of 2.0 h (treatment difference − 1.1 h, 95% confidence interval − 2.0 to − 0.2, p < 0.02).
In a long-term open-label safety study, which included patients of the EASE LID and LID 3 trials, MDS-UPDRS part IV scores were reduced by ADS-5102 and remained stable for up to 64 weeks (Hauser et al. 2017). MDS-UPDRS Parts I–III mean scores showed relatively small changes from baseline at each measured time point across all groups.
Intravenous formulation
As mentioned earlier, amantadine IV is not commonly used in the clinical practice. Notwithstanding, its efficacy has been assessed by Ruzicka et al. (2000) in an open-label study, and by Del Dotto et al. (2001) in double-blind, randomized, cross-over study in nine patients (Table 2). In addition, it has also been tested as a “dopaminergic drug holidays” with some success (Koziorowski and Friedman 2007) (Table 2). This interesting use has not been further tested, to the best of our knowledge.
Safety
Toxicology data and drug use during pregnancy
Mutagenesis has not been observed in in vitro studies (Alliance Pharmaceuticals 2010). Amantadine deleterious effects on the central nervous system were assessed in CF-1 mice (Kaefer et al. 2010). Amantadine 15 mg/kg did not induce DNA damage and had no effects on memory, locomotion, exploration or motivation in mice. However, higher doses increased DNA damage in brain tissue, produced locomotor disturbances severe enough to preclude testing for learning and memory effects, and induced stereotypy, suggesting neurotoxicity (Kaefer et al. 2010). A study using postmortem human brain tissue of patients previously treated with amantadine failed to show changes in the hippocampus, retrosplenial cortex, and cingulate gyrus (Kornhuber et al. 1991).
Amantadine should be avoided in women who are pregnant or trying to become pregnant, as it may induce teratogenesis and increased risk of miscarriage (Seier and Hiller 2017).
Adverse events in clinical trials
In a recent meta-analysis, it was shown that the risk of any adverse event was higher in patients under amantadine immediate-release vs placebo patients (RR 1.86, 95% CI 1.38–2.52) (Kong et al. 2017). According to the Summary of Product Characteristics, the most common adverse events with amantadine IR (5–10%) are nausea, dizziness, and insomnia (Alliance Pharmaceuticals 2010). Depression, anxiety and irritability, hallucinations, confusion, anorexia, dry mouth, constipation, ataxia, livedo reticularis, peripheral edema, orthostatic hypotension, headache, somnolence, nervousness, dream abnormality, agitation, dry nose, diarrhea and fatigue are observed less frequently (1–5%) (Alliance Pharmaceuticals 2010).
Most frequent adverse events in the clinical trials with the ER formulation were orthostatic hypotension, hallucinations, dry mouth, nausea and edemas (Table 3). In an 88-week open-label follow-up study, 49.3% of patients on amantadine ER experimented adverse drug reactions (ADRs) (Hauser et al. 2017). Discontinuation due to ADRs occurred in 8.2% of patients. Most frequent adverse events were falls (25.1%), hallucinations (19.3%), peripheral edema (13.0%), constipation (12.6%), livedo reticularis (8.1%), nausea (8.1%), dry mouth (7.2%), insomnia (7.2%), and dizziness (6.7%).
Post-marketing surveillance
As amantadine IR has been on the market since the 60s, the amount of post-marketing surveillance data is abundant. In this section, the most important findings will be discussed.
Neuropsychiatric adverse reactions are frequent and expected with amantadine, due to the blockade of the NMDA and muscarinic receptors. Hallucination is one of the most common adverse drug reactions. In addition, abrupt changes in amantadine dosage can produce a severe withdrawal syndrome, which might include delirium, catatonia, or neuroleptic malignant syndrome (Fryml et al. 2017). These cases can be treated effectively by amantadine IV infusion (Marxreiter et al. 2017). Serotonin syndrome (Cheng et al. 2008) or dropped head syndrome (Kataoka and Ueno 2011) have also been reported. Impulse control disorders have also been positively related to amantadine prescription, both in case reports and large cross-sectional studies (McNamara and Durso 1991; Weintraub et al. 2010). A potential confounding effect of high dopaminergic therapy doses, which usually accompany amantadine usage, might not have been, however, completely accounted for in these studies. In fact, amantadine has been reported to have short-term efficacy for pathological gambling in a double-blind cross-over trial (Thomas et al. 2010). This result is inconsistent with the aforementioned results of case reports and epidemiological surveys (McNamara and Durso 1991; Weintraub et al. 2010). It has been proposed that LIDs and ICD might share molecular mechanisms and cognitive mechanisms of habit learning (Voon et al. 2009). Therefore, the role of amantadine on ICDs is not clear and should be further studied.
Orthostatic hypotension (OH) is a frequent ADR to amantadine, as shown in clinical trials. In a cross-section trial conducted by our group, the risk of OH increased dose-dependently with amantadine (Perez-Lloret et al. 2012). The mechanism leading to OH is not clear, but it might be related to alteration of cardiovascular reflexes (Korchounov et al. 2004). Finally, a case of inappropriate antidiuretic hormone secretion with amantadine has been reported (Alonso Navarro et al. 2009).
QT prolongation might be observed in patients treated with amantadine. Notwithstanding there is a paucity of clinical studies on the matter and further objective data should be welcome. Even if there are no recommendations on the Summary of Product Characteristics, electrocardiogram monitoring might be useful, especially in the elderly, in patients with long QT interval or in patients with renal failure. Arrhythmias can be observed with overdosage (see below).
Livedo reticularis has also been observed during clinical trials in PD and may affect up to 40% of patients (Quaresma et al. 2015). It is a purplish-red mottling of the skin, sometimes described as fishnet-like that may affect upper or lower extremities (Faulkner 2014). Even if it is harmless, it is a frequent cause of treatment abandon (Rana and Masroor 2012).
Corneal adverse reactions such as superficial punctuate keratitis, punctuate subepithelial opacification, epithelial edema and stromal edema although ocular toxicity are rare but critical (Kim et al. 2013). A recent cohort study in 8195 Taiwanese PD patients revealed an incidence of corneal edema of 1.5 (vs 1.0% in the control group, p < 0.004), which was increased by amantadine in a dose-dependent fashion (Lee et al. 2016). The effect of amantadine on corneal endothelial cells has been assessed in 169 PD patients and age- and gender-matched controls (Chang et al. 2010), showing significant toxicity. Furthermore, many changes were permanent and dose-dependent. The report of a case with acute visual loss after beginning amantadine suggests that dose-independent hypersensitivity may also play a role (Kubo et al. 2008).
Finally, amantadine may also cause other less studied adverse reactions. For example, it has been reported to cause Patulous Eustachian tube syndrome, which produces symptoms of aural fullness and autophony (Boyd and Silverman 2013). Acute respiratory failure has also been reported in one case (Cattoni and Parekh 2014). Anemia may also be seen with amantadine, which may result from accelerated clearance of erythrocytes due to suicidal erythrocyte death or eryptosis (Foller et al. 2008).
Overdosage and intoxication
Drug overdose can result in cardiac, respiratory, renal, and central nervous system toxicity (Pimentel and Hughes 1991; Schwartz et al. 2008; Snoey and Bessen 1990). Cardiac dysfunction includes arrhythmia, tachycardia and hypertension (Pimentel and Hughes 1991; Sartori et al. 1984). The lowest reported acute lethal dose was 1 g. Acute toxicity may be attributable to the anticholinergic effects of amantadine.
There is no specific antidote for amantadine, but the treatment with physostigmine has been reported to effectively control central nervous system toxicity (Alliance Pharmaceuticals 2010). Furthermore, the administration of urine acidifying drugs may increase drug clearance, as renal proximal reabsorption is dependent on a bicarbonate transporter (Goralski et al. 1999).
Conclusion
The efficacy and safety of amantadine IR have been documented in relatively old randomized, double-blind, controlled trials of imperfect quality due to heterogeneous sample sizes, follow-up periods and outcomes. Nevertheless, based on such evidence, the International Parkinson and Movement Disorders Society concluded that amantadine IR is “clinically useful” for the treatment of LIDs (Fox et al. 2011). The evidence supporting the clinical utility of amantadine ER (ADS-5102) is supported by three recent trials of better quality, which included larger (although limited) samples, with longer follow-up periods (up to 6 months), and used more standardized and valid assessment of LIDs (i.e., UDysRS and home diaries). The FDA has recently approved this 274 mg ER formulation of amantadine (presented as equivalent to 340 mg/day of the IR formulation) for the treatment of LIDs. Theoretically, once-daily intake of amantadine ER at bedtime might offer some benefits over the IR formulation, including increased compliance and better tolerance, as it exhibits a slow initial rise in plasma concentration, a delayed Tmax of 12 h with sustained high plasma concentrations during waking hours, when LIDs and OFF symptoms can be most bothersome. Unfortunately, direct double-blind head-to-head parallel or switch sequential comparisons of both formulations are lacking. The exact equivalence between the IR and ER doses is not clear, which might complicate attempts to compare their clinical effects. Moreover, the IR formulation can be used at flexible doses (from 100 to 400 mg/day), while the ER formulation 274 mg ADS-5102 once nightly is the sole dose that has been assessed in Phase III, as it was considered as providing the best balance between efficacy and safety from the Phase II study. At the moment, the added value of the novel ER formulation is therefore uncertain, while the cost-effectiveness of using this novel but more expensive formulation rather than older and cheaper generics of the IR formulation remains to be demonstrated.
Amantadine has also some antiparkinsonian effects which are poorly known, but explains its traditional use as monotherapy in early PD. Results of a recent meta-analysis showed significant reductions of UPDRS motor scores with amantadine IR (Kong et al. 2017). Notwithstanding, size effect was 1.86 points, which is below the 6.1 minimal clinically important difference (MCID) (Hauser et al. 2014). The effects of amantadine ER on OFF-time seem more robust, in the sense that they were detected in two randomized placebo-controlled trials (Pahwa et al. 2017; Oertel et al. 2017), and approached the MCID of 1.0–1.3 h (Hauser et al. 2014). This is quite a unique profile, as all other antiparkinsonian drugs marketed to reduce time spent OFF do so at the expense of a worsening of LIDs. Finally, some non-motor symptoms might respond to amantadine treatment as suggested by Ory-Magne et al. (2014) for apathy and fatigue. A positive effect of amantadine on fatigue has been reported in other neurological disorders (Van Reekum et al. 1995; Zifko 2004), and this should be better tested in PD patients. To our best knowledge, there is no information yet about the effects of amantadine ER on non-motor symptoms.
The impact of the early use of amantadine on the subsequent development of LIDs is unknown. It is theoretically conceivable that this strategy may provide a long-term “disease-modifying” effect, preventing the emergence or reducing the risk of subsequent LIDs. The French NS-Park/FCRIN network is currently testing this hypothesis in the PREMANDYSK trial (NCT01538329), a randomized, double-blind, placebo-controlled study that is prospectively following for 18 months 200 patients with early PD (< 3 years from diagnosis) who have been treated with l-DOPA for less than 1 year and are still free of LIDs. The primary objective of this study is to demonstrate that early combination of amantadine (200 mg/day) to l-DOPA decreases the rate of subjects who will develop LIDs.
One of the factors limiting widespread clinical use of amantadine is the many adverse drug reactions associated with its use, including neuropsychiatric symptoms and cardiovascular dysfunction, especially at high doses which are most effective for the treatment of LIDs. Doses of amantadine IR used in clinical practice to manage LIDs are usually 200–300 mg per day. The daily dose for ER amantadine assessed in Phase III studies was 274 mg/day (considered to be equivalent to 340 mg amantadine IR), induced up to 20% of hallucinations, leg edema and dizziness, while AEs leading to treatment discontinuation occurred in 21% patients vs 7% on placebo. This is not trivial. Amantadine should probably be avoided, or doses kept to the minimum possible in patients with other risk factors for these conditions. Results from the study of Verhagen Metman et al. (1998b) indicated that 8 mcg/ml are related to a 50% reduction in LIDs, which according to previous results can be achieved with doses between 100 and 200 mg/day of amantadine IR (Nishikawa et al. 2009). There have not been proper dose-finding studies which might justify the efficacy of lower doses to be used in high-risk patient populations, and further dose-finding studies are required to improve the care of our patients.
References
Adamas Pharmaceuticals (2017) Summary of product characteristics: Gocovri, amantadine extended-release. https://www.gocovri.com/. Accessed 02 Oct 2017
Ahlskog JE, Muenter MD (2001) Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord 16(3):448–458
Allers KA, Bergstrom DA, Ghazi LJ, Kreiss DS, Walters JR (2005) MK801 and amantadine exert different effects on subthalamic neuronal activity in a rodent model of Parkinson’s disease. Exp Neurol 191(1):104–118. https://doi.org/10.1016/j.expneurol.2004.08.030
Alliance Pharmaceuticals (2010) Summary of product characteristics: Symmetrel(R) capsules (amantadine hydrochloride 100 mg)
Alonso Navarro H, Sanz-Aiz A, Izquierdo L, Jimenez Jimenez FJ (2009) Syndrome of inappropriate antidiuretic hormone secretion possibly associated with amantadine therapy in Parkinson disease. Clin Neuropharmacol 32(3):167–168. https://doi.org/10.1097/WNF.0b013e3181900115
Aoki FY, Sitar DS (1988) Clinical pharmacokinetics of amantadine hydrochloride. Clin Pharmacokinet 14(1):35–51. https://doi.org/10.2165/00003088-198814010-00003
Aron Badin R, Spinnewyn B, Gaillard MC, Jan C, Malgorn C, Van Camp N, Dolle F, Guillermier M, Boulet S, Bertrand A, Savasta M, Auguet M, Brouillet E, Chabrier PE, Hantraye P (2013) IRC-082451, a novel multitargeting molecule, reduces l-DOPA-induced dyskinesias in MPTP Parkinsonian primates. PLoS ONE 8(1):e52680. https://doi.org/10.1371/journal.pone.0052680
Bezard E, Tronci E, Pioli EY, Li Q, Porras G, Bjorklund A, Carta M (2013) Study of the antidyskinetic effect of eltoprazine in animal models of levodopa-induced dyskinesia. Mov Disord 28(8):1088–1096. https://doi.org/10.1002/mds.25366
Bibbiani F, Oh JD, Kielaite A, Collins MA, Smith C, Chase TN (2005) Combined blockade of AMPA and NMDA glutamate receptors reduces levodopa-induced motor complications in animal models of PD. Exp Neurol 196(2):422–429. https://doi.org/10.1016/j.expneurol.2005.08.017
Bido S, Marti M, Morari M (2011) Amantadine attenuates levodopa-induced dyskinesia in mice and rats preventing the accompanying rise in nigral GABA levels. J Neurochem 118(6):1043–1055. https://doi.org/10.1111/j.1471-4159.2011.07376.x
Birkmayer W, Hornykiewicz O (1998) The effect of l-3,4-dihydroxyphenylalanine (= DOPA) on akinesia in parkinsonism. Parkinsonism Relat Disord 4(2):59–60
Blanchet PJ, Konitsiotis S, Chase TN (1998) Amantadine reduces levodopa-induced dyskinesias in parkinsonian monkeys. Mov Disord 13(5):798–802. https://doi.org/10.1002/mds.870130507
Blanpied TA, Clarke RJ, Johnson JW (2005) Amantadine inhibits NMDA receptors by accelerating channel closure during channel block. J Neurosci 25(13):3312–3322. https://doi.org/10.1523/JNEUROSCI.4262-04.2005
Bortolanza M, Bariotto-Dos-Santos KD, Dos-Santos-Pereira M, da-Silva CA, Del-Bel E (2016) Antidyskinetic effect of 7-nitroindazole and sodium nitroprusside associated with amantadine in a rat model of Parkinson’s disease. Neurotox Res 30(1):88–100. https://doi.org/10.1007/s12640-016-9618-4
Boyd JT, Silverman DA (2013) Amantadine-induced patulous eustachian tubes in Parkinson’s disease. Case Rep Otolaryngol 2013:426413. https://doi.org/10.1155/2013/426413
Brenner M, Haass A, Jacobi P, Schimrigk K (1989) Amantadine sulphate in treating Parkinson’s disease: clinical effects, psychometric tests and serum concentrations. J Neurol 236(3):153–156
Calabresi P, Ghiglieri V, Mazzocchetti P, Corbelli I, Picconi B (2015) Levodopa-induced plasticity: a double-edged sword in Parkinson’s disease? Philos Trans R Soc Lond B Biol Sci. https://doi.org/10.1098/rstb.2014.0184
Calabresi P, Pisani A, Rothwell J, Ghiglieri V, Obeso JA, Picconi B (2016) Hyperkinetic disorders and loss of synaptic downscaling. Nat Neurosci 19(7):868–875. https://doi.org/10.1038/nn.4306
Cattoni J, Parekh R (2014) Acute respiratory distress syndrome: a rare presentation of amantadine toxicity. Am J Case Rep 15:1–3. https://doi.org/10.12659/ajcr.889931
Chang KC, Jeong JH, Kim MK, Wee WR, Lee JH, Jeon BS (2010) The effect of amantadine on corneal endothelium in subjects with Parkinson’s disease. Ophthalmology 117(6):1214–1219. https://doi.org/10.1016/j.ophtha.2009.10.039
Chase TN, Oh JD (2000) Striatal dopamine- and glutamate-mediated dysregulation in experimental parkinsonism. Trends Neurosci 23(10 Suppl):S86–S91
Chaudhuri KR, Schapira AH (2009) Non-motor symptoms of Parkinson’s disease: dopaminergic pathophysiology and treatment. Lancet Neurol 8(5):464–474
Cheng PL, Hung SW, Lin LW, Chong CF, Lau CI (2008) Amantadine-induced serotonin syndrome in a patient with renal failure. Am J Emerg Med 26(1):112.e115–116.e115. https://doi.org/10.1016/j.ajem.2007.07.015
da Silva-Junior FP, Braga-Neto P, Sueli Monte F, de Bruin VM (2005) Amantadine reduces the duration of levodopa-induced dyskinesia: a randomized, double-blind, placebo-controlled study. Parkinsonism Relat Disord 11(7):449–452. https://doi.org/10.1016/j.parkreldis.2005.05.008
Damiano AM, McGrath MM, Willian MK, Snyder CF, LeWitt PA, Reyes PF, Richter RR, Means ED (2000) Evaluation of a measurement strategy for Parkinson’s disease: assessing patient health-related quality of life. Qual Life Res 9(1):87–100
Deep P, Dagher A, Sadikot A, Gjedde A, Cumming P (1999) Stimulation of dopa decarboxylase activity in striatum of healthy human brain secondary to NMDA receptor antagonism with a low dose of amantadine. Synapse 34(4):313–318 (https://doi.org/10.1002/(SICI)1098-2396(19991215)34:4<313:AID-SYN7>3.0.CO;2-1)
Dekundy A, Lundblad M, Danysz W, Cenci MA (2007) Modulation of l-DOPA-induced abnormal involuntary movements by clinically tested compounds: further validation of the rat dyskinesia model. Behav Brain Res 179(1):76–89. https://doi.org/10.1016/j.bbr.2007.01.013
Del Dotto P, Pavese N, Gambaccini G, Bernardini S, Metman LV, Chase TN, Bonuccelli U (2001) Intravenous amantadine improves levadopa-induced dyskinesias: an acute double-blind placebo-controlled study. Mov Disord 16(3):515–520
Deleu D, Northway MG, Hanssens Y (2002) Clinical pharmacokinetic and pharmacodynamic properties of drugs used in the treatment of Parkinson’s disease. Clin Pharmacokinet 41(4):261–309. https://doi.org/10.2165/00003088-200241040-00003
Fahn S, Oakes D, Shoulson I, Kieburtz K, Rudolph A, Lang A, Olanow CW, Tanner C, Marek K (2004) Levodopa and the progression of Parkinson’s disease. N Engl J Med 351(24):2498–2508
Faulkner MA (2014) Safety overview of FDA-approved medications for the treatment of the motor symptoms of Parkinson’s disease. Expert Opin Drug Saf 13(8):1055–1069. https://doi.org/10.1517/14740338.2014.931369
Fisher A, Biggs CS, Starr MS (1998) Effects of glutamate antagonists on the activity of aromatic l-amino acid decarboxylase. Amino Acids 14(1–3):43–49
Foller M, Geiger C, Mahmud H, Nicolay J, Lang F (2008) Stimulation of suicidal erythrocyte death by amantadine. Eur J Pharmacol 581(1–2):13–18. https://doi.org/10.1016/j.ejphar.2007.11.051
Fox SH, Katzenschlager R, Lim SY, Ravina B, Seppi K, Coelho M, Poewe W, Rascol O, Goetz CG, Sampaio C (2011) The Movement Disorder Society evidence-based medicine review update: treatments for the motor symptoms of Parkinson’s disease. Mov Disord 26(Suppl 3):S2–41. https://doi.org/10.1002/mds.23829
Fryml LD, Williams KR, Pelic CG, Fox J, Sahlem G, Robert S, Revuelta GJ, Short EB (2017) The role of amantadine withdrawal in 3 cases of treatment-refractory altered mental status. J Psychiatr Pract 23(3):191–199. https://doi.org/10.1097/pra.0000000000000237
Goetz CG (1998) New lessons from old drugs: amantadine and Parkinson’s disease. Neurology 50(5):1211–1212
Goetz CG, Stebbins GT, Chung KA, Hauser RA, Miyasaki JM, Nicholas AP, Poewe W, Seppi K, Rascol O, Stacy MA, Nutt JG, Tanner CM, Urkowitz A, Jaglin JA, Ge S (2013) Which dyskinesia scale best detects treatment response? Mov Disord 28(3):341–346. https://doi.org/10.1002/mds.25321
Goetz CG, Stebbins GT, Chung KA, Nicholas AP, Hauser RA, Merkitch D, Stacy MA (2017) Topiramate as an adjunct to amantadine in the treatment of dyskinesia in Parkinson’s disease: a randomized, double-blind, placebo-controlled multicenter study. Mov Disord. https://doi.org/10.1002/mds.27092
Goralski KB, Smyth DD, Sitar DS (1999) In vivo analysis of amantadine renal clearance in the uninephrectomized rat: functional significance of in vitro bicarbonate-dependent amantadine renal tubule transport. J Pharmacol Exp Ther 290(2):496–504
Grace AA (2008) Physiology of the normal and dopamine-depleted basal ganglia: insights into levodopa pharmacotherapy. Mov Disord 23(Suppl 3):S560–S569. https://doi.org/10.1002/mds.22020
Hauser RA, Gordon MF, Mizuno Y, Poewe W, Barone P, Schapira AH, Rascol O, Debieuvre C, Frassdorf M (2014) Minimal clinically important difference in Parkinson’s disease as assessed in pivotal trials of pramipexole extended release. Parkinsons Dis 2014:467131. https://doi.org/10.1155/2014/467131
Hauser RA, Pahwa R, Tanner CM, Oertel W, Isaacson SH, Johnson R, Felt L, Stempien MJ (2017) ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson’s disease (EASE LID 2 study): interim results of an open-label safety study. J Parkinsons Dis 7(3):511–522. https://doi.org/10.3233/jpd-171134
Heikkila RE, Cohen G (1972) Evaluation of amantadine as a releasing agent or uptake blocker for H 3-dopamine in rat brain slices. Eur J Pharmacol 20(2):156–160
Hesselink MB, De Boer AG, Breimer DD, Danysz W (1999) Adaptations of NMDA and dopamine D2, but not of muscarinic receptors following 14 days administration of uncompetitive NMDA receptor antagonists. J Neural Transm (Vienna) 106(5–6):409–421. https://doi.org/10.1007/s007020050168
Hill MP, Ravenscroft P, Bezard E, Crossman AR, Brotchie JM, Michel A, Grimee R, Klitgaard H (2004) Levetiracetam potentiates the antidyskinetic action of amantadine in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-lesioned primate model of Parkinson’s disease. J Pharmacol Exp Ther 310(1):386–394. https://doi.org/10.1124/jpet.104.066191
Horadam VW, Sharp JG, Smilack JD, McAnalley BH, Garriott JC, Stephens MK, Prati RC, Brater DC (1981) Pharmacokinetics of amantadine hydrochloride in subjects with normal and impaired renal function. Ann Intern Med 94(4 pt 1):454–458
Hubsher G, Haider M, Okun MS (2012) Amantadine: the journey from fighting flu to treating Parkinson disease. Neurology 78(14):1096–1099. https://doi.org/10.1212/WNL.0b013e31824e8f0d
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184
Huot P, Johnston TH, Koprich JB, Fox SH, Brotchie JM (2013) The pharmacology of l-DOPA-induced dyskinesia in Parkinson’s disease. Pharmacol Rev 65(1):171–222. https://doi.org/10.1124/pr.111.005678
Jackisch R, Link T, Neufang B, Koch R (1992) Studies on the mechanism of action of the antiparkinsonian drugs memantine and amantadine: no evidence for direct dopaminomimetic or antimuscarinic properties. Arch Int Pharmacodyn Ther 320:21–42
Johnston TH, Huot P, Fox SH, Koprich JB, Szeliga KT, James JW, Graef JD, Letchworth SR, Jordan KG, Hill MP, Brotchie JM (2013) TC-8831, a nicotinic acetylcholine receptor agonist, reduces l-DOPA-induced dyskinesia in the MPTP macaque. Neuropharmacology 73:337–347. https://doi.org/10.1016/j.neuropharm.2013.06.005
Kaefer V, Semedo JG, Silva Kahl VF, Von Borowsky RG, Gianesini J, Ledur Kist TB, Pereira P, Picada JN (2010) DNA damage in brain cells and behavioral deficits in mice after treatment with high doses of amantadine. J Appl Toxicol 30(8):745–753. https://doi.org/10.1002/jat.1550
Kataoka H, Ueno S (2011) Dropped head associated with amantadine in Parkinson disease. Clin Neuropharmacol 34(1):48–49. https://doi.org/10.1097/WNF.0b013e318204d35c
Kim YE, Yun JY, Yang HJ, Kim HJ, Kim MK, Wee WR, Jeon BS (2013) Amantadine induced corneal edema in a patient with primary progressive freezing of gait. J Mov Disord 6(2):34–36. https://doi.org/10.14802/jmd.13008
Ko WK, Pioli E, Li Q, McGuire S, Dufour A, Sherer TB, Bezard E, Facheris MF (2014) Combined fenobam and amantadine treatment promotes robust antidyskinetic effects in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-lesioned primate model of Parkinson’s disease. Mov Disord 29(6):772–779. https://doi.org/10.1002/mds.25859
Kobylecki C, Hill MP, Crossman AR, Ravenscroft P (2011) Synergistic antidyskinetic effects of topiramate and amantadine in animal models of Parkinson’s disease. Mov Disord 26(13):2354–2363. https://doi.org/10.1002/mds.23867
Kong M, Ba M, Ren C, Yu L, Dong S, Yu G, Liang H (2017) An updated meta-analysis of amantadine for treating dyskinesia in Parkinson’s disease. Oncotarget. https://doi.org/10.18632/oncotarget.17622
Koppel C, Tenczer J (1985) A revision of the metabolic disposition of amantadine. Biomed Mass Spectrom 12(9):499–501
Korchounov A, Kessler KR, Schipper HI (2004) Differential effects of various treatment combinations on cardiovascular dysfunction in patients with Parkinson’s disease. Acta Neurol Scand 109(1):45–51
Kornhuber J, Bormann J, Hubers M, Rusche K, Riederer P (1991) Effects of the 1-amino-adamantanes at the MK-801-binding site of the NMDA-receptor-gated ion channel: a human postmortem brain study. Eur J Pharmacol 206(4):297–300
Koziorowski D, Friedman A (2007) Levodopa “drug holiday” with amantadine infusions as a treatment of complications in Parkinson’s disease. Mov Disord 22(7):1033–1036. https://doi.org/10.1002/mds.21448
Kubo S, Iwatake A, Ebihara N, Murakami A, Hattori N (2008) Visual impairment in Parkinson’s disease treated with amantadine: case report and review of the literature. Parkinsonism Relat Disord 14(2):166–169. https://doi.org/10.1016/j.parkreldis.2007.03.003
Lang AE, Lozano AM (1998) Parkinson’s disease. First of two parts. N Engl J Med 339(15):1044–1053
Lee PY, Tu HP, Lin CP, Chang CH, Cheng KC, Lin CC, Hsu SL (2016) Amantadine use as a risk factor for corneal edema: a nationwide cohort study in Taiwan. Am J Ophthalmol 171:122–129. https://doi.org/10.1016/j.ajo.2016.08.034
Luginger E, Wenning GK, Bosch S, Poewe W (2000) Beneficial effects of amantadine on l-dopa-induced dyskinesias in Parkinson’s disease. Mov Disord 15(5):873–878
Lundblad M, Usiello A, Carta M, Hakansson K, Fisone G, Cenci MA (2005) Pharmacological validation of a mouse model of l-DOPA-induced dyskinesia. Exp Neurol 194(1):66–75. https://doi.org/10.1016/j.expneurol.2005.02.002
Lupp A, Lucking CH, Koch R, Jackisch R, Feuerstein TJ (1992) Inhibitory effects of the antiparkinsonian drugs memantine and amantadine on N-methyl-d-aspartate-evoked acetylcholine release in the rabbit caudate nucleus in vitro. J Pharmacol Exp Ther 263(2):717–724
Marxreiter F, Winkler J, Uhl M, Madzar D (2017) A case report of severe delirium after amantadine withdrawal. Case Rep Neurol 9(1):44–48. https://doi.org/10.1159/000460814
Matsubayashi H, Swanson KL, Albuquerque EX (1997) Amantadine inhibits nicotinic acetylcholine receptor function in hippocampal neurons. J Pharmacol Exp Ther 281(2):834–844
McNamara P, Durso R (1991) Reversible pathologic jealousy (Othello syndrome) associated with amantadine. J Geriatr Psychiatry Neurol 4(3):157–159
Metman LV, Del Dotto P, LePoole K, Konitsiotis S, Fang J, Chase TN (1999) Amantadine for levodopa-induced dyskinesias: a 1-year follow-up study. Arch Neurol 56(11):1383–1386
Mizoguchi K, Yokoo H, Yoshida M, Tanaka T, Tanaka M (1994) Amantadine increases the extracellular dopamine levels in the striatum by re-uptake inhibition and by N-methyl-d-aspartate antagonism. Brain Res 662(1–2):255–258
Montel S, Bonnet A-M, Bungener C (2009) Quality of life in relation to mood, coping strategies, and dyskinesia in Parkinson’s disease. J Geriatr Psychiatry Neurol 22(2):95–102. https://doi.org/10.1177/0891988708328219
Moresco RM, Volonte MA, Messa C, Gobbo C, Galli L, Carpinelli A, Rizzo G, Panzacchi A, Franceschi M, Fazio F (2002) New perspectives on neurochemical effects of amantadine in the brain of parkinsonian patients: a PET-[(11)C]raclopride study. J Neural Transm 109(10):1265–1274. https://doi.org/10.1007/s00702-002-0694-7
Nishikawa N, Nagai M, Moritoyo T, Yabe H, Nomoto M (2009) Plasma amantadine concentrations in patients with Parkinson’s disease. Parkinsonism Relat Disord 15(5):351–353. https://doi.org/10.1016/j.parkreldis.2008.08.005
Obeso JA, Marin C, Rodriguez-Oroz C, Blesa J, Benitez-Temino B, Mena-Segovia J, Rodriguez M, Olanow CW (2008) The basal ganglia in Parkinson’s disease: current concepts and unexplained observations. Ann Neurol 64(Suppl 2):S30–S46. https://doi.org/10.1002/ana.21481
Oertel W, Eggert K, Pahwa R, Tanner CM, Hauser RA, Trenkwalder C, Ehret R, Azulay JP, Isaacson S, Felt L, Stempien MJ (2017) Randomized, placebo-controlled trial of ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson’s disease (EASE LID 3). Mov Disord. https://doi.org/10.1002/mds.27131
Olanow WC, Kieburtz K, Rascol O, Poewe W, Schapira AH, Emre M, Nissinen H, Leinonen M, Stocchi F, Stalevo Reduction in Dyskinesia Evaluation in Parkinson’s Disease I (2013) Factors predictive of the development of levodopa-induced dyskinesia and wearing-off in Parkinson’s disease. Mov Disord 28(8):1064–1071. https://doi.org/10.1002/mds.25364
Ory-Magne F, Corvol JC, Azulay JP, Bonnet AM, Brefel-Courbon C, Damier P, Dellapina E, Destee A, Durif F, Galitzky M, Lebouvier T, Meissner W, Thalamas C, Tison F, Salis A, Sommet A, Viallet F, Vidailhet M, Rascol O, Network NS-PC (2014) Withdrawing amantadine in dyskinetic patients with Parkinson disease: the AMANDYSK trial. Neurology 82(4):300–307. https://doi.org/10.1212/WNL.0000000000000050
Paci C, Thomas A, Onofrj M (2001) Amantadine for dyskinesia in patients affected by severe Parkinson’s disease. Neurol Sci 22(1):75–76
Pahwa R, Tanner CM, Hauser RA, Sethi K, Isaacson S, Truong D, Struck L, Ruby AE, McClure NL, Went GT, Stempien MJ (2015) Amantadine extended release for levodopa-induced dyskinesia in Parkinson’s disease (EASED study). Mov Disord. https://doi.org/10.1002/mds.26159
Pahwa R, Tanner CM, Hauser RA, Isaacson SH, Nausieda PA, Truong DD, Agarwal P, Hull KL, Lyons KE, Johnson R, Stempien MJ (2017) ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson disease (EASE LID study): a randomized clinical trial. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2017.0943
Paquette MA, Martinez AA, Macheda T, Meshul CK, Johnson SW, Berger SP, Giuffrida A (2012) Anti-dyskinetic mechanisms of amantadine and dextromethorphan in the 6-OHDA rat model of Parkinson’s disease: role of NMDA vs. 5-HT1A receptors. Eur J Neurosci 36(9):3224–3234. https://doi.org/10.1111/j.1460-9568.2012.08243.x
Parsons CG, Panchenko VA, Pinchenko VO, Tsyndrenko AY, Krishtal OA (1996) Comparative patch-clamp studies with freshly dissociated rat hippocampal and striatal neurons on the NMDA receptor antagonistic effects of amantadine and memantine. Eur J Neurosci 8(3):446–454
Pèchevis M, Clarke CE, Vieregge P, Khoshnood B, Deschaseaux-voinet C, Berdeaux G, Ziegler M (2005) Effects of dyskinesias in Parkinson’ s disease on quality of life and health-related costs : a prospective European study. Eur J Neurol 12:956–963
Peeters M, Page G, Maloteaux JM, Hermans E (2002) Hypersensitivity of dopamine transmission in the rat striatum after treatment with the NMDA receptor antagonist amantadine. Brain Res 949(1–2):32–41
Perez-Lloret S, Barrantes FJ (2016) Deficits in cholinergic neurotransmission and their clinical correlates in Parkinson’s disease. NPJ Parkinson’s Dis 2:16001–16012
Perez-Lloret S, Rey MV, Fabre N, Ory F, Spampinato U, Senard JM, Pavy-Le Traon A, Montastruc JL, Rascol O (2012) Factors related to orthostatic hypotension in Parkinson’s disease. Parkinsonism Relat Disord 18(5):501–505. https://doi.org/10.1016/j.parkreldis.2012.01.012
Perez-Lloret S, Negre-Pages L, Damier P, Delval A, Derkinderen P, Destee A, Meissner WG, Tison F, Rascol O, Group CS (2017) l-DOPA-induced dyskinesias, motor fluctuations and Health-related Quality of Life: the COPARK survey. Eur J Neurol. https://doi.org/10.1111/ene.13466
Pimentel L, Hughes B (1991) Amantadine toxicity presenting with complex ventricular ectopy and hallucinations. Pediatr Emerg Care 7(2):89–92
Pringsheim T, Jette N, Frolkis A, Steeves TD (2014) The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 29(13):1583–1590. https://doi.org/10.1002/mds.25945
Quaresma MV, Gomes AC, Serruya A, Vendramini DL, Braga L, Bucard AM (2015) Amantadine-induced livedo reticularis—case report. Ann Bras Dermatol 90(5):745–747. https://doi.org/10.1124/jpet.115.230201 (https://doi.org/10.1590/abd1806-4841.20153394)
Rana AQ, Masroor MS (2012) Patient perception of Levido reticularis due to amantadine. Int J Neurosci 122(7):363–366. https://doi.org/10.3109/00207454.2012.668727
Reichmann H, Emre M (2012) Optimizing levodopa therapy to treat wearing-off symptoms in Parkinson’s disease: focus on levodopa/carbidopa/entacapone. Expert Rev Neurother 12(2):119–131. https://doi.org/10.1586/ern.11.203
Reis J, John D, Heimeroth A, Mueller HH, Oertel WH, Arndt T, Rosenow F (2006) Modulation of human motor cortex excitability by single doses of amantadine. Neuropsychopharmacology 31(12):2758–2766. https://doi.org/10.1038/sj.npp.1301122
Reuther M, Spottke EA, Klotsche J, Riedel O, Peter H, Berger K, Athen O, Khne-Volland R, Dodel RC (2007) Assessing health-related quality of life in patients with Parkinson’s disease in a prospective longitudinal study. Parkinsonism Relat Disord 13(2):108–114. https://doi.org/10.1016/j.parkreldis.2006.07.009
Rohrbacher J, Bijak M, Misgeld U (1994) Suppression by memantine and amantadine of synaptic excitation intrastriatally evoked in rat neostriatal slices. Neurosci Lett 182(1):95–98
Ruzicka E, Streitova H, Jech R, Kanovsky P, Roth J, Rektorova I, Mecir P, Hortova H, Bares M, Hejdukova B, Rektor I (2000) Amantadine infusion in treatment of motor fluctuations and dyskinesias in Parkinson’s disease. J Neural Transm (Vienna) 107(11):1297–1306. https://doi.org/10.1007/s007020070019
Sartori M, Pratt CM, Young JB (1984) Torsade de Pointe. Malignant cardiac arrhythmia induced by amantadine poisoning. Am J Med 77(2):388–391
Sawada H, Oeda T, Kuno S, Nomoto M, Yamamoto K, Yamamoto M, Hisanaga K, Kawamura T, Amantadine Study G (2010) Amantadine for dyskinesias in Parkinson’s disease: a randomized controlled trial. PLoS One 5(12):e15298. https://doi.org/10.1371/journal.pone.0015298
Schwartz M, Patel M, Kazzi Z, Morgan B (2008) Cardiotoxicity after massive amantadine overdose. J Med Toxicol 4(3):173–179
Sebastianutto I, Maslava N, Hopkins CR, Cenci MA (2016) Validation of an improved scale for rating l-DOPA-induced dyskinesia in the mouse and effects of specific dopamine receptor antagonists. Neurobiol Dis 96:156–170
Seier M, Hiller A (2017) Parkinson’s disease and pregnancy: an updated review. Parkinsonism Relat Disord 40:11–17. https://doi.org/10.1016/j.parkreldis.2017.05.007
Snoey ER, Bessen HA (1990) Acute psychosis after amantadine overdose. Ann Emerg Med 19(6):668–670
Snow BJ, Macdonald L, McAuley D, Wallis W (2000) The effect of amantadine on levodopa-induced dyskinesias in Parkinson’s disease: a double-blind, placebo-controlled study. Clin Neuropharmacol 23(2):82–85
Stoof JC, Booij J, Drukarch B, Wolters EC (1992) The anti-parkinsonian drug amantadine inhibits the N-methyl-d-aspartic acid-evoked release of acetylcholine from rat neostriatum in a non-competitive way. Eur J Pharmacol 213(3):439–443
Takahashi T, Yamashita H, Zhang YX, Nakamura S (1996) Inhibitory effect of MK-801 on amantadine-induced dopamine release in the rat striatum. Brain Res Bull 41(6):363–367
Thomas A, Iacono D, Luciano AL, Armellino K, Di Iorio A, Onofrj M (2004) Duration of amantadine benefit on dyskinesia of severe Parkinson’s disease. J Neurol Neurosurg Psychiatry 75(1):141–143
Thomas A, Bonanni L, Gambi F, Di Iorio A, Onofrj M (2010) Pathological gambling in Parkinson disease is reduced by amantadine. Ann Neurol 68(3):400–404. https://doi.org/10.1002/ana.22029
Van Reekum R, Bayley M, Garner S, Burke IM, Fawcett S, Hart A, Thompson W (1995) N of 1 study: amantadine for the amotivational syndrome in a patient with traumatic brain injury. Brain Inj 9(1):49–53
Verhagen Metman L, Del Dotto P, Blanchet PJ, van den Munckhof P, Chase TN (1998a) Blockade of glutamatergic transmission as treatment for dyskinesias and motor fluctuations in Parkinson’s disease. Amino Acids 14(1–3):75–82
Verhagen Metman L, Del Dotto P, van den Munckhof P, Fang J, Mouradian MM, Chase TN (1998b) Amantadine as treatment for dyskinesias and motor fluctuations in Parkinson’s disease. Neurology 50(5):1323–1326
Volonte MA, Moresco RM, Gobbo C, Messa C, Carpinelli A, Rizzo G, Comi G, Fazio F (2001) A PET study with [11-C]raclopride in Parkinson’s disease: preliminary results on the effect of amantadine on the dopaminergic system. Neurol Sci 22(1):107–108
Voon V, Fernagut PO, Wickens J, Baunez C, Rodriguez M, Pavon N, Juncos JL, Obeso JA, Bezard E (2009) Chronic dopaminergic stimulation in Parkinson’s disease: from dyskinesias to impulse control disorders. Lancet Neurol 8(12):1140–1149. https://doi.org/10.1016/S1474-4422(09)70287-X
Weintraub D, Sohr M, Potenza MN, Siderowf AD, Stacy M, Voon V, Whetteckey J, Wunderlich GR, Lang AE (2010) Amantadine use associated with impulse control disorders in Parkinson disease in cross-sectional study. Ann Neurol 68(6):963–968. https://doi.org/10.1002/ana.22164
Wolf E, Seppi K, Katzenschlager R, Hochschorner G, Ransmayr G, Schwingenschuh P, Ott E, Kloiber I, Haubenberger D, Auff E, Poewe W (2010) Long-term antidyskinetic efficacy of amantadine in Parkinson’s disease. Mov Disord 25(10):1357–1363. https://doi.org/10.1002/mds.23034
Zifko UA (2004) Management of fatigue in patients with multiple sclerosis. Drugs 64(12):1295–1304
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Perez-Lloret, S., Rascol, O. Efficacy and safety of amantadine for the treatment of l-DOPA-induced dyskinesia. J Neural Transm 125, 1237–1250 (2018). https://doi.org/10.1007/s00702-018-1869-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-018-1869-1