Abstract
Transcranial direct current stimulation (tDCS) is a non-invasive brain stimulation method that has shown promising results in various neuropsychiatric disorders in adults. This review addresses the therapeutic use of tDCS in children and adolescents including safety, ethical, and legal considerations. There are several studies addressing the dosage of tDCS in children and adolescents by computational modeling of electric fields in the pediatric brain. Results suggest halving the amperage used in adults to obtain the same peak electric fields, however, there are some studies reporting on the safe application of tDCS with standard adult parameters in children (2 mA; 20–30 min). There are several randomized placebo controlled trials suggesting beneficial effects of tDCS for the treatment of cerebral palsy. For dystonia there are mixed data. Some studies suggest efficacy of tDCS for the treatment of refractory epilepsy, and for the improvement of attention deficit/hyperactivity disorder and autism. Interestingly, there is a lack of data for the treatment of childhood and adolescent psychiatric disorders, i.e., childhood onset schizophrenia and affective disorders. Overall, tDCS seems to be safe in pediatric population. More studies are needed to confirm the preliminary encouraging results; however, ethical deliberation has to be weighed carefully for every single case.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transcranial direct current stimulation (tDCS) is a non-invasive brain stimulation technique with application of constant weak direct current (e.g. 1–2 mA) to the brain via skin–electrode interface. Although brain galvanisation is known since ancient history and has been pursued over centuries, modern neurophysiological research followed the seminal experiments of Bindman et al. (1964) who found that application of direct current (DC) modulates spontaneous neuronal activity in the rat brain in a polarity-dependent manner. Several studies with DC application in animals and humans followed in the 1960s and 1970s, suggesting some efficacy of DC stimulation in depression, however, mixed results led to an abandonment of this research direction (Nitsche et al. 2009). Nitsche and Paulus (2000) reactivated the research on electrical brain stimulation at the beginning of the 21st century and found a modulation of motor cortex excitability after anodal and cathodal polarization which they called tDCS. Contrarily to transcranial magnetic stimulation (TMS), tDCS provokes a sub-threshold modulation of neuronal excitability without depolarizing action potentials. This modulation is polarity-dependent toward depolarization after anodal stimulation (=excitatory) and toward hyperpolarization after cathodal stimulation (=inhibitory), leading to transient changes in the resting membrane potential. The cumulative effect of longer stimulation results in a polarity-dependent facilitation or inhibition of the spontaneous neuronal firing rate (Nitsche et al. 2003) and is considered neuromodulatory. Post stimulation effects of tDCS are also depending from the duration of stimulation and last from several minutes up to some hours and can be found in the areas under the electrodes and also remote by network changes. For tDCS of the primary motor cortex, these excitability changes can be measured by amplitude changes of motor evoked potentials (MEP) after single pulses of TMS over the cortical representation area of finger muscles (abductor digiti minimi, abductor pollicis brevis, first digitus interosseous) (Nitsche and Paulus 2001). Thus, MEP changes are viewed as a surrogate for non-focal neuroplasticity, i.e., the activity-dependent change of neuronal functioning. Modern tDCS research looks back on a history of 15 years of neurophysiological and clinical studies, including one decade of research in the treatment of depressive disorders in adults (Palm et al. 2016). Due to the promising results in adult psychiatric disorders and the low rate of adverse effects, tDCS has gained interest in the treatment of childhood and adolescent neuropsychiatric disorders over the past years. This review aims to comprehensively assess research directions and clinical findings of tDCS application in childhood and adolescent neuropsychiatric disorders.
Methods
The search engine of the US National Institutes of Health (Pubmed) was used to retrieve the respective literature until mid-February 2016. The search term “tDCS + children” retrieved 108 hits, the search term “tDCS + adolescent” 177 hits. Review articles, meta-analyzes, clinical trials and case reports were considered. After the exclusion of irrelevant literature (conference proceedings, papers without reference to children/adolescents or brain stimulation), “tDCS + children” retrieved 40 hits, and “tDCS + adolescents” after filtering for duplicates 18 hits. References of the retrieved articles were searched for further literature.
Results
Rationale for the use of tDCS in children and adolescents
There are various neuropsychiatric and developmental disorders that are commonly treated by standardized rehabilitation therapy, as well as partially by psychopharmacology and psychotherapy. Despite effective (physio)-therapeutic treatments for neuropsychiatric developmental disorders with motor deficits, there is a need for improvement of cognitive dysfunction and psychiatric symptoms in a variety of disorders that are only inadequately covered by pharmacological or psycho-social interventions. Therefore, non-invasive brain stimulation methods, i.e. TMS, have been investigated in childhood and adolescents neuropsychiatric disorders and TMS has shown promising results (Krishnan et al. 2015; Rajapakse and Kirton 2013). Another, more recent non-invasive brain stimulation method is tDCS that seems to cause less uncomfortable side effects in adults than TMS. Common side effects for TMS application are headache, facial and cranial muscle contractions due to the magnet impulse, and very rarely seizures. For tDCS, headache and burning/tingling skin sensations (itching sensation when the current flow irritates skin nerves) under the electrodes are reported. Thus, tDCS application in childhood and adolescent neuropsychiatric disorders was following the promising results in psychiatric disorders and a low rate of side effects in adults. Children and adolescents show accelerated neural plasticity compared to adults (Brunoni et al. 2012; Kolb and Teskey 2012; Stortelder and Ploegmakers-Burg 2010), therefore, tDCS could be useful to regulate and enhance plasticity; however, it could theoretically also worsen brain development and alter cognitive function in unintended ways, e.g., by wrong placement of electrodes, reversing the polarity, interaction with pharmacological treatment, or unintended long lasting effects that occur after enhanced or repeated treatment (Fitz and Reiner 2015; Reiner 2013). With regard to the development of non-invasive brain stimulation methods in the last years, tDCS may be used for two functions in pediatric patients (Chung and Lo 2015):
-
1.
For a diagnostic purpose to characterize physiological and pathological states of the nervous system, e.g., by measuring excitability and plasticity; and
-
2.
For a therapeutic purpose with the use of repeated or continuous brain stimulation to enhance or inhibit neural activity in the target brain region.
Concerning diagnostic purposes, non-invasive brain stimulation can be used to investigate neuronal excitability and plasticity and its interhemispheric connections. Usually neuronal plasticity is measured by preconditioning single pulse TMS-elicited motor evoked potentials (MEP) with anodal or cathodal tDCS over the primary motor cortex, leading to increased or decreased MEP responses as a measure for plasticity (Nitsche and Paulus 2000). Disturbed interhemispheric connectivity and plasticity is a frequent finding in a variety of psychiatric disorders in adults pointing to the hypothesis of dysconnectivity in neuropsychiatric disorders, e.g., in schizophrenia (Hasan et al. 2012a; Schmitt et al. 2011).
Concerning therapeutic purposes, non-invasive brain stimulation aims to change regional neuronal activity that is assumed to be in a dysfunctional hypo- or hyperactive state. Effects of local stimulation spread out by neuronal network changes into more remote areas and lead to rearrangement of disturbed neuronal circuits. Thus, placement of TMS pulses or tDCS electrodes depends on the assumption of pathophysiological changes in distinct brain areas that may be modulated by changes in neuronal excitability. Effects, therefore, depend on an increase of local excitability by anodal tDCS to enhance a desired brain function in the targeted area and on a decrease by cathodal tDCS to reduce an undesired brain function. As tDCS needs a closed current circuit, the reference electrode is usually placed over an area that is deemed functionally inert in terms of the targeted symptoms. Therefore, tDCS could play a major role in the treatment of developmental disorders, e.g., learning difficulties, dyscalculia, and others. To date, it is not yet extensively and systematically investigated, probably due to unawareness of medical personnel or due to the fear of a potentially harmful intervention (Krause and Cohen Kadosh 2013).
Ethical and legal aspects
The core problem of the evidence of therapeutic tDCS interventions in children is the limited data. The main concern is about the vulnerability of the pediatric/adolescent population and the ethic aspects of investigating new and potentially incalculable techniques (Reiner 2013). Randomized controlled trials have a further ethical disadvantage to offer a promising therapy only to a part of participants. Therefore, new techniques are often investigated in compassionate use until they are deemed to be safe in a pediatric population. In view of the controversial discussions which have surrounded the issue of TMS in children or adolescent patients regarding the question of use, safety, and ethical aspects, a consensus conference issued recommendations on TMS in 2009 (Rossi 2009). As proposed for tDCS, the development of consensus guidelines could help to steer clinical research and to answer patients’ and parents’ requests for non-invasive brain stimulation (Reiner 2013).
Davis (2014) calls for “extreme caution” in the use of non-invasive brain stimulation and points out four major issues:
-
1.
the lack of knowledge regarding the effects of treatment,
-
2.
the lack of knowledge concerning side effects,
-
3.
the lack of clear guidelines for dosage, and
-
4.
especially the lack of translational studies from adults to children, seeing as children are not and should not be treated as small adults.
He emphasizes that a child’s brain is still developing, a process that is not yet fully understood (Davis 2014). Researchers have to take into account that neuroanatomical differences of children’s brains will impact their stimulation protocols based on an adult population, thus same tDCS parameters will have larger impact in children and adolescents (Kolb and Teskey 2012; Reiner 2013). This could lead to unexpected or even dangerous results as it misdirects plasticity or causes brain tissue lesion due to the thinner skull of the pediatric population, resulting in higher peak current density in the children’s brain.
In light of the growing importance of brain stimulation even in minors, Maslen et al. (2014) extensively discussed ethical aspects. They underline the importance of distinguishing between enhancement and treatment before drawing conclusions, as treatment contains by definition a pathology that threatens the child’s well-being. In the absence of reasonable alternatives, even the risk of significant side effects could be outweighed by the method’s benefits. However, lacking a clear pathology, the question of the child’s autonomy (i.e., intellectual maturity) should carry greater relative weight. Maslen et al. (2014) request that brain stimulation purely for enhancement should be delayed until the patient has reached the state of intellectual maturity. Regardless from bioethical or legal viewpoints, the question if non-invasive brain stimulation methods used as a neuroenhancement undermine autonomy as well as self-determination in children and adolescents also has a variety of philosophical aspects and has been discussed controversially, e.g., that neuroenhancement could be ‘dehumanizing’ versus neuroenhancement could ‘improve humanity’ (Bostrom 2005; Maslen et al. 2014). At the same time, from a more legal view, it has to be questioned if and how far a child is capable to give informed consent to an intervention that surmounts simple diagnostics, e.g., a blood withdrawal. Thus, Maslen et al. (2014) recommend that the consent to brain stimulation for any reason but treatment should not be possible for adolescents under the age of 16. To conclude, most ethical considerations conform the opinion that there are no ethical reasons against tDCS in children and adolescents in the case of a medical pathology threatening the child’s well-being and especially in the absence of a reasonable alternative.
Concerning legal issues there is acceptance of ‘galvanic micropolarization’ methods by medical regulatory authorities since many years in Russia (Pinchuk et al. 2013) and they are used for a variety of disorders, e.g., cerebral palsy, associated deficits in motor and mental development, and ADHD (Ilyukhina et al. 2005) (see also: https://sites.google.com/site/micropolarization/). However, there are no laws in either Europe or the United States that regulate the use of tDCS in minors. Even in adults tDCS is still an investigative application that is used for off-label treatment in Europe or the USA (Fregni et al. 2015). A comprehensive documentation of medical considerations, failure or contraindication of alternative interventions as well as written and oral informed consent of both children/adolescents and parents about the new method and possible side effects of tDCS are mandatory.
Computational models of current flow
Several studies addressed the dosage adaption of tDCS for use in the pediatric brain. This takes into account the smaller skull thickness and corticospinal fluid volume resulting in a smaller scalp-brain distance as well as differences in gray and white matter differentiation (Group 2012; Beauchamp et al. 2011). Therefore, current strength and duration usually deemed safe in adults (e.g. 2 mA, 20–30 min) have to be adjusted. Kessler et al. (2013) performed a computational model study comparing current distribution by different electrode montages in magnet resonance imaging (MRI) derived head models. They compared three adults’ and two children’s head models with temporal, prefrontal, and motor cortex stimulation with standard sponge (25 cm2) and 4 × 1 high definition ring electrodes. They found that peak electrical fields in children are higher when using standard stimulation parameters. Furthermore, they found that applied current strength ~1 mA in children is comparable to the densities seen in the adult brain at 2 mA current strength. Another modeling study by Minhas et al. (2012) used an MRI derived finite element model of a 12 year old healthy child, compared to a standard adult model. They also used 25 cm2 standard sponge electrodes (anode: C3; cathode: supraorbital contralateral) versus 4 × 1 high definition ring electrode over C3 and found that same stimulation intensity (2 mA) provoked a 1.5-fold higher peak electric field in the child model and that modulation of cortical tissue was deeper in the child than in the adult model at 1.5 mA. Although similar patterns of current flow were observed in child and adult model, peak electric fields were higher in the child model (Minhas et al. 2012). Parazzini et al. (2014) performed computational models of three healthy children (6, 8, 11 years) with the cathode over C3-F3 (35 cm2) and the anode over contralateral orbit, respectively contralateral shoulder to assess current flow for the treatment of refractory childhood epilepsy. Their analysis of 1 mA current strength revealed more cortical peak amplitudes under the anode and the cathode when using the cortical electrode montage, and an asymmetric current distribution with the peak under the cathode when using the extracephalic montage, reaching more deep brain structures and the cerebellum. They conclude that the extracephalic montage does not influence the peak current density under the cathode, albeit deeper brain structures.
Finally, Gillick et al. (2014) used a head model to design a tDCS protocol for pediatric stroke. For this purpose, the field of the 35 cm2 electrode was modeled over M1/supraorbital and C3/C4 as target regions of pediatric stroke in a 10 year old child with perinatal ischemic stroke and hemiparesis. Calculation was made with 0.7 mA and current distribution was assumed to be safe for 10 min (to rest within established safety parameters) and the child was afterwards treated with these parameters in M1/supraorbital montage without adverse events. Peak electric fields resembled to those seen in the adult brain at 1 mA.
Safety and dosage of tDCS in children and adolescents
Andrade et al. (2014) investigated the application of 30 min of 2 mA tDCS over 10 days in 14 children (5–12 years) suffering from different neuropsychiatric disorders (expressive language disorder, dyspraxia, pervasive developmental disorder, Asperger syndrome). Main adverse effects were mood changes, discomfort of skin perception (itching, tingling, burning), headache and sleepiness. The authors discuss that some of these symptoms reported may be attributed to the disorder itself rather than to the stimulation. The only study regarding safety of tDCS in childhood onset schizophrenia demonstrated safety and tolerability of repeated 2 mA tDCS (10 sessions, 20 min) in twelve patients (Mattai et al. 2011). Ekici (2015) reported on a seizure after anodal tDCS for improvement of spasticity in a 4 year old boy with tetraparesis and a history of epilepsy. However, the context of tDCS and seizure is not clear by the description and other factors may have contributed.
Adverse effects of tDCS in children and adolescents was systematically reviewed by Krishnan et al. (2015) and they found skin sensations (itching, tingling, redness, scalp discomfort, etc.) to be the most frequent adverse effects, however, mood change does not seem to be a critical issue.
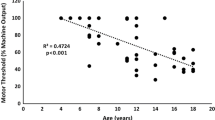
Adverse effects were also investigated by Moliadze et al. (2015a) in 19 children (mean age 13.9 years; range 11–16) in a randomized controlled cross over trial with EEG and motor evoked potentials (MEP) measures before and after a 10 min/1 mA tDCS. Anodal, cathodal, and sham tDCS (electrode 35 cm2) were applied over C3 with the reference electrode over the contralateral orbit. Standardized questionnaires revealed frequent occurrence of well-known tDCS induced side effects like itching, tingling, and headache. Occurrence was not different between stimulation conditions and participants were not able to correctly guess the type of stimulation. EEG showed a decrease of all bands after tDCS except for alpha band after active tDCS. Spectra analyzes showed a decrease in delta and theta bands after anodal and cathodal stimulation. The MEP results were published separately (Moliadze et al. 2015b) and showed an increase of amplitudes after anodal and cathodal 1 mA tDCS. This result contrasted the notion of excitability decrease after cathodal tDCS, therefore, the authors performed the same experiment with 0.5 mA and found excitability decrease after cathodal tDCS and no changes after anodal tDCS. They hypothesize that 1 mA tDCS in children could already have a ceiling effect and that 0.5 mA in children probably correspond to 1 mA in adults.
Safety and feasibility of a single session of tDCS in patients with congenital hemiparesis was assessed by Gillick et al. (2015a). Thirteen patients (7–18 years) underwent TMS to assess cortical excitability (motor evoked potentials) of the affected hemisphere before receiving a single session of 0.7 mA tDCS for 10 min with the anode over the ipsilateral motor cortex and the cathode over the contralateral motor cortex. TMS-elicited motor evoked potentials showed inconsistent changes in both hemispheres. tDCS was well tolerated, change of vital sign or worsening of motor function did not occur.
Interestingly, studies do not define chronological age uniformly to separate between children and adolescents. Most studies include children from 5 to 12 years, some others until 15 years. Some other studies including persons up to 18 (respectively 21) years report to have included ‘children and adolescents’. Furthermore, differentiation between chronological and biological age is not discussed in the studies or in review articles dealing with safety of non-invasive brain stimulation in children and adolescents, e.g. Krishnan et al. (2015).
tDCS for ADHD
Treatment of Attention Deficit and Hyperactivity Disorder (ADHD) with non-invasive brain stimulation techniques, i.e. TMS and tDCS, has recently been reviewed by Rubio et al. (2015). One of the most influential theories of the neural basis of ADHD has focused on deficient inhibitory control leading to executive dysfunction (Sonuga-Barke 2005; Gilbert et al. 2011) which is likely genetically influenced (Goos et al. 2009). The neuroanatomic substrate of inhibitory control has been imputed to the basal ganglia-thalamocortical circuits (Alexander et al. 1990; Christakou et al. 2004). Specifically, this network links the prefrontal cortex to the dorsal neostriatum via excitatory glutaminergic cells, the basal ganglia to the dorsomedial thalamus via inhibitory projections, and the thalamus back to the prefrontal cortex via excitatory projections (Aron et al. 2004). Inhibitory control is processed during the maturation of this circuit, and both structural and functional neuroimaging studies reveal differences in this circuit in association with ADHD (Castellanos et al. 2002; Rubia et al. 1999; Batty et al. 2010). A potential benefit of tDCS could be the improvement of behavioral inhibition, memory, and attention, as already shown in healthy adults (Ditye et al. 2012; Fregni et al. 2005) and adults with ADHD (Cosmo et al. 2015).
Soltaninejad et al. (2015) included 20 pupils with ADHD (15–17 years) in a randomized controlled clinical trial. Participants underwent three stimulations with each 1.5 mA anodal, cathodal, and sham tDCS (15 min, electrode size 35 cm2) in F3-Fp2 montage to improve inhibition control by anodal stimulation of the left DLPFC, measured by a go-no-go-task and Stroop test. Interestingly, cathodal stimulation of the left DLPFC improved no-go accuracy in the go-no-go-task. This broadens previous findings in adults suggesting that predominantly cathodal stimulation of the right DLPFC improves inhibitory control. The Stroop test did not show significant differences between both groups.
Bandeira et al. (2016) conducted an open-label study including 9 children with ADHD (mean age 11.1 years, range 7–15). Patients performed a card matching game for training during five sessions of 2 mA tDCS (30 min, anode over left DLPFC, cathode right supraorbital). Attentional changes were measured by a visual attention test, a digit span test, the Corsi cubes, and an inhibitory control task. There was an improvement of selective attention and a decrease of errors in the inhibitory control task. Most tests revealed lower errors rates and shorter run time.
Munz et al. (2015) hypothesized that slow-oscillating tDCS (so-tDCS; unipolar current flow with undulating current strength) could interact with physiological slow-oscillating neuronal activity during sleep and could enhance inhibition in ADHD. Fourteen children (12.3 years mean; range 10–14) underwent active and sham so-tDCS (0.75 Hz; two stimulators: anodal F3 + F4, cathodal: both mastoids; electrode size: 13 mm round electrodes; current 0–250 µA) at non-REM sleep stage 2 for 5 × 5 min with 1 min break for EEG recording after each stimulation. The next morning, a go-no-go-task was performed and showed a shorter reaction time after active stimulation, whereas alertness showed no difference between groups. Active so-tDCS increased slow-oscillatory power in REM sleep stage 4.
Another study focusing on impaired memory consolidation by modulation of slow-wave activity during non-REM sleep phase 2 was conducted by Prehn-Kristensen et al. (2014). Twelve boys with ADHD (12.1 years mean, range 10–14) and 12 healthy boys (11.9 years mean, range 9–14) underwent a memory task (card game) before receiving so-tDCS with the same protocol reported by Munz et al. (2015), however, no stimulation was performed in the healthy boys due to ethical concerns. ADHD children showed worse memory performance (retrieval) compared to healthy children that vanished after so-tDCS and reached the level of the healthy children.
In sum, tDCS over prefrontal areas seems to have some efficacy in ADHD (Table 1), however, standardized study protocols are needed to determine polarity and frequency of application. Except for one randomized controlled trial, the quality of the reported studies is debatable due to several methodological and procedural shortcomings.
tDCS for autism
Autism spectrum disorder (ASD), a neurodevelopmental disorder with a prevalence rate of 6.2/1000 (Elsabbagh et al. 2012; Levy et al. 2009) is defined by three core symptoms: (1) impaired language and communication, (2) deficits in social interactions, and (3) restricted or repetitive behaviors and interests. Furthermore, it is frequently associated with a variety of health-related problems, e.g., sensory abnormalities, sleep disturbances, and gastrointestinal symptoms (Geschwind 2009). Although pathophysiology of ASD has still to be elucidated (Trottier et al. 1999), brain imaging studies detected an increased volume of right hemispheric brain structures associated with language and social function compared with patients’ left hemispheres and with healthy controls (Herbert et al. 2002). In addition, ASD patients showed a hypoactivation in the left hemisphere compared with the right hemisphere (Cardinale et al. 2013; Floris et al. 2013; Kleinhans et al. 2008; Lindell and Hudry 2013). Pathophysiology models of ASD include abnormal synaptic maturation, disturbed brain connectivity, and mirror neuron dysfunction (Dinstein et al. 2008; Hamilton 2008; Iacoboni and Dapretto 2006; Persico and Bourgeron 2006). Neurophysiology examinations revealed lower EEG alpha activity in ASD children compared with healthy controls (Cantor et al. 1986; Chan et al. 2007).
Therefore, Amatachaya et al. (2015) investigated whether anodal tDCS could increase in alpha frequency to increase synaptic connectivity, thus resulting in an improvement of ASD symptoms. They performed an RCT with twenty male ASD children receiving anodal tDCS over F3 (2 mA, 20 min) and found significant improvement in social and health/behavior scales of the autism treatment evaluation checklist (ATEC) and an increase of peak alpha frequency under the site of anodal stimulation. Behavioral changes were correlated to alpha frequency changes and suggest a potential role of tDCS to improve ASD symptoms by modulation of DLPFC action.
For the modulation of behavior, measured by the childhood autism rating scale (CARS) and the ATEC, Amatachaya et al. (2014) performed another RCT with twenty ASD children with 1 mA tDCS over 5 days (anode over F3). Both rating scales improved significantly after the active stimulation compared with sham.
Costanzo et al. (2015) reported on the case of a 14-year old girl with ASD and drug-refractory catatonia who was treated with 1 mA tDCS (20 min, 28 treatments, anode F3, cathode F4) and showed a 30 % improvement of catatonia symptoms, stable for 1 month.
Retardation of speech development in 10 children/adolescents (6–21 years) with ASD was investigated by Schneider and Hopp (2011) with 2 mA anodal stimulation (30 min, electrode size 25 cm2) over the left DLPFC (cathode Fp2). Despite elevated stimulation parameters, tDCS was well tolerated and vocabulary scores (syntax comprehension) increased after tDCS.
Overall, different aims of the studies mentioned above and syndromal diversity of the disorder do not allow to draw any conclusion for the use of tDCS in ASD (Table 1). The quality of the studies is heterogeneous including two randomized controlled clinical trials and one open-label study and one case report.
tDCS for childhood onset schizophrenia
Childhood-onset schizophrenia (COS) is defined as the onset of psychosis before 13 years of age (Rapoport 2004). Patients with this rare, severe, and nonepisodic form of disorder show symptoms resembling the chronic and treatment refractory schizophrenia in adults (Rapoport et al. 2005). Antipsychotic drugs are the first-line treatment to control psychotic symptoms in COS, however, insufficient efficacy and a high level of adverse events related to medication have been shown in previous studies with first generation antipsychotics (Campbell et al. 1999). As in adults, negative symptoms are severely resistant to medication (Stahl and Buckley 2007; Hasan et al. 2012b) and mainly account to the specific neurocognitive function loss, decline of social cognition, and working memory (Leucht and Lasser 2006). In adults, tDCS seems to exert some positive effects on different schizophrenia symptoms, e.g., improvement of negative symptoms by anodal stimulation of the left DLPFC and reduction of auditory hallucinations by cathodal stimulation of the left temporo-parietal junction (Mondino et al. 2015).
To date, the study of Mattai et al. (2011) is the only one to investigate tDCS in COS (Table 1). The primary focus of this study was to evaluate the tolerability of bilateral frontal/temporal tDCS in COS. Twelve children (10–17 years) were assigned to two groups either receiving bilateral anodal tDCS to the DLPFC for cognitive difficulties or bilateral cathodal tDCS to the superior temporal gyrus stimulation for auditory hallucinations at 2 mA for 20 min. The reference electrodes were placed on the non-dominant forearm. Patients were randomized to receive active or sham stimulation over 10 days. Those patients assigned to sham group were offered an open label active phase afterwards. There were neither clinically significant changes in mood, arousal, global cognitive performance (Mini Mental Status Examination), or verbal output during active or sham tDCS, nor any significant change in autonomous measures (respiration, blood pressure, or heart rate) or general adverse effects over time. Cranial MRI (t1-weighted) did not show any alterations after tDCS. The clinical data were not reported due to the limited number of patients.
Future directions in the treatment of COS comprise the systematic assessment of tDCS with enhanced stimulation parameters, the effects of a combination of antipsychotics and tDCS, and the combination of tDCS with neuroimaging (David et al. 2013).
tDCS for epilepsy
The rationale for the use of tDCS in childhood epilepsy is deriving from the neuromodulatory effect of tDCS, i.e., cathodal tDCS, leading to a reduction of cortical excitability by different mechanisms, e.g., decrease of neuronal firing rate and induction of long-term depression (LTD) of neuronal excitability in animal studies. Animal models support the hypothesis of a tDCS-induced elevation of seizure threshold (Liebetanz et al. 2006). An early study reported on the use of 0.3–0.7 mA tDCS for 20–40 min (max. 15 treatments, anode posterior temporal, cathode parietal cortex) in 18 patients (4–8 years, various diagnoses: cerebral palsy, organic brain lesions, generalized epilepsy) (Shelyakin et al. 2001). All children improved concerning seizure frequency, no generalized or focal paroxysmal activity was observed after tDCS and epileptiform activity was insignificant. Furthermore, slow wave activity was decreased.
A sham controlled, crossover trial in 5 children (6–11 years) with a syndrome of refractory continuous spikes and waves in sleep (CSWSS) showed safety and tolerability of cathodal stimulation with 1 mA for 20 min over the area of epileptiform discharges with a large return electrode (100 cm2) (Varga et al. 2011). No difference between active cathodal (1 mA, 20 min) and sham stimulation regarding reduction of spike-index during slow wave sleep was found. Auvichayapat et al. (2013) investigated the effects of 1 mA cathodal tDCS for 20 min in 36 children with focal epilepsy. The 3:1 active:sham randomization design revealed a significant reduction of epileptiform discharges after active tDCS up to 48 h after tDCS. Active stimulation was well tolerated, skin reaction occurred in one patient.
Yook et al. (2012) reported the case of an 11 year old girl with epilepsy treated with 2 mA/20 min cathodal tDCS over the epileptic zone (right temporo-parietal) for 10 days. Application of these elevated parameters was safe and epileptiform discharges were reduced after stimulation. Another case report by Faria et al. (2012) included two 7- and 11-year-old children with refractory epilepsy. Repeated sessions of 1 mA stimulation/30 min during slow wave sleep with the cathode over C5–C6 resulted in a reduction of interictal epileptiform discharges during after tDCS. San-Juan et al. (2011) reported two cases of Rasmussen’s Encephalitis treated with cathodal tDCS for seizures. One of these two cases was a 17 year old adolescent with secondarily generalized seizures despite antiepileptic combination treatment. After application of 2 mA tDCS for 30 min (4 sessions in 2 months, cathode F2, anode F8), there was a mild improvement of partial seizure frequency, stable up to 6 months after tDCS.
Overall, data on tDCS treatment in pediatric epilepsy is sparse and stimulation protocols are heterogeneous, furthermore data is collected mostly in case reports and an open-label study; there are only two sham controlled studies (Table 1). Follow-up periods are rather short and further limit the available evidence.
tDCS for movement disorders
The use of tDCS in the treatment of childhood dystonia, a disorder characterized by involuntary muscle contractions with repetitive movements and/or abnormal postures (Sanger et al. 2010), is made on the assumption that tDCS modulates motor learning in various disorders, e.g. Parkinson’s disease (Fregni et al. 2006) or stroke (Kang et al. 2015), by either excitatory modulation (anodal tDCS) to enhance insufficient motor function or inhibitory modulation (cathodal tDCS) to diminish overshooting motor function. Bhanpuri et al. (2015) treated nine dystonia patients (10–21 years old) with anodal and cathodal tDCS (2 mA, 9 min, 10 sessions) as well as sham tDCS for both electrode positions. The anode and cathode were placed over C3 and C4, respectively, contralateral to the most affected limb, and the reference electrode was placed over the contralateral forehead. Movement changes were recorded by electromyogram of the first dorsal interosseous muscle in a finger tracking task (tracking a visually presented target by voluntary muscle action of the first digitus interosseus). tDCS was well tolerated, however, cathodal and anodal stimulation results were inconsistent and anodal tDCS even worsened motor performance in patients. These results are in contrast to previous studies where cathodal tDCS showed a beneficial effect on dystonia (Young et al. 2013, 2014). The first study by Young et al. (2013) investigated the effect of cathodal tDCS in 11 patients (7–18 years) with different types of dystonia (e.g., cerebral palsy, idiopathic, etc.) in an open label design. Cathode was placed over C3 or C4, contralateral to the most affected hemisphere; the anode was placed over the contralateral forehead. Stimulation was performed for 9 min at 1 mA current strength, followed by 20 min break and another 9 min stimulation period. An electromyogram-based finger tracking task showed an improvement in active control over muscle activity after tDCS and a partially reduced involuntary overflow. The Barry-Albright Dystonia Scale was unchanged. Overall, the stimulation protocol was well tolerated, one patient withdrew, and another noticed scalp discomfort. Young et al. (2014) repeated the same study design in a sham controlled randomized double blind trial, and included 14 children with various types of dystonia. Active tDCS reduced motor overflow in few children, however, there was no significant superiority of active cathodal compared to sham tDCS. Stimulation was well tolerated, two patients reported scalp discomfort.
The results of tDCS application in movement disorders are heterogeneous and are limited by different patient samples and stimulation protocols. Two of the three reported studies are sham controlled clinical trials (Table 1).
tDCS for cerebral palsy and developmental deficits
Cerebral palsy (CP) is a permanent motor development disorder resulting from a primary brain lesion, and is followed by secondary musculoskeletal problems and limited ability to participate sufficiently in the activities of daily living (Rosenbaum et al. 2007). Aerobic exercise alone seems to have no sufficient treatment effect; therefore, additional treatment strategies are needed, e.g., the combination of physiotherapeutic training with non-invasive brain stimulation methods to improve the exercising effect.
There are several early studies using pulsed transcranial electrical stimulation (short electrical stimuli of some milliseconds with intervals between) for the treatment of cerebral palsy in children and adolescents (Alon et al. 1998; Malden and Charash 1985; Okoye and Malden 1986). All studies reported a beneficial effect of active stimulation compared to sham stimulation regarding improvement of physiotherapeutic training, and stimulation was well tolerated. Although pilot studies suggested promising results, pulsed transcranial electrical stimulation was not further assessed in cerebral palsy in Europe or the USA, however, in Russia, ‘galvanic micropolarization’ (synonymous for tDCS) has a longer tradition in the treatment of cerebral palsy or other neuropsychiatric developmental disorders with residual organic background. Ilyukhina et al. (2005) reported on 30 children (4–6 years) with delayed neuropsychological development due to several brain diseases who were treated with 0.03–0.08 mA tDCS for 15–20 min over frontal and parietal areas of the left hemisphere. After an individual treatment phase with several blocks of up to 6 stimulations (blocks separated by at least on week interval) and standard speech rehabilitation program, children with greater impairment showed moderate improvement compared to children with lower impairment and better outcome.
Recent research focused on randomized controlled clinical trials to investigate the effect of tDCS on physiotherapeutic training, e.g., the study protocols for a combination of tDCS and constraint-induced movement therapy (Gillick et al. 2015b) or tDCS and treadmill training (Grecco et al. 2013). Clinical results of the Gillick study protocol are not yet available. The results of the Grecco study protocol (Grecco et al. 2013) have been already published (Grecco et al. 2014a) and are reported in Table 2. There are several other randomized placebo controlled trials (Aree-uea et al. 2014; Grecco et al. 2014b; Duarte et al. 2014; Lazzari et al. 2015; Collange Grecco et al. 2015) and one open label study (Bogdanov et al. 1994) reported in Table 2. Overall, anodal tDCS over the primary motor cortex over the more lesioned/affected hemisphere combined with standard physiotherapeutic training or as a monotherapeutic approach seems to provoke an increase of mobility, gait distance, body sway velocity, and balance and a decrease of spasticity, for a short period already after a single tDCS session and more sustained after a tDCS series, reaching from several weeks to a few months.
Finally, Grecco et al. (2014c) published a single case report of a 3 year old child with delayed psychomotor development treated with treadmill training and add-on tDCS (1 mA, 20 min, anode C3/C4, cathode supraorbital contralateral, each 10 stimulations on both hemispheres). They observed an improvement of oscillations, step length, and gait velocity, and the child began to walk independently.
In sum, there is some evidence that tDCS improves motor functioning after combined physiotherapeutic treatment and tDCS. However, study designs are heterogeneous and follow-up periods are short. There is a need for longer treatment and observation protocols. The quality of the reported studies is relatively high, consisting mostly in sham controlled clinical studies.
tDCS for developmental dyslexia
The use of tDCS developmental dyslexia, an isolated impairment to learn reading, has been proposed by Vicario and Nitsche (2013) under the assumption that dysfunction in relevant brain structures, i.e., the left and right middle occipital gyrus, the left superior temporal gyrus, and the left and right inferior frontal gyrus, could be improved by tDCS in combination with standard speech remediation programs. Costanzo et al. (2016a, b) conducted two studies addressing the impact of left anodal/right cathodal tDCS to enhance left parietotemporal neuronal activity. In the first study (Costanzo et al. 2016a), 19 children and adolescents with dyslexia (mean age 13 years, range 10–17) were treated with 1 mA tDCS for 20 min in three conditions: left anodal (F7-Tp7), right cathodal (F8-Tp8); left cathodal, right anodal; sham condition in left anodal/right temporal montage. The sessions were separated by an interval of at least 24 h. Patients underwent several neuropsychological tests including word and text reading, lexical decision, phoneme blending, naming task, and verbal n-back at baseline and after the three interventions. The left anodal/right cathodal stimulation was significantly superior to baseline, sham, and right anodal/left cathodal stimulation in terms of text reading accuracy and decrease of errors. Conversely, right anodal/left cathodal stimulation significantly reduced accuracy and increased error rate compared to baseline, sham, and left anodal/right cathodal stimulation. However, high-frequency words, low-frequency words, and non-word tasks did not show relevant differences between the conditions. The authors discuss that only one tDCS session could have led to limited effects on dyslexia. Participants reported only mild side effects, such as tingling or burning; mood changes were not reported. In their second study, Costanzo et al. (2016b) applied a longer stimulation protocol with 18 tDCS sessions (1 mA, 20 min, anode left parieto-temporal, cathode contralateral) within 6 weeks. 18 children and adolescents were randomly assigned to active or sham group and were additionally treated with cognitive training including text reading, high and low frequency wording, and non-word tasks. The active group showed a lower error rate in low frequency word reading and shorter delay in non-word reading compared to the sham group up to 1 month after end of stimulation series. Adverse effects did not occur. The authors discuss that tDCS improves non-word and low-frequency word reading in children and adolescents with dyslexia.
Overall, data is too sparse to draw any conclusion for this disorder although both studies were sham controlled (Table 1).
tDCS in other disorders
Khedr et al. (2014) conducted a pilot study in 7 anorexia patients, four of them were 16 and 17 years old. tDCS was applied 10 times at 2 mA for 25 min with the anode over the left DLPFC and the cathode at the right arm. There was no clear and sustained improvement of depressive symptoms, eating behavior and insight facilitation; however, tDCS was well tolerated in the juvenile patients. The authors discuss that the improvement of depressive symptoms by tDCS could be the key to mediate insight facilitation and weight gain.
Pinchuk et al. (2013) reported on the treatment of chronic posttraumatic headache with ‘transcranial micropolarization’ (monophasic electrical stimulation with low amperage over longer periods) in 44 adolescents (13.6 years mean, range 11–16) with different electrode positions: anode frontal and cathode ipsilateral mastoid; anode center forehead and cathode 2 cm over mastoid on the dominant hemisphere; anode frontal pole and cathode 2 cm over mastoid on non-dominant hemisphere. A current of 60–90 µA was applied for 30–45 min in 5–9 sessions. Results and tolerability are not differentially reported for the different montages. The second electrode position was effective in 6 adolescents to reduce headache. A possible reason for the low responder rates could be the low current strength used in this study.
Conclusions
Although there are several expert position papers proposing the therapeutic application of tDCS in child and adolescent psychiatry, there is a lack of supporting data except for pilot studies or case reports addressing the safety of repeated tDCS in single disorders: Though computational models of current flow in the brain suggest the reduction of the applied current strength in children to a half of the amperage usually applied in adults (i.e. 2 mA, 20–30 min), higher intensities have been used in many studies. Of note, no severe adverse events are reported at this time and even in epilepsy, tDCS does not seem to worsen seizures. However, there are no longitudinal studies to explore the impact of tDCS in the developing brain although tDCS in its current parameters is performed since more than a decade in humans. At the moment, there are highly heterogeneous study designs and applied stimulation parameters that hamper comparability of results. Furthermore it remains elusive if age and gender specific differences impact tDCS efficacy.
The application of tDCS or ‘galvanic micropolarization’ has a longer history in the treatment of movement disorders and spasticity in neurodevelopmental disorders, whereas the treatment of psychiatric disorders is underrepresented except for some data in the treatment of ADHD and autism. Interestingly, pediatric depression is not covered by the literature although tDCS for depressive disorders has been investigated since a decade in adults (Palm et al. 2016). For the treatment of COS, there is one safety study without reporting on clinical results. Thus, it remains unclear if tDCS could be a treatment option in children and adolescents with affective or psychotic disorders. Furthermore, the treatment of substance abuse disorders in children and adolescents with tDCS is not investigated yet although there is already some promising data in adults. To date, most randomized placebo controlled clinical trials have investigated the therapeutic application of tDCS in movement disorders due to cerebral palsy and provide predominantly positive data on the efficacy of a combined tDCS and physiotherapeutic treatment. The use of tDCS as a diagnostic tool, as proposed in the ethical and legal aspects section, is not yet covered in the literature, but could serve for the assessment of altered brain plasticity in combination with TMS or for the investigation of brain networks with functional connectivity magnet resonance imaging.
Overall, tDCS in children and adolescents may have the potential to develop to safe, tolerable, and powerful treatment option for a few neuropsychiatric and developmental disorders, taking into account specific needs and concerns in a very vulnerable population. Therefore, ethical concerns should be critically weighed in every single treatment decision. Hence, tDCS should be a tool for therapeutic purpose in neuropsychiatric disorders but not for cognitive enhancement in healthy children and adolescents.
References
Alexander GE, Crutcher MD, DeLong MR (1990) Basal gangliathalamocortical circuits: parallel substrates for motor, oculomotor, ‘‘prefrontal’’ and ‘‘limbic’’ functions. Prog Brain Res 85:119–146. doi:10.1016/S0079-6123(08)62678-3
Alon G, Syron SC, Smith GV (1998) Is transcranial electrical stimulation (tCES) a safe intervention for children with cerebral palsy? J Neuro Rehab 12:65–72
Amatachaya A, Auvichayapat N, Patjanasoontorn N, Suphakunpinyo C, Ngernyam N, Aree-Uea B et al (2014) Effect of anodal transcranial direct current stimulation on autism: a randomized double-blind crossover trial. Behav Neurol 2014:173073. doi:10.1155/2014/173073
Amatachaya A, Jensen MP, Patjanasoontorn N, Auvichayapat N, Suphakunpinyo C, Janjarasjitt S et al (2015) The short-term effects of transcranial direct current stimulation on electroencephalography in children with autism: a randomized crossover controlled trial. Behav Neurol 2015:928631. doi:10.1155/2015/928631
Andrade AC, Magnavita GM, Allegro JV, Neto CE, Lucena Rde C, Fregni F (2014) Feasibility of transcranial direct current stimulation use in children aged 5–12 years. J Child Neurol 29:1360–1365. doi:10.1177/0883073813503710
Aree-uea B, Auvichayapat N, Janyacharoen T, Siritaratiwat W, Amatachaya A, Prasertnoo J et al (2014) Reduction of spasticity in cerebral palsy by anodal transcranial direct current stimulation. J Med Assoc Thai 97:954–962
Aron AR, Robbins TW, Poldrack RA (2004) Inhibition and the right inferior frontal cortex. Trends Cogn Sci 8:170–177. doi:10.1016/j.tics.2004.02.010
Auvichayapat N, Rotenberg A, Gersner R, Ngodklang S, Tiamkao S, Tassaneeyakul W, Auvichayapat P (2013) Transcranial direct current stimulation for treatment of refractory childhood focal epilepsy. Brain Stimul 6:696–700. doi:10.1016/j.brs.2013.01.009
Bandeira ID, Guimarães RS, Jagersbacher JG, Barretto TL, de Jesus-Silva JR, Santos SN, Argollo N, Lucena R (2016) Transcranial direct current stimulation in children and adolescents with attention-deficit/hyperactivity disorder (ADHD): a pilot study. J Child Neurol
Batty MJ, Liddle EB, Pitiot A, Toro R, Groom MJ, Scerif G, Liotti M, Liddle PF, Paus T, Hollis C (2010) Cortical gray matter in attention-deficit/hyperactivity disorder: a structural magnetic resonance imaging study. J Am Acad Child Adolesc Psychiatry 49:229–238
Beauchamp MS, Beurlot MR, Fava E, Nath AR, Parikh NA, Saad ZS, Bortfeld H, Oghalai JS (2011) The developmental trajectory of brain-scalp distance from birth through childhood: implications for functional neuroimaging. PLoS One 6:e24981. doi:10.1371/journal.pone.0024981
Bhanpuri NH, Bertucco M, Young SJ, Lee AA, Sanger TD (2015) Multiday transcranial direct current stimulation causes clinically insignificant changes in childhood dystonia: a pilot study. J Child Neurol 30:1604–1615. doi:10.1177/0883073815575369
Bindman LJ, Lippold OC, Redfearn JW (1964) The action of brief polarizing currents in the cerebral cortex of the rat (1) during current flow and (2) in the production of long-lasting after-effects. J Physiol 172:369–382
Bogdanov OG, Pinchuk DY, Pisar’kova EV, Shelyakin AM, Sirbiladze KT (1994) The use of the method of transcranial micropolarization to decrease the severity hyperkineses in patients with infantile cerebral palsy. Neurosci Behav Physiol 24:442–445
Bostrom N (2005) In defence of posthuman dignity. Bioethics 19:202–214
Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, Edwards DJ, Valero-Cabre A, Rotenberg A, Pascual-Leone A, Ferrucci R, Priori A, Boggio PS, Fregni F (2012) Clinical research with transcranial direct current stimulation (tDCS): challenges and future directions. Brain Stimul 5:175–195. doi:10.1016/j.brs.2011.03.002
Campbell M, Rapoport JL, Simpson GM (1999) Antipsychotics in children and adolescents. J Am Acad Child Adolesc Psychiatry 38:537–545
Cantor DS, Thatcher RW, Hrybyk M, Kaye H (1986) Computerized EEG analyses of autistic children. J Autism Dev Disord 16:69–187
Cardinale RC, Shih P, Fishman I, Ford LM, Müller RA (2013) Pervasive rightward asymmetry shifts of functional networks in autism spectrum disorder. JAMA Psychiatry 70:975–982
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, Blumenthal JD, James RS, Ebens CL, Walter JM, Zijdenbos A, Evans AC, Giedd JN, Rapoport JL (2002) Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA 288:1740–1748
Chan AS, Sze SL, Cheung MC (2007) Quantitative electroencephalographic profiles for children with autistic spectrum disorder. Neuropsychol 21:74–81
Christakou A, Robbins TW, Everitt BJ (2004) Prefrontal cortical-ventral striatal interactions involved in affective modulation of attentional performance: implications for corticostriatal circuit function. J Neurosci 24:773–780. doi:10.1523/JNEUROSCI.0949-03.2004
Chung MG, Lo WD (2015) Noninvasive brain stimulation: the potential for use in the rehabilitation of pediatric acquired brain injury. Arch Phys Med Rehabil 96:S129–S137. doi:10.1016/j.apmr.2014.10.013
Collange Grecco LA, de Almeida Carvalho Duarte N, Mendonça ME, Galli M, Fregni F, Oliveira CS (2015) Effects of anodal transcranial direct current stimulation combined with virtual reality for improving gait in children with spastic diparetic cerebral palsy: a pilot, randomized, controlled, double-blind, clinical trial. Clin Rehabil 29:1212–1223. doi:10.1177/0269215514566997
Cosmo C, Baptista AF, de Araújo AN, do Rosário RS, Miranda JG, Montoya P, de Sena EP (2015) A randomized, double-blind, sham-controlled trial of transcranial direct current stimulation in attention-deficit/hyperactivity disorder. PLoS One 10:e0135371. doi:10.1371/journal.pone.0135371
Costanzo F, Menghini D, Casula L, Amendola A, Mazzone L, Valeri G, Vicari S (2015) Transcranial direct current stimulation treatment in an adolescent with autism and drug-resistant catatonia. Brain Stimul 8:1233–1235. doi:10.1016/j.brs.2015.08.009
Costanzo F, Varuzza C, Rossi S, Sdoia S, Varvara P, Oliveri M, Koch G, Vicari S, Menghini D (2016a) Reading changes in children and adolescents with dyslexia after transcranial direct current stimulation. NeuroReport 27:295–300. doi:10.1097/WNR.0000000000000536
Costanzo F, Varuzza C, Rossi S, Sdoia S, Varvara P, Oliveri M, Koch G, Vicari S, Menghini D (2016b) Evidence for reading improvement following tDCS treatment in children and adolescents with Dyslexia. Restor Neurol Neurosci 34:215–226. doi:10.3233/RNN-150561
David CN, Rapoport JL, Gogtay N (2013) Treatments in context: transcranial direct current brain stimulation as a potential treatment in pediatric psychosis. Expert Rev Neurother 13:447–458. doi:10.1586/ern.13.29
Davis NJ (2014) Transcranial stimulation of the developing brain: a plea for extreme caution. Front Hum Neurosci 8:600
Dinstein I, Thomas C, Behrmann M, Heeger DJ (2008) A mirror up to nature. Curr Biol 18:R13–R18
Ditye T, Jacobson L, Walsh V, Lavidor M (2012) Modulating behavioural inhibition by tDCS combined with cognitive training. Exp Brain Res 219:363–368. doi:10.1007/s00221-012-3098-4
Duarte Nde A, Grecco LA, Galli M, Fregni F, Oliveira CS (2014) Effect of transcranial direct-current stimulation combined with treadmill training on balance and functional performance in children with cerebral palsy: a double-blind randomized controlled trial. PLoS One 9:e105777. doi:10.1371/journal.pone.0105777
Ekici B (2015) Transcranial direct current stimulation-induced seizure: analysis of a case. Clin EEG Neurosci 46:169
Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, Montiel-Nava C, Patel V, Paula CS, Wang C, Yasamy MT, Fombonne E (2012) Global prevalence of autism and other pervasive developmental disorders. Autism Res 5:160–179
Faria P, Fregni F, Sebastião F, Dias AI, Leal A (2012) Feasibility of focal transcranial DC polarization with simultaneous EEG recording: preliminary assessment in healthy subjects and human epilepsy. Epilepsy Behav 25:417–425
Fitz NS, Reiner PB (2015) The challenge of crafting policy for do-it-yourself brain stimulation. J Med Ethics 41:410–412. doi:10.1136/medethics-2013-101458
Floris DL, Chura LR, Holt RJ, Suckling J, Bullmore ET, Baron-Cohen S, Spencer MD (2013) Psychological correlates of handedness and corpus callosum asymmetry in autism: the left hemisphere dysfunction theory revisited. J Autism Dev Dis 43:1758–1772
Fregni F, Boggio PS, Nitsche M, Bermpohl F, Antal A, Feredoes E, Marcolin MA, Rigonatti SP, Silva MT, Paulus W, Pascual-Leone A (2005) Anodal transcranial direct current stimulation of prefrontal cortex enhances working memory. Exp Brain Res 166:23–30. doi:10.1007/s00221-005-2334-6
Fregni F, Boggio PS, Santos MC, Lima M, Vieira AL, Rigonatti SP, Silva MT, Barbosa ER, Nitsche MA, Pascual-Leone A (2006) Noninvasive cortical stimulation with transcranial direct current stimulation in Parkinson’s disease. Mov Disord 21:1693–1702
Fregni F, Nitsche MA, Loo CK, Brunoni AR, Marangolo P, Leite J et al (2015) Regulatory considerations for the clinical and research use of transcranial direct current stimulation (tDCS): review and recommendations from an expert panel. Clin Res Regul Aff 32:22–35
Geschwind DH (2009) Advances in autism. Ann Rev Med 60:367–380
Gilbert DL, Isaacs KM, Augusta M, Macneil LK, Mostofsky SH (2011) Motor cortex inhibition: a marker of ADHD behavior and motor development in children. Neurology 76:615–621. doi:10.1212/WNL.0b013e31820c2ebd
Gillick BT, Kirton A, Carmel JB, Minhas P, Bikson M (2014) Pediatric stroke and transcranial direct current stimulation: methods for rational individualized dose optimization. Front Hum Neurosci 8:739. doi:10.3389/fnhum.2014.00739
Gillick BT, Feyma T, Menk J, Usset M, Vaith A, Wood TJ et al (2015a) Safety and feasibility of transcranial direct current stimulation in pediatric hemiparesis: randomized controlled preliminary study. Phys Ther 95:337–349. doi:10.2522/ptj.20130565
Gillick B, Menk J, Mueller B, Meekins G, Krach LE, Feyma T, Rudser K (2015b) Synergistic effect of combined transcranial direct current stimulation/constraint-induced movement therapy in children and young adults with hemiparesis: study protocol. BMC Pediatr 15:178. doi:10.1186/s12887-015-0498-1
Goos LM, Crosbie J, Payne S, Schachar R (2009) Validation and extension of the endophenotype model in ADHD patterns of inheritance in a family study of inhibitory control. Am J Psychiatry 166:711–717. doi:10.1176/appi.ajp.2009.08040621
Grecco LA, Duarte Nde A, de Mendonça ME, Pasini H, Lima VL, Franco RC et al (2013) Effect of transcranial direct current stimulation combined with gait and mobility training on functionality in children with cerebral palsy: study protocol for a double-blind randomized controlled clinical trial. BMC Pediatr 13:168. doi:10.1186/1471-2431-13-168
Grecco LA, de Almeida Carvalho Duarte N, Mendonça ME, Cimolin V, Galli M, Fregni F, Santosoliveira C (2014a) Transcranial direct current stimulation during treadmill training in children with cerebral palsy: a randomized controlled double-blind clinical trial. Res Dev Disabil 35:2840–2848. doi:10.1016/j.ridd.2014.07.030
Grecco LA, Duarte NA, Zanon N, Galli M, Fregni F, Oliveira CS (2014b) Effect of a single session of transcranial direct-current stimulation on balance and spatiotemporal gait variables in children with cerebral palsy: a randomized sham-controlled study. Braz J Phys Ther 18:419–427
Grecco LA, Mendonça EM, Duarte NA, Zanon N, Fregni F, Oliveira CS (2014c) Transcranial direct current stimulation combined with treadmill gait training in delayed neuro-psychomotor development. J Phys Ther Sci 26:945–950. doi:10.1589/jpts.26.945
Group BD (2012) Total and regional brain volumes in a population based normative sample from 4 to 18 years: the NIH MRI study of normal brain development. Cereb Cortex 22:1–12
Hamilton AF (2008) Emulation and mimicry for social interaction: a theoretical approach to imitation in autism. Q J Exp Psychol 61:101–115
Hasan A, Aborowa R, Nitsche MA, Marshall L, Schmitt A, Gruber O et al (2012a) Abnormal bihemispheric responses in schizophrenia patients following cathodal transcranial direct stimulation. Eur Arch Psychiatry Clin Neurosci 262:415–423
Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF et al (2012b) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry 13:318–378
Herbert MR, Harris GJ, Adrien KT, Ziegler DA, Makris N, Kennedy DN, Lange NT, Chabris CF, Bakardjiev A, Hodgson J, Takeoka M, Tager-Flusberg H, Caviness VS Jr (2002) Abnormal asymmetry in language association cortex in autism. Ann Neurol 52:588–596
Iacoboni M, Dapretto M (2006) The mirror neuron system and the consequences of its dysfunction. Nat Rev Neurosci 7:942–951
Ilyukhina VA, Kozhushko NY, Matveev YK, Ponomareva EA, Chernysheva EM, Shaptilei MA (2005) Transcranial micropolarization in the combined therapy of speech and general psychomotor retardation in children of late preschool age. Neurosci Behav Physiol 35:969–976
Kang N, Summers JJ, Cauraugh JH (2015) Transcranial direct current stimulation facilitates motor learning post-stroke: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry
Kessler SK, Minhas P, Woods AJ, Rosen A, Gorman C, Bikson M (2013) Dosage considerations for transcranial direct current stimulation in children: a computational modeling study. PLoS One 8:e76112. doi:10.1371/journal.pone.0076112
Khedr EM, Elfetoh NA, Ali AM, Noamany M (2014) Anodal transcranial direct current stimulation over the dorsolateral prefrontal cortex improves anorexia nervosa: a pilot study. Restor Neurol Neurosci 32:789–797. doi:10.3233/RNN-140392
Kleinhans NM, Müller RA, Cohen DN, Courchesne E (2008) Atypical functional lateralization of language in autism spectrum disorders. Brain Res 1221:115–125
Kolb B, Teskey GC (2012) Age, experience, injury, and the changing brain. Dev Psychobiol 54:311–325
Krause B, Cohen Kadosh R (2013) Can transcranial electrical stimulation improve learning difficulties in atypical brain development? A future possibility for cognitive training. Dev Cogn Neurosci 6:176–194. doi:10.1016/j.dcn.2013.04.001
Krishnan C, Santos L, Peterson MD, Ehinger M (2015) Safety of noninvasive brain stimulation in children and adolescents. Brain Stimul 8:76–87. doi:10.1016/j.brs.2014.10.012
Lazzari RD, Politti F, Santos CA, Dumont AJ, Rezende FL, Grecco LA et al (2015) Effect of a single session of transcranial direct-current stimulation combined with virtual reality training on the balance of children with cerebral palsy: a randomized, controlled, double-blind trial. J Phys Ther Sci Mar 27:763–768. doi:10.1589/jpts.27.763
Leucht S, Lasser R (2006) The concepts of remission and recovery in schizophrenia. Pharmacopsychiatry 39:161–170
Levy SE, Mandell DS, Schultz RT (2009) Autism. Lancet 374:1627–1638
Liebetanz D, Klinker F, Hering D, Koch R, Nitsche MA, Potschka H, Löscher W, Paulus W, Tergau F (2006) Anticonvulsant effects of transcranial direct-current stimulation (tDCS) in the rat cortical ramp model of focal epilepsy. Epilepsia 47:1216–1224
Lindell AK, Hudry K (2013) Atypicalities in cortical structure, handedness, and functional lateralization for language in autism spectrum disorders. Neuropsychol Rev 23:257–270
Malden JW, Charash LI (1985) Transcranial stimulation for inhibition of primitive reflexes in children with cerebral palsy. Neurol Rep 9:33–38
Maslen H, Earp BD, Cohen Kadosh R, Savulescu J (2014) Brain stimulation for treatment and enhancement in children: an ethical analysis. Front Hum Neurosci 8:953
Mattai A, Miller R, Weisinger B, Greenstein D, Bakalar J, Tossell J, David C, Wassermann EM, Rapoport J, Gogtay N (2011) Tolerability of transcranial direct current stimulation in childhood-onset schizophrenia. Brain Stimul 4:275–280. doi:10.1016/j.brs.2011.01.001
Minhas P, Bikson M, Woods AJ, Rosen AR, Kessler SK (2012) Transcranial direct current stimulation in pediatric brain: a computational modeling study. Conf Proc IEEE Eng Med Biol Soc 2012:859–862. doi:10.1109/EMBC.2012.6346067
Moliadze V, Andreas S, Lyzhko E, Schmanke T, Gurashvili T, Freitag CM, Siniatchkin M (2015a) Ten minutes of 1 mA transcranial direct current stimulation was well tolerated by children and adolescents: self-reports and resting state EEG analysis. Brain Res Bull 119:25–33. doi:10.1016/j.brainresbull.2015.09.011
Moliadze V, Schmanke T, Andreas S, Lyzhko E, Freitag CM, Siniatchkin M (2015b) Stimulation intensities of transcranial direct current stimulation have to be adjusted in children and adolescents. Clin Neurophysiol 126:1392–1399. doi:10.1016/j.clinph.2014.10.142
Mondino M, Brunelin J, Palm U, Brunoni AR, Poulet E, Fecteau S (2015) Transcranial direct current stimulation for the treatment of refractory symptoms of schizophrenia. current evidence and future directions. Curr Pharm Des 21:3373–3383
Munz MT, Prehn-Kristensen A, Thielking F, Mölle M, Göder R, Baving L (2015) Slow oscillating transcranial direct current stimulation during non-rapid eye movement sleep improves behavioral inhibition in attention-deficit/hyperactivity disorder. Front Cell Neurosci 9:307. doi:10.3389/fncel.2015.00307
Nitsche MA, Paulus W (2000) Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol 527:633–639
Nitsche MA, Paulus W (2001) Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology 57:1899–1901
Nitsche MA, Liebetanz D, Antal A, Lang N, Tergau F, Paulus W (2003) Modulation of cortical excitability by weak direct current stimulation—technical, safety and functional aspects. Suppl Clin Neurophysiol 56:255–276
Nitsche MA, Boggio PS, Fregni F, Pascual-Leone A (2009) Treatment of depression with transcranial direct current stimulation (tDCS): a review. Exp Neurol 219:14–19
Okoye R, Malden RW (1986) Use of neurotransmitter modulation to facilitate sensory integration. Neurol Report 10:67–72
Palm U, Hasan A, Strube W, Padberg F (2016) tDCS for the treatment of depression: a comprehensive review. Eur Arch Psychiatry Clin Neurosci. doi:10.1007/s00406-016-0674-9
Parazzini M, Fiocchi S, Liorni I, Priori A, Ravazzani P (2014) Computational modelling of transcranial direct current stimulation in the child brain: implications for the treatment of refractory childhood focal epilepsy. Int J Neural Syst 24:1430006. doi:10.1142/S012906571430006X
Persico AM, Bourgeron T (2006) Searching for ways out of the autism maze: genetic, epigenetic and environmental clues. Trends Neurosci 29:349–358
Pinchuk D, Pinchuk O, Sirbiladze K, Shugar O (2013) Clinical effectiveness of primary and secondary headache treatment by transcranial direct current stimulation. Front Neurol 4:25
Prehn-Kristensen A, Munz M, Göder R, Wilhelm I, Korr K, Vahl W et al (2014) Transcranial oscillatory direct current stimulation during sleep improves declarative memory consolidation in children with attention-deficit/hyperactivity disorder to a level comparable to healthy controls. Brain Stimul 7:793–799. doi:10.1016/j.brs.2014.07.036
Rajapakse T, Kirton A (2013) Non-invasive brain stimulation in children: applications and future directions. Transl Neurosci. doi:10.2478/s13380-013-0116-3
Rapoport JL (2004) Childhood onset schizophrenia: a progressive neurodevelopmental disorder. Int J Neuropsychopharmacol 7:S22
Rapoport JL, Addington AM, Frangou S, Psych MR (2005) The neurodevelopmental model of schizophrenia: update 2005. Mol Psychiatry 10:434–449
Reiner PB (2013) Comment on “Can transcranial electrical stimulation improve learning difficulties in atypical brain development? A future possibility for cognitive training” by Krause and Cohen Kadosh. Dev Cogn Neurosci 6:195–196. doi:10.1016/j.dcn.2013.05.002
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M (2007) A report: the definition and classification of cerebral palsy. Dev Med Child Neurol 49:8–14
Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Safety of TMS Consensus Group (2009) Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120:2008–2039
Rubia K, Overmeyer S, Taylor E, Brammer M, Williams SC, Simmons A, Bullmore ET (1999) Hypofrontality in attention deficit hyperactivity disorder during higher-order motor control: a study with functional MRI. Am J Psychiatry 156:891–896
Rubio B, Boes AD, Laganiere S, Rotenberg A, Jeurissen D, Pascual-Leone A (2015) Noninvasive brain stimulation in pediatric attention-deficit hyperactivity disorder (ADHD): a review. J Child Neurol
Sanger TD, Chen D, Fehlings DL, Hallett M, Lang AE, Mink JW et al (2010) Definition and classification of hyperkinetic movements in childhood. Mov Disord 25:1538–1549
San-Juan D, Calcáneo Jde D, González-Aragón MF, Bermúdez Maldonado L, Avellán AM, Argumosa EV, Fregni F (2011) Transcranial direct current stimulation in adolescent and adult Rasmussen’s encephalitis. Epilepsy Behav 20:126–131. doi:10.1016/j.yebeh.2010.10.031
Schmitt A, Hasan A, Gruber O, Falkai P (2011) Schizophrenia as a disorder of disconnectivity. Eur Arch Psychiatry Clin Neurosci 261(Suppl 2):S150–S154
Schneider HD, Hopp JP (2011) The use of the Bilingual Aphasia Test for assessment and transcranial direct current stimulation to modulate language acquisition in minimally verbal children with autism. Clin Linguist Phon 25:640–654. doi:10.3109/02699206.2011.570852
Shelyakin AM, Preobrazhenskaya IG, Kassil’ MV, Bogdanov OV (2001) The effects of transcranial micropolarization on the severity of convulsive fits in children. Neurosci Behav Physiol 31:555–560
Soltaninejad Z, Nejati V, Ekhtiari H (2015) Effect of anodal and cathodal transcranial direct current stimulation on DLPFC on modulation of inhibitory control in ADHD. J Atten Disord
Sonuga-Barke EJ (2005) Causal models of attention-deficit/hyperactivity disorder: from common simple deficits to multiple developmental pathways. Biol Psychiatry 57:1231–1238. doi:10.1016/j.biopsych.2004.09.008
Stahl SM, Buckley PF (2007) Negative symptoms of schizophrenia: a problem that will not go away. Acta Psychiatr Scand 115:4–11
Stortelder F, Ploegmakers-Burg M (2010) Adolescence and the reorganization of infant development: a neuro-psychoanalytic model. J Am Acad Psychanal Dyn Psychiatry 38:503–531
Trottier G, Srivastava L, Walker CD (1999) Etiology of infantile autism: a review of recent advances in genetic and neurobiological research. J Psychiatry Neurosci 24:103–115
Varga ET, Terney D, Atkins MD, Nikanorova M, Jeppesen DS, Uldall P, Hjalgrim H, Beniczky S (2011) Transcranial direct current stimulation in refractory continuous spikes and waves during slow sleep: a controlled study. Epilepsy Res 97:142–145
Vicario CM, Nitsche MA (2013) Transcranial direct current stimulation: a remediation tool for the treatment of childhood congenital dyslexia? Front Hum Neurosci 7:139. doi:10.3389/fnhum.2013.00139
Yook SW, Park SH, Seo JH, Kim SJ, Ko MH (2012) Suppression of seizure by cathodal transcranial direct current stimulation in an epileptic patient—a case report. Ann Rehabil Med 35:579–582
Young SJ, Bertucco M, Sheehan-Stross R, Sanger TD (2013) Cathodal transcranial direct current stimulation in children with dystonia a pilot open-label trial. J Child Neurol 28:1238–1244. doi:10.1177/0883073812460092
Young SJ, Bertucco M, Sanger TD (2014) Cathodal transcranial direct current stimulation in children with dystonia: a sham-controlled study. J Child Neurol 29:232–239. doi:10.1177/0883073813492385
Acknowledgments
This work was supported by the German Center for Brain Stimulation (GCBS) research consortium (FKZ 01EE1403), funded by the Federal Ministry of Education and Research (BMBF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. P. has received speaker’s honorarium from Mag&More GmbH and support with equipment from neuroConn GmbH, Ilmenau, Germany, and Brainsway Inc., Jerusalem, Israel.
Rights and permissions
About this article
Cite this article
Palm, U., Segmiller, F.M., Epple, A.N. et al. Transcranial direct current stimulation in children and adolescents: a comprehensive review. J Neural Transm 123, 1219–1234 (2016). https://doi.org/10.1007/s00702-016-1572-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-016-1572-z