Abstract
In 2001, Dance for Parkinson’s disease (DfPD®) classes for persons with Parkinson’s disease and care partners were developed by Brooklyn Parkinson Group and Mark Morris Dance Group. A previous assessment suggested that individuals experience positive benefits from DfPD®. The current preliminary uncontrolled study investigated the effects of a dance intervention on several motor and quality of life aspects of PD following 16 sessions (8 weeks; 20 h) taught by professional dancers/teachers. A mixed methods design was used to determine the effects of the class. Assessment instruments administered at baseline and post-intervention included the Hoehn and Yahr, UPDRS (part III), Berg Balance Scale, Beck Depression Inventory, and PDQ-39 and individual interviews after the last class. Hoehn and Yahr scores ranged from 1 to 4. UPDRS III total scores and sub scores of gait and tremor improved following the intervention (P < 0.05). During interviews participants reported physical, emotional, and social benefits. Despite the diversity of baseline measures post-class interview results were consistently positive across the sample. Twelve of 14 subjects (mean age 66.2) with idiopathic PD completed the sessions. After 4 years, four participants regularly attended DfPD® classes. The low attrition rate and continued attendance suggest notable adherence to the DfPD® class. The importance of the results is both clinical and conceptual, highlighting the value of using both quantitative and qualitative data to evaluate the benefits of dance with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cardinal features of Parkinson’s disease (PD) are resting tremor, rigidity, and bradykinesia, all of which can negatively impact the fluidity and pacing of movement. Motor manifestations of PD may be compounded by non-motor symptoms, such as apathy and depression (Jones et al. 2009; Pontone et al. 2009), and often lead to isolation (McRae et al. 2009).
Recent reports have found positive effects on balance, locomotion, gait, and aspects of quality of life from several types of dance classes (Westheimer 2008; Earhart 2009; Hackney et al. 2007; Hackney and Earhart 2009a, b, c; Heiberger et al. 2011; Houston and McGill 2012). Execution of dance sequences requires motor planning and memory. Dance training employs strategic methods such as visual focus, rhythm, imagery, proprioceptive input, and imitation of discrete parts of dance sequences to gain superior control of posture, balance, and movement. Dance is an esthetic, communal activity and a form of exercise that develops muscle flexibility and strength. The potential for persons with PD to experience the joy of dance and possible physical and cognitive benefits led to the development in 2001 of Dance for Parkinson’s Disease® (DfPD®), a collaboration between Brooklyn Parkinson Group (BPG) and Mark Morris Dance Group (MMDG), an internationally known company based in Brooklyn, to provide dance classes for the Parkinson community and to train other teachers.
There is a limited but increasing number of studies on the effects of dance on people with PD (Hackney and Bennett 2014). Few of these have evaluated both standard measures and qualitative perspectives of patients on the effect that dance has on them. Here we explored both objective and subjective effects of dance with the same participants.
An initial evaluation of DfPD® in 2006 (Westheimer 2008) used the quality of life scale (QOLS) (Burckhardt and Anderson 2003). Dance participants (n = 15) reported improvement in feeling fit and vigorous, socializing, engaging in active recreation, and understanding of self. Five participants answered open-ended questions about the effect of the classes on the body, mental attitude, and quality of life. While results of the QOLS documented some improvements, responses to open-ended questions suggested the classes had a more intense impact and broader range of positive effects than found on the QOLS. Respondents described their experience as “graceful,” “symptom-free,” “courageous,” “focused,” “much happier,” “confident,” “optimistic,” “exhilarated,” and “fluid.” In an effort to further investigate the impact of DfPD®, we designed this exploratory study with participants serving as their own control in an 8-week series of DfPD® classes (16 sessions, 1.25 h twice a week for a total of 20 h). Participants volunteered for the study and had not danced as adults before. They were not members of the ongoing dance class. The study class was implemented over the summer break. The questions addressed were (1) are there changes in motor symptoms and/or QOL as assessed by standardized rating scales following the intervention? (2) What do qualitative interviews reveal about how DfPD® impacts QOL among persons with PD?
Methods
Participants
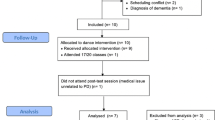
Fourteen participants with idiopathic PD [Hoehn and Yahr (HY) stages 1–4] were enrolled; all were first-time DfPD® dancers who volunteered for the summer session. In designing this pilot study no power analysis was conducted to determine the optimal sample size. Instead, the purpose of this study was to determine the effect size associated with the intervention that could be used in power analyses for subsequent evaluation studies. Of these, 12 (6 women and 6 men) completed the classes and all assessments. Attrition rate was low (14 %). Average attendance at each class was 10. Demographic information is presented in Table 1. Participants were recruited through neurologists and by referral from other patients. Inclusion criteria were as follows: age over 30; diagnosis of PD confirmed by a movement disorder specialist; mobility without or with assistance; ability to give informed consent; and medical clearance.
The study was approved by the Institutional Review Board of SUNY Downstate Medical Center and has, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their informed consent prior to their inclusion to the study.
Dance classes
Classes were held at Mark Morris Dance Center and led by the dance teachers who developed the DfPD® curriculum with BPG. Teachers’ qualifications included over a decade of experience observing and analyzing ways dance students initiate and execute movement and at least 6 years conducting specialized dance classes for persons with PD. The teaching method uses verbal instruction, imagery, attention to visual focus, repetition, rhythm, and imitation of movement, all with piano accompaniment.
The class started with 40 min seated warm up followed by 15 min standing at the barre, and 20 min moving across the floor. Participants were asked to carry out varied movements such as repeated stretching of the leg and pointing the foot (“tendu,” a basic ballet step), flexing the foot, moving feet and legs at angles side to side, arm extensions and curves in various directions (port de bras). Leg and arm movements were combined and varied. For instance, port de bras and tendu might be performed in opposition; or, dancing sharply (staccato) or smoothly (legato). This was done seated and at the barre where participants were taught to perform plié (bending the knees with feet in various positions). In addition, some modern, jazz, and tap moves were taught. Movement across the floor emphasized walking in a variety of ways including gliding, marching, waltz, and combinations of these. See link to video: http://www.brooklynparkinsongroup.org/classes/dance-for-pd.
Volunteer dance students or an instructor danced with persons with balance problems or difficulty standing. One participant used a walker while moving across the floor. A second ballet barre was available to hold for unstable participants. An assistant stayed with each of these persons. Participants were reminded to adapt or do part of difficult movements and if tired, to rest.
Measures
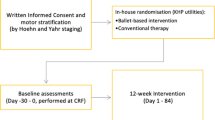
Quantitative data were collected at baseline and post-intervention and qualitative data were collected immediately after the last class. Physical assessments were performed before the first class, and immediately after the last class. Participants reported taking dopaminergic medication on the average 139 (SD = 109) min before the baseline assessment and 179 (SD = 121) min before the final assessment. Patients were not asked to change their medication timing; rather, the assessment timing was accommodating the patient’s routine medication schedule. Instruments included several standard PD measures: Hoehn and Yahr (HY; stage of disease) (Hoehn and Yahr 1967), Unified Parkinson’s Disease Rating Scale (UPDRS; Part III, motor scores) (Fahn and Elton 1987), and the Parkinson’s Disease Questionnaire [PDQ-39: a self-report measure of quality of life (QOL)] (Jenkinson et al. 1997), the Berg Balance Scale (BBS: a measure of performance on balance tasks of varying difficulty) (Qutubuddin et al. 2005), and the Beck Depression Inventory (BDI: a self-report measure of depression) (Beck et al. 1996). The interpretation of improvement is supported by statistical test and previous UPDRS motor score research. The clinically important difference (CID) on the UPDRS scaling was established with 2.3 points (minimal CID) and with 5.2 points for a moderate CID (Shulman et al. 2010). The HY, UPDRS, and BBS were administered by one of four physicians, all certified as UPDRS raters. Each participant was assessed while in his/her best ON medication state. One co-author experienced in qualitative research methods (CM) developed broad, structured, open-ended interview questions to learn about the experience of the class from the participants’ perspectives. Interviewers were provided with a scripted introduction and questions for this part of the study; interviews were conducted and audio-recorded by physician assessors after the last class.
Analyses
Paired-samples t tests were used to examine change over time on the outcome variables.
A correlational analysis was used to investigate a possible relationship between the change in total UPDRS III scores and time interval between last dose of medication and evaluation. Statistical significance level was set at P ≤ 0.05. The qualitative interviews were transcribed and analyzed through a process of coding and categorization (Lincoln and Guba 1985) for salient themes. Because of the broad range of physical functioning noted at baseline (e.g., HY 1–4), and to determine if there were differences in subjective responses to the class based on pre-intervention level of functioning, the patients were divided into two groups (“Better” and “Worse”) based on PDQ-39 single index (PDQ-39SI), or summary, scores at baseline (Jenkinson et al. 1997). Although no statistical analyses were performed (to avoid Type I error), average scores of all measures were calculated to examine possible differences in scale scores between participants in the “Better” and “Worse” groups.
Results
Motor symptoms
There was a significant change from baseline to post-intervention in total UPDRS III, an improvement of 10.4 % over baseline (Table 2). There was a remarkable significant change in the UPDRS III gait subscore (item 27), which improved by 26.7 %. There was improvement in the UPDRS rest tremor subscore (item 20), which improved 18.5 %, but the difference was not statistically significant. Effect sizes, which indicate the standardized size of differences, were small to medium for difference tests significant at P < 0.05 (Cohen 1988). There was no relationship between change in total UPDRS III scores and precise medication timing. There were no significant changes in the HY or BBS scores.
Quality of life
As shown in Table 2 there were no significant changes from baseline to post-intervention in PDQ-39SI or BDI scores. Pre- and post-intervention scores for the “Better” and “Worse” groups are presented in Table 3. The table shows that the UPDRS-III score in the “Better” group changed by 4.5 points and in the “Worse” group by 1.5 points. However, these changes did not reach statistical significance.
Qualitative interviews
Responses to five interview questions are shown for the six participants in each group (“Better” and “Worse”), in Tables 4 and 5, respectively. Through the process of coding and categorization used to analyze the transcripts, it was found that the answers participants gave in the interviews were very similar, despite the differences between the two groups in their scores on HY, UPDRS III, BBS, BDI, and PDQ-39 as shown in Table 3. Individuals in both the “Better” and “Worse” groups mentioned physical, social and emotional benefits of the class.
All participants said they would attend the class if it were ongoing. Four participants (33 %) continue to attend DfPD® classes regularly. The main reasons for dropping out were not dance related. The answers to how long positive effects of the class lasted ranged from 1 hour to 1 day. One person stated, “The glow lasts an hour or so. Self-confidence lasts until the next major freeze or fall (3–5 days).”
Discussion
Over the 20-h of dance classes, the total UPDRS III (motor) score improved by an average of three points (10.4 %) for the group. This result is statistically significant and represents improvement that demonstrates a “minimal” clinically important difference (CID, Shulman et al. 2010) that patients can recognize and value. This improvement is consistent with the change noted in other studies assessing the impact of dance in PD (Hackney and Earhart 2009b, c). Of the items within the UPDRS III, gait showed significant change while tremor showed a trend to improvement. Gait impairment is a major problem in PD. In addition to being a motor deficit it often leads to anxiety and social isolation. Our study shows the beneficial effect of dance on gait. Further studies on dance may directly address the effect of dance on anxiety.
There was no change in the Hoehn and Yahr staging over the short period of the study. The HY score broadly reflects level of disability and all three cardinal symptoms of PD as well as gait and balance. The HY was included as a descriptive instrument to document stage of disease for participants in the study. Thus, change in the HY score was not expected.
Considerable evidence has emerged of subtypes of motor impairment in PD, particularly for gait and tremor (Burn et al. 2012; Factor et al. 2011). Our results suggest an improvement in these areas and the potential utility of examining the sub-scores of the UPDRS III in a larger sample.
Our multisensory method consists of giving auditory, visual, and cognitive cues. There are reasons why the multisensory cueing method used in classes might contribute to improvement of gait. Studies show that an auditory cue of a steady rhythm or beat in music or from a metronome helps persons with PD walk in synchrony with the beat they hear. Visual cues, such as equidistant stripes to step over, and imagining long steps, increase stride (Morris et al. 2010; Nieuwboer et al. 2007). In dance class auditory rhythm from music is combined with instructive verbal imagery which serves as a cognitive cue (“March across the floor like the leader of a parade”) and with the visual cue of copying the dance leaders.
The potential importance of cognitive cues is suggested by recent studies which indicate cholinergic impairment in PD (Bohnen et al. 2013). In addition to well-known effects on cognition, cholinergic pathways may be responsible for aspects of gait dysfunction observed in PD (Bohnen et al. 2013; Chung et al. 2010). Possibly, the cognitive strategies used repeatedly in dance classes engage cholinergic pathways and stimulate more focus on movement tasks.
Falls related to postural instability are a significant source of morbidity and mortality in PD. Previous dance intervention studies have demonstrated modest, but significant improvements on the BBS (Earhart 2009; Hackney and Earhart 2010), which we did not find. One potential reason is that in the DfPD® study participants spend one-third of class time seated. Other dance interventions that have been studied (Tango and Foxtrot/Ballroom) are perhaps more intensive in their demands upon balance mechanisms than DfPD®. However, BBS is only modestly effective in predicting falls (Leddy et al. 2011; Neuls et al. 2011). Other balance measures, such as the BESTest and the miniBEST, may be more helpful in detecting changes in balance in individuals with PD (King et al. 2012; Leddy et al. 2011). A battery of balance measures has been suggested as a more comprehensive way of assessing interventions (Dibble et al. 2008; Neuls et al. 2011).
We found no effect of dance on the PDQ-39 scores, although four of 12 subjects showed improvement on questions 15, 34, and 39, which were related to cutting up food, difficulty with speech, and feeling unpleasantly hot or cold. We did not perform item-level analyses on the PDQ-39 as the sample size was too small, inviting the strong possibility of Type 1 error, or finding significant differences that were an artifact of performing too many analyses without statistical correction. Lack of improvement on overall PDQ-39 is in contrast to the results of some, but not all studies of dance and Parkinson’s (Hackney and Bennett 2014).
The outcomes of this study may have been influenced by the short period of observation and/or small sample size, which affects power. Alternatively, recent large-scale studies suggest that the PDQ-39 is insensitive to relatively short-term changes in PD symptoms or the need for symptomatic therapy (Parashos et al. 2014). Possibly, the PDQ-39 does not include a sufficient number of items that detect the kind of changes that persons in the DfPD® classes reported in the interviews (Tables 4, 5). The interview questions were open ended and asked about participants’ experiences and responses to the class and allowed for expression of a range of observations not covered in the PDQ-39.
Interview responses appear more positive than some of the quantitative results indicate. Responses in both “Better” and “Worse” groups (Tables 4, 5) were consistently positive and remarkably similar in spite of differences between the two groups in scores on the quantitative measures (Table 3). Thus, interview results suggest that the value of the class was not limited to physical functioning. The participants reported benefits related to QOL and well-being that were not reflected in changes on quantitative measures. It appears that some standard instruments (BBS, BDI, PDQ-39) used in this study did not capture the full benefits of dance from the participants’ perspectives.
Results similar to ours in suggesting the benefits of dance beyond physical assessment scores were also reported by the English National Ballet (Houston and McGill 2012). These results support the recommendation of the Office of Behavioral and Social Sciences Research at the National Institutes of Health, which described best practices for using mixed methods designs (inclusion of both quantitative and qualitative data) in the health sciences (Creswell et al. 2011).
Results of the study indicated consistent and high class attendance compared to other forms of exercise (Hackney and Earhart 2009b). The often observed problem of decreasing motivation over time in exercise programs seems not to have occurred here. As reported in the interviews, the supportive emotional and social experience along with physical activity appears to have kept attendance strong.
There are several limitations of this study. The small sample size presents challenges in terms of the risk of Type II errors (i.e., not finding statistically significant positive effects of the dance intervention that did occur). In addition, constraints on scheduling at the dance studio meant that the dance class could only be held for 2 months during the summer. This may have been too short a period of time for persons with PD to experience other measurable improvements in the physical domains that were assessed.
We recommend that a randomized controlled trial of DfPD® be conducted. A larger study might separate participants into tremor predominant vs. postural instability gait disorder forms of PD to determine whether there are differences in responsiveness of motor symptoms to the intervention. It is important to compare the effect of DfPD® classes and fitness classes. Because adherence appears to be very high in DfPD®, investigation of the contributors to this behavior is warranted.
Conclusions
This small study showed that some specific motor measures of PD improved over the short time of the dance classes. Standardized instruments of PDQ39, BDI, and BBS did not show significant changes, whereas responses to the qualitative questions developed by us indicated a variety of positive outcomes to the classes. The low attrition rate and continuing attendance of DfPD® classes demonstrate adherence and high motivation to participate in this activity. The growing interest in DfPD® classes and the current results demonstrate the need to better understand the specific effects of DfPD® with objective, standardized instruments, such as the UPDRS, and also with more attention to qualitative assessment that attempts to capture the individual experience of the effects of dance.
References
Beck AT, Steer RA, Brown GK (1996) Manual for the beck depression inventory-II. Psychological Corporation, San Antonio
Bohnen N, Frey KA, Studenski S, Kotagal V, Koeppe RA, Scott PJ, Albin RL, Muller ML (2013) Gait speed in Parkinson disease correlates with cholinergic degeneration. Neurol 81(18):1611–1616
Burckhardt CS, Anderson KL (2003) The quality of life scale (QOLS); reliability, validity and utilization. Health Qual Life Outcomes 1:60
Burn DJ, Landau S, Hindle JV, Samuel M, Wilson KC, Hurt CS, Brown RG (2012) PROMS-PD Study Group: Parkinson’s disease motor subtypes and mood. Mov Disord 27(3):379–386
Chung KA, Lobb BM, Nutt JG, Horak FB (2010) Effects of a central cholinesterase inhibitor on reducing falls in Parkinson disease. Neurol 75:1263–1269
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Psychology Press, New York
Creswell JW, Klassen AC, Plano Clark VL, Smith KC (2011) Best practices for mixed methods research in the health sciences. Office of Behavioral and Social Sciences Research (OBSSR) National Institutes of Health. http://obssr.od.nih.gov/mixed_methods_research
Dibble LE, Christensen J, Ballard DJ, Foreman KB (2008) Diagnosis of fall risk in Parkinson Disease: an analysis of individual and collective clinical balance test interpretation. Phys Ther 88(3):323–332
Earhart GM (2009) Dance as therapy for individuals with Parkinson disease. Eur J Phys Rehabil Med 45:231–238
Factor SA, Steenland NK, Higgins DS et al (2011) Postural instability/gait disturbance in Parkinson’s disease has distinct subtypes: an exploratory analysis. J Neurol Neurosurg Psychiatry 82(5):564–568
Fahn S, Elton RL(1987) The unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Goldstein M, Calne DB (eds) Recent developments in Parkinson’s disease, vol 2. Florham Park Macmillan Healthcare Information, pp 153–163, 293–304
Hackney MD, Bennett CG (2014) Dance therapy for individuals with Parkinson’s disease: improving quality of life. J Parkinsonism Restless Legs Syndrome 4:17–25
Hackney ME, Earhart GM (2009a) Health-related quality of life and alternative forms of exercise in Parkinson disease. Parkinsonism Relat Disord 15:644–648
Hackney ME, Earhart GM (2009b) Short duration, intensive tango dancing for Parkinson disease: an uncontrolled pilot study. Complement Ther Med 17:203–207
Hackney ME, Earhart GM (2009c) Effects of dance on movement control in Parkinson’s disease: a comparison of Argentine tango and American ballroom. J Rehabil Med 41:475–481
Hackney ME, Earhart GM (2010) Effects of dance on balance and gait in severe Parkinson disease: a case study. Disabil Rehabil 32(8):679–684
Hackney ME, Kantorovich S, Levin R, Earhart GM (2007) Effects of tango on functional mobility in Parkinson’s disease: a preliminary study. J Neurol Phys Ther 31:1–7
Heiberger L, Maurer C, Amtage F (2011) Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson’s disease. Front Aging Neurosci 3:1–15
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurol 17:427–442
Houston S, McGill A (2012) A mixed-methods study into ballet for people living with Parkinson’s. Arts Health 5:1–17
Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N (1997) The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Aging 26:353–357
Jones CA, Pohar SL, Patten SB (2009) Major depression and health-related quality of life in Parkinson’s disease. Gen Hosp Psychiatry 31:334–340
King LA, Priest KC, Salarian A, Pierce D, Horak FB (2012) Comparing the Mini-BEST with the Berg Balance Scale to evaluate balance disorders in Parkinson’s Disease. Parkinsons Dis 1–7
Leddy AL, Crowner BE, Earhart GM (2011) Functional gait assessment and balance evaluation system test: reliability, validity, sensitivity, and specificity for identifying individuals with Parkinson disease who fall. Phys Ther 91(1):102–113
Lincoln YS, Guba EG (1985) Naturalistic Inquiry. Sage, Newbury Park
McRae C, Fazio E, Hartsock G, Kelley L, Urbanski S, Russell D (2009) Predictors of loneliness in caregivers of persons with Parkinson’s disease. Parkinsonism Relat Disord 15:544–547
Morris ME, Martin CL, Schenkman ML (2010) Striding out with Parkinson disease: evidence-based physical therapy for gait disorders. Phys Ther 90(2):280–288
Neuls PD, Clark TL, Van Heuklon NC et al (2011) Usefulness of the Berg Balance Scale to predict falls in the elderly. J Geriatr Phys Ther 34(1):3–10
Nieuwboer A, Kwakkel G, Rochester L et al (2007) Cueing training in the home improves gait related mobility in Parkinson’s disease: the RESCUE trial. J Neurol Neurosurg Psychiatry 78:134–140
Parashos SA, Luo S, Biglan KM, Bodis-Wollner I, He B, Liang GS, Ross GW, Tilley BC, Shulman LM, For the NET-PD Investigators (2014) Measuring disease Progression in Early Parkinson Disease: the National Institutes of Health Exploratory Trials in Parkinson Disease (NET-PD) Experience. JAMA Neurol 71(6):710–716
Pontone GM, Williams JR, Anderson KE (2009) Prevalence of anxiety disorders and anxiety subtypes in patients with Parkinson’s disease. Mov Disord 24:1333–1338
Qutubuddin AA, Pegg PO, Cifu DX, Brown R, McNamee S, Carne W (2005) Validating the Berg Balance Scale for patients with Parkinson’s disease: a key to rehabilitation evaluation. Arch Phys Med and Rehabil 86:789–792
Shulman LM, Gruber-Baldini AL, Anderson KE, Fishman PS, Reich SG, Weiner WJ (2010) The clinically important difference on the Unified Parkinson’s Disease Rating Scale. Arch Neurol 67(1):64–70
Westheimer O (2008) Why dance for Parkinson’s disease. Top Geriatr Rehabil 24:127–140
Acknowledgments
The Mark Morris Dance Group: Nancy Umanoff, Eva Nichols, John Heginbotham, David Leventhal, Misty Owens; Accompanists: Bruce Lazarus and Colleen Jones; Neurological evaluators: Drs. Muhammad Javaid and Abishek Gulati; BPG: Ava Jarden; Advisors: Heiner Ellgring and Dan Russell; and most especially, the students who participated in the study class. This study was unfunded.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Westheimer, O., McRae, C., Henchcliffe, C. et al. Dance for PD: a preliminary investigation of effects on motor function and quality of life among persons with Parkinson’s disease (PD). J Neural Transm 122, 1263–1270 (2015). https://doi.org/10.1007/s00702-015-1380-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-015-1380-x