Abstract
Background
Basilar invagination (BI) is a common disease in the craniocervical junction (CVJ) area. Posterior fossa decompression with/without fixation is a controversial surgical strategy for BI type B. This study aimed to evaluate the efficacy of simple posterior fossa decompression in treating BI type B.
Methods
This study retrospectively enrolled BI type B patients who underwent simple posterior fossa decompression at Huashan Hospital, Fudan University between 2014.12 and 2021.12. Patient data and images were recorded pre- and postoperatively (at the last follow-up) to evaluate the surgical outcomes and craniocervical stability.
Results
A total of 18 BI type B patients (13 females), with a mean age of 44.2±7.9 years (range 37–62 years), were enrolled. The mean follow-up period was 47.7±20.6 months (range 10–81 months). All patients received simple posterior fossa decompression without any fixation. At the last follow-up, compared with preoperation, the JOA scores were significantly higher (14.2±1.5 vs. 9.9±2.0, p = 0.001); the CCA was improved (128.7±9.6° vs. 121.5±8.1° p = 0.001), and the DOCL was reduced (7.9±1.5 mm vs. 9.9±2.5 mm, p = 0.001). However, the follow-up and preoperative ADI, BAI, PR, and D/L ratio were similar. No patients had an unstable condition between the C1-2 facet joints that was observed in the follow-up CT and dynamic X-ray.
Conclusions
In BI type B patients, simple posterior fossa decompression could improve neurological function and will not induce CVJ instability in BI type B patients. Simple posterior fossa decompression could be a satisfactory surgical strategy for BI type B patients, but preoperative CVJ stability assessment is crucial.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Basilar invagination (BI) is a common ossification-malformation in the craniocervical junction (CVJ) area and is characterized by abnormal protrusion of the odontoid process to the foramen magnum, resulting in crowding in the foramen magnum and compression symptoms of the medulla oblongata, upper cervical spinal cord and posterior cranial nerves [28,29,30, 32, 38]. In recent years, a classification based on the stability of the CVJ was proposed [16, 23]: BI type A (type A BI, BI type I) is defined as an unstable basilar invagination that is combined with atlantoaxial dislocation or any other upper cervical spine instability factors; in contrast, BI type B (type B BI, BI type II) is regarded as a relatively stable basilar invagination without distinct upper cervical instability factors [9, 11, 17].
In clinical practice, for unstable BI type A treatment, the principles of reduction, decompression, fusion and fixation have been well recognized by neurosurgeons [40].
Among the surgical methods for BI type B, simple posterior decompression, such as posterior fossa decompression (PFD) or posterior fossa decompression with duraplasty (PFDD), is a common strategy since BI type B is relatively stable. Moreover, simple posterior decompression without any fixation has been demonstrated to be able to effectively relieve the compress of the oblongata and superior cervical medulla and achieve a satisfying prognosis with less surgical damage and more surgical safety [4, 10, 35]. However, recently, some neurosurgeons have argued that BI type B has potential instability. Therefore, simple posterior decompression is not enough, and CVJ fusion and fixation are the key steps in treating BI type B [20, 22].
As the surgical strategies have been widely debated, various kinds of surgeries for BI type B treatment have been performed. Therefore, we designed this study to evaluate the efficacy of simple posterior fossa decompression without any fixation in BI type B treatment. In this retrospective study, we detailed the clinical characteristics and surgical outcomes for 18 BI type B cases using simple posterior fossa decompression to add more information and evidence for BI type B treatment.
Methods and materials
Patient population and study design
A retrospective, observational study was performed. BI type B patients who were admitted to the Department of the Neurosurgery at Fudan University Huashan Hospital between Dec. 2014 and Dec. 2021 were included. This study was approved by the Ethical Review Boards of Fudan University Huashan Hospital. Informed consent was obtained from all individual participants. If a patient cannot sign informed consents by himself, informed consents would be signed by his statutory guardians. The article is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. All patients were evaluated and treated by full-time neurosurgeons with specific fellow training, and all surgeries were performed by two attending neurosurgeons.
Inclusion criteria included the following: (a) age from 18 to 65 years; (b) diagnosis of BI type B; (c) underwent simple posterior fossa decompression to treat BI.
Exclusion criteria included the following: (a) any instability factors evaluated by classical CVJ stability judgement (such as ADI, BAI, BDI) pre-opeartion; (b) underwent CVJ area or craniocerebral surgery previously; (c) combined other CVJ abnormities (such as CVJ tumors, CVJ trauma); (d) reject to participate the study.
Diagnosing criteria of BI type B
(a) The odontoid process above the Chamberlain line more than 5mm in sagittal computed tomography (CT) scan; (b) the atlantodental interval (ADI) was within the normal range, no more than 3mm in sagittal computed tomography (CT) scan and without any instable factors confirmed by dynamic X-ray or CT.
Radiological evaluation
CT scans of CVJ area (0.6 mm each slice) with the head in neutral were obtained pre- and post-operatively (at last follow-up) from each BI type B patient on a 256-slice multi-detector CT scanner (Siemens, Germany) to evaluate the stability of CVJ area. The high-resolution T2-weighted magnetic resonance images of CVJ area were also obtained on a 3.0T GEMR750 MRI scanner with an eight-channel phased-array head coil (Siemens, Germany) to evaluate the level of magnum foramen compression induced by BI and the volume of intramedullary syringemyelia. Dynamic X-ray was also performed to evaluate CVJ instability.
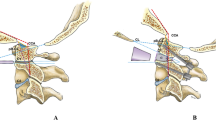
To evaluate the basilar invagination and CVJ stability (atlantoaxial and atlanto-occipital stability) pre- and post-operatively (at last follow-up), the clivus-canal angle (CCA) (Fig. 1a), the distance of the odontoid apex to Chamberlain’s line (DOCL) (Fig. 1b), the atlantodental interval (ADI) (Fig. 1c), the basion-dens interval (BDI) (Fig. 1e), the basion-axial interval (BAI) (Fig. 1f), the Powers ratio (PR) (Fig. 1g), and the atlanto-occipital angle (O-C1 angle) (Fig. 1i) on sagittal median CT were measured. In addition, the atlanto-occipital joint depth/length ratio (D/L ratio) (Fig. 1h) on paramedian sagittal CT and the position of C1-2 facets joints (Fig. 1d) in coronal CT were also evaluated (Table 1) [2, 3, 7, 12, 15, 24, 25, 27, 39, 41].
Diagrams of CVJ area measurement on mid-sagittal, paramedial-sagittal, and coronal images. a The line extending from the surface of the clivus (CO), the line extending from the inferodorsal portion of the C2 body (DO), and the angle (COD) was the clivus-canal angle (CCA). b Chamberlain’s line (CL), odontoid apex (D), the distance from point D to the line CL was the distance from the odontoid apex to Chamberlain’s line (DOCL). c Posterior edge of the atlas anterior arch (A), anterior edge of the odontoid (D), and the length of segment AD was the atlantodental interval (ADI). d The blue dotted line indicates the relationship between the position of two atlantoaxial lateral mass articular facets, which were used to evaluate the stability of the atlantoaxial. e Basion (B), odontoid apex (D), the length of BD was the basion-dens interval (BDI). f Basion (B), the posterior axial line (AD), the distance from the basion (B) to the posterior axial line (AD) was the basion-axis interval (BAI). g Basion (B), opisthion (O), the midpoint of the inner table of the posterior atlas arch (A), and the midpoint of the inner table of the posterior atlas arch (P). The ratio of BP to AO was the powers ratio (PR). h The depth of the atlanto-occipital joint (AB), the length of the atlanto-occipital joint (CD), and the ratio of CD to AB were calculated as the atlanto-occipital joint depth/length ratio (D/L ratio). i Basion (B), opisthion (O), the midpoint of the inner table of the posterior atlas arch (A), and the midpoint of the inner table of the posterior atlas arch (P). The angle (O-C1) formed by the extension line along AP and the extension line along BO was the atlanto-occipital angle (O-C1 angle)
Neurological function evaluation
The Japanese Orthopaedic Association (JOA, version 1975) Score [14, 42] was used to evaluate neurological function of each patient enrolled pre- and post-operatively (at last follow-up), performed by at least two qualified independent investigators in a blinded manner.
Surgical strategies
PFD (posterior fossa decompression) or PFDD (posterior fossa decompression with duraplasty) as a simple posterior fossa decompression procedure was performed in previous studies [1, 5]. For PFD, through the posterior midline approach, a bone-window suboccipital craniectomy (diameter, 3–4 cm) was performed, the posterior arch of the atlas (1.5–2 cm) was resected, and the ligaments, soft tissues and other structures attached to the dura were also removed to achieve complete decompression of the magnum foramen. For PFDD, a dural incision was subsequently performed, and the attached arachnoid membrane, especially around the medial and lateral apertures of the fourth ventricle, was thoroughly released. Then, the dura mater was grafted with the autologous graft. The wound was closed in layers.
Statistical analysis
Continuous variables were expressed as means ± standard deviation (SD) or medians (interquartile range) and categorical variables as percentages. The univariate analyses of categorical data were performed using the chi-squared test. Equality of variance was assessed using Levene’s test. Normally distributed variables were compared using Student’s t-tests or one-way ANOVA, whereas non-normally distributed variables were compared using the Kruskal-Wallis or Mann–Whitney U-tests. All statistical tests were two-tailed and p values < 0.05 were considered statistically significant. Statistical analysis was carried out using IBM SPSS Statistics (version 26, IBM, U.SA.).
Results
Patient characteristics
A total of 18 patients with BI type B (13 females) with a mean age of 44.2±7.9 years (range 37-62 years) were included. The mean follow-up period was 47.7±20.6 months (range 10-81 months). All patients received simple posterior fossa decompression without any fixation (Fig. 2) (Table 2).
All patients presented with one or more neurological symptoms. Eleven (61.1%) patients presented with muscle weakness, 15 (83.3%) with limb numbness, 5 (27.8%) with ataxia, 13 (72.2%) with neck pain and mobility restriction and 4 (22.2%) with dysphagia or dyspnoea. Moreover, 8 (44.4%) patients had atlantooccipital fusion, 4 (22.2%) had C2-3 fusion, and 13 (72.2%) had syringomyelia (Table 3).
Decompression of the posterior fossa was favourable in BI type B patients
To assess the decompression efficiency, the CCA and DOCL obtained from CT scans were used. Compared with preoperation, the CCA at the last follow-up significantly increased (128.7±9.6° vs. 121.5±8.1°, p < 0.001); however, the DOCL at the last follow-up was reduced (7.9±1.5 mm vs. 9.9±2.5 mm, p < 0.001).
In addition, compression of the ventral dural sac was decreased in 17 of the BI type B patients (17/18, 94.4%), and the volume of syringomyelia was reduced in 12 patients (12/13, 92.3%) (Fig. 3) (Table 4). Only one patient who had suffered progressed syringomyelia also showed continuous compression to the ventral medulla, indicating that sufficient decompression was favourable in BI type B patients.
Image of decompression effects on a mid-sagittal position at last follow-up. a Mid-sagittal image of T2 MR showed syringomyelia and the compression level of the ventral dural sac of the medulla oblongata with abnormal CCA and DOCL in type B BI postoperatively. b Mid-sagittal T2 MR image showing syringomyelia and the compression level of the ventral dural sac of the medulla oblongata with improved CCA and DOCL in Type B BI at follow-up
Simple posterior fossa decompression was associated with neurological functional improvements in BI type B patients
At the last follow-up, the postoperative JOA scores of all patients were significantly higher than the preoperative scores (p < 0.001) (Table 4). Ten patients (out of 11, 90.9%) showed improvement in muscle strength, with three of them recovering fully. Limb numbness was alleviated in 14 patients (out of 15, 93.3%), with four of them recovering fully. Four out of five patients (80%) recovered from ataxia, whereas 11 out of 12 patients (91.7%) experienced improvement in neck pain and mobility restriction, with four of them recovering fully. All patients who suffered from dysphagia and dyspnoea recovered (Table 5).
Our study showed that in most BI type B patients, simple posterior fossa decompression was associated with improvement in neurological functions, with 94.4% (17/18) of the participants achieving distinct improvement in their neurological symptoms. However, one patient (patient #4) did not show significant neurofunction improvement after simple posterior fossa decompression, which we presumed was due to insufficient decompression. These results suggest that satisfactory decompression by simple posterior decompression may be associated with neurological outcome improvements in BI type B patients.
Simple posterior fossa decompression was not associated with CVJ instability in BI type B patients
In general, CVJ stability includes bilateral atlantoaxial and atlanto-occipital stability. For atlantoaxial stability evaluation, no differences in the ADI were found pre- and postoperation (1.5±0.3 mm vs. 1.6±0.4 mm, p = 0.178). Additionally, the ADI of each BI type B patient, whether measured pre- or postoperatively (at last follow-up), was within the normal range (Fig. 4a, b). Moreover, in dynamic X-ray, normal physiological relationships of the C1-2 facet joint positions were observed in all patients at the last follow-up (Table 6).
Images of CVJ stability in mid-sagittal and horizontal positions at the last follow-up. a Horizontal CT scan showing type B BI with normal ADI postoperatively. b Horizontal CT scan confirmed normal postoperative ADI without any deterioration at the last follow-up. c Mid-sagittal CT scan showing confirmed normal postoperative BDI and BAI without any deterioration at the last follow-up. d Paramedial-sagittal T2 MR image showing the condition of the atlanto-occipital joint with a normal depth/length ratio postoperatively. e Paramedial-sagittal T2 MR image showing the natural position of the atlanto-occipital joint facets with a normal depth/length ratio at the last follow-up
In addition, BDI, BAI, PR, D/L ratio, and O-C1 angle were used to assess atlanto-occipital stability. Our results showed that no differences in BAI, PR or D/L ratio were observed pre- and postoperation (6.2±2.2 vs. 5.9±2.3 mm, p = 0.064; 0.70±0.08 vs. 0.73±0.05 p = 0.063; 0.27±0.06 vs. 0.24±0.05, p = 0.055, respectively). Moreover, the BAI, PR and D/L ratio, either measured pre- or postoperatively (at the last follow-up), were within the normal range. Similarly, although the BDI and O-C1 angle had statistically significant differences pre- and postoperation (p = 0.036; p = 0.001), the pre- and postoperative BDI and O-C1 angle in all patients were within the normal range (6.9±1.9 vs. 6.5±2.1 mm; 5.0±1.3° vs. 3.6±1.7°). According to previous literature, a BDI > 12 mm or an O-C1 angle far from the neutral position (5.06 ±0.48°) was considered atlanto-occipital dislocation [33]. Therefore, our data indicated that no distinct CVJ instability was observed after simple fossa decompression (Fig. 4c, d, e) (Table 7).
In summary, no progressive CVJ instability was detected after simple posterior fossa decompression in any of the included BI patients.
Discussion
In this study, we found that simple posterior fossa decompression could effectively decrease the compression of the ventral medulla oblongata and improve neurological function in BI type B patients. Moreover, simple posterior fossa decompression will not induce CVJ instability in BI type B patients.
Posterior fossa decompression may improve neurological outcomes in BI type B patients
“Decompression” is the classical surgical procedure for BI and has been performed since 1968 [4]. Posterior fossa decompression could achieve satisfactory outcomes in some BI cases [6, 10, 31]. However, in BI patients with complicated conditions of CVJ stability, especially in BI type B patients, the choice of surgical strategy is controversial. Some scholars believe that due to the potential instability in BI type B, fusion and fixation are able to improve outcomes in these patients [18, 20, 22, 43]. However, fusion and fixation procedures do not seem to be a “wonderful” procedure without risks. For instance, fusion and fixation might injure the C1-2 nerve root, spinal cord, and vertebral artery and limit the range of movements of the cervical spine. Moreover, fusion and fixation were considered to be associated with a longer duration of surgery, higher cost, more blood loss, and implant risks [36, 37]. Our study found that PFD/PFDD could improve neurological outcomes in BI type B patients, indicating that simple posterior fossa decompression may be sufficient for BI type B patients whose preoperative CVJ stability is favourable. We suggest that not all BI type B patients require fusion and fixation and that the choice of fusion and fixation procedure for BI type B patients should be carefully considered.
Posterior fossa decompression and CVJ stability: preoperative stability assessment is crucial
To date, surgery has remained the most effective treatment for BI [38, 40]; however, it was previously reported that preoperative CVJ instability may cause neurological function deterioration after simple decompression [40]. This indicates that detailed assessments of CVJ stability should be carried out preoperatively.
Unlike BI type A, which is characterized by CVJ instability [13, 34, 38], it may not be necessary for BI type B patients to receive fixation and fusion. As previously mentioned, CVJ instability may worsen neurological outcomes in BI patients; thus, it was reasonable to assess the stability of CVJ preoperatively. We proposed that the therapeutic strategy of BI type B patients should be designed according to CVJ stability.
Additionally, our study aims to determine whether simple posterior decompression without fusion and fixation would affect the CVJ stability of BI type B patients at the last follow-up. In our study, atlantoaxial stability was assessed by the ADI and C1-2 facet positions, while the BDI, BAI, PR, O-C1 angle and atlanto-occipital D/L ratio were used to evaluate atlanto-occipital stability. Based on these indicators both pre- and postoperation, no CVJ instability was found in our patients’ pre/post-simple posterior fossa decompression. Moreover, almost all follow-up patients achieved a certain degree of neurological improvement, indicating that simple fossa decompression may not harm CVJ stability in BI type B patients. However, we stress that if CVJ instability is identified preoperatively, other strategies, including fusion and fixation, may be needed.
Most favorable strategies to assess CVJ stability are unclear
For the evaluation of CVJ stability, the presence of atlantoaxial dislocation is a crucial factor. ADI and C1-2 facet position were the classical indices used to assess atlantoaxial stability. However, Goel et al. defined a new classification for atlantoaxial dislocation [18] and suggested that potential atlantoaxial instability existed in BI type B patients [19, 21, 43]; thus, “fusion and fixation” was necessary in treating these patients [18, 20, 22]. However, to date, clinical evidence of “chronic instability,” as described by Goel, is rare [40].
On the other hand, atlanto-occipital instability is also vital to CVJ stability. Lu et al. evaluated CVJ stability by measuring clivus length, clivo-canal angle (CCA), basion-dens interval (BDI), basion-axial interval (BAI), and other indicators in kinematic CT scans. Based on these indicators, they suggested that occipitocervical fusion, combined with foramen magnum decompression, was beneficial to BI type B patients [43]. However, in Lu et al.’s study, the index values, especially the classical atlanto-occipital stability indices (BDI, BAI), were mostly within the normal range. This may indicate that there was no obvious CVJ instability [25, 33]. Moreover, the relationship between joint range of motion and joint instability is not clear. Recently, Lu et al. provided a new classification of the atlanto-occipital joint (AOJ) by measuring the curvature of the AOJ, indicating that most Chiari malformation with BI type B may be classified as type III AOJ. Type III AOJ was considered to be atlanto-occipital instability [26].
In our study, similar to the above indices, we also focused on the atlanto-occipital joint depth/length (D/L ratio, similar to the curvature of the AOJ). However, as previously mentioned, we found no difference in the D/L ratio between pre- and postoperative BI type B patients. This may indicate that no significant AOJ stability depravation was observed in BI type B patients after simple fossa decompression.
To date, the diagnostic criteria of atlantoaxial and atlanto-occipital instability remain controversial [8, 12, 17, 23, 25, 33, 43]. Recently, more studies have paid more attention to the CVJ stability evaluation methods [8, 25, 39, 40], but more clinical evidence is required to verify these methods.
Limitations
There were several drawbacks in the current study. First, the sample size was relatively small. Second, in our future study, we will select dynamic CT scans, which are considered to be more sensitive and accurate for CVJ instability diagnosis than dynamic X-rays [43], to assess the CVJ stability of our patients. Therefore, caution should be exercised in interpreting our conclusions, and a prospective multicentre study is justified to further elucidate the potential mechanism of this phenotype.
Conclusion
In this study, we found that simple posterior fossa decompression could effectively decrease compression on the ventral medulla oblongata and improve neurological function in BI type B patients. Furthermore, simple posterior fossa decompression will not induce CVJ instability in BI type B patients. Therefore, simple posterior fossa decompression could be a satisfactory surgical strategy for BI type B patients, but preoperative CVJ stability assessment is crucial.
Abbreviations
- ADI:
-
atlantodental interval
- AOJ:
-
atlanto-occipital joint
- BAI:
-
basion-axis interval
- BDI:
-
basion-dens interval
- BI:
-
basilar invagination
- CCA:
-
the clivus-canal angle
- CVJ:
-
craniocervical junction
- D/L ratio:
-
the atlanto-occipital joint depth/length ratio
- DOCL:
-
the distance of the odontoid apex to Chamberlain’s line
- O-C1 angle:
-
atlanto-occipital angle
- PFD:
-
posterior fossa decompression
- PFDD:
-
posterior fossa decompression with duraplasty
- PR:
-
Powers ratio
- SD:
-
standard deviation
References
Aslan A, Rakip U, Boyacı MG, Yildizhan S, Kormaz S, Atay E, Coban N (2021) Posterior fossa decompression and superficial durotomy rather than complete durotomy and duraplasty in the management of chiari 1. Neurol Res 43(6):440–446
Batista UC, Joaquim AF, Fernandes YB, Mathias RN, Ghizoni E, Tedeschi H (2015) Computed tomography evaluation of the normal craniocervical junction craniometry in 100 asymptomatic patients. Neurosurg Focus 38(4):E5
Batista UC, Joaquim AF, Fernandes YB, Mathias RN, Ghizoni E, Tedeschi H (2015) Computed tomography evaluation of the normal craniocervical junction craniometry in 100 asymptomatic patients. Neurosurg Focus 38(4):E5
Caetano de Barros M, Farias W, Ataíde L, Lins S (1968) Basilar impression and Arnold-Chiari malformation. A study of 66 cases. J Neurol Neurosurg Psychiatry 31(6):596–605
Caffo M, Cardali SM, Caruso G, Fazzari E, Abbritti RV, Barresi V, Germanò A (2019) Minimally invasive posterior fossa decompression with duraplasty in Chiari malformation type I with and without syringomyelia. Surg Neurol Int 10:88
Chai Z, Xue X, Fan H, Sun L, Cai H, Ma Y, Ma C, Zhou R (2018) Efficacy of Posterior Fossa Decompression with Duraplasty for Patients with Chiari Malformation Type I: A Systematic Review and Meta-Analysis. World Neurosurg 113:357–365.e1
Chamberlain WE (1939) Basilar Impression (platybasia): a bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med 11(5):487–496
Chandra PS, Goyal N, Chauhan A, Ansari A, Sharma BS, Garg A (2014) The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Neurosurgery 10(Suppl 4):621–629 discussion 629-630
de O JNP B, BAD S, Nascimento IF, Martins LA, Tavares CB (2019) Basilar invagination associated with Chiari malformation type I: a literature review. Clin Sao Paulo Braz 74:e653
de Oliveira SU, de Oliveira MF, Heringer LC, Barcelos ACES, Botelho RV (2018) The effect of posterior fossa decompression in adult Chiari malformation and basilar invagination: a systematic review and meta-analysis. Neurosurg Rev 41(1):311–321
de Oliveira Filho ÍT, Romero PC, Fontoura EAF, Botelho RV (2019) Chiari malformation and types of basilar invagination with/without syringomyelia. Surg Neurol Int 10:206
Deininger-Czermak E, Villefort C, von Knebel DN et al (2021) Comparison of MR ultrashort echo time and optimized 3D-Multiecho in-phase sequence to computed tomography for assessment of the osseous craniocervical junction. J Magn Reson Imaging JMRI 53(4):1029–1039
Feng S-P, Wang H-W, Qiao G-Y, Yu X-G (2022) Indirect ventral brainstem decompression by posterior C1-C2 distraction and fixation for basilar invagination. World Neurosurg 163:e98–e105
Furlan JC, Catharine Craven B (2016) Psychometric analysis and critical appraisal of the original, revised, and modified versions of the Japanese Orthopaedic Association score in the assessment of patients with cervical spondylotic myelopathy. Neurosurg Focus 40(6):E6
Gire JD, Roberto RF, Bobinski M, Klineberg EO, Durbin-Johnson B (2013) The utility and accuracy of computed tomography in the diagnosis of occipitocervical dissociation. Spine J Off J North Am Spine Soc 13(5):510–519
Goel A (2004) Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 1(3):281–286
Goel A (2009) Basilar invagination, Chiari malformation, syringomyelia: a review. Neurol India 57(3):235–246
Goel A (2014) Goel’s classification of atlantoaxial “facetal” dislocation. J Craniovertebral Junction Spine 5(1):3–8
Goel A (2015) Is atlantoaxial instability the cause of Chiari malformation? Outcome analysis of 65 patients treated by atlantoaxial fixation. J Neurosurg Spine 22(2):116–127
Goel A (2018) Cervical Fusion as a Protective Response to Craniovertebral Junction Instability: A Novel Concept. Neurospine 15(4):323–328
Goel A (2018) Basilar invagination, syringomyelia and Chiari formation and their relationship with atlantoaxial instability. Neurol India 66(4):940–942
Goel A (2019) A Review of a new clinical entity of “central atlantoaxial instability”: expanding horizons of craniovertebral junction surgery. Neurospine 16(2):186–194
Goel A, Sathe P, Shah A (2017) Atlantoaxial Fixation for basilar invagination without obvious atlantoaxial instability (group B Basilar invagination): Outcome Analysis of 63 Surgically Treated Cases. World Neurosurg 99:164–170
Goel A, Jadhav D, Shah A, Rai S, Dandpat S, Vutha R, Dhar A, Prasad A (2020) Chiari 1 formation redefined-clinical and radiographic observations in 388 surgically treated patients. World Neurosurg 141:e921–e934
Kaneko S, Ishii K, Watanabe K, Tsuji T, Nakamura M, Matsumoto M, Yato Y, Asazuma T (2018) Exploration for reliable radiographic assessment method for hinge-like hypermobility at atlanto-occipital joint. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 27(6):1303–1308
Huang Q, Yang X, Zheng D, Zhou Q, Li H, Peng L, Ye J, Qi S, Lu Y (2022) Exploring the pathogenesis of atlanto-occipital instability in Chiari Malformation with type ii basilar invagination: a systematic morphological study. Neurosurgery. https://doi.org/10.1227/neu.0000000000002284
Ma L, Guo L, Li X, Qin J, He W, Xiao X, Lu L, Xu Y, Wu Y (2019) Clivopalate angle: a new diagnostic method for basilar invagination at magnetic resonance imaging. Eur Radiol 29(7):3450–3457
McGREGER M (1948) The significance of certain measurements of the skull in the diagnosis of basilar impression. Br J Radiol 21(244):171–181
Menezes AH (2008) Craniocervical developmental anatomy and its implications. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 24(10):1109–1122
Menezes AH, VanGilder JC, Graf CJ, McDonnell DE (1980) Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg 53(4):444–455
Osborne-Grinter M, Arora M, Kaliaperumal C, Gallo P (2021) Posterior FOSSA decompression and duraplasty with and without arachnoid preservation for the treatment of adult Chiari Malformation type 1: a systematic review and meta-analysis. World Neurosurg 151:e579–e598
Ray BS (1942) Platybasia with involvement of the central nervous system. Ann Surg 116(2):231–250
Rojas CA, Bertozzi JC, Martinez CR, Whitlow J (2007) Reassessment of the craniocervical junction: normal values on CT. AJNR Am J Neuroradiol 28(9):1819–1823
Sai Kiran NA, Vidyasagar K, Sivaraju L, Raj V, Aryan S, Thakar S, Mohan D, Hegde AS (2021) Outcome of Surgery for congenital craniovertebral junction anomalies with atlantoaxial dislocation/basilar invagination: a retrospective study of 94 patients. World Neurosurg 146:e313–e322
Salunke P, Sura S, Futane S, Aggarwal A, Khandelwal NK, Chhabra R, Mukherjee KK, Gupta SK (2012) Ventral compression in adult patients with Chiari 1 malformation sans basilar invagination: cause and management. Acta Neurochir (Wien) 154(1):147–152
Salunke P, Karthigeyan M, Futane S (2018) Pros and cons of C2 nerve sectioning/preservation in posterior fusion for congenital atlantoaxial dislocation. World Neurosurg 118:e925–e932
Salunke P, Karthigeyan M, Malik P, Panchal C (2020) Changing perception but unaltered reality: how effective is C1-C2 Fixation for chiari malformations without instability? World Neurosurg 136:e234–e244
Smith JS, Shaffrey CI, Abel MF, Menezes AH (2010) Basilar invagination. Neurosurgery 66(3 Suppl):39–47
Wan M, Zong R, Tong H-Y, Zhang Z-Z, Zhao B, Yu X-G (2020) A morphometric study of the atlanto-occipital joint in adult patients with Chiari malformation type I. Br J Neurosurg:1–4
Wagner A, Grassner L, Kögl N, Hartmann S, Thomé C, Wostrack M, Meyer B (2020) Chiari malformation type I and basilar invagination originating from atlantoaxial instability: a literature review and critical analysis. Acta Neurochir (Wien) 162(7):1553–1563
Yin Q, Wang J (2015) Current Trends in management of atlantoaxial dislocation. Orthop Surg 7(3):189–199
Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K (2001) Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine 26(17):1890–1894 discussion 1895
Zhou Q, Song C, Huang Q et al (2022) Evaluating Craniovertebral stability in chiari malformation coexisting with type II Basilar invagination: an observational study based on kinematic computed tomography and its clinical application. World Neurosurg S1878-8750(22):00675–00671
Funding
This study was funded by CAMS Innovation Fund for Medical Sciences (CIFMS, 2019-12M-5-0008), National Key R&D Program of China (2018AAA0100300 and 2018AAA0100302, R.X.), and National Natural Science Foundation of China (NSFC) (81870909, 82071315 and 82271342, R.X.).
Author information
Authors and Affiliations
Contributions
The study was designed by Xing-Yu Chen. Data collection was performed by Wei Chen, Jian-Lan Zhao, Hao-Ru Dong, Long-Nian Zhou, Xiao Xiao and Gong Chen. Data analysis was performed by Xing-Yu Chen, Wei Chen, Jian-Lan Zhao, Hao-Ru Dong, Long-Nian Zhou, Xiao Xiao, Gong Chen. The first draft of the manuscript was written by Xing-Yu Chen. Xiao-Ming Che and Rong Xie supervised the study and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Ethical Review Boards of Fudan University Huashan Hospital. The article is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. All patients were evaluated and treated by full-time neurosurgeons with specific fellow training, and all surgeries were performed by two attending neurosurgeons.
Informed consent
Informed consent was obtained from all individual participants included in the study. If a patient cannot sign informed consents by himself, informed consents would be signed by his statutory guardians.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, XY., Chen, W., Zhao, JL. et al. Surgical outcomes of basilar invagination type B without atlantoaxial dislocation through simple posterior fossa decompression: a retrospective study of 18 cases. Acta Neurochir 165, 3051–3063 (2023). https://doi.org/10.1007/s00701-023-05625-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05625-3