Abstract
Background
As a pioneer center in the field of stereotaxy, Sainte-Anne school has always advocated the use of intraoperative imaging for stereotactic procedures to optimize both safety and accuracy. With the advent of intraoperative mobile CT unit, the robot-assisted stereotactic biopsy procedure has been recently updated.
Method
Herein, we aim at describing our new surgical procedure that combines robotic assistance (NeuroMate, Renishaw) and intraoperative cone beam CT imaging (O-Arm, Medtronic).
Conclusion
Intraoperative imaging with the O-Arm was efficiently incorporated into the workflow. This new equipment leads to optimizing operative time and an easier realization of intraoperative imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Relevant surgical anatomy
The present surgical technique, i.e., the combined use of robot and intraoperative mobile cone-beam CT, does not rely on specific anatomy. Basic rules to well approach and avoid anatomical structures during stereotactic surgery should be followed:
-
The head should be placed in neutral position to ease the image co-registration processes and the recognition of a mechanical deviation.
-
The mechanical accuracy of the skull drilling is higher if positioned perpendicular to the cranial vault.
-
The stereotactic biopsy trajectory has to be carefully planned, by avoiding blood vessels, cerebral sulci, and sparing eloquent brain cortical/subcortical areas and cerebral ventricles as much as possible.
-
The stereotactic biopsy entry point should avoid exposed zones of the scalp, i.e., the forehead, whenever feasible.
Description of the technique
Figure 1 illustrates the planning process, Fig. 2 the procedure workflow, and Fig. 3 presents the positions of the O-Arm and the robot in the operating room.
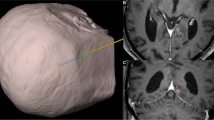
The stereotactic planning process with iPlan Stereotaxy planning software (version 3.0, BrainLAB AG, Feldkirchen, Germany). A After importing the preoperative MRI into iPlan, the AC/PC line is defined to allow the preoperative MRI to be navigated in a reproducible plan. B The preoperative stereotactic MRI (tridimensional T1-weighted sequence with and without contrast agent including midface, acquired the eve of surgery) is co-registered with the previous oncological MRI, including fluid-attenuated inversion recovery sequence, tridimensional T1-weighted sequence with and without contrast agent, and perfusion sequence. C-D The different components of the lesion are segmented automatically using the iPlan automated segmentation tool. E A safe stereotactic trajectory is planned and carefully checked using the Probe’s eye view reconstruction of iPlan in the different MR series. F The DICOM coordinates are extracted, and an additional verification of the safety of the trajectory is performed using our homemade MATLAB app Through The Brain
Presentation of the current surgical procedure of robot-assisted stereotactic biopsy. A General overview of the operating room with the mobile CT unit O-Arm and the robot NeuroMate. B Close-up on the Talairach stereotactic head clamp made up of the base of the Talairach frame secured to the robot NeuroMate. C The different steps of the procedure with (C1) a first 3D series acquisition of the Neurolocate tool locked on the robot arm and moved close to the patient’s head; (C2) a control of the proper robot’s positioning with a second 3D acquisition with a metallic punch simulating the trajectory; (C3) the robot arm is positioned close to the patient’s skin to minimize the mechanical deviation; (C4) fine adjustments of the drill with a mechanical stop with accurate measurement of the depth of drilling; (C5) fine adjustment of the monopolar coagulation 10 mm below the dura mater plane with accurate measurement of the depth of coagulation; (C6) intraoperative control of the biopsy cannula position after insertion to the biopsy target using a third O-Arm acquisition; and (C7) the puncture wound is closed with absorbable suture (minimal shaving)
Stereotactic biopsy is performed under general anesthesia along one single trajectory. Serial biopsy samples are made to specimen and all the components of the lesion. The neurosurgeon uses the iPlan Stereotaxy planning software (version 3.0, BrainLAB AG, Feldkirchen, Germany) to define the optimal biopsy trajectory [4]. The head of the patient is placed in a Talairach head clamp (Dixi, Besançon, France) fixed to the 5 degrees of freedom passive NeuroMate robot (Renishaw, New Mills, UK). Tridimensional acquisitions of the head with O-Arm (Medtronic, Minneapolis, Minnesota) are performed intraoperatively. The O-Arm is a cone beam CT designed for intraoperative imaging. The frameless positioning of the robot into the operating room space is made with the Neurolocate (Renishaw) tool. The five ruby spheres of the Neurolocate tool must be positioned as close to the patient’s head as possible. A 3D series is then acquired with the O-Arm. This imaging series allows to co-register preoperative MRI with intraoperative acquisition via a dedicated module of neuroinspire software (Renishaw). This planning software was specifically developed for NeuroMate robot: the automated recognition of the five ruby spheres on the 3D series allows the robot to place itself in the operating space with excellent accuracy (below 0.1 mm in most cases). The automated co-registration of preoperative MRI and intraoperative 3D series is then performed using neuroinspire software. Subsequently, the robot can navigate within the preoperative imaging space. Trajectory coordinates planned previously are transferred on the neuroinspire planning software thanks to the DICOM coordinates. Following the safety check—the agreement between a test trajectory and the actual robot’s arm movement—the robot’s arm is moved until the tool holder approaches the skin at 1 mm. This point is of utmost practical importance as it reduces the mechanical inaccuracy of the drill bit’s trajectory to its minimum. A metallic punch is placed into the tool holder to depict the direction of the planned trajectory. The entry point and the biopsy trajectory are then verified using a second O-Arm 3D acquisition. If required, fine adjustments of the robot’s final arm position are done. The drill hole is performed with a 2.5-mm diameter drill bit: the drilling movement must be as smooth as possible and the bit as sharp as possible (single-use disposable drill favored). The 10-mm window side-cutting Sedan-Vallicioni biopsy cannula is then inserted, and its movements are controlled by the robot. The accurate positioning at each biopsy site is ensured before sampling via O-Arm acquisition.
The Talairach head clamp is still in use in Sainte Anne Hospital, but the NeuroMate robot can be used with other head fixation systems such as the Leksell frame G [2].
Indications
The present technique—MRI-based and robot-assisted stereotactic procedure with intraoperative CT imaging—may be applied for any stereotactic procedures [5]. Although the initial indications were the procedures requiring great accuracy such as deep brain stimulation and stereoelectroencephalography, the same method should also apply for stereotactic biopsies [1]. Indeed, these are frequent procedures, and their requirement in terms of accuracy should by no means be overlooked. This surgical method seems particularly well-suited for deep-seated or brainstem lesions. The general anesthesia ensures a better comfort for both the patient and the neurosurgeon and enables better control of the blood pressure. The mechanical accuracy of the robot is the highest possible, lowering the risk of trajectory deviation and their related complications [6].
Limitations
Limitations include the price of the devices, the need of available and trained neurosurgical staff, and the prolonged duration of the surgical procedure. Considering the substantial cost of the robot and the mobile cone beam CT unit, it is possible to rationalize their use such as the CT in daily practice for spine surgery and the robot for neuro-endoscopic procedures, for instance. The duration of the surgery remains longer compared to non-stereotactic biopsies, such as MRI-based neuronavigation-assisted biopsies. However, it should be considered that this encompasses the time required to obtain a better accuracy to improve both efficacy and safety. Furthermore, if the procedure were to carry legal ramifications, it would undoubtedly be highly valuable for the surgeon to show where and how the procedure was performed.
How to avoid complications
The anesthetic management is important: anticoagulant and/or antiplatelet therapy should be stopped before surgery and blood pressure must be strictly controlled during the whole procedure.
The head should be firmly secured: Talairach head clamp is non-deformable. The proper drilling of the cranial vault constitutes a delicate step: the applied force should not be excessive, and the angle is preferentially perpendicular to reduce the risk of deviation.
Intraoperative imaging should be performed: it allows to be aware of and correct an eventual mechanical deviation. Moreover, it enables to demonstrate the actual site of sampling for postoperative analyses.
To lower the risk of inconclusive biopsy, we recommend to obtain at least four samples, from the four quadrants. The specimens should be as representative as possible of the different components of imaging abnormalities. The number of biopsy samples was not found to be associated with increased morbidity in our experience [7].
We have recently shown that postoperative hemorrhagic complications mainly arose from planning “errors” [6]. The imaging quality should be sufficient to properly identify blood vessels and sulci that must be avoided along the trajectory: MRI enhancement should always be checked. The stereotactic trajectory is better analyzed in the axis direction: the Probe’s eye view reconstruction is useful in that respect. The biopsy trajectory must be checked from the pia matter to the deepest part of the target since intratumoral vessels should be avoided as well [6]. If possible, the trajectory planning should be performed on the day prior to the surgery and reviewed by at least one other neurosurgeon to reduce planning errors.
Specific perioperative considerations
Preoperative stereotactic MRI (tridimensional T1-weighted sequence with and without contrast agent including midface, acquired on the day before surgery) is co-registered with preoperative oncological MRI including fluid-attenuated inversion recovery (FLAIR) sequence and perfusion sequence. The combined MRI is used for biopsy trajectory planning and sample selection.
Postoperative CT scan is systematically obtained on postoperative day 1 or immediately in the event of postoperative alteration of the clinical status of the patient.
Specific information to give to the patient about surgery and potential risks
The specific information to be delivered to the patient concerns the risks of surgery: 1.3% of inconclusive biopsy and 4.0% of > 20-mm postoperative cerebral hemorrhage, in our experience [7]. Another important point to discuss is the time required to obtain an integrated histomolecular diagnosis according to the current WHO classification updates [3].
References
Daumas-Duport C, Szikla G, Vedrenne C (1979) [Stereotactic serial cerebral biopsies. Methodology (author’s transl)]. Arch Anat Cytol Pathol 27(3):135–139
Kajita Y, Nakatsubo D, Kataoka H, Nagai T, Nakura T, Wakabayashi T (2015) Installation of a NeuroMate robot for stereotactic surgery: efforts to conform to japanese specifications and an approach for clinical use—technical notes. Neurol Med Chir Tokyo 907–914
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol (Berl) 131(6):803–820
Pallud J, Varlet P, Devaux B, Geha S, Badoual M, Deroulers C, Page P, Dezamis E, Daumas-Duport C, Roux F-X (2010) Diffuse low-grade oligodendrogliomas extend beyond MRI-defined abnormalities. Neurology 74(21):1724–1731
Talairach J, Bancaud J, Bonis A, Tournoux P, Szikla G, Morel P (1961) Functional stereotaxic investigations in epilepsy. Methodological remarks concerning a case. Rev Neurol (Paris) 105:119–130
Zanello M, Roux A, Debacker C et al (2021) Postoperative intracerebral haematomas following stereotactic biopsies: poor planning or poor execution? Int J Med Robot Comput Assist Surg MRCAS 17(2):e2211
Zanello M, Roux A, Senova S et al (2021) Robot-assisted stereotactic biopsies in 377 consecutive adult patients with supratentorial diffuse gliomas: diagnostic yield, safety, and postoperative outcomes. World Neurosurg 148:e301–e313
Funding
This study was funded by the Nuovo-Soldati Foundation for Cancer Research scholarship, the Servier Foundation scholarship, and the Fundapro Foundation scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patient consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
10 key points summary
1. Inform the patient about the time required to obtain definitive histomolecular diagnosis.
2. The planning of the stereotactic trajectory is a key step and requires time and attention (the planification is therefore best performed the day prior to surgery and ideally by two neurosurgeons).
3. Robotic assistance has many advantages over frame-based procedures including high mechanical accuracy, and it is less prone to human error (no reading and manual settings of the target coordinates).
4. Intraoperative imaging ensures the highest possible accuracy for a biopsy trajectory and makes it possible to know precisely the sites where the samples are taken for postoperative analyses.
5. General anesthesia precludes any high blood pressure episode.
6. The head should be firmly fixed using a head clamp.
7. Robot tool holder should be approached very close and ideally come in contact with the skin surface when drilling to avoid the potential bending of the drill bit and minimize mechanical inaccuracy.
8. Drilling of the skull should be smooth and slow, followed by coagulation of the dura, and measurement of the biopsy cannula based on the imagery.
9. The biopsy cannula is to be inserted with closed side cutting windows and subsequently opened once in the biopsy site, to perform a minimum of 10-s-long suction in order to obtain biopsy samples of a substantial size.
10. Several biopsy samples from different imaging components of the targeted lesion are to be obtained (the number of biopsy samples is not associated with increased morbidity).
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Tumors
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 80038 kb)
Rights and permissions
About this article
Cite this article
Zanello, M., Simboli, G.A., Carron, R. et al. MRI-based and robot-assisted stereotactic biopsy with intraoperative CT imaging. Acta Neurochir 164, 3311–3315 (2022). https://doi.org/10.1007/s00701-022-05271-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05271-1