Abstract
Background
The subtonsillar transcerebellomedullary approach (STA) has been well established as one of the surgical options to access lesions in the foramen of Luschka. The middle cerebellar peduncle has been defined as the superior limit of this corridor, and tumors extending beyond this landmark were often approached through combined accesses.
Method
We illustrate the access to the suprasellar cistern, from a purely STA for a large tumor arising from the foramen of Luschka.
Conclusion
This manuscript demonstrates the STA as a valid alternative for certain tumors of the foramen of Luschka, which extend into crural and suprasellar cisterns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Relevant surgical anatomy
The cerebellomedullary fissure represents the natural separation between the cerebellar tonsils and the medulla, extending laterally to the cerebellopontine cisterns [5, 10] The fissure is defined dorsally by the cerebellar tonsil and ventrally by inferior aspect of the roof of the 4th ventricle [4]. Between the tonsil and the roof of the ventricle, the posteroinferior cerebellar artery should be identified, specifically the telovelotonsillar segment, before the bifurcation between vermian and hemispheric branches [9]. The middle cerebellar peduncle constitutes the superior wall of the cerebellomedullary junction [10]. Large tumors arising from the foramen of Luschka and extending superiorly displace the middle cerebellar peduncle dorsally and laterally. Following the tumor, we surpass the natural limit of cerebellomedullary fissure gaining access to the cerebellopontine cistern laterally and the prepontine cistern medially [2]. In the cerebellopontine cistern, we identify the nerves from the V to the VIII. The facial and vestibularcochlear nerves arise in the inferior part of the cerebellopontine cistern just above the pontomedullary membrane [2]. The abducens arises at the level of the pontomedullary sulcus heading superiorly towards Dorello’s canal. Finally, the trigeminal nerve arises from the midpons and runs through the superolateral portion of the cistern [2]. In these cisterns, we should also identify the superior cerebellar artery (SCA) and the anterior inferior cerebellar artery (AICA) [2, 8].
If we continue the dissection superiorly, we will identify the oculomotor nerve on its origin in the interpeduncular cistern [6]. The dorsal limit of this subtonsillar approach should be the posterior aspect of the cerebral peduncle, anterior to the limitans mesencephalic sulcus. It can be challenging to identify the trochlear nerve in the ambient cistern through this view unless we seek it in the oculomotor trigone before it hides in the petroclinoid fold [1].
Description of the technique
The patient is intubated under general anesthesia with remifentanil and continuous infusion of propofol for continuous intra-operative monitoring, including motor evoked potentials (MEPs), somatosensory evoked potentials (SSEPs), electromyogram (EMG) for facial nerve, cranial nerve XI, and brainstem auditory evoked responses (BAERs). The patient is placed in a three-fourth prone position, with the head flexed using a Mayfield headframe, and turned to the contralateral side of the tumor. Surgical incision is performed, extending from the inion to the spinous process of C2. Cervical musculature is detached in midline and mobilized laterally through a subperiosteal dissection to expose the occipital bone from the external occipital protuberance to the asterion and down to the foramen magnum. The vertebral artery is dissected dorsally on the arch of C1, and the occipital condyle is identified, but not drilled. Suboccipital and retrosigmoid craniotomy exposing the ipsilateral transverse and sigmoid sinus and down to the foramen magnum is performed. There is no need to drill the mastoid. Wide C1 laminectomy is also performed, removing the posterior arch of C1 bilaterally and up to the lateral mass on the tumor side. A “Y” shaped durotomy is performed to expose the cerebellum and opened caudally to expose the medulla and upper cervical spinal cord (Fig. 1). Using an operative microscope, a dissection of the posterolateral fissure begins between the uvula and the cerebellar tonsil, along the division of the posteroinferior cerebellar artery, and continues with the dissection to the tonsillo-medullary fissure. These dissections provided access to the telovelar junction on the ipsilateral side. Following the tela laterally gains access to the lateral recess of the foramen of Luschka, extending the exposure to access the 4th ventricle.
Illustration of the subtonsillar transcerebellomedullary approach. On the left representation of the exposure with the craniotomy and C1 laminectomy. On the right operating view of the tumor after the dissection of the tonsillomedullary junction and posterolateral fissure and elevation of the tonsil
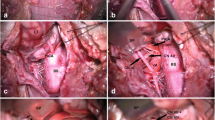
The middle cerebellar peduncle is usually displaced posteriorly and laterally, so with careful tumor resection, access to the prepontine, crural, and suprasellar cisterns is obtained. The 3rd cranial nerve is usually identified during dissection as is noted in the video, in addition to the arachnoid membranes within the suprasellar cistern, representing the superior limit of the resection. A retrosigmoid and cervical posterolateral approach can also be added under the same positioning to reach the tumor component in the ambient cistern, posterior to the lateral mesencephalic sulcus, and ventral to cervical spinal cord. Once resection is complete, a duraplasty graft is sewn in and the bone flap replaced using titanium plates and screws. A multi-layer closure is completed in a standard fashion (Figs. 2 and 3, Video 1).
a and b Sagittal T1 pre- and post-gadolinium MR image that shows a large retroclival mass extending from the suprasellar cistern (superior white arrow) down to the ventral cervical space at the level of C2-C3 (inferior white arrow), c–f axial preoperative T2-weighted MR image (FLAIR) sequence showing also the encasement of the vertebral artery, basilar artery, AICA, PICA, and presumably the cranial nerves 3–12
Indications and limitations
Large tumors extending from the foramen of Luschka into the ventricle and superior and anteriorly to the suprasellar and crural cisterns often require a complicated combined approach to adequately access all tumor margins. A combination of far lateral or middle cranial fossa approach for the superior portion and a midline suboccipital approach for the 4th ventricular component has been used historically to approach these difficult tumors.
While a purely lateral approach is a reasonable option for these tumors, especially for large tumors that displace the brainstem, they typically require extensive bony drilling of the occipital condyle, petrous bone, or both. This extensive drilling, especially of the occipital condyle, carries additional morbidity with a risk of craniocervical instability and vascular injury and adds significant time to the surgery [7]. A retrosigmoid approach is also a reasonable option for tumors with lateral extension; however, it does not offer adequate exposure to the suprasellar, 4th ventricle, or superior spinal components of these tumors. Staging the tumor resection by combining multiple different approaches is also a reasonable option and is generally our chosen approach for large, deep, fibrous tumors, such as teratomas.
While there are many reasonable options for surgical access, the strength of the subtonsillar approach is that entire lesion is accessed in one procedure, without the need for multiple approaches with different incisions and craniotomies. The subtonsillar approach allows for an extensive lateral and suprasellar exposure, while still retaining access to the 4th ventricle via the posterolateral fissure [4]. This dissection provides access to the junction of the tela choroidea and the inferior medullary vellum on the ipsilateral side [3].
The main limitation is the view that this approach provides to medial extension of tumors in front of the brainstem. For tumors that cross the plane of the basilar artery, lateral or bilateral approaches may provide a superior view of this region.
How to avoid complications
As with any surgical procedure, perfect knowledge of the relevant anatomy and exquisite care of the local structures help to assure a good surgical outcome. In cases where the tumor is encasing the neurovascular structures, identifying reliable and consistent anatomic landmarks is essential. With this approach, the interface between tumor and brainstem is easily found at the beginning of the case, allowing for early identification of a potentially hazardous step in dissection. Following the anatomy of the cerebellomedullary fissure allows the surgeon to quickly access the lateral recess of the 4th ventricle and foramen of Luschka, allowing for quick identification of the cranial nerves and PICA to avoid injury.
Information for the patient
Cranial nerve injury is the main concern with any surgery approaching the foramen of Luschka. The size and extent of the tumor determine the cranial nerves involved, but the possibility of lower cranial nerve dysfunction postoperatively should be discussed with the patient and family. Some degree of dysphonia or dysphagia is to be expected after surgery and could require the need for temporary feeding tube and possibly gastrostomy or tracheostomy. In our experience, the need of tracheostomy postoperatively has occurred only in patients with recurrent tumors, especially if they have received radiation.
In addition to lower cranial nerve dysfunction, the risks should be also individualized based on the tumor extension and the structures involved. Thus, in case where the tumor encases all the cranial nerves from III to XII additional deficits, such as hearing loss, dizziness, facial palsy, and facial numbness, double vision or ptosis may be also a concern and therefore should be explained to the patient and the family.
References
Al R (2000) Tentorial incisura. Neurosurgery 47(3 Suppl):S131–S153. https://doi.org/10.1097/00006123-200009001-00015
Al R (2000) The posterior fossa cisterns. Neurosurgery 47(3 Suppl):S287–S297. https://doi.org/10.1097/00006123-200009001-00029
Herlan S, Ebner FH, Nitz A, Hirt B, Tatagiba M, Roser F (2014) The midline suboccipital subtonsillar approach to the cerebellomedullary cistern and its structures: anatomical considerations, surgical technique and clinical application. Clin Neurol Neurosurg 125:98–105. https://doi.org/10.1016/j.clineuro.2014.07.029
Herlan S, Roser F, Ebner FH, Tatagiba M (2017) How i do it-neurosurgical anatomy The midline suboccipital subtonsillar approach to the cerebellomedullary cistern: how I do it. Emirates Acta Neurochir 159:1613–1617. https://doi.org/10.1007/s00701-017-3270-5
Jean WC, Abdel Aziz KM, Keller JT et al (2003) Subtonsillar approach to the foramen of Luschka: an anatomic and clinical study. Neurosurgery 52(4):860–866. https://doi.org/10.1227/01.NEU.0000053146.83780.74
Matsushima K, Yagmurlu K, Kohno M, Rhoton AL (2016) Anatomy and approaches along the cerebellar-brainstem fissures. J Neurosurg 124(1):248–263. https://doi.org/10.3171/2015.2.JNS142707
Menezes AH (2008) Surgical approaches: postoperative care and complications “posterolateral-far lateral transcondylar approach to the ventral foramen magnum and upper cervical spinal canal.” Child’s Nerv Syst 24(10):1203–1207. https://doi.org/10.1007/s00381-008-0597-5
Rhoton AL (2002) The cerebrum. Neurosurgery 51(4 SUPPL.):1–51. https://doi.org/10.1097/00006123-200210001-00002
Ucerler H, Saylam CY, Cagli S, Orhan M, Zileli M (2008) The posterior inferior cerebellar artery and its branches in relation to the cerebellomedullary fissure. Clin Anat 21(2):119–126. https://doi.org/10.1002/ca.20581
Ziyal IM, Sekhar LN, Salas E (1999) Subtonsillar-transcerebellomedullary approach to lesions involving the fourth ventricle, the cerebellomedullary fissure and the lateral brainstem. Br J Neurosurg 13(3):276–284. https://doi.org/10.1080/02688699943682
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study did not require IRB approval by the Ethics Committee.
Informed consent
The parents of the patient did provide informed consent for the procedure and for the publication of the manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. The subtonsillar approach represents an alternative for certain large tumors of the foramen of Luschka that extend supratentorially into crural and suprasellar cistern.
2. Lateral extension into the ambient cistern may require supracerebellar approach.
3. In large tumors extending from the foramen of Luschka superiorly, the middle cerebellar peduncle is usually displaced posteriorly and laterally.
4. This corridor allows access to certain tumors in a single stage, instead of more involved combined lateral and medial or staged approaches.
5. Finding the interface between tumor and brainstem and subsequently the origin of lower cranial nerves is key to decreasing the risk of cranial nerve injury.
6. Taking advantage of the corridor created by the tumor avoids any significant retraction of the tonsil to access the suprasellar cistern.
7. PICA should be identified in the cleft between the tonsil and the roof of the 4th ventricle and the AICA in the cerebellopontine cistern, anterior, and superior to the cerebellomedullary fissure.
8. A limitation of this approach is for tumors that extend in front of the brainstem, especially those that cross the basilar artery to the contralateral side.
9. Transient lower cranial nerve dysfunction can be expected postoperatively and should be discussed with the patient.
10. Electrophysiological monitoring of the cranial nerves is key to reducing the risk of injury.
This article is part of the Topical Collection on Tumor—Other
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 287032 KB) Video 1 2D surgical video of the subtonsillar transcerebellomedullary approach
Rights and permissions
About this article
Cite this article
McClugage, S.G., Weiner, H.L. & Aldave, G. Maximizing the subtonsillar transcerebellomedullary approach to suprasellar cistern: how I do it. Acta Neurochir 164, 751–755 (2022). https://doi.org/10.1007/s00701-021-05033-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-05033-5