Abstract
Objective
To investigate the effect of pre- and postoperative magnetic resonance imaging (MRI) findings on the prognosis of patients with spinal dural arteriovenous fistulas (SDAVFs) treated surgically.
Method
A total of 76 patients from Jan 1, 2013, to June 30, 2020, were enrolled in this study. Their spinal neurological function was evaluated and graded by the modified Aminoff-Logue Scale (mALS). Preoperative and 3 months postoperative MRI results were evaluated, and their relationship with patients’ pre- and postoperative spinal neurological function at 1 year after surgery was calculated. Analysis of variance (ANOVA), the chi-square test, and others were used to investigate the prognostic value of MRI for patients with SDAVFs treated surgically.
Results
According to our results, the extent of spinal edema on preoperative MRI was significantly correlated with the patients’ degrees of preoperative spinal neurological dysfunction. The severity of preoperative spinal neurological dysfunction was significantly greater in patients whose extent of spinal edema was identified at ≥ 5 vertebral levels. Importantly, patients with a reduction in the degree of spinal edema ≥ 50% on 3-month postoperative MRI demonstrated significant improvement in spinal neurological function 1 year after surgery.
Conclusion
In patients with SDAVFs, the extent of spinal edema on preoperative MRI may predict the severity of preoperative spinal neurological dysfunction. There was a significant correlation between the degree of reduction in spinal edema at 3 months after operation and patients’ clinical outcomes 1 year after surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal dural arteriovenous fistula (SDAVF) is a rare lesion, and patients consistently present with myelopathy caused by chronic venous hypertension [6] [9]. Surgery has been demonstrated to be a reliable method for obliterating the abnormal connection between the feeding artery and draining vein [8] [14]. Spinal edema and dilation of the draining vein have been reported to be important pathophysiological changes in SDAVF and present as intramedullary high signal and flow voids on magnetic resonance imaging (MRI) [6] [5]. However, whether the extent of intramedullary high signal or flow voids on preoperative MRI are correlated with patient prognosis is not fully understood [12]. Although previous studies have reported that the severity of SDAVF may be predicted by the extent of flow voids and spinal edema [4] [10], their credibility was still limited by their scale and inconsistent with other studies [7] [3]. In addition, studies on postoperative MRI and its impact on patient prognosis are rare [13] [16]. Thus, it is worth investigating the changes in postoperative MRI and its impact on the prognosis of patients’ spinal neurological function.
Based on previous studies and our clinical experience [7] [15], the extent of spinal edema or flow voids on preoperative MRI may reflect the severity of preoperative dysfunction, and a good reduction in spinal edema or flow voids may be associated with a satisfactory functional outcome.
In the present study, we used a retrospective approach to uncover the prognostic value of pre- and postoperative MRI in patients with SDAVFs after surgical treatment. We hope our results can provide a good result that is close to that experienced in the clinic.
Method
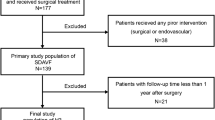
Subjects
A retrospective study was performed involving all patients diagnosed with SDAVFs who were treated surgically from Jan 1, 2013, to June 30, 2020, in our institution. Basic data such as sex, age, fistula location, and modified Aminoff-Logue Scale (mALS) score were extracted from the medical records. Participants had to meet the following inclusion criteria:
-
1)
Fistula identified by spinal digital subtraction angiography (DSA)
-
2)
Available preoperative and postoperative MRI of the spine
-
3)
Follow-up for at least 1 year after surgery
The exclusion criteria were as follows:
-
1)
Any prior intervention (surgical or endovascular)
-
2)
Neurological deficits caused by other lesion(s)
Evaluation of clinical results
Neurological function was evaluated by the mALS and graded according to the total score as follows: mild disability (0–3), moderate disability (4–7), and severe disability (8–11). Surgical results were evaluated by the mALS and identified as follows: (1) improvement, decrease in the mALS score by at least 1 point; and (2) no improvement, no change or increase in the mALS score. The mALS score was evaluated by three senior individual neurosurgeons, and the average of their scores was taken as the final outcome. Postoperative neurological function evaluation was performed through clinical visit or telephone questionnaire.
Imaging evaluation
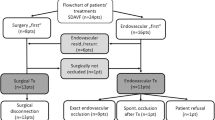
Preoperative MRI refers to MRI performed within 5 days before surgery, and postoperative MRI refers to MRI obtained between 90 and 120 days after surgery. (Fig. 1) The extent of intramedullary edema and flow voids on preoperative MRI were calculated and represented as the number of vertebral levels spanned. The degree of reduction in spinal edema or flow voids was calculated as (1-\(\frac{\mathrm{po}L}{\mathrm{pr}L}\)) * 100% (poL, extent of spinal edema or flow voids on postoperative MRI; prL, extent of spinal edema or flow voids on preoperative MRI). MRI results were evaluated by three individual senior neuroradiologists, and three individual senior neurosurgeons who were blinded to the changes/improvement for each participant retrospectively reviewed the randomized MRI findings, and the final results were calculated as the average of their results.
Statistical analysis
Continuous variables with a normal distribution were analyzed by analysis of variance (ANOVA). The Wilcoxon rank-sum test and Kruskal–Wallis test were used for data with a nonnormal distribution. The chi-square test was used to analyze the relationship between the degree of reduction in spinal edema or flow voids and the patient’s clinical outcome. Data are presented as the mean ± standard deviation (SD). The abovementioned data were analyzed by statistical software (SPSS, version 24, IBM Corp, ARMONK, NY), and p < 0.05 was considered statistically significant. This study was approved by the ethics committee of the West China Hospital.
Results
Baseline data
Finally, a total of 76 patients with 76 fistulas met our inclusion criteria, and the baseline characteristics are summarized in Table 1.
Among these fistulas, 8 (10.5%) were located at T1–T6, 42 (55.3%) were located at T7–T12, and 26 (34.2%) were located below T12. According to the preoperative mALS score, 25 (32.9%) patients were classified with mild disability, 33 (43.4%) patients with moderate disability, and 18 (23.7%) patients with severe disability.
Clinical results
The mean interval between surgery and latest follow-up was 13.8 ± 0.7 months (range from 12.3 to 15.2 months). Fifty-four (71.06%) patients experienced improvement, and 22 (28.94%) patients felt worse or stable after surgery. Regarding motor function, 48 (63.16%) patients experienced improvement, and 20 (26.32%) patients experienced stabilization 1 year after surgery. For micturition, 39 (51.31%) patients experienced improvement, and 28 (36.84%) patients experienced stabilization. Similarly, when comparing defecation status 1 year after surgery with preoperative results, 37 (48.68%) and 29 (38.16%) patients experienced improvement and stabilization, respectively. In addition, when comparing the mALS scores before and 1 year after surgery, significant differences were identified in the gait (G), micturition (M), defecation (D), and total (T) scores (Table 2).
Imaging results
The extent of spinal edema and flow voids spanned from 2 to 7 and 3 to 12 vertebrae on preoperative MRI, respectively. The results revealed that the extent of spinal edema was significantly different for different grades of preoperative neurological dysfunction (Fig. 2), and the more severe the patients’ neurological dysfunction was, the more significant the extent of the spinal edema. However, we did not find any correlation between the extent of flow voids and the grade of preoperative neurological dysfunction (p = 0.62, Kruskal–Wallis test).
Importantly, if the patients’ extent of spinal edema was identified at ≥ 5 vertebral levels, their degree of preoperative neurological dysfunction tended to be more severe (Table 3). However, we did not find such a threshold when we investigated the correlation between flow voids and preoperative neurological dysfunction.
Patients enrolled in this study all underwent postoperative MRI from 99 to 120 days after surgery (mean days 104.5 ± 6.6 days). The extent of spinal edema spanned from 0 to 5 vertebral levels, and the length of the flow voids spanned from 0 to 2 vertebral levels. According to our evaluation of the postoperative MRI results, none revealed extents of spinal edema or flow voids larger than their preoperative counterparts. In addition, significant differences were also identified when comparing the pre- and postoperative extents of these two characteristics on MRI (Table 4).
Regarding the relationship between the degree of reduction in imaging abnormities and clinical outcome, the results showed that patients were more likely to experience improvement in neurological function 1 year after surgery if their degree of reduction in spinal edema 3 months after surgery was ≥ 50% (Table 5). Regretfully, we did not find any relationship between the degree of reduction in flow voids and clinical outcome.
Discussion
The objective of this study was to explore the impact of pre- and postoperative MRI results on the prognosis of patients with SDAVF who were treated surgically. According to our results, the extent and degree of reduction in spinal edema were correlated with the prognosis of patient spinal neurological function.
In our series, the degree of patient preoperative neurological dysfunction was found to be correlated with the extent of spinal edema. It seems that if patients had more severe preoperative dysfunction, their extents of spinal edema also tended to be more substantial. In accordance with our experience, the larger the extent of spinal edema was, the more obvious the patient’s clinical presentation. Therefore, if the extent of spinal edema exceeds a certain degree, the severity of patients’ preoperative neurological dysfunction may be more significant.
Yen et al. reported that the correlation between the severity of disease and spinal edema was greater when the cutoff for the extent of spinal edema was set to 6 vertebral levels [19], while other scholars had previously set the threshold to 10 vertebral levels [4]. However, our results revealed that the threshold may be set to 5 vertebral levels. Although the threshold is different from that in the previous study, which may have been caused by differences in the study scales and follow-up periods, both of these results confirm the correlation between the extent of spinal edema and patient preoperative status. However, we did not find that the degree of preoperative spinal neurological dysfunction was correlated with the extent of flow voids. Flow voids on MRI represent venous congestion of the medulla and may be affected by variability in vascular structures in different segments [1] [2] [17]. Considering the different distributions of fistulas and follow-up periods in the different studies [4] [15] [19], the relationship between the extent of flow voids and neurological status may need further exploration in a larger and prospective study.
To our knowledge, this is the first study to demonstrate the relationship between the prognosis of patients with SDAVFs treated surgically and the degree of reduction in spinal edema. In previous studies, some scholars used the change in the number of levels spanned by spinal edema or flow voids to depict patients’ imaging responses to treatment [7] [16]. However, according to our experience and the above statistical results, patients with a smaller extent of spinal edema always have better postoperative neurological function outcomes and relatively less significant changes in spinal edema if assessed in vertebral levels. On the other hand, in patients with a longer extent of spinal edema, the number of vertebral levels corresponding to spinal edema might change relatively more significantly, but a less satisfying clinical outcome might occur. Thus, to individually reflect patients’ responses to surgery, we used “degree of reduction” as the index to evaluate the postoperative MRI results. In addition, given that neurological recovery often requires a longer period of time, we used patients’ mALS scores 1 year after surgery as the clinical outcome.
According to our results, if the patients’ extents of spinal edema were reduced by at least 50%, their clinical outcomes were better than those with a lower degree of reduction. Although imaging abnormalities can last for several months [7], a significant imaging reduction at an early stage at least represents a good response to surgery, and patients are more likely to experience improvement in their neurological function [18]. Despite the negative results Kaufmann et al. reported [7], we still agree with their view that a good clinical outcome is associated with a good reduction in postoperative MRI abnormalities. For the first time, our statistical results confirm the above view.
Compared with spinal edema, the degree of reduction in flow voids seems unrelated to patient clinical outcome. However, the diminishment of flow voids and intramedullary high signal are of crucial importance in evaluating whether residual disease or recurrence are present after surgery, especially for those with unsatisfactory clinical outcomes. In our department, if the patient’s clinical outcome and imaging results both point to recurrence or residual disease, we will recommend that the patient undergo another spinal digital subtraction angiography. In our series, there were 2 patients without significant imaging reduction, and their neurological function did not show improvement until 6 months after surgery. Considering that they were over 70 years old and refused another invasive examination, they did not receive another spinal DSA 3 months after surgery.
In addition, imaging reduction mainly represents structural recovery after surgery. As long as the abnormal connection are shown to have been obliterated, the presence of abnormalities on MRI will gradually diminish after several months [4] [11]. However, if a patient has suffered irreversible impairment of spinal neurological function, no matter how significant his/her reduction degree was, he/she has already missed the chance to experience improvement in spinal neurological function.
Limitation
There are some limitations in this study. First, a larger and prospective study will provide a firmer conclusion. Second, further exploration is required to determine whether the location of the fistula should be considered in calculating threshold for the degree of reduction. Last but not least, with the development of endovascular technology, whether our results will be different from those of patients who accept endovascular treatment is also worthy of research.
Conclusion
The extent of spinal edema was significantly correlated with preoperative neurological status in patients with SDAVF. Patients with a significant reduction in spinal edema on postoperative MRI were more likely to experience improvements in spinal neurological function. This study reveals that a satisfactory reduction in postoperative MRI results is a predictive factor of patient prognosis.
References
Cenzato M, Versari P, Righi C, Simionato F, Casali C, Giovanelli M (2004) Spinal dural arteriovenous fistulae: analysis of outcome in relation to pretreatment indicators. Neurosurgery 55:815–22 (discussion 822-3)
Cenzato M, Debernardi A, Stefini R, D’Aliberti G, Piparo M, Talamonti G et al (2012) Spinal dural arteriovenous fistulas: outcome and prognostic factors. Neurosurg Focus 32:E11
Fugate, J.E., G. Lanzino, and A.A. Rabinstein (2012) Clinical presentation and prognostic factors of spinal dural arteriovenous fistulas: an overview. Neurosurgical Focus, 32
Hetts SW, Moftakhar P, English JD, Dowd CF, Higashida RT, Lawton MT et al (2012) Spinal dural arteriovenous fistulas and intrathecal venous drainage: correlation between digital subtraction angiography, magnetic resonance imaging, and clinical findings. J Neurosurg Spine 16:433–440
Hunt R, Roberts RM, Mortimer AM (2018) Spinal dural arteriovenous fistula: delay to radiological diagnosis and sources of radiological error. Clin Radiol 73(835):e11-835 e16
Jellema K, Tijssen CC, van Gijn J (2006) Spinal dural arteriovenous fistulas: a congestive myelopathy that initially mimics a peripheral nerve disorder. Brain 129:3150–64
Kaufmann TJ, Morris JM, Saladino A, Mandrekar JN, Lanzino G (2011) Magnetic resonance imaging findings in treated spinal dural arteriovenous fistulas: lack of correlation with clinical outcomes. J Neurosurg Spine 14:548–54
Koch Matthew J, JS C, Agarwalla Pankaj K et al (2017) Open and endovascular treatment of spinal dural arteriovenous fistulas: a 10-year experience. J Neurosurg Spine 26:519–523
Krings T, Geibprasert S (2009) Spinal dural arteriovenous fistulas. AJNR Am J Neuroradiol 30:639–48
Lee J, Lim YM, Suh DC, Rhim SC, Kim SJ, Kim KK (2016) Clinical presentation, imaging findings, and prognosis of spinal dural arteriovenous fistula. J Clin Neurosci 26:105–9
Mascalchi M, Ferrito G, Quilici N, Mangiafico S, Cosottini M, Cellerini M et al (2001) Spinal vascular malformations: MR angiography after treatment. Radiology 219:346–353
Muralidharan R, Mandrekar J, Lanzino G, Atkinson JL, Rabinstein AA (2013) Prognostic value of clinical and radiological signs in the postoperative outcome of spinal dural arteriovenous fistula. Spine (Phila Pa 1976) 38:1188–93
Nagata S, Morioka T, Natori Y, Matsukado K, Sasaki T, Yamada T (2006) Factors that affect the surgical outcomes of spinal dural arteriovenous fistulas. Surg Neurol 65:563–8 (discussion 568)
Saladino A, Atkinson JL, Rabinstein AA, Piepgras DG, Marsh WR, Krauss WE et al (2010) Surgical treatment of spinal dural arteriovenous fistulae: a consecutive series of 154 patients. Neurosurgery 67:1350–7 (discussion 1357-8)
Shin DA, Park KY, Ji GY, Yi S, Ha Y, Park SW et al (2015) The use of magnetic resonance imaging in predicting the clinical outcome of spinal arteriovenous fistula. Yonsei Med J 56:397–402
Song JK, Vinuela F, Gobin YP, Duckwiler GR, Murayama Y, Kureshi I et al (2001) Surgical and endovascular treatment of spinal dural arteriovenous fistulas: long-term disability assessment and prognostic factors. J Neurosurg 94:199–204
Tadié M, Hemet J, Freger P, Clavier E, Creissard P (1985) Morphological and functional anatomy of spinal cord veins. J Neuroradiol 12:3–20
Willinsky RA, terBrugge K, Montanera W, Mikulis D, Wallace MC (1995) Posttreatment MR findings in spinal dural arteriovenous malformations. AJNR Am J Neuroradiol 16:2063–71
Yen PP, Ritchie KC, Shankar JJ (2014) Spinal dural arteriovenous fistula: correlation between radiological and clinical findings. J Neurosurg Spine 21:837–42
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine – Other
Rights and permissions
About this article
Cite this article
Luo, M., Li, J., Wu, C. et al. Prognostic value of magnetic resonance imaging in spinal dural arteriovenous fistulas. Acta Neurochir 164, 49–54 (2022). https://doi.org/10.1007/s00701-021-04970-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04970-5