Abstract
Background
The endoscopic endonasal approach for optic nerve decompression is suited for the management of non-traumatic optic neuropathy but remains underreported, presumably due to transcranial approaches still being favoured at individual centres.
Method
The optic canal is approached endoscopically and transsphenoidally through the contralateral nostril. Its inferomedial wall is opened using an irrigated diamond drill, and neuronavigation is used to confirm anatomical bearings.
Conclusion
This technique provides rapid and easy access to the inferomedial aspect of the optic canal and nerve. Optic nerve decompression through this approach is associated with low morbidity and should be considered as an alternative to transcranial approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic transnasal optic canal decompression is a well-described technique for traumatic optic neuropathy due to the easier access and view that it provides of the orbital apex and optic canal as compared with transcranial approaches [6, 9]. Reports of its use in non-traumatic, compressive pathology of the optic nerve have further expanded its indications [7, 9, 5]. Nonetheless, such reports remain few, presumably reflecting the technique’s underuse in individual centres. The reasons for this may be unawareness of the indications, which are rare, as well as unease with the endoscopic approach. Here we describe this versatile technique and provide our own adaptations.
Relevant surgical anatomy
The sphenoid ostium (Fig. 1) is located medial to the postero-inferior aspect of the superior turbinate and within 1 cm of the midline [3].
0-degree endoscopic view through left nostril of a 41-year-old patient with a right-sided intracanalicular ON sheath meningioma. a The nasal septum is on the left of the caption and the Freer dissector is in contact with the left middle turbinate. b The left middle turbinate is pushed aside with the Freer dissector, revealing the superior turbinate above and behind it. c The superior turbinate is in turn gently displaced superolaterally to reveal the sphenoid ostium. The left choana is also seen in the inferior part of this panel. d Same view as in c following enlargement of the left sphenoid ostium superiorly and contralaterally. Its expansion inferiorly is more modest than when performed for pituitary surgery where the aim is to reach the floor of the sella. e The mucosa inferomedial to the ostium is elevated to avoid injury to the branches of the sphenopalatine artery, the base of the anterior sphenoid wall is weakened with the punch up and down cuts, and the posterior nasal septum is disarticulated from its base and displaced into the contralateral nostril. f Same view as in d and e with the superior turbinate seen on the top right. The contralateral sphenoid ostium is joined to the anterior sphenoidotomy and itself expanded. The right-sided posterior ethmoid cells are opened retrogradely from the sphenoid sinus, as seen here where the upcut is removing the posterior-most wall of the posterior ethmoid cells to gain access to the orbital apex (see also Fig. 2). Elements of the sellar wall anatomy are appreciable on this caption
The sellar, optic and carotid prominences constitute the sellar wall of the sphenoid sinus (Fig. 1f; Fig. 2). The carotid prominence corresponds to the cavernous segment of the ICA. The tuberculum recess is a depression in the wall of the sella between the sellar prominence and the planum sphenoidale superiorly. Bilaterally, this recess becomes the MOCR. The MOCR is flanked by sellar prominence inferiorly, carotid prominence laterally and optic prominence superiorly. It accesses the superomedial aspect of the ICA’s clinoid and supraclinoid (ophthalmic) segments. The LOCR is a bony indentation between the optic prominence and the lateral aspect of the carotid prominence. It may be difficult to discern due to the variation in septations within the sphenoid sinus and their frequent relation with the carotid prominence [8]. The LOCR is endocranially in relation with the base of the optic strut, and its medial projection is in relation with the clinoid segment of the ICA. The OC’s endocranial opening is situated superiorly to the medial border of the LOCR [8, 1] (Fig. 2b).
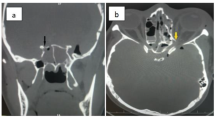
a Axial, bone-windowed computed tomography slice through the ethmoid and sphenoid sinuses in the patient from Fig. 1. The red arrows indicate the posterior-most wall of the right posterior ethmoid sinus. This same wall is indicated in b by the three white arrow heads. b Same trajectory of view as in Fig. 1f, showing sphenoid sinus anatomy. Asterisk, sphenoid septum; diamonds, carotid prominences; star, sellar prominence; cross, clival recess. The black dotted trapezoid shows the contour of the tuberculum recess. The medial optico-carotid recesses (MOCR) correspond to the bottom angles of the trapezoid, bilaterally. The dotted white lines delineate the superior and inferior aspects of the right optic prominence. The angle between the inferior dotted white line and the dotted blue line corresponds to the right lateral optico-carotid recess (LOCR). The white arrow heads point to the remaining posterior-most wall of the right posterior ethmoid sinus, which has been opened in a retrograde fashion to gain access to the orbital apex. The hollow arrow points to a defect made in the lamina papyracea, through which a lobule of orbital fat is seen to protrude
The intracanalicular ON measures approximately 10 mm in length [4]. Seeing that it is an extension of the central nervous system, it is also surrounded by an arachnoid space in communication with the chiasmatic cistern. The dura is continuous with the periorbita at the orbital apex [1].
The OA takes an intradural, inferolateral course within the OC. However, seeing that it branches off the anteromedial aspect of the ICA, it can be found inferomedially to the ON at the intracranial end of the OC [1]. And in 50% of these cases, it will pursue a medial course within the OC [10].
An Onodi air cell—or spheno-ethmoid air cell—is a posterior ethmoid air cell that extends superolaterally to the sphenoid sinus, to involve the ON or even the ICA. This variant is not infrequent and requires recognition to avoid inadvertent damage to the ON or ICA [7].
Description of the technique
Anaesthetic phase and positioning
Following intubation, the nasal mucosa is prepared with Moffett’s solution. The patient’s head is fixed in a head holder, in a slightly less flexed “conversational position” [2], and is registered to the neuronavigation station.
Transnasal phase
In contrast to the previous reports [7, 5], we perform a contralateral mononostril approach enabling a greater angle of access to the OC; also, the middle turbinate is not removed but only displaced laterally with the Freer dissector (Fig. 1a–b). The sphenoid ostium (Fig. 1c) is enlarged (Fig. 1d–e), the posterior septum is disarticulated and a wide anterior sphenoidotomy is made using punch-cuts towards the pathological side (Fig. 1f).
Transsphenoidal phase
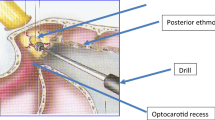
Septations are removed as necessary. The optico-carotid prominences and recesses are identified anatomically and confirmed with neuronavigation. The posterior-most ethmoid cells (Fig. 2) are opened in a retrograde fashion to obtain access to the orbital apex; this is in contrast to other techniques where a posterior ethmoidectomy is performed as a first step and independently of the sphenoidotomy [5]. The endoscope is fixed in the anterior sphenoidotomy’s supero-external corner, on the side of the approach. A high-speed diamond drill, with integrated irrigation, is used to remove or thin down the OC’s medial wall and floor, from the orbital apex to the OC’s endocranial opening, steering clear of the optic prominence’s inferior aspect at the endocranial end (Fig. 3). During drilling the sphenoid sinus is allowed to fill up with saline to the level of the optic canal such that the drill is partly submerged so reducing the risk of heat damage to the ON. A microcurette/dissector can be used to remove the thinned out layers of the bone.
Same view as in Fig. 2b. a The drill is used to remove the remnant posterior and posteromedial walls of the right posterior ethmoid sinus, b thereby opening the orbital apex. The exposed ON sheath is followed posteriorly, and the medial OC wall is drilled off (c) all the way to its endocranial opening, located superiorly to the medial border of the LOCR.
Closure
Haemostatic gelatin sponge is apposed over the opening. The septal wall is medialised. No nasal packing.
Indications
Aside from traumatic optic neuropathy [6], indications include inflammatory or tumoural intracanalicular pathology compressing the ON and causing visual disturbance, such as meningioma of the ON sheath prior to adjuvant radiotherapy (Fig. 4), sphenoid sinus pathology with OC extension and sphenoid fibro-osseous lesions [5, 7, 9]. The risk of ON damage from radiotherapy is reduced when the nerve is uncompressed. Patients with visual deterioration due to endocrine orbitopathy (Graves’ disease) generally require decompression of the orbital apex alone without opening of the OC [9].
a Coronal MRI slices (T2, turbo inversion recovery magnitude (TIRM) sequence) and b axial MRI slice (T1, fat-saturated post-gadolinium sequence) in a 63-year-old patient with a right ON sheath meningioma extending from the ON’s intraorbital segment, through the OC to wrap over the anterior clinoid process. The ON is displaced inferiorly. c Postoperative bone-windowed, oblique coronal slice, running perpendicularly through the right OC; the trajectory of this slice is shown by the light blue line on the inset of an axial slice of this CT (right upper corner of panel c). d Postoperative bone-windowed, oblique axial slice from the same CT, running through the long axis of the right OC. The extent of the decompression of the OC’s medial wall can be appreciated on panels c and d.
The technique is particularly suited for pathology located in the inferomedial OC quadrants [1] (Fig. 4).
Limitations
Pathology with intracranial extension: In such cases a transsphenoidal transtubercular endoscopic approach may also be indicated or a two-staged management with (a) transcranial resection of the intracranial pathology and (b) endoscopic endonasal OC decompression (if OC cannot be opened through the transcranial approach).
How to avoid complications
-
Detailed study of preoperative imaging (CT and MRI):
-
Sphenoid sinus pneumatisation and septation pattern; presence of Onodi cell
-
Variation in sphenoid sinus anatomy:
-
Attention to dehiscent ICA/ON
-
Absence of optic prominence when ICA is anterior to the ON in the medial aspect of the OC [8]
-
-
Course of OA
-
-
Use neuronavigation.
-
Drilling:
-
Copious irrigation
-
Leaving a thin shell of bone that can subsequently be removed with a blunt dissector
-
-
Doppler for ICA identification, in case of doubt.
-
Respect the periorbita to avoid outflow of orbital fat obliterating surgical view.
-
Prep abdomen for harvesting of fat graft in case of CSF leak.
-
Close association of the lesion with the ON sheath usually precludes its resection and even biopsy.
-
The questionable benefit of optic sheath opening should be weighed against its risks (injury to OA; CSF leak). If performed, should be in the superomedial quadrant to avoid the OA [7].
Specific perioperative considerations
-
Pre- and postoperative ophthalmological assessments.
-
Discharge is possible from postoperative day 1.
Specific information to give to the patient about surgery and potential risks
-
Expectations:
-
Extent of salvageable vision is difficult to predict. Eventual preoperative response to corticosteroids may provide an indication.
-
-
Risks:
-
CSF leak
-
Meningitis
-
Loss of monocular vision
-
Injury to ICA
-
Epistaxis
-
-
Post-operatively:
-
Avoid blowing of nose and other Valsalva manoeuvres for 4 weeks.
-
Abbreviations
- ICA:
-
Internal carotid artery
- OC :
-
Optic canal
- ON :
-
Optic nerve
- LOCR :
-
Lateral optico-carotid recess
- MOCR :
-
Medial optico-carotid recess
- OA:
-
Ophthalmic artery
- CSF :
-
Cerebrospinal fluid leak
References
Caporlingua A, Prior A, Cavagnaro MJ, Winston G, Oliveira DLC, Sadwhani SD, Arias GA, Schwalb JN, Akhbari M, Evins AI, Bernardo A (2019) The intracranial and intracanalicular optic nerve as seen through different surgical windows: endoscopic versus transcranial. World Neurosurg 124:522–538. https://doi.org/10.1016/j.wneu.2019.01.122
Ekanayake J, Baudracco I, Quereshi A, Vercauteren T, Dorward NL (2018) The conversational position in endoscopic pituitary surgery. Br J Neurosurg 32:44–46. https://doi.org/10.1080/02688697.2017.1406058
Gupta T, Aggarwal A, Sahni D (2013) Anatomical landmarks for locating the sphenoid ostium during endoscopic endonasal approach: a cadaveric study. Surg Radiol Anat 35:137–142. https://doi.org/10.1007/s00276-012-1018-8
Habal MB, Maniscalco JE, Rhoton AL Jr (1977) Microsurgical anatomy of the optic canal: correlates to optic nerve exposure. J Surg Res 22:527–533. https://doi.org/10.1016/0022-4804(77)90036-1
Jacquesson T, Abouaf L, Berhouma M, Jouanneau E (2014) How I do it: the endoscopic endonasal optic nerve and orbital apex decompression. Acta Neurochir 156:1891–1896. https://doi.org/10.1007/s00701-014-2199-1
Lin J, Hu W, Wu Q, Zhang J, Yan W (2019) An evolving perspective of endoscopic transnasal optic canal decompression for traumatic optic neuropathy in clinic. Neurosurg Rev. https://doi.org/10.1007/s10143-019-01208-y
Luxenberger W, Stammberger H, Jebeles JA, Walch C (1998) Endoscopic optic nerve decompression: the Graz experience. Laryngoscope 108:873–882. https://doi.org/10.1097/00005537-199806000-00016
Peris-Celda M, Kucukyuruk B, Monroy-Sosa A, Funaki T, Valentine R, Rhoton AL Jr (2013) The recesses of the sellar wall of the sphenoid sinus and their intracranial relationships. Neurosurgery 73:ons117–ons131; discussion ons131. https://doi.org/10.1227/NEU.0000000000000184
Pletcher SD, Metson R (2007) Endoscopic optic nerve decompression for nontraumatic optic neuropathy. Arch Otolaryngol Head Neck Surg 133:780–783. https://doi.org/10.1001/archotol.133.8.780
Zoli M, Manzoli L, Bonfatti R, Ruggeri A, Mariani GA, Bacci A, Sturiale C, Pasquini E, Billi AM, Frank G, Cocco L, Mazzatenta D (2016) Endoscopic endonasal anatomy of the ophthalmic artery in the optic canal. Acta Neurochir 158:1343–1350. https://doi.org/10.1007/s00701-016-2797-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
10 key points
1) Endoscopic endonasal approach provides minimally invasive access to the OC’s inferomedial quadrants.
2) Although rare, its indications include non-traumatic compressive pathology of the intracanalicular ON.
3) Its aim is to prevent further deterioration of vision and possibly to recover lost function.
4) Its morbidity is low.
5) Detailed study of preoperative imaging and the use of neuronavigation are essential.
6) Approach is through the contralateral nostril, to augment the angle of access to the pathological ON.
7) Transsphenoidal retrograde opening of the posterior ethmoid cells is usually sufficient.
8) Copious irrigation during drilling to prevent thermal injury of ON.
9) Vertical projection of LOCR’s medial border marks OC’s endocranial opening.
10) Intracanalicular pathology is usually unresectable due to the risk of injury to ON; the procedure is therefore often only intended as a means of decompression.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgical technique evaluation
Electronic supplementary material
Surgical video of patient from Figures 1-3: A 41-year-old female, with several small-sized meningiomata and a previous history of olfactory groove meningioma (transitional, WHO Grade I) resection, presented to us for the first time, with a 9-month history of progressive right monocular visual deterioration. A dedicated MRI of the orbits showed a right optic canal meningioma extending to the orbital apex. The video demonstrates a left nostril endoscopic approach for decompression of the right ON and describes the steps illustrated in Figures 1-3. Surgery was uneventful. Subjectively, the patient immediately noticed an improvement in the acuity and field of vision of her right eye. She was discharged the day following surgery. An ophthalmological assessment performed three months postoperatively demonstrated slight improvement in the results of visual field testing in comparison to the pre-operative assessment, but no objective improvement in visual acuity. The swelling of the optic disc noted pre-operatively had resolved. The patient was referred for intensity-modulated radiotherapy, for tumour stabilisation and protection of her residual vision (50.4 Gy in 28 fractions over 5½ weeks). (MP4 436634 kb).
Rights and permissions
About this article
Cite this article
Cabrilo, I., Dorward, N.L. Endoscopic endonasal intracanalicular optic nerve decompression: how I do it. Acta Neurochir 162, 2129–2134 (2020). https://doi.org/10.1007/s00701-020-04476-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04476-6