Abstract
Background
Few data are available on disability and quality of life (QOL) after surgery versus conservative management for unruptured brain arteriovenous malformations (uAVMs).
Objective
The aim of this study was to test the hypothesis that QOL and disability are worse after surgery ± preoperative embolisation for uAVM compared with conservative management.
Methods
We included consecutive patients diagnosed with uAVM from a prospective population-based study in Scotland (1999–2003; 2006–2010) and a prospective hospital-based series in Australia (2011–2015). We assessed outcomes on the modified Rankin Scale (mRS) and the Short Form (SF)-36 at ~ 12 months after surgery or conservative treatment and compared these groups using continuous ordinal regression in the two cohorts separately.
Results
Surgery was performed for 29% of all uAVM cases diagnosed in Scotland and 84% of all uAVM referred in Australia. There was no statistically significant difference between surgery and conservative management at 12 months among 79 patients in Scotland (mean SF-36 Physical Component Score (PCS) 39 [SD 14] vs. 39 [SD 13]; mean SF-36 Mental Component Score (MCS) 38 [SD 14] vs. 39 [SD 14]; mRS > 1, 24 vs. 9%), nor among 37 patients in Australia (PCS 51 [SD 10] vs. 49 [SD 6]; MCS 48 [SD 12] vs. 49 [SD 10]; mRS > 1, 19 vs. 30%). In the Australian series, there was no statistically significant change in the MCS and PCS between baseline before surgery or conservative management and 12 months.
Conclusions
We did not find a statistically significant difference between surgery ± preoperative embolisation and conservative management in disability or QOL at 12 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The multicentre, non-blinded randomised trial of unruptured brain arteriovenous malformation (uAVM) management (ARUBA) found medical management to be superior to interventional therapy for the prevention of death or stroke [14]. The results of ARUBA were similar in the non-randomised Scottish Audit of Intracranial Vascular Malformations (SAIVMs) [1]. Surgery constituted 16% of interventions in ARUBA but is used to treat as many as 100% of uAVM in some case series [3]. One of the criticisms of ARUBA is that the frequency of the use of endovascular, radiosurgery, surgery, or a combination of therapies may have confounded its overall finding that medical management was superior to interventional therapy [3, 8, 13, 15, 22, 32]. Therefore, the association between surgery and outcomes for uAVM deserves further and specific scrutiny.
A further consideration is the outcome measurement instruments and the outcome of interest to the patient and clinician in the management of uAVM. Outcome studies of AVM report survival [1, 3], risk of haemorrhage [6, 11, 31], and disability [1, 3, 4, 12, 15, 17, 22, 32]. Studies have infrequently reported quality of life (QOL) outcomes [5, 21]. Published studies that have reported on QOL for patients with uAVM either have focused on a subset of uAVM patients or have not been restricted to uAVM [7, 20, 26]. Although ARUBA found worse functional outcome after interventional therapy versus conservative management, QOL outcomes have yet to be reported [13]. For the patient, QOL is important because it encompasses the beneficial and adverse consequences of any management strategy from the patient’s perspective. However, patients with an uAVM may not experience the anticipated adverse impact of disability (measured by the modified Rankin Scale (mRS)) on QOL if left untreated, nor the anticipated benefit of disability avoidance if treated [5, 16, 26].
Therefore, we set out to test the hypothesis that QOL and disability are worse after surgery ± preoperative embolisation for uAVM compared with conservative management. Because outcomes may be very context-specific, we tested the hypothesis in two observational cohorts separately: a population-based cohort in Scotland [1] and a single-centre specialist cerebrovascular neurosurgical practice in Australia [3].
Methods and materials
Enrolment protocol
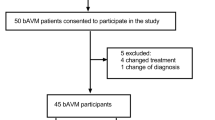
The flow chart of patient enrolment is illustrated in Fig. 1. The National Health Service SAIVMs is a prospective, population-based cohort study that includes Scottish residents aged 16 years or older when first diagnosed as having a bAVM in 1999–2003 or 2006–2010 [1]. This cohort includes patients seen in general and specialist neurosurgical practice at all four neuroscience centres in Scotland. The SAIVMs used multiple overlapping sources of case ascertainment to identify adults meeting the inclusion criteria. The surgical patients in the SAIVMs cohort included patients who underwent preoperative embolisation. The Scottish Intracranial Vascular Malformation Study (SIVMS) is a subset of SAIVMs, in which participants consent to complete annual postal outcome questionnaires. Macquarie Health, Neurosurgery, Macquarie University (Macquarie University) in Sydney, Australia, consists of a university hospital with both campus and remote clinics. Referrals to a specialist vascular neurosurgeon with an interest in AVM at Macquarie University are mostly residents of the state of New South Wales (NSW) but also include interstate and international patients. Patients who were prospectively enrolled with newly diagnosed uAVM at the time of first referral to Macquarie University between 2011 and 2015 consented to participate in the study. No patient at Macquarie University had preoperative embolisation.
The SIVMS was approved by the Multicenter Research Ethics Committee for Scotland and the Fife and Forth Valley Research Ethics Committee. The Macquarie University study was approved by the Macquarie University Human Ethics Committee. Both components of this study were performed in accordance with their respective institutional ethics committee guidelines.
Baseline demographic, angioarchitectural, and clinical data
Demographic, angioarchitectural, and clinical data were collected for each patient. This included data that allowed the Spetzler-Martin (SM) grade to be calculated (Table 1) [24]. The SM grade was established by allocating points for size (1 for less than 3 cm, 2 for size between 3 and 6 cm, and 3 for size greater than 6 cm), the presence of deep venous drainage (adding 1 point if present), and location in “eloquent” brain (adding 1 point if located in the primary sensory cortex, motor cortex, language cortex, visual cortex, internal capsule, diencephalon, brainstem, deep cerebellar nuclei, or cerebellar peduncle). However, not everyone with uAVM in SAIVMS underwent catheter angiography if they were managed conservatively, so SM grade for these cases was not calculable due to a lack of information on venous drainage. Cases with an allocated SM grade were grouped by Spetzler-Ponce class (SPC) to facilitate analyses. The SPC is a simplification of the SM grading system that has been validated to predict the risk of surgery, combines SM grades 1 and 2 as SPC A, SM grade 3 as SPC B, and SM grades 4 and 5 as SPC C [25].
QOL and disability outcome assessments
The following outcome measures were collected:
-
i.
The Medical Outcomes Study Short Form-36 Health Survey Questionnaire (SF-36) is a measure that provides an eight-item profile of scores across physical, mental, and emotional aspects of subjective health [30]. Factor analytic techniques have been used to produce summary scores from the eight subscales: the Physical Component Score (PCS) and Mental Component Score (MCS) [29]. We used formulae for z-score standardisations, estimating aggregate component scores and T-score transformation of component scores to convert raw scores from SF-36 version 1 to PCS and MCS using 1998 general U.S. population means, standard deviations, and 1990 factor score coefficients [29]. This enabled comparison of PCS and MCS between the SIVMS and Macquarie University cohorts. For the purpose of dichotomising outcomes, significant adverse outcomes for PCS and MCS were considered to be a decline in score by 6.5, based upon standards used by Bayliss and colleagues and Ware and colleagues of the minimally important change for individuals studied longitudinally [2, 28]. These are termed minimally important change (MIC) for PCS and MIC for MCS [2, 28].
-
ii.
The Barthel Index (BI) is a measure of self-care performance. The BI has a maximum score of 20 [9]. The modified Barthel Index (mBI) uses the same categories as the BI but has a maximum score of 100. The mBI was developed for rating of self-care performance by observation or interview [23]. The BI was collected in the SIVMS and the mBI in the Macquarie University study. To enable comparison, scores were dichotomised; a poor outcome was a score less than the optimal (maximum).
-
iii.
The mRS is a measure of disability for everyday life activities and was used in both cohorts. Patients and clinicians rated the mRS in the SIVMS, and the clinician rated the mRS for the Macquarie University cohort. The mRS scores were dichotomised; a poor outcome was considered to be a mRS score of greater than 1 [18, 27].
Administration of outcome instruments
SIVMS
Questionnaires were posted to all uAVM patients in the SIVMS cohort after approval to contact was provided by the treating general practitioner and opt-in consent was granted from the participant/carer. Once consent was confirmed, questionnaires were sent annually shortly before the anniversary of the initial presentation that led to uAVM diagnosis. Questionnaires included self-rating scales for the SF-36 [30], BI [9], and mRS [27]. The initial presentation mRS score was rated by researchers’ review of medical records. The first version of the SF-36 was available and administered in the SIVMS. This version was implemented throughout the study period in order to maintain consistency in repeated measures.
Macquarie University
At Macquarie University, consent to participate in the study was sought at presentation of an uAVM from 2011 to 2015 and enrolment was prospective. Follow-up occurred 6 to 12 weeks postoperatively if surgically treated, and a 12-month follow-up was conducted either following surgery or initial presentation (for conservatively managed cases). It was often not possible for regional, interstate, and overseas participants to attend all follow-up appointments on-site. Correspondence from local doctors and family was monitored for changes in functional status, and questionnaires were posted to all participants who did not attend the 12-month follow-up. Questionnaires were also posted to all participants for whom the 12-month follow-up period had expired. The SF-36v2 (with software converting scores to 1998 US norms summary scores; licence number QM008025) was administered, and the mBI was rated by a single occupational therapist. The mRS scores were allocated by the treating surgeons, and the occupational therapist was blinded to these scores until after the final follow-up data were collected.
Timing of administration of outcome instruments
Time points of data collection were not uniform between the SIVMS and Macquarie University. In the SIVMS, because of the method of case identification, the completed battery of assessments was related to the time of the initial clinical presentation that led to uAVM diagnosis. Following referral to a specialist referral centre, preoperative data were available from Macquarie University, as were outcomes 12 months after surgery, which were used to analyse change over the first year after referral with a new diagnosis of uAVM. The common time point for outcome data collection in the SIVMS and Macquarie University was ~ 12 months after initial presentation/assessment for conservatively managed uAVM and ~ 12 months after surgery for surgically managed uAVM.
Statistical analysis
We performed statistical analysis using IBM SPSS (version 22; IBM Corp, Armonk, NY) and Prism (version 7; GraphPad Software Inc., La Jolla, CA). Baseline characteristics were grouped into categorical variables and compared within and between cohorts using the Pearson chi-square test (or Fisher’s exact test if cell sizes were < 5). We analysed continuous variables using Welch’s t test to account for unequal sample sizes and variance, and QOL using Pearson’s bivariate correlations or Spearman’s rho (where appropriate). Because of the ordinal ranking of the mRS outcome score, continuous ordinal regression was used to detect relationships between variables [10]. We used a statistical significance level of 5%.
Results
Seventy-nine patients (29%) from the SIVMS cohort and 37 (84%) patients from the Macquarie University cohort were eligible for inclusion in the study (Fig. 1). There were relatively similar distributions of SPC categories of uAVM in the two cohorts (Table 1). Because of the differences in study design between the SIVMS and Macquarie University cohorts, we analysed the SIVMS cohort and Macquarie University series separately.
Differences in baseline characteristics and management between cohorts
SIVMS cohort
From the 204 Scottish residents diagnosed with an uAVM between 1999–2003 and 2006–2010, 134 were conservatively managed or had surgical treatment with or without endovascular intervention or radiosurgery. Eighty patients consented to complete annual postal QOL questionnaires, of whom one was excluded due to no response in either the first or second year. Fifty-six were conservatively managed, and 23 had surgical treatment, of whom ten were treated exclusively by surgery (Fig. 1). Examination of baseline characteristics found no significant difference in age, gender, presentation mRS, uAVM eloquence, or SPC group between responders and people who did not consent to complete the annual questionnaire. Of the patients who responded, patients undergoing conservative management were significantly older (mean years 52 ± 15 SD vs. mean years 41 ± 11 SD; p < 0.01), had more uAVM in surgically eloquent brain areas (59 vs. 39%; p < 0.01), and had higher uAVM SPC grades (23 vs. 0%; p = 0.02) than the surgically managed group (Table 1). Socioeconomic status, indicated by the deprivation category of residents’ postcodes, was not significantly lower in the surgically managed group. There were no significant differences between the conservatively and surgically managed groups in the SF-36 subscales (Table 2). There were no significant differences in BI or mRS scores between the conservative and surgical groups in either of the 2 years of follow-up.
Macquarie University cohort
Forty-seven patients referred to Macquarie University with a newly diagnosed uAVM between 2011 and 2015 consented to participate in the study (Fig. 1). Three patients who lived interstate did not return for follow-up, four did not complete the QOL questionnaire on each occasion, and three proceeded to have non-surgical treatment. Six were conservatively managed, and 31 had surgery to excise the uAVM (Fig. 1). There was a non-significantly higher proportion of patients with an uAVM in an eloquent region in the conservative group (83%) than in the surgical group (39%) (p = 0.08). There was a significantly higher proportion of SPC A uAVM in the surgical group (70%) compared with the conservative group (17%; p < 0.01). There were no significant differences between the surgical and conservative groups in any of the SF-36v2 subscale scores, mBI or mRS at initial or 12-month follow-up (Table 2). No significant differences were found in any of the mental health subscales of the SF-36v2 or either of the outcome scales.
Change in QOL and disability for each cohort comparing preoperative with postoperative outcomes
There were no significant differences in either cohort between the conservative and the surgical groups in the proportion of patients experiencing a MIC in MCS, PCS, mBI, or mRS 1 year after initial assessment (Table 3). It was only possible to examine the clinician-rated mRS in the SIVMS cohort over this time interval. In the two patients with deterioration in mRS managed conservatively at Macquarie University, one patient had a progressive neurological deficit (24 year old with SPC C) and the second a haemorrhage event (68 year old with SPC B). In the 14 patients with deterioration in mRS managed conservatively in the SIVMS cohort, it was not possible to ascertain the reason for this deterioration from the questionnaires.
Discussion
In this study of two prospective uAVM cohorts, there was no statistically significant difference in outcome between surgery ± preoperative embolisation and conservative management in either cohort. Therefore, we were unable to confirm our hypothesis that QOL and disability are worse after surgery ± preoperative embolisation for uAVM compared with conservative management.
For the Macquarie cohort, there was no significant deterioration in the outcome scores (PCS, MCS, mRS, and mBI) for the interval between assessment and 12 months following surgery. Those undergoing surgery had a mean younger age, were less often in eloquent brain, had a mean smaller size, and were more likely to be SPC A than conservatively managed uAVM. Because of these differences, direct comparison between conservative and surgical management is probably confounded. We did not find a loss of QOL or function for patients who had conservative management for their uAVM.
There are a number of limitations in this study. These include a small number of cases managed in both cohorts. This has the potential for a type II error in statistical analysis. mRS has limitations in capturing the full patient experience. This finding has been previously reported with serious complications of surgery that do not result in disability [19], and despite the association between mRS and QOL outcomes of PCS and MCS, adverse QOL outcome (as measured by SF-36) may occur in the absence of an adverse mRS outcome. There were differences between the two cohorts that prevented the combination of data for the purpose of determining overall outcomes. For surgically managed uAVM, the presentation mRS was significantly better in the Macquarie University cohort than in the Scottish cohort. In addition, these two cohorts differed with respect to the distribution of patients undergoing surgery, 29% of the Scottish cohort and 84% of the Macquarie University cohort.
Another limitation is that the two cohorts are sourced from very different origins. One cohort is an all-inclusive national cohort, and the other is a single-institution referral centre, recruiting patients prospectively, with the initial assessments occurring shortly after referral. Despite the potential biases arising from the variations in cohort acquirement, there was no overall difference in the patients’ perceived QOL or function for the management of their uAVM. Cohort acquirement also did not affect the range of severity of uAVM in the two cohorts. Both cohorts had a similar distribution of low- and high-grade uAVM.
There was a lack of selection bias in the all-inclusive national SAIVMS cohort; however, there is the possibility of a different national culture of treatment for uAVM. Cerebrovascular surgery is less frequently performed in Scotland, indicated by the number of patients who had surgical treatment (23) compared with conservative management (56) for their uAVM over the 11-year period. In the Macquarie University cohort, 31 of the 37 patients had surgery during the 5-year period. Being a hospital-based practice, this may reflect a referral bias. These differences exemplify the importance that the manner of sourcing a cohort needs solicitous scrutiny of the potential impact upon results. The results from a population may not reflect institutional experiences and vice versa.
There was the potential for observer bias in both cohorts, as outcomes were not rated blind to treatment. In the Macquarie University cohort, each patient rated QOL and clinician rated the disability scales. Whereas in the SIVMS cohort, each patient rated both disability and QOL scales. There are limitations in the self-reporting nature of QOL measures such as the SF-36. The scores do not necessarily indicate the higher level of function of patients, such as the ability to return to driving a motor vehicle. All patients were able to complete the SF-36 at 12 months after initial presentation in the Macquarie University cohort. The SIVMS cohort contained only patients or carers who responded to the posted questionnaire containing the SF-36 and mRS. QOL may also have been confounded by other co-morbidities that were not assessed or described in this study, which could have worsened the QOL in the SIVMS conservatively managed group by virtue of being a decade older than the surgically managed patients.
This is not a study of all management pathways for uAVM. Of the 204 uAVM cases identified in the SAIVMS cohort during this time, 70 were managed by endovascular or radiosurgery and excluded from this analysis. Of the Macquarie University cohort, three patients that had changed treatments after agreeing to participate at Macquarie University had radiosurgery uAVM and no patient had endovascular treatment. Therefore, no conclusions can be drawn about endovascular and radiosurgery. However, in the light of the criticism that ARUBA enrolled only 18 patients that underwent surgery (or surgery following preoperative embolisation), it is important to compare outcome following surgery versus conservative management.
Further comparative observational studies are needed to ascertain the association between uAVM treatment and QOL. In the absence of dramatic treatment effects on QOL in our observational data and other studies, QOL outcomes in the ARUBA trial (and other ongoing randomised trials such as TOBAS, NCT02098252) are keenly awaited.
References
Al-Shahi Salman R, White PM, Counsell CE, du Plessis J, van Beijnum J, Josephson CB, Wilkinson T, Wedderburn CJ, Chandy Z, St George EJ, Sellar RJ, Warlow CP, Scottish Audit of Intracranial Vascular Malformations Collaborators (2014) Outcome after conservative management or intervention for unruptured brain arteriovenous malformations. JAMA 311:1661–1669
Bayliss EA, Bayliss MS, Ware JE (2004) Predicting declines in physical function in persons with multiple chronic medical conditions: what we can learn from the medical problem list. Health Qual Life Outcomes 2:47. https://doi.org/10.1186/1477-7525-2-47
Bervini D, Morgan MK, Ritson EA, Heller G (2014) Surgery for unruptured arteriovenous malformations of the brain is better than conservative management for selected cases: a prospective cohort study. J Neurosurg 121:878–890
Davidson AS, Morgan MK (2010) How safe is arteriovenous malformation surgery? A prospective, observational study of surgery as first-line treatment for brain arteriovenous malformations. Neurosurgery 66:498–504
Della Puppa A, Rustemi O, Scienza R (2015) Quality of life of patients affected by unruptured brain AVMs. J Neurosurg 122:984–985
Iansek R, Elstein AS, Balla JI (1983) Application of decision analysis to management of cerebral arteriovenous malformation. Lancet 1(8334):1132–1135
Lai EHP, Lun SLC (2002) Impact on the quality of life of patients with arteriovenous malformations during the latent interval between gamma knife radiosurgery and lesion obliteration. J Neurosurg 97(SUPPL. 5):471–473
Magro E, Gentric J-C, Darsault TE, Ziegler D, Bojanowski MW, Raymond J (2017) Response to ARUBA: a systematic review and critical analysis for the design of future arteriovenous malformation trials. J Neurosurg 126:486–494
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Manuguerra M, Heller GZ (2010) Ordinal regression models for continuous scales. Int J Biostat 6:Article 14
Mast H, Young WL, Koennecke HC, Sciacca RR, Osipov A, Pile-Spellman J, Hacein-Bey L, Duong H, Stein BM, Mohr JP (1997) Risk of spontaneous haemorrhage after diagnosis of cerebral arteriovenous malformation. Lancet 350:1065–1068
Mohr JP, Moskowitz AJ, Stapf C, Hartmann A, Lord K, Marshall SM, Mast H, Moquete E, Moy CS, Parides M, Pile-Spellman J, Al-Shahi Salman R, Weinberg A, Young WL, Estevez A, Kureshi I, Brisman JL (2010) The ARUBA trial: current status, future hopes. Stroke 41(8):e537–e540
Mohr JP, Overby JR, von Kummer R, Stefani MA, Libman R, Stapf C, Parides MK, Pile-Spellman J, Moquete E, Moy CS, Vicaut E, Moskowitz AJ, Harkness K, Cordonnier C, Biondi A, Houdart E, Berkefeld J, CJM K, Barreau X, Kim H, Hartmann A, International ARUBA investigators (2017) Functional impairments for outcomes in a randomized trial of unruptured brain AVMs. Neurology 89(14):1499–1506
Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, Al-Shahi Salman R, Vicaut E, Young WL, Houdart E, Cordonnier C, Stefani MA, Hartmann A, von Kummer R, Biondi A, Berkefeld J, Klijn CJ, Harkness K, Libman R, Barreau X, Moskowitz AJ, international ARUBA investigators (2014) Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet 383:614–621
Moon K, Levitt MR, Nakaji P, Albuquerque FC, Zabramski JM, McDougall CG, Spetzler RF (2015) Safety and efficacy of surgical resection of unruptured low-grade arteriovenous malformations from the modern decade. Neurosurgery 77:948–953
O’Donnell J, Morgan MK (2015) Response. J Neurosurg 122(4):985–986
Potts MB, Lau D, Abla AA, Kim H, Young WL, Lawton MT (2015) Current surgical results with low-grade arteriovenous malformations. J Neurosurg 122:912–920
Quinn TJ, Dawson J, Walters MR, Lees KR (2009) Reliability of the modified Rankin Scale. A systematic review. Stroke 40:3393–3395
Reponen E, Tuominen H, Hernesniemi J, Korja M (2016) Modified Rankin Scale and short-term outcome in cranial neurosurgery: a prospective and unselected cohort study. World Neurosurg 91:567–573
Rohn B, Haenggi D, Etminan N, Kunz M, Turowski B, Steiger HJ (2014) Epilepsy, headache, and quality of life after resection of cerebral arteriovenous malformations. J Neurol Surg A Cent Eur Neurosurg 75(4):282–288
Rohn B, Hänggi D, Etminan N, Turowski B, Steiger HJ (2017) Relief of epilepsy and headache and quality of life after microsurgical treatment of unruptured brain AVM—audit of a single-center series and comprehensive review of the literature. Neurosurg Rev 40(1):59–65
Schramm J, Schaller K, Esche J, Bostrom A (2017) Microsurgery for cerebral arteriovenous malformations: subgroup outcomes in a consecutive series of 288 cases. J Neurosurg 125:1056–1063
Shah S, Cooper B (1993) Issues in the choice of activities of daily living assessment. Aust Occup Ther J 40(2):77–82
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65(4):476–483
Spetzler RF, Ponce FA (2011) A 3-tier classification of cerebral arteriovenous malformations. J Neurosurg 114(3):842–849
van der Schaaf IC, Brilstra EH, Rinkel GJ, Bossuyt PM, van Gijn J (2002) Quality of life, anxiety, and depression in patients with an untreated intracranial aneurysm or arteriovenous malformation. Stroke 33(2):440–443
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJA, Van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5):604–607
Ware JE Jr, Bayliss MS, Rogers WH, Kosinski M, Tarlov AR (1996) Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems. Results from the Medical Outcomes Study. JAMA 276:1039–1047
Ware JE Jr, Kosinski MA (2002) SF-36 physical and mental health summary scales: a manual for users of version 1, 2nd edn. QualityMetric Incorporated, Lincoln
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Wedderburn CJ, van Beijnum J, Bhattacharya JJ, Counsell CE, Papanastassiou V, Ritchie V, Roberts RC, Sellar RJ, Warlow CP, Al-Shahi Salman R (2008) Outcome after interventional or conservative management of unruptured brain arteriovenous malformations: a prospective, population-based cohort study. Lancet Neurol 7(3):223–230
Wong J, Slomovic A, Ibrahim G, Radovanovic I, Tymianski M (2017) Microsurgery for ARUBA trial (A Randomized Trial of Unruptured Brain Arteriovenous Malformations)-eligible unruptured brain arteriovenous malformations. Stroke 48:136–144
Funding
The Australian series was funded by the Macquarie University Post-Graduate Research Fund and Australian Government Research Training Program Scholarship. The Scottish study was funded by the Medical Research Council (grants G84/5176, G108/613, and G1002605), the Chief Scientist Office of the Scottish Government (grants K/MRS/50/C2704 and CZB/4/35), and the Stroke Association (grant TSA04/01). The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Conflict of interest
The authors declared that they have no competing interests.
Rights and permissions
About this article
Cite this article
O’Donnell, J.M., Al-Shahi Salman, R., Manuguerra, M. et al. Quality of life and disability 12 months after surgery vs. conservative management for unruptured brain arteriovenous malformations: Scottish population-based and Australian hospital-based studies. Acta Neurochir 160, 559–566 (2018). https://doi.org/10.1007/s00701-017-3451-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3451-2