Abstract
Background
Severe traumatic brain injury (sTBI) is a major cause of morbidity and mortality. Intracranial pressure (ICP) monitoring and management form the cornerstone of treatment paradigms for sTBI in developed countries. We examine the available randomized controlled trial (RCT) data on the impact of ICP management on clinical outcomes after sTBI.
Methods
A systematic review of the literature on ICP management following sTBI was performed to identify pertinent RCT articles.
Results
We identified six RCT articles that examined whether ICP monitoring, decompressive craniectomy, or barbiturate coma improved clinical outcomes after sTBI. These studies support (1) the utility of ICP monitoring in the management of sTBI patients and (2) craniectomy and barbiturate coma as effective methods for the management of intracranial hypertension secondary to sTBI. However, despite adequate ICP control in sTBI patients, a significant proportion of surviving patients remain severely disabled.
Conclusions
If one sets the bar at the level of functional independence, then the RCT data raises questions pertaining to the utility of decompressive craniectomy and barbiturate coma in the setting of sTBI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Severe traumatic brain injury (sTBI) is a major source of morbidity, mortality, and health care costs in the US. Approximately 1.7 million patients suffer TBI annually, causing 124,000 disabilities and 52,000 deaths [21, 25]. Health costs associated with TBI in the US total more than $60 billion annually [19]. In Europe, sTBI is the most common cause of disability in young adults, with related health care costs of approximately $37.5 billion [2]. Similar findings are reported globally [1, 11, 16], indicating the public health importance of and the personal cost exacted by sTBI.
As determinants of clinical outcome, the relative contributions of the injuries sustained at the time of sTBI and injuries secondary to persistently elevated intracranial pressure (ICP) remain unclear. There are currently no medical or surgical interventions that can reverse the physical damage incurred during the traumatic event. While brain oxygenation and metabolism monitoring may provide opportunities for therapeutic intervention in sTBI patients [15, 18], the current tenet of sTBI management rests on mitigating secondary brain injury, much of which is related to ICP elevation. Medically refractory intracranial hypertension following sTBI is the most common cause of death in this setting [20]. First-tier interventions to maintain ICPs include ventricular drainage of cerebrospinal fluid, osmotic agents such as mannitol or hypertonic saline, moderate sedation/paralytics, and transient hyperventilation as a temporizing measure. Second-tier interventions, reserved for patients with ICPs refractory to first-tier maneuvers, include decompressive craniectomy and barbiturate coma [3, 12].
Here we perform a comprehensive search of the literature to identify randomized controlled trials (RCTs) that examine the clinical efficacy of ICP monitoring, decompressive craniectomy, and barbiturate coma in patients with sTBI.
Methods
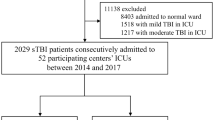
The English-language literature was searched using the PubMed (MEDLINE) electronic database (https://www.ncbi.nlm.nih.gov/pubmed/) (1980–2017, cutoff date May 1, 2017) and the following search terms: traumatic brain injury, head injury, craniocerebral trauma, intracranial pressure, and intracranial hypertension (see Supplemental Materials for the precise search methodology). Initial inclusion criteria were set by the following search restrictions: (1) original research as defined by a ‘comparative study’ or ‘randomized controlled trial’ study type, (2) published in English, and (3) involved human subjects. Nine hundred forty-eight articles were identified using these search criteria. These articles were then screened by RR and CC. Returned articles meeting these search criteria were excluded on manual review if they did not include RCT data related to the efficacy of ICP monitoring, decompressive craniectomy, and barbiturate therapy following TBI (Fig. 1). Six relevant articles were identified. Secondary searches of the EMBASE and Cocharne databases did not identify additional RCTs that were not captured using our PubMed (MEDLINE) search. Paper components reported include: author, year of publication, years of data collection, number of study sites, study design, number of patients, patient inclusion and exclusion criteria, interventions utilized in the study groups, primary and secondary outcomes, main findings with an emphasis on those pertaining to intracranial pressure, complication rates, and study limitations or sources of potential bias (see Table 1 for a summary of included studies).
Results
Utility of ICP monitoring
Benchmark evidence from South American trials: treatment of intracranial pressure: BEST-TRIP
The placement of an ICP monitor following sTBI is an accepted standard of care in developed countries, including the US [3]. As such, randomizing sTBI patients to forego ICP monitoring would not be acceptable if proposed in these countries. In this context, Chesnut et al. conducted an RCT based in Bolivia and Ecuador (2008–2011), where ICP monitoring is not the standard of care [6]. The authors randomized 324 patients with sTBI to either guideline-based care using continuous ICP monitoring (157 patients) or a treatment protocol based on serial imaging and neurologic examinations (167 patients). Inclusion criteria were sTBI (defined by GCS 3–8 on admission or decline to GCS 3–9 within 48 h of injury) and ≥13 years old. Patients with non-survivable injuries or a GCS of 3 with bilateral fixed and dilated pupils were excluded. Randomization was stratified by clinical site, severity of injury, and patient age. Patients randomized to ICP monitoring had intraparenchymal monitors placed at presentation, with management aimed to maintain ICPs < 20 mmHg using a standard progression from hyperosmolar therapy and ventricular drainage to high-dose barbiturate therapy for intractable intracranial hypertension. Patients in the non-ICP monitoring group were treated for clinical or radiographic signs of intracranial hypertension at fixed schedules via hyperosmolar therapies and/or ventricular drainage. High-dose barbiturates were initiated for patients with persistent radiographic or clinical findings. Decompressive craniectomy was utilized for treatment of medically intractable intracranial hypertension. The primary outcome was a composite score based on (1) overall survival, (2) functional status at 3 and 6 months [assessed using the Extended Glasgow Outcome Scale (GOS-E)], and (3) neuropsychologic status at 6 months. Secondary outcomes included frequency of first- (hyperosmolar therapy) and second-tier treatments (barbiturate or craniectomy) for elevated ICPs, systemic complications, and various measures of hospital stay. The sample size of 324 patients would detect an increase of 10 percentage points in patients with a good outcome or moderate disability based on GOS-E.
Baseline characteristics of the study participants were comparable across groups; 92% of randomized patients were followed for 6 months or until death. This study found no difference in composite score with or without ICP monitoring (56 versus 53, p = 0.49). Six-month mortality was also not significantly different between groups (39 versus 41%; p = 0.60). The rates of non-neurologic complications (85 versus 88%; p = 0.52) and serious adverse events (70 versus 76 events; p = 0.91) were similar between the pressure-monitoring and imaging/clinical examination groups. Patients in the imaging/clinical examination group received more hypertonic saline (p = 0.008) and hyperventilation (p = 0.003). In contrast, use of barbiturates was higher in the ICP monitoring arm (24 versus 13%; p = 0.02). Approximately 30% of enrolled patients underwent decompressive craniectomy, with a similar frequency between the two study arms (p = 0.81). Six percent of patients suffered complications related to placement of the ICP monitor.
We assessed the quality of BEST-TRIP using the Cochrane risk of bias tool [13]. The likelihood for selection bias in this study is low given the use of random sequence generators and allocation concealment. The baseline characteristics of the two arms were comparable. Due to the nature of the study, it was impossible to blind the participants to the intervention. However, given the selection of unconscious patients with a GCS of 3–8, it is unlikely that patients performed differentially as a result of unblinded clinical interventions. The likelihood of detection bias is low since the outcomes were determined by trained examiners who were unaware of the group assignments. Handling of attrition and data exclusion are documented in detail. There was little evidence of selective reporting in terms of outcome.
Utility of decompressive craniectomy
Two RCTs have assessed the clinical outcome of sTBI patients with sustained ICP elevations randomized to treatment with decompressive craniectomy versus medical management alone [7, 14].
Decompressive craniectomy in diffuse traumatic brain injury (DECRA)
The DECRA study by Cooper et al. involved 15 centers and 155 patients from 2002 to 2010 [7]. Inclusion criteria were: ages 15 to 59 years and severe non-penetrating TBI (defined as GCS 3 to 8 or Marshall class III [moderate diffuse injury on computerized tomography] [17]) with intracranial hypertension refractory to first-tier treatments (ICP > 20 mmHg for > 15 min within a 1-h period) within the first 72 h of presentation. Patients with non-survivable injuries, dilated unreactive pupils, surgical mass lesions, spinal cord injuries, or cardiac arrest following trauma were excluded. Patients were randomized within 72 h of injury to undergo a bifrontal craniectomy with bilateral dural openings plus standard medical care, or standard medical care alone [second-tier ICPs therapies included mild hypothermia (to 35 °C) and/or barbiturates]. Patients assigned to medical therapy were eligible for life-saving decompressive craniectomies. Randomization was stratified by study site and type of ICP monitoring device (intraparenchymal catheter or external ventricular drain). The primary outcome was the proportion of patients with favorable GOS-E (defined as 5–8 or moderate disability to good recovery) 6 months after injury. Secondary outcomes included hourly ICPs, the intracranial hypertension index (% of end hourly measures of ICPs > 20 mmHg), proportion of surviving patients dependent or with severe disability (GOS-E scores of 2 to 4), days in the ICU and hospital, and 6-month mortality.
Overall, 73 patients were randomized to medical therapy, and 82 were randomized to decompressive craniectomy. Fifteen patients (18%) assigned to the medically managed group underwent delayed decompressive craniectomy. Intent-to-treat analysis was performed using ordinal GOS-E. Although the craniectomy group showed worse 6-month GOS-E relative to the medically managed group (median GOS-E score of 3 versus 4; p = 0.03), this difference lost significance when adjusted for baseline pupil reactivity on a post-hoc analysis (p = 0.15). Patients treated with craniectomies showed lower mean ICPs (14.4 versus 19.1 mmHg; p < 0.001), less time with ICPs above 20 mmHg (9.2 versus 30.0 h; p < 0.001), and a lower intracranial hypertension index (11.5 versus 19.9; p < 0.001), suggesting that decompressive craniectomy is an effective means of managing ICP. There were no significant differences in 6-month mortality (19 versus 18%) between the craniectomy and medically managed cohorts. Thirty-seven percent of patients in the craniectomy group and 17% of the medically managed patients suffered one or more medical or surgical complications.
We assessed the quality of DECRA using the Cochrane risk of bias tool [13]. There is evidence for selection bias since a higher proportion of patients with unreactive pupils were randomized to the craniectomy group relative to medical management (27 versus 12%, p = 0.04). The criteria for performing craniectomy (ICP > 20 mmHg for 15 min) and the type of craniectomy performed were standardized (bifrontotemporoparietal craniectomy with bilateral dural opening), minimizing the risk for selection bias. However, the pertinence of these criteria to routine clinical practice remains unclear. For instance, hemicraniectomy (instead of bi-frontal craniectomy) is often performed for traumatic brain injuries that predominantly involve a single hemisphere. Moreover, it is unclear that most surgeons would perform craniectomies after 15 min of ICP elevation. Likelihood of detection bias is low since the outcomes were determined by examiners who were unaware of the group assignments administered. Handling of attrition and data exclusion are documented in detail. There are issues related to selective reporting since (1) the primary end was altered after an interim analysis and (2) the definition of favorable and unfavorable outcome was based on arbitrary dichotomization of a continuous variable.
Randomized evaluation of surgery with craniectomy for uncontrollable elevation of intracranial pressure (RESCUEicp)
The RESCUEicp study performed by Hutchinson et al. involved 52 centers and 398 patients between 2004 and 2014 [14]. Inclusion criteria were: ages 10 to 65 years, traumatic brain injury with an abnormal CT scan, and intracranial hypertension refractory to first/second tier treatments (defined as ICPs > 25 mmHg for 1 to 12 h). Patients with non-survivable injuries, bilateral fixed and dilated pupils, or coagulopathies were excluded. Patients requiring an operation for evacuation of an intracranial hematoma were not excluded if the bone flap was replaced at the end of the surgery. Patients were randomized to undergo either a unilateral hemicraniectomy or bifrontal craniectomy (with dural opening) plus standard medical care, or standard medical care alone (continued first/second tier ICP therapies, plus addition of barbiturates). Patients assigned to medical therapy were eligible for life-saving decompressive craniectomy. Randomization was stratified based upon study site. The primary outcome was the proportion of patients with favorable GOS-E (defined as > 4 or upper severe disability) 6 months after randomization. Secondary outcomes included GOS-E 12 and 24 months after randomization, 6, 12, and 24-month mortality and quality of life (assessed via the 36-item Short-Form Health Survey in adults and the 10-item Short-Form Health Survey in children), discharge Glasgow Coma Scale (GCS) score, overall ICP control, and time in the ICU and hospital. Study size was pre-determined based on an estimate that 400 patients would be required to detect an increase in the proportion of favorable GOS-E patients from 45% to 60%.
Between 2004 and 2014, 398 patients were randomized: 198 into medical therapy and 202 to decompressive craniectomy. Baseline characteristics of the study participants were comparable across groups, except there were more patients with a history of drug or alcohol abuse in the medical management group (35.2 versus 24.8%, p = 0.02). Seventy-three patients (37.2%) assigned to the medically managed group underwent delayed decompressive craniectomy. Intent-to-treat analysis was performed using ordinal GOS-E. A favorable 6-month GOS-E outcome was found in 42.8% of patients in the surgical group versus 34.6% in the medical group (p = 0.12). This improvement in favorable GOS-E scores with surgery remained at 12 months (45.4 versus 32.4%, p = 0.01). Other notable secondary outcomes include a significantly reduced mortality in the surgical group (30.4% versus 52%, p < 0.01), lower mean ICPs (14.5 mmHg versus 17.1 mmHg, p < 0.001), and less time with ICPs above 25 mmHg (5.0 h versus 17.0 h, p < 0.001). Adverse events occurred in 16.3% of patients in the craniectomy group (adverse events relating to cranioplasties not recorded) versus 9.2% in the medical group (p = 0.03).
We assessed the quality of RESCUEicp using the Cochrane risk of bias tool [13]. The likelihood for selection bias in this study is low given the use of permuted blocks of random sizes. The baseline characteristics of the two arms were comparable. Due to the nature of the study, it was impossible to blind the participants to the intervention. However, given the selection of unconscious patients with ICPs > 25 mmHG, it is unlikely that the patients willingly performed differentially as a result of unblinded clinical intervention. Likelihood of detection bias is low since the outcomes were determined by trained examiners who were unaware of the group assignments. Handling of attrition and data exclusion are documented in detail. Given that a high proportion of patients in the medical management group underwent salvage craniectomy (37.2%), and an intent-to-treat analysis was performed, result reporting is biased toward minimizing the life-preserving impact of decompressive craniectomy.
Use of barbiturate therapy
There is one published RCT study that examined the effect of barbiturates on intracranial hypertension refractory to tier 1 interventions. The study by Eisenberg et al. enrolled 73 patients at 5 centers between 1982 and 1985 [10]. Inclusion criteria were: ages 15–50 years with GCS ≤ 7 and elevated ICPs refractory to tier 1 interventions. Patients who were pregnant, had a GCS score of 3, or had nonreactive pupils were excluded. Eligible patients were randomized to either pentobarbital therapy plus continued tier 1 interventions, or tier 1 interventions alone. In patients randomized to pentobarbital therapy, pentobarbital was discontinued when ICPs < 20 mmHg were achieved for 48 h. Patients with a GCS of 3 or non-reactive pupils were excluded. Patients failing tier 1 interventions were allowed to crossover and receive pentobarbital therapy. Thirty-seven patients were randomized to pentobarbital therapy and 36 patients to continued tier 1 interventions. Baseline characteristics of the two arms were generally comparable. Notably, 26 of the 36 patients assigned to non-pentobarbital treatment crossed over. Endpoints evaluated included sustained ICPs < 20 mmHg for 48 h and 1-month survival. The study revealed that 32.4% of the pentobarbital-treated group achieved ICP control compared to 16.7% of the non-pentobarbital group (p = 0.12). A multiple logistic model accounting for treatment and baseline characteristics demonstrated a positive treatment effect of barbiturates (odds ratio = 2.18, p = 0.02). Furthermore, ICP control was achieved in 85.7% of the crossover patients. Despite the improvement in ICP control, the overall survival of patients in the two cohorts did not significantly differ. The rate of hypotension was modestly increased in the barbiturate group (62 versus 50%).
Insufficient data were included in this article to allow a detailed assessment by the Cochrane risk of bias tool [13]. An important limitation of this study is that the planned sample size was not achieved. As such, inadequate sample size is a major concern in the interpretation of a negative survival association.
Two other RCTs reported that barbiturate therapy did not significantly affect mortality outcome in sTBI patients. Ward et al. enrolled 53 consecutive sTBI patients at a single center between 1979 and 1983 [26]. Inclusion criteria were: sTBI, age greater than 12 years, and an acute intradural hematoma (large enough to warrant surgical decompression) or no mass lesion but a best motor response of abnormal flexion or extension. Exclusion criteria were comorbid hypertension, heart disease, or liver disease. Outcomes of interest included Glasgow Outcome Scale (GOS) score at 1 year, hourly ICPs, incidence of elevated ICP, and mortality from uncontrollable intracranial hypertension. Patients were randomized to prophylactic pentobarbital treatment (n = 27) or no-pentobarbital treatment (n = 26). There was no significant survival difference between the pentobarbital and the control group. However, higher incidence of arterial hypotension was observed in the pentobarbital group relative to the untreated group (54 versus 7%).
In the second study, Schwartz et al. enrolled 59 patients at a single center between 1980 and 1982 [23]. Inclusion criteria were: sTBI, GCS ≤ 7 and ICPs > 25 mmHg for > 125 min. ICP-monitored sTBI patients who did not develop raised ICPs were excluded. Patients with elevated ICPs after intracranial hematoma evacuation and patients with elevated ICPs in the absence of a hematoma were separately randomized to initial treatment with mannitol or pentobarbital followed by the second drug as needed. Outcomes studied included failure to control ICPs, 3-month survival, and quality of life for surviving patients. For patients with intracranial hypertension following hematoma evacuation, there was no significant difference in mortality between the pentobarbital and mannitol groups (40 versus 43%). For patients with intracranial hypertension without a hematoma, there was a higher mortality rate in the pentobarbital group (77% versus 41%). In both cohorts, ICP control was worse with pentobarbital.
For the Ward and Schwartz studies, insufficient data were included to allow detailed assessment by the Cochrane risk of bias tool [13]. Notable limitations of these studies include the absence of a power calculation to determine necessary sample size, failure to designate primary versus secondary outcomes, and lack of appropriate statistical analyses.
Discussion
Despite the non-zero risk of ICP monitoring [8, 9], and variable neurosurgeon adherence to strict monitoring criteria based on individual patient factors [24], current treatment guidelines clearly reflect the importance of ICP control as it pertains to the management of sTBI patients [3, 4, 12, 22]. While the inverse relation between cerebral perfusion and intracranial pressure is overly simplified, it generally holds true. Also, the association between poor clinical outcome and uncontrolled intracranial hypertension in sTBI patients remains undisputed. In this context, the BEST-TRIP results should not be mistaken as an indictment of the importance of ICP management. Instead, this study demonstrates that ICP management based on diligent clinical observation achieves outcomes comparable to those based on direct ICP monitoring.
Two other findings in BEST-TRIP are worth noting. The increased utilization of hyperosmolar therapy and hyperventilation in the non-ICP monitor arm suggests tendencies of treating physicians to overestimate ICP based on clinical and radiographic findings, in the absence of direct ICP measurement. Additionally, the increased acute-care length for patients in the ICP-monitoring arm suggests that overreliance on ICP measurement in the subacute phase of injury may prolong intensive care stay. To the extent that patient outcomes were comparable between cohorts despite these differences, these findings suggest opportunities for cost-effective improvements in resource allocation rather than for meaningful gains in clinical outcome.
In DECRA and the barbiturate RCTs, ICP control was not associated with survival improvement. On the other hand, ICP control was associated with improved survival in RESCUEicp. Our synthesis of this literature is that control of ICP is, by itself, insufficient for optimizing clinical outcome following sTBI. While there is no doubt that intracranial hypertension and consequent intracranial hypoperfusion is a key factor in secondary brain injury after sTBI, the traumatic injury itself likely triggers biologic processes, such as excitotoxic injury or autoregulatory failure, that exacerbate the deleterious effects of the initial insult. Until these mechanisms are mitigated, the severity of the initial TBI will likely remain a primary determinant of clinical outcome.
In the RCTs reviewed, the most striking effect of decompressive craniectomy appeared to be lowering the proportion of patients who died while increasing the proportion of vegetative or severely disabled patients. Approximately 70% of sTBI patients become variably dependent on others for care irrespective of whether decompressive craniectomy is performed. If one sets the bar at the level of functional independence, as we should, then the data raise serious questions pertaining to the utility of decompressive craniectomy in the setting of sTBI. The major issue is that it is impossible to predict the benefit of craniectomy on an individual level. Further confounding the issue is the observation that craniectomy is associated with an approximately 16% risk of surgical morbidity.
The aggregate of the RCT literature suggests that a significant proportion of patients surviving sTBI remain severely disabled, raising ethical considerations in terms of informed consent and societal responsibility. By definition, informed consent cannot be secured from sTBI patients themselves. Treatment decisions are often based on consent of available surrogates or on life preservation in a crisis situation. However, given that the outcome is likely one of significant physical disability with associated psycho-social challenges, whether the sTBI patients would opt to live under such circumstances remains an open question. In a survey of patients who survived catastrophic neurologic injury with severe disability, nearly 50% of the interviewed patients reported that they would not have opted for life-preserving measures [5]. What is the responsibility of our society to these patients?
It is clear that health care decisions should not be based purely on economic calculations or a utilitarian framework. Compassion, preservation of life, and maximization of human potential are fundamental values shared by most societies and remain ideals to which health care providers aspire. The difficulty arises when well-intended efforts are not bolstered by knowledge that genuinely affects clinical outcome. Investment in the ascertainment of that knowledge should be a clear priority. Until such knowledge is attained, thoughtful consideration should be devoted to the minimization of unnecessary human suffering.
References
Agrawal A, Coronado VG, Bell JM, Baisakhiya N, Kakani A, Galwankar S, Dwivedi S (2014) Characteristics of patients who died from traumatic brain injury in two rural hospital emergency Departments in Maharashtra, India, 2007-2009. Int J Crit Illn Inj Sci 4:293–297
Andrews PJD, Sinclair HL, Rodriguez A, Harris BA, Battison CG, Rhodes JKJ, Murray GD, Eurotherm Trial C, Noble D, Galt S, Taylor J, Addison J, Wallis C, Paterson R, Harris G, Mullan B, Quinn V, Bannon L, Gordon A, Templeton M, Wilson R, Thomas E, McMillan H, Tantam K, Gratrix A, Smith N, Martinson V, Barrera-Groba C, Littlejohn I, Spurling G, Hopkins P, Casboult S, Hadfield D, McKinlay J, Beardow Z, Elliot S, Jain R, Bellini A, McCluskey T, Harvey D, Chikhani M, Bolland A, Waldmann C, Jacques N, Prowse H, Turnbull D, Eapen G, Birchall K, Verma V, Creary T, Niebrzegowska E, Owen T, Baldwin J, Williams A, Thompson C, Salt R, Cartlidge D, Vincent A, Calder V, Scott C, Ferris P, Roberts J, Evans T, Burgess N, Della Torre V, Mellinghoff J, Stotz M, Hauer V, Ochelli-Okpue A, McMahon C, Tweedie I, Murray L, Bassford C, Ward G, McCauley M, Wise M, Palmer N, Cole J, Damas F, Xavier N, Duliere G-L, Simoens G, Biston P, Joosten A, Simon M, Antoine A, Zieppen B, Bulpa P, Dive A, Bouhon S, Taccone F, Vincent J-L, Durand D, Spapen H, Troubleyn J, Van Malderen C, Toome V, Sillaots P, Koger I, Stuttmann R, Jakubetz J, Langer S, Michalia M, Clouva-Molyvdas P-M, Vassiliadis I, Nanas S, Douka L, Dimopolous S, Pneumatikos I, Dragoumanis C, Kouliatsis G, Nakos G, Kostanti E, Zakynthinos E, Makris D, Palli E, Koukoulitsios G, Tsikritsaki K, Kalogeromitros A, Nagy E, Lampiri C, Valtoy M, Barzo P, Kis D, Fulop B, Gupta D, Bindra A, Breen D, Barry J, Neau E, Spoto M, Fusilli N, Malossini S, Antonelli M, Caricato A, Tersali A, Seabra F, Aragao I, Antunes R, Petrikov S, Titova J, Solodov A, Al-Jabbary A, Deeb A, Richi H, del Campo MM, Casado JMT, Perez EB, Perez AZ, Diez MA, Echeverri SO, Blesa A, Romero F, Sanchez M, van der Jagt M, Haitsma I, van Duijn D, Dennesen P, Koole M, Krishnareddy K, Hegazi M, Sharma BS (2015) Hypothermia for intracranial hypertension after traumatic brain injury. N Engl J Med 373:2403–2412
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons (2007) Guidelines for the management of severe traumatic brain injury. J Neurotrauma 24(Suppl 1):S1–106
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, Rubiano AM, Shutter L, Tasker RC, Vavilala MS, Wilberger J, Wright DW, Ghajar J (2017) Guidelines for the Management of Severe Traumatic Brain Injury, fourth edition. Neurosurgery 80:6–15
Carter BS, Ogilvy CS, Candia GJ, Rosas HD, Buonanno F (1997) One-year outcome after decompressive surgery for massive nondominant hemispheric infarction. Neurosurgery 40:1168–1175 discussion 1175-1166
Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, Petroni G, Lujan S, Pridgeon J, Barber J, Machamer J, Chaddock K, Celix JM, Cherner M, Hendrix T, Global Neurotrauma Research G (2012) A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 367:2471–2481
Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, D’Urso P, Kossmann T, Ponsford J, Seppelt I, Reilly P, Wolfe R, DECRA Trial Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group (2011) Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med 364:1493–1502
Cremer OL, van Dijk GW, van Wensen E, Brekelmans GJF, Moons KGM, Leenen LPH, Kalkman CJ (2005) Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med 33:2207–2213
Dang Q, Simon J, Catino J, Puente I, Habib F, Zucker L, Bukur M (2015) More fateful than fruitful? Intracranial pressure monitoring in elderly patients with traumatic brain injury is associated with worse outcomes. J Surg Res 198:482–488
Eisenberg HM, Frankowski RF, Contant CF, Marshall LF, Walker MD (1988) High-dose barbiturate control of elevated intracranial pressure in patients with severe head injury. J Neurosurg 69:15–23
El-Matbouly M, El-Menyar A, Al-Thani H, Tuma M, El-Hennawy H, AbdulRahman H, Parchani A, Peralta R, Asim M, El-Faramawy A, Zarour A, Latifi R (2013) Traumatic brain injury in Qatar: age matters—insights from a 4-year observational study. ScientificWorldJournal 2013:354920
Haddad SH, Arabi YM (2012) Critical care management of severe traumatic brain injury in adults. Scand J Trauma Resusc Emerg Med 20:12
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Group CBM, Group CSM (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J, Anderson I, Bulters DO, Belli A, Eynon CA, Wadley J, Mendelow AD, Mitchell PM, Wilson MH, Critchley G, Sahuquillo J, Unterberg A, Servadei F, Teasdale GM, Pickard JD, Menon DK, Murray GD, Kirkpatrick PJ, Collaborators RT (2016) Trial of Decompressive Craniectomy for traumatic intracranial hypertension. N Engl J Med 375:1119–1130
Jalloh I, Carpenter KL, Helmy A, Carpenter TA, Menon DK, Hutchinson PJ (2015) Glucose metabolism following human traumatic brain injury: methods of assessment and pathophysiological findings. Metab Brain Dis 30:615–632
Lee KK, Seow WT, Ng I (2006) Demographical profiles of adult severe traumatic brain injury patients: implications for healthcare planning. Singap Med J 47:31–36
Marshall LF, Marshall SB, Klauber MR, Clark MB, Eisenberg HM, Jane JA, Luerssen TG, Marmarou A, Foulkes MA (1991) A new classification of head injury based on computerized tomography. J Neurosurg 75(Suppl 1):S14–S20
Martini RP, Deem S, Treggiari MM (2013) Targeting brain tissue oxygenation in traumatic brain injury. Respir Care 58:162–172
Melhem S, Shutter L, Kaynar A (2014) A trial of intracranial pressure monitoring in traumatic brain injury. Crit Care 18:302
Romner B, Grände PO (2013) Traumatic brain injury: intracranial pressure monitoring in traumatic brain injury. Nat Rev Neurol 9:185–186
Rutland-Brown W, Langlois JA, Thomas KE, Xi YL (2006) Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil 21:544–548
Saiki RL (2009) Current and evolving management of traumatic brain injury. Crit Care Nurs Clin North Am 21:549–559
Schwartz ML, Tator CH, Rowed DW, Reid SR, Meguro K, Andrews DF (1984) The University of Toronto head injury treatment study: a prospective, randomized comparison of pentobarbital and mannitol. Can J Neurol Sci 11:434–440
Talving P, Karamanos E, Teixeira PG, Skiada D, Lam L, Belzberg H, Inaba K, Demetriades D (2013) Intracranial pressure monitoring in severe head injury: compliance with brain trauma foundation guidelines and effect on outcomes: a prospective study. J Neurosurg 119:1248–1254
Traumatic Brain Injury in the United States (2010) Centers for Disease Control and Prevention. Accessed June 15th, 2016. Available from: http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf
Ward JD, Becker DP, Miller JD, Choi SC, Marmarou A, Wood C, Newlon PG, Keenan R (1985) Failure of prophylactic barbiturate coma in the treatment of severe head injury. J Neurosurg 62:383–388
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethics approval/informed consent
This literature review did not involve direct human procedures. This article does not contain any studies with human participants performed by any of the authors. For this type of study formal consent is not required.
Electronic supplementary material
ESM 1
(DOCX 58 kb)
Rights and permissions
About this article
Cite this article
Abraham, P., Rennert, R.C., Gabel, B.C. et al. ICP management in patients suffering from traumatic brain injury: a systematic review of randomized controlled trials. Acta Neurochir 159, 2279–2287 (2017). https://doi.org/10.1007/s00701-017-3363-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3363-1