Abstract
Retroclival epidural haematoma (REDH) has been reported infrequently. It is a rare entity which is probably underdiagnosed. It is most commonly seen in the paediatric population and is generally associated with high-velocity injuries. We report three cases of paediatric patients diagnosed with REDHs: two of them secondary to high-energy trauma related to a motor-vehicle accident and the other a low-energy trauma after a slip while playing football. All three patients were managed conservatively by cervical immobilisation with favourable outcome. REDH is probably underdiagnosed by computed tomography scan. When the suspicion is high, sagittal reconstructions or magnetic resonance imaging should be considered to confirm the diagnosis. Usually, it is related to hyperflexion or hyperextension cervical injuries secondary to motor vehicle accident. However, it can also be observed in milder injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and importance
Retroclival epidural haematoma (REDH) is a particularly rare entity, making up an estimated 1.2–12.9% of all epidural haematomas [1]. Only a few isolated cases and small case series have been reported in the literature, with the largest being of eight patients [29]. The vast majority of REDHs are diagnosed in children, although some have been reported in adults. It has been described in adults in relation to cranioencephalic trauma [9, 25], as secondary to decompressive craniectomy for cerebellar infarction [4] and to pituitary apoplexy [2, 11]. Cho et al. [5] reported a unique case of spontaneous epidural retroclival haematoma. Silvera et al. [26] reported the association of the REDH with abusive head trauma, being the retroclival collections especially common in these patients, mainly subdural haematomas. It typically develops after a high-energy trauma, with almost all the patients being a victim of a motor vehicle crash as a pedestrian, bicyclist or passenger in the vehicle [29]. Only one REDH has been reported in relation to a minor head trauma. The patient suffered a hyperextension injury after a fall forward while running [13]. These haematomas are probably underdiagnosed by computed tomography (CT) scan because of artefacts caused by cranial bones, like other lesions in the posterior fossa. For this reason, sagittal reconstructions using multi-detector CT and magnetic resonance imaging (MRI) might be considered if REDH is suspected [3, 12, 23, 27, 29].
Usually, the neurological symptoms of REDH are due to cranial nerve involvement on one or both sides. The lesion might be a result of the trauma, causing the compression or inflammation of the cranial nerve. The abducens nerve is the most commonly injured, probably because of its longest intracranial course [3, 15, 21, 29]. Glossopharyngeal, hypoglossal, optic, oculomotor and trigeminal nerves can also be involved [29]. Rarely, hemiparesia or paraparesia in upper or lower limbs or centromedullary syndrome might be the clinical presentation [12].
Case reports
Case 1
A 7-year-old boy suffered a hyperextension injury to his neck caused by occipital trauma after slipping while playing soccer. He was brought to the emergency department with drowsiness within 1 h of the incident. On clinical examination, his vitals were stable. Witnesses reported a transient loss of consciousness with progressive recovery. He did not develop nausea or vomiting. His Glasgow Coma Scale (GCS) score was E3V5M6. Neurological examination revealed diplopia caused by right abducens palsy and right hemiparesis 4/5.
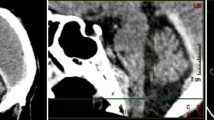
The patient underwent CT scan of the head, which showed an REDH with brainstem compression (Fig. 1a–c). He was immobilised with a Philadelphia brace and was transferred to the paediatric intensive care unit for close neurological monitoring. An MRI scan of the head and cervical spine was performed 2 days later. It confirmed an REDH and demonstrated a slight decrease in the size of the haematoma (Fig. 1d). The patient improved progressively in diplopia and weakness over one week and was discharged.
Axial (a, b) and sagittal (c) CT scan revealing a well-defined heterogeneous hyperdense collection from midpons to odontoid process. Its maximum thickness is 14 mm. No fractures are observed in clivus and craniovertebral junction. T2-weighted sagittal MRI (d) showing a hypodense lesion in contact with pontomedullary junction without compressing it. The diagnosis of the mass is consistent with an epidural retroclival haematoma
Flexion and extension cervical spine X-rays were performed 2 weeks after discharge. They demonstrated stable alignment at the craniocervical junction (CVJ) and the Philadelphia brace was removed. On 6-month follow-up at the outpatient clinic, the patient was found to be completely asymptomatic.
Case 2
A 9-year-old boy was admitted to the emergency department after being involved in a motor-vehicle accident. The patient was sitting in the back seat with his brother (patient of case 3) wearing the seat belt. On examination, he was sleepy with a GCS score of 14 and no other neurological symptoms. He complained of headache accompanied by nausea and vomiting.
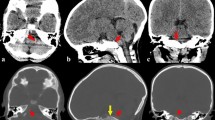
Brain CT scan revealed an REDH, left peri-rolandic contusion and atlantoaxial rotatory subluxation (type I-II Fielding and Hawkins classification) with no odontoid process fracture. The craneocervical instability was treated conservatively with cervical brace (Philadelphia). He developed progressive diplopia caused by a complete VI nerve palsy on the right side and VI nerve paresis on the left side. Brain and cervical spine MRI was performed on the second day and confirmed the REDH (Fig. 2) and the atlantoaxial rotatory subluxation. He was discharged on 15th day post admission with partial VI right nerve palsy.
Flexion and extension cervical spine X-ray did not demonstrate any craniocervical junction instability and cervical collar was discontinued. On 6-month follow-up at the outpatient clinic the right VI nerve palsy had almost resolved. There was no other neurological deficit. Repeat imaging showed resolution of the haematoma.
Case 3
A 5-year-old boy was brought to the emergency department after suffering the same accident as case 2. On arrival he was haemodynamically unstable with a GCS score of 8 with normoreactive and isochoric pupils. The patient underwent orotracheal intubation and was transferred for CT scan (Fig. 3a). He was admitted to the paediatric intensive care unit where his mental status improved and the endotracheal tube was removed. On clinical examination, he presented a GCS of 12 (E3, V3, M6) with right VI nerve complete palsy. Conservative treatment with a cervical brace (Philadelphia) was decided.
Brain and cervical spine MRI obtained 2 days after admission showed right frontotemporal and parietal microcontusions and an REDH haematoma (Fig. 3b). There were no lesions in the cervical spine so the cervical brace was removed. During his stay the patient improved in sensorium and his diplopia. He was discharged on day 17 after admission.
On 6-month follow-up, he had recovered partially in his VI nerve palsy. There was no other neurological deficit. Control MRI was performed showing complete resolution of the haematoma.
Discussion
REDH is an uncommon entity that typically affects the paediatric population. The first case was reported by Coleman et al. [6] in 1941. Since then, 33 paediatric cases of epidural haematoma have been described in the literature (Table 1). Most REDHs are associated with a motor-vehicle accidents with high-energy trauma [29]. Apart from our first case, to our knowledge only one REDH caused by a minor head trauma has been reported previously. [13] Despite its relation with cranioencephalic trauma and polytrauma, no direct relation has been observed between GCS scores on admission and neurological outcome in these patients [15, 29]. Tubbs et al. [29] have reported the largest series of retroclival epidural haematoma and they found no correlation between haematoma size and presenting symptoms.
Patients 2 and 3 were both diagnosed with REDH after suffering a motor-vehicle crash as passengers sitting in the rear seats. To our knowledge, this is the first time that two cases of epidural retroclival haematoma are reported after suffering the same traffic accident. Based on our experience and previous studies this pathology is likely to be underdiagnosed [29].
Pathophysiology
The pathophysiology of the formation of a REDH remains controversial [3, 29]. It has been suggested that the unique characteristics of the craniovertebral junction in children predispose them to the formation of these haematomas [29]. The incomplete development of paediatric bones [12], smaller occipital condyles [3, 21], horizontally oriented atlanto-occipital joints [29] and an increased elasticity of the ligaments [28] accounts for relative hypermobility of the paediatric craniovertebral junction. The tectorial membrane can be disrupted from the clivus by hyperflexion or hyperextension injuries and result in vascular lesions and blood accumulation in the retroclival area (basilar venous plexus, dorsal meningeal branch of meningohypophyseal trunk) [3, 21, 23, 29]. Atlanto-axial [22] and atlanto-occipital dislocations [24, 30] or clivus and cranial base fractures have been reported as the causes of REDH [14]. Nevertheless, a fracture of the clivus may not be accompanied with an epidural retroclival haematoma [7]. In fact, most of haematomas result from ligament injury.
Treatment
In the literature, the majority of the patients have been managed conservatively with a cervical brace [15, 21, 28, 29]. Conservative management results in good recovery in the majority of cases if there is no progressive neurological deterioration. Evacuation of the haematoma can be considered in cases with progressive brainstem compression and fusion in CVJ instability [15, 29]. Surgery has been required in four cases: two transoral decompressions [16] and two posterior decompressions [10, 20, 24]. Atlanto-occipital dislocation must be ruled out and may required fusion if unstable [15, 28, 29]. Prognosis has remained excellent in the majority of cases reported in the literature [21, 29]. The deaths are usually associated with the patients’ comorbidities.
Conclusions
Traumatic REDH is a rare entity and likely to be underdiagnosed with CT. When the suspicion is high, sagittal reconstructions or MRI should be considered to confirm the diagnosis. Usually, this haematoma is related to sudden hyperflexion or hyperextension injuries at the CVJ sustained in a traffic accident. However, it has been observed in milder injuries. Injury of the occipito-atlanto-axial complex should be discarded by cervical CT to detect bone lesions and cervical MRI looking for inflammatory changes in STIR sequence. Classically, the VI nerve palsy is the most frequent symptom. Conservative management is the treatment of choice in the majority of cases and it is associated with good prognosis.
The next of kin has consented to submission of this case report to the journal.
References
Agrawal D, Cochrane DD (2006) Traumatic retroclival epidural hematoma—a pediatric entity? Childs Nerv Syst 22(7):670–673
Azizyan A, Miller JM, Azzam RI, Maya MM, Famini P, Pressman BD et al (2015) Spontaneous retroclival hematoma in pituitary apoplexy: case series. J Neurosurg 123(3):808–812
Becco de Souza R, Brasileiro de Aguiar G, Sette Dos Santos ME, Acioly MA (2011) Retroclival epidural hematoma in a child affected by whiplash cervical injury: a typical case of a rare condition. Pediatr Neurosurg 47(4):288–291
Calli C, Katranci N, Guzelbag E, Alper H, Yunten N (1998) Retroclival epidural hematoma secondary to decompressive craniectomy in cerebellar infarction: MR demostration. J Neuroradiol 25(3):229–232
Cho CB, Park HK, Chough CK, Lee KJ (2009) Spontaneous bilateral supratentorial subdural and retroclival extradural hematomas in association with cervical epidural venous engorgement. J Korean Neurosurg Soc 46(2):172–175
Coleman CC, Thompson JL (1941) Extradural hemorrhage in the posterior fossa. Surgery 10:985–990
Corradino G, Wolf AL, Mirvis S, Joslyn J (1990) Fractures of the clivus: classification and clinical features. Neurosurgery 27:592–596
Dal Bo S, Cenni P, Marchetti F (2015) Retroclival hematoma. J Pediatr 166(3):773
Datar S, Daniels D, Wijdicks EF (2013) A major pitfall to avoid: retroclival hematoma due to odontoid fracture. Neurocrit Care 19(2):206–209
Fuentes S, Bouillot P, Dufour H, Grisoli F (2000) Occipital condyle fractures and clivus epidural hematoma: case report. Neurochirurgie 46:563–567
Goodman JM, Kuzma B, Britt P (1997) Retroclival hematoma secondary to pituitary apoplexy. Surg Neurol 47(1):79–80
Guillaume D, Menezes AH (2006) Retroclival hematoma in pediatric population. Report of two cases and rewiew of the literature. J Neurosurg 105(4 suppl):321–325
Itshayek E, Goldman J, Rosenthal G, Chikoya L, Gomori M, Segal R (2006) Extradural hematoma of the clivus, not limited to the severely injured patient: case report and review of the literature. J Trauma 60(2):417–420
Kurosu A, Amano K, Kubo O et al (1990) Clivus epidural hematoma: case report. J Neurosurg 72:660–662
Kwon TH, Joy H, Park YK, Ching HS (2008) Traumatic retroclival epidural hematoma in a child—case report. Neurol Med Chir (Tokyo) 48:347–350
Marks SM, Paramaraswaren RN, Johnston RA (1997) Transoral evacuation of a clivus extradural haematoma with good recovery: a case report. Br J Neurosurg 11:245–247
McDougall CM, Sankar T, Mehta V, Pugh JA (2011) Pediatric traumatic retroclival epidural hematoma. Can J Neurol Sci 38(2):338–340
Mizushima H, Kobayashi N, Sawabe Y, Hanakawa K, Jinbo H, Iida M et al (1998) Epidural hematoma of the clivus. Case report. J Neurosurg 88(3):590–593
Momjian S, Dehdashti AR, Kehrli P, May D, Rilliet B (2003) Occipital condyle fractures in children. Case report and review of the literature. Pediatr Neurosurg 38(5):265–270
Muller JU, Piek J, Kallwellis G, Stenger RD (1998) Prepontine epidural hemorrhage. Zentralbl Neurochir 59:185–188
Nguyen HS, Shabani S, Lew S (2016) Isolated traumatic retroclival hematoma: case report and review of literature. Childs Nerv Syst 32(9):1749–1755
Orrison WW, Rogde S, Kinard RE, Williams JE, Torvik A, Sackett JF et al (1986) Clivus epidural hematoma: a case report. Neurosurgery 18(2):194–196
Paterakis KN, Karantanas AH, Hadjigeorgiou GM, Anagnostopoulos V, Karavelis A (2005) Retroclival epidural hematoma secondary to a longitudinal clivus fracture. Clin Neurol Neurosurg 108(1):67–72
Papadopoulos SM, Dickman CA, Sonntag VK, Rekate HL, Spetzler RF (1991) Traumatic atlantoocipital dislocation with survival. Neurosurgery 28(4):574–579
Pérez-Bovet J, Garcia-Armengol R, Martín FS (2013) Traumatic epidural retroclival hematoma with odontoid fracture and cardiorespiratory arrest. Spinal Cord 51(12):926–928
Silvera VM, Danehy AR, Newton AW, Stamoulis C, Carducci C, Grant PE et al (2014) Retroclival collections associated with abusive head trauma in children. Pediatr Radiol 44(Suppl 4):S621–S631
Suliman HM, Merx HL, Wesseling P, van der Sluijs B, Vos PE, Thijssen HO (2001) Retroclival extradural hematoma is a magnetic resonance imaging diagnosis. J Neurotrauma 18(11):1289–1293
Tahir MZ, Quadri SA, Hanif S, Javed G (2011) Traumatic retroclival epidural hematoma in pediatric patient—case report and review of literature. Surg Neurol Int 2:78
Tubbs RS, Griessenauer CJ, Hankinson T, Rozzelle C, Wellons JC III, Blount JP (2010) Retroclival epidural hematomas: a clinical series. Neurosurgery 67(2):404–406
Vera M, Navarro R, Esteban E, Costa JM (2007) Association of atlanto-occipital dislocation and retroclival haematoma in a child. Childs Nerv Syst 23(8):913–916
Yang BP (2003) Traumatic retroclival epidural hematoma in a child. Pediatr Neurosurg 39(6):339–340
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article. We have no conflicts of interest to disclose. There has not been any financial disclosure.
Ethical approval
Due to the cases were managed conservatively neither a statement regarding IRB/ethics committee approval were required at our institution. No identifiable protected health information of any person was included in the manuscript.
Rights and permissions
About this article
Cite this article
Zabalo, G., Ortega, R., Díaz, J. et al. Retroclival epidural haematoma: a diagnosis to suspect. Report of three cases and review of the literature. Acta Neurochir 159, 1571–1576 (2017). https://doi.org/10.1007/s00701-017-3214-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3214-0