Abstract
Background
Symptomatic lumbar spinal stenosis (LSS) is the most common reason for lumbar surgery in the elderly. There is growing evidence that decompressive surgery offers an advantage over non-surgical management for selected patients with persistent severe symptoms. Based on treatment traditions, open laminectomy has been the gold standard surgical treatment, but various other surgical and non-surgical treatments for LSS are widely used in clinical practice. Therefore, we conducted a survey study to capture potential diversities in surgeons’ management of LSS in Norway.
Methods
All spine surgeons in Norway were contacted by e-mail and asked to answer a 20-item questionnaire by using an Internet-based survey tool. We asked eight questions about the respondent (gender, surgical specialty, workplace, experience, number of surgeries performed per year, use of magnification devices) and 12 questions about different aspects of the surgical treatment of LSS (indication for surgery and preoperative imaging, different surgical techniques, clinical outcome).
Results
The questionnaire was answered by 51 spine surgeons (47% response rate). The preferred surgical technique for LSS in Norway is microdecompression via a unilateral approach and crossover technique, followed by microdecompression via a bilateral approach. Other techniques are not much used in Norway.
Conclusions
Most Norwegian spine surgeons use minimally invasive decompression techniques in the surgical treatment of LSS, and unilateral microsurgical decompression with crossover decompression is the preferred technique. Where evidence is lacking (e.g., fusion procedures), there is a larger variation of opinions and preferred procedures among Norwegian spine surgeons.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Symptomatic lumbar spinal stenosis (LSS) is the most common reason for lumbar surgery in the elderly [5]. There is growing evidence that decompressive surgery offers an advantage over non-surgical management for selected patients with persistent severe symptoms [18]. Improvement in radiating pain, neurogenic claudication, functional status, and quality of life are common treatment goals. Based on treatment traditions, open laminectomy has been the gold standard surgical treatment. Recently, the equivalence between microsurgical decompression and open laminectomy has been demonstrated [12], but various other surgical and non-surgical treatments for LSS are widely used in clinical practice [3, 4, 12].
We conducted a survey study to capture potential diversities in surgeons’ management of LSS in Norway and all Norwegian spine surgeons, both orthopedic surgeons and neurosurgeons, were invited.
Methods
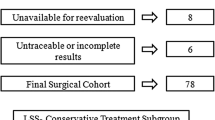
We identified all orthopedic surgeons and neurosurgeons (n = 108) treating patients with LSS in 2015 via the Norwegian Orthopedic Society, the Norwegian Neurosurgical Society and the Norwegian Spine Society. All spine surgeons were contacted by e-mail and asked to answer a 20-item questionnaire by using an Internet-based survey tool (SelectSurvey.NETTM, version 4.131.000, ClassApps, Kansas City, MO, USA). Those who did not respond within 2 weeks were sent a reminder. We asked eight questions about the respondent (gender, surgical specialty, workplace, experience, number of surgeries performed per year, use of magnification devices) and 12 questions about different aspects of the surgical treatment of LSS (indication for surgery and preoperative imaging, different surgical techniques, clinical outcome).
Statistical analysis was performed by using IBM Statistical Package for the Social Sciences (SPSS) Statistics (version 21) and statistical significance level was set to p < 0.05. All tests were two-sided. Normal distribution was assessed with Q–Q plots. Data were analyzed with Pearson’s Chi-square test.
Results
Surgeons’ characteristics
The questionnaire was answered by 51 spine surgeons (47% response rate) of whom 31 were neurosurgeons and 20 orthopedic surgeons. Two surgeons declined to answer the questionnaire and 55 did not respond to the inquiry at all. Among the respondents, 55% had more than 10 years of working experience within the field of spinal surgery, and 76% performed more than 50 lumbar surgeries per year. Further, 82% performed more than 20 non-instrumented decompression surgeries for LSS per year, but only 28% performed more than 20 fusion surgeries per year. Only one surgeon did not use a magnification device, 89% used a microscope, and 9% used surgical loupes. There were more orthopedic spine surgeons performing more than ten fusion surgeries for LSS (94 vs. 25%; p = 0.000) and more neurosurgeons working at university hospitals (94 vs. 40%; p = 0.000). There were no significant differences in respondent characteristics between orthopedic and neurosurgical survey respondents regarding gender, years of experience, surgeries performed per year, and preferred magnification device. The respondents’ characteristics are presented in Table 1.
Indication for surgery and preoperative imaging
Only 11% of surgeons considered a conservative treatment attempt as an absolute requirement before setting the indication for surgery. Many surgeons considered conservative treatment in patients with minor or moderate symptoms (64%). In patients with minor or moderate stenosis on imaging studies, but more severe clinical presentation, 34% of surgeons recommended conservative treatment. All surgeons assessed preoperative imaging themselves; however, various imaging evaluation techniques for LSS were used and morphological assessment was preferred to quantitative measures (Fig. 1). The important factors influencing surgeons’ decision-making are presented in Fig. 2.
Surgical techniques
As seen in Table 2, the preferred surgical technique for LSS in Norway is microdecompression via a unilateral approach and crossover technique, followed by microdecompression via a bilateral approach. Hemilaminectomy, laminectomy, laminarthrectomy, spinous process osteotomy, indirect decompression via interspinous process device, and endoscopic decompression are surgical techniques that are not much used in Norway. The surgeons also rated the perceived effectiveness and the perceived complication risk with the various techniques. The most popular operation techniques were also the ones with highest perceived effectiveness. Thirty-seven surgeons performed fusion surgeries for LSS, and their opinions on indication for fusion surgery in patients with LSS are presented in Fig. 3. In total, 47% of the respondents performed open fusion procedures. Among the respondents, 41% performed mini-open procedures and 22% performed percutaneous techniques. The preferred fusion techniques are presented in Fig. 4.
Clinical outcome
The surgeons’ answers about the estimated percentages of successfully operated patients are presented in Fig. 5. Figure 6 shows assumed predictors for negative outcome after surgery for LSS.
Discussion
This survey reflects on many aspects of the current surgical management of LSS in Norway. There were basically no differences between orthopedic and neurosurgical spine surgeons besides the facts that orthopedic spine surgeons performed significantly more fusion procedures and more neurosurgical spine surgeons are working at university hospitals.
Norwegian spine surgeons seem to be quite stringent when considering surgical treatment for LSS, and this is in concordance with results from randomized trials [7]. Most Norwegian spine surgeons do require a conservative treatment attempt before considering surgery for LSS. For a surgeon, there are several ways to assess preoperative imaging; both surface measurements and morphology are evaluated. Norwegian spine surgeons, like other European spine surgeons, are influenced by the morphological appearance of the spinal canal on imaging studies [15], but the severity of symptoms seems to be slightly more important than imaging findings when considering surgical treatment [2, 10].
Both open and microsurgical techniques are used in Norway, however unilateral crossover microdecompression has become the preferred approach whereas open procedures such as laminectomy are less used. Two smaller randomized controlled trials [9, 17] and a large observational study [12] have shown that in the treatment of LSS, microdecompression is equivalent to open laminectomy. Lumbar instrumented fusion surgery is usually considered when segmental instability or spondylolisthesis are present in addition to LSS, whereas degenerative disc disease and low back pain are not common indications for fusion surgery in Norway [8]. Unlike in decompression procedures, there is a larger variation in the use of different fusion procedures in Norway, with posterolateral lumbar fusion and transforaminal lumbar interbody fusion being the most popular techniques. There is also larger variation in the preferred approach when fusion is added to decompression, both open, mini-open, and percutaneous techniques are used. Recently published research on the (un)necessity of adding fusion to decompression in patients with LSS with or without low-grade spondylolisthesis was not available at the time point of our survey [6].
Surgical treatment with decompression of the neural elements within the spinal canal is considered to be a very effective treatment modality for patients with LSS [18]; between 50 and 80% of surgically patients experience less pain and functional improvement [13, 16]. However, there is a risk of deterioration after surgical treatment and a recent study identified younger age, smoking, comorbidity, and previous surgery as risk factors for postoperative deterioration [11]. According to our survey, it seems that Norwegian spine surgeons are aware of these risk factors.
A similar survey on practice variations was conducted among Dutch spine surgeons and the results showed a larger variety in the treatment of LSS [14]. This may be due to the evolving evidence in the last years as the Dutch survey was performed 5 years earlier than our study.
Strengths and limitations
The study results have to be interpreted with caution, as only 47% of all Norwegian spinal surgeons answered the questionnaire. The survey response rate is similar to both the Dutch LSS survey [14] and other Web-based surveys [1]. The fact that there were more neurosurgeons working at university hospitals is due to the fact that all Norwegian neurosurgical departments are located at university hospitals, whereas orthopedic departments can be found at both university and other hospitals.
Conclusions
Most Norwegian spine surgeons use minimally invasive decompression techniques in the surgical treatment of LSS, and unilateral microsurgical decompression with crossover decompression is the preferred technique. Where evidence is lacking (e.g., fusion procedures) there is a larger variation of opinions and preferred procedures among Norwegian spine surgeons.
References
Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, Samuel S, Ghali WA, Sykes LL, Jette N (2015) Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 15:32
de Schepper EI, Overdevest GM, Suri P, Peul WC, Oei EH, Koes BW, Bjerma-Zeinstra SM, Luijsterburg PA (2013) Diagnosis of lumbar spinal stenosis: an updated systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 38(8):E469–81
Delitto A, Piva SR, Moore CG, Welch WC (2015) Surgery versus nonsurgical treatment of lumbar spinal stenosis. Ann Intern Med 163(5):397–8
Deyo RA (2010) Treatment of lumbar spinal stenosis: a balancing act. Spine J 10(7):625–7
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303(13):1259–65
Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, Ohagen P, Michaelsson K, Sanden B (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374(15):1413–23
Kovacs FM, Urrutia G, Alarcon JD (2011) Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: a systematic review of randomized controlled trials. Spine (Phila Pa 1976) 36(20):E1335–51
Mannion AF, Brox JI, Fairbank JC (2013) Comparison of spinal fusion and nonoperative treatment in patients with chronic low back pain: long-term follow-up of three randomized controlled trials. Spine J 13(11):1438–48
Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ (2014) Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine 21(2):179–86
Moojen WA, Schenck CD, Nijeholt GJ, Jacobs WC, Van der Kallen BF, Arts MP, Peul WC, Vleggeert-Lankamp CL (2015) Preoperative MR imaging in patients with intermittent neurogenic claudication: relevance for diagnosis and prognosis. Spine (Phila PA 1976). doi:10.1097/BRS.0000000000001301
Nerland US, Jakola AS, Giannadakis C, Solheim O, Weber C, Nygaard OP, Solberg TK, Gulati S (2015) The risk of getting worse: predictors of deterioration after decompressive surgery for lumbar spinal stenosis—a multicenter observational study. World Neurosurg 84(4):1095–102
Nerland US, Jakola AS, Solheim O, Weber C, Rao V, Lonne G, Solberg TK, Salvesen Ø, Carlsen SM, Nygaard ØP, Gulati S (2015) Minimally invasive decompression versus open laminectomy for central stenosis of the lumbar spine: pragmatic comparative effectiveness study. BMJ 350:h1603
Neukamp M, Perler G, Pigott T, Munting E, Aebi M, Roder C (2013) Spine Tango annual report 2012. Eur Spine J 22(Suppl 5):767–86
Overdevest GM, Moojen WA, Arts MP, Vleggeert-Lankamp CL, Jacobs WC, Peul WC (2014) Management of lumbar spinal stenosis: a survey among Dutch spine surgeons. Acta Neurochir (Wien) 156(11):2139–45
Schizas C, Kulik G (2012) Decision-making in lumbar spinal stenosis: a survey on the influence of the morphology of the dural sac. J Bone Joint Surg (Br) 94(1):98–101
Stromqvist B, Fritzell P, Hagg O, Jonsson B, Sanden B (2013) Swedish Society of Spinal S. Swespine: the Swedish spine register: the 2012 report. Eur Spine J 22(4):953–74
Thome C, Zevgaridis D, Leheta O, Bazner H, Pockler-Schoniger C, Wohrle J, Schmiedek P (2005) Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine 3(2):129–41
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2008) Sport Investigators. (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358(8):794–810
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. This article does not contain any studies with human participants performed by any of the authors.
Funding
No funding was received for this research.
Rights and permissions
About this article
Cite this article
Weber, C., Lønne, G., Rao, V. et al. Surgical management of lumbar spinal stenosis: a survey among Norwegian spine surgeons. Acta Neurochir 159, 191–197 (2017). https://doi.org/10.1007/s00701-016-3020-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-3020-0