Abstract
Background
The Neck Disability Index (NDI) is widely used as a self-rated disability score in patients with cervical radiculopathy. The purpose of this study was to evaluate whether the NDI score correlated with other assessments of quality of life and mental health in a specific group of patients with single-level cervical disc disease and corresponding radiculopathy.
Methods
One hundred thirty-six patients were included in a prospective, randomized controlled clinical multicenter study on one-level anterior cervical discectomy with arthroplasty (ACDA) versus one-level anterior cervical discectomy with fusion (ACDF). The preoperative data were obtained at hospital admission 1 to 3 days prior to surgery. The NDI score was used as the dependent variable and correlation as well as regression analyses were conducted to assess the relationship with the short form-36, EuroQol-5Dimension-3 level and Hospital Anxiety and Depression Scale.
Results
The mean age at inclusion was 44.1 years (SD ±7.0, range 26–59 years), of which 46.3 % were male. Mean NDI score was 48.6 (SD = 12.3, minimum 30 and maximum 88). Simple linear regression analysis demonstrated a significant correlation between NDI and the EuroQol-5Dimension-3 level [R = -0.64, 95 % confidence interval (CI) -30.1– -19.8, p < 0.001] and to a lesser extent between NDI and the short form-36 physical component summary [R = -0.49, 95 % CI (-1.10– -0.58), p < 0.001] and the short form-36 mental component summary [R = -0.25, 95 % CI (-0.47– -0-09), p = 0.004]. Regarding NDI and the Hospital Anxiety and Depression Scale, a significant correlation for depression was found [R = 0.26, 95 % CI (0.21–1.73), p = 0.01]. Multiple linear regression analysis showed a statistically significant and the strongest correlation between NDI and the independent variables in the following order: EuroQol-5Dimension-3 level [R = -0.64, 95 % CI (-23.5– -7.9), p <0.001], short form-36 physical component summary [R = -0.41, 95 % CI (-0.93– -0.23), p = 0.001] and short form-36 mental component summary [R = -0.36, 95 % CI (-0.53– -0.15), p = 0.001].
Conclusion
The results from the present study show that the NDI correlated significantly with a different quality of life and mental health measures among patients with single-level cervical disc disease and corresponding radiculopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Neck Disability Index (NDI) was originally developed to evaluate activities of daily living among patients with disabling neck pain, especially following whiplash trauma [24], and is based on the Oswestry Low Back Pain Index (OI) [5].
Although its primary use is in patients with neck pain, the NDI has been found well suited as an outcome measure in clinical trials among patients with cervical radiculopathy [19]. Over the years, it has been widely used as the primary outcome variable in large prospective, randomized controlled clinical trials [22, 4, 13, 8, 12]. It has been shown to correlate well with the Health-Related Quality of Life (HRQoL) questionnaire Short Form-36 (SF-36) [25, 11, 18] and the EuroQol-5Dimension-3 Level (EQ-5D-3 L) [1, 2]. However, correlation analyses between these two questionnaires and the NDI have been conducted in outpatient settings on patients with various disorders of the cervical spine and neck.
The present study is the first to explore the relationship between the NDI and HRQoL questionnaires SF-36 and EQ-5D-3 L and between the NDI and the Hospital Anxiety and Depression Scale (HADS) [28] in a specific group of patients with single-level cervical radiculopathy. The purpose of the study was to assess whether the NDI score could provide a broader understanding of the patients' overall health situation and thus add value to the clinical assessment and selection of patients for surgery.
Study population
One hundred thirty-six patients were included in a prospective, randomized controlled clinical multicenter trial on single-level anterior cervical discectomy with arthroplasty (ACDA) versus anterior cervical discectomy with fusion (ACDF) [9]. Patients were enrolled at five university hospitals in Norway during the time period November 2008 to January 2013. Demographics, duration of symptoms, length of sick leave, social status, profession and smoking habits were recorded in addition to quality of life and mental health questionnaires.
Inclusion criteria were age 25–60 years, clinical C6 or C7 root radiculopathy with corresponding radiological findings with or without neurological deficits, Neck Disability Index (NDI) ≥30 %, and the patient did not respond to nonoperative treatment and had no sign of improvement during the last 6 weeks prior to surgery.
Exclusion criteria were significant spondylosis involving more than one level, adjacent level ankylosis, intramedullary changes on magnetic resonance imaging (MRI), clinical suspicion of myelopathy, chronic generalized pain syndrome, mental illness, infection, active cancer disease, rheumatoid arthritis involving the cervical spine, previous trauma involving the cervical spine, pregnancy, allergy against contents of the cage/artificial disc, previous neck surgery, the patient did not understand Norwegian orally or in writing, and abuse of medication/narcotics.
Method
The NDI was used as our primary and dependent variable regarding preoperative self-rated disability. The NDI questionnaire is composed of ten items (pain, personal care, lifting, reading, headache, concentration, work/daily activities, driving, sleep and recreation). Each item is scored from 0–5. Scores range from 0 to 100 %, with a lower score indicating less severe symptoms.
As secondary variables regarding HRQoL we used: (1) the SF-36 and (2) the EQ-5D-3 L. The SF-36 is a generic health-related quality of life questionnaire. It measures along eight dimensions and has been used to assess health status and to measure the impact of clinical and social interventions. The baseline SF-36 scores for the eight dimensions: physical functioning (PF), role-physical (RP), bodily pain (BP), general health GH), vitality (VT), social functioning (SF), role-emotional (RE), mental health (MH) and the two summary scales, physical component summary (PCS) and mental component summary (MCS), were calculated. Regarding SF-36, each subscale is scored from 0–100, with higher scores representing better function. We used the Norwegian (chronic) version v 2.0.of the Short Form-36, and for scoring of the questionnaire, we used QualityMetric Health OutcomesT Scoring Software 2.0 (QualityMetric Incorporated, Lincoln, RI, USA).
The EQ-5D-3 L utility index is a generic score with five dimensions: mobility, self-care, activities of daily life, pain and anxiety/depression. Each dimension has three levels: no problems, some problems and extreme problems. This gives 243 possible combinations, or health states, revised into an index ranging from -0.59 to 1.00. Higher scores represent better health. The 243 possible health states are evaluated against a normal population using the time trade-off method (TTO). We used the Norwegian version of EQ-5D-3 L. For conversion to utilities, we used the UK TTO tariff to calculate the index [23].
The Hospital Anxiety and Depression Scale (HADS) was used to assess anxiety and depression. This is a 14-item scale that generates ordinal data. Seven of the scale items relate to anxiety (HAD-A) and seven to depression (HAD-D). An HAD-A or HAD-D subscore of 8–10 points is considered a possible case of anxiety or depression and ≥11 points a definite case [28]. The HADS questionnaire was introduced approximately 1 year after patient enrollment started. Accordingly only 92 out of 136 patients answered the HADS questionnaire. Demographic and HRQol analyses were performed to rule out differences between the patients who answered the questionnaire and those who missed answering it because of the late introduction.
Statistics
The patients' NDI scores were defined as the dependent variable and analyzed as continuous data. The independent variables SF-36, EQ-5D-3 L and HADS were also analyzed as continuous data. The relationships between the two mental health variables SF-36 MCS score and HAD-A and HAD-D were separately analyzed.
Continuous or categorical data are presented as means and standard deviations (SD) or number and percentages, respectively. A simple linear regression analysis was conducted to explore the relationship between increasing NDI score and the SF-36 subscores PF, RP, BP, GH, VT, SF, RE and MH and the two summary scores PCS and MCS, and between increasing NDI score and EQ-5D-3 L, HAD-A and HAD-D. Where statistical significance was found, regression coefficients (Rs) and confidence intervals (CIs) are specified. The R square (R2) was calculated to assess how much of the total variation in the dependent variable could be explained by the independent variable. A multiple regression analysis was performed to explore the relationship between NDI and SF-36 PCS, SF-36 MCS, EQ-5D-3 L, HAD-A and HAD-D. A stepwise multiple regression analysis was conducted to assess which of our independent variables best predicted our dependent variable, the NDI. The relationship between the SF-36 MCS score and HAD-A and HAD-D was investigated using Pearson product-moment correlation coefficient. The strength of the relationship between variables was interpreted as suggested by Cohen [3].
Comparison of continuous or categorical data between the patients who answered the HADS questionnaire (included after the first year of enrolment) and those who did not (included the first year) were statistically tested with an independent T-test or Pearson chi-square tests, respectively.
Nonparametric data were analyzed by Mann-Whitney U test. A p value < 0.05 was used as level of significance.
SPSS version 18.0 (IBM Corp., Armonk, NY) was used for all analysis.
Ethical considerations
The study was approved by the Regional Committee for Medical and Health Research Ethics and the Data Protection Official for Research. The study was registered at clinicaltrials.gov [9]. All patients included in the trial gave their written informed consent to participation.
Results
One hundred thirty-six patients were included in the trial. Mean age was 44.1 (SD = ±7.0, range 26–59 years), and 63 (46.3 %) study participants were male. Forty-one percent were smokers (40 % of mlaes and 41 % of females). Forty percent had higher education defined as college or university. Ninety-two percent had Norwegian as their native language. Fifty-four percent of the patients had radiculopathy related to cervical disc level C5/C6 and the remaining to C6/C7. Mean NDI score was 48.6 (SD = 12.3, minimum 30 and maximum 88). The patients (n = 136) answered the SF-36 and EQ-5D-3 L questionnaires at inclusion 1–3 days prior to surgery. Ninety-two patients answered the HADS questionnaire. To assess possible differences between the patients who had answered the HADS questionnaire and those who did not, analysis of demographics and comparison of HRQoL variables was performed. No statistically significant differences were found.
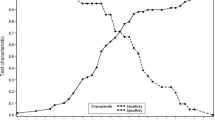
First a simple linear regression analysis was performed, which demonstrated a statistically significant relationship between an increasing NDI score and decline in the SF-36 subscales PF, RP, BP, VT, SF, RE and MH and the two summary scales PCS and MCS, and between NDI and EQ-5D-3 L (Table 1). The strongest correlation was found between NDI and EQ-5D-3 L [R = -0.64, 95 % CI (-30.1– -19.8), p < 0.001], indicating that a higher NDI is associated with poorer HRQoL. There was a positive correlation between NDI scores and HAD-A and HAD-D, but these were only significant for HAD-D [R = 0.26, 95 % CI (0.21–1.73), p = 0.01] (Table 1).
Second, a multiple linear regression analysis was used to assess the ability of the independent variables EQ-5D-3 L, SF-36 summary scores PCS and MCS and HAD-A and HAD-D to predict the level of the NDI score. Preliminary analyses were conducted to ensure no violation of the assumptions of normality, linearity, multicollinearity and homoscedasticity. A high correlation between SF-36 MCS and HAD-D (R = -0.7) resulted in HAD-D being excluded from the multiple regression analysis to avoid multicollinearity. There was a significant positive correlation, most pronounced for EQ-5D-3 L, intermediate for SF-36 PCS and lowest for SF-36 MCS (Table 2).
Finally, a stepwise multiple regression analysis was conducted to assess which of our independent variables best predicted our dependent variable, the NDI. The analysis excluded HAD-A and explained the variance in NDI (Table 3).
To analyze the relationship between the SF-36 MCS score and HAD-A and HAD-D, Pearson product moment correlation was used. The results were interpreted as suggested by Cohen [3] and showed an intermediate negative correlation for HAD-A [R = -0.45, 95 % CI (-0.61– -0.27), p <0.001] and a strong negative correlation for HAD-D [R = -0.69, 95 % CI (-0.79– -0.56), p <0.001]. Both analyses reached statistical significance. A higher MCS score means better metal health and is thus associated with lower HAD-A and D scores, indicating fewer symptoms of anxiety and depression.
Discussion
The present study demonstrates that in patients with single-level cervical disc disease and corresponding radiculopathy, the NDI captures patients' HRQoL and mental health. We found statistically significantly poorer HRQol with increasing NDI scores for both SF-36 summary scales, PCS and MCS, and for all SF-36 subscales except for general health (GH). The strongest correlation was found between NDI and EQ-5D-3 L.
A weaker correlation was seen between NDI and symptoms of depression. Symptoms of anxiety also correlated with increasing NDI, although not statistically significantly. There was, however, a significant correlation between the mental component summary of SF-36 and both HAD-A and HAD-D.
The prevalence of cervical radiculopathy has been estimated at 3.3 cases per 1000 [20] with an average age-adjusted incidence per year of 0.8 per 1000 [17], and 75–90 % of patients with cervical radiculopathy will improve with nonoperative treatment [17, 21]. Until 1991 no instruments were available to assess the self-rated disability among these patients. The NDI provides an opportunity for objective evaluation of the degree of disability both before treatment and as an outcome measure following treatment. The severity of the patients’ ailments is related to the NDI score and has been graded as follows: 0–20 normal, 21–40 mild disability, 41–60 moderate disability, 61–80 severe and >80 complete/exaggerated [11].
The preoperative NDI score has proven useful to assess outcome after surgery in patients with cervical radiculopathy. A low preoperative score and low current pain on the visual analog scale (VAS) [26] correlate significantly with low postoperative disability [16, 15, 14]. A previous study showed that NDI correlated with current pain intensity, and the patients’ experience of pain was the most important predictor for NDI outcome following ACDF [14].
In the present study, there was a significant correlation between NDI and EQ-5D-3 L, which corresponds well with recently published data [2]. EQ-5D-3 L is easy to administer and score, and it is increasingly used in the clinical setting. The NDI is the most commonly used primary outcome assessment of patients with cervical radiculopathy and neck pain, and the EQ-5D-3 L explained 41 % of the variance in NDI in our study, which is somewhat lower than recently reported by Carreon and colleagues [2].
The NDI is well suited for both pre- and postoperative assessment of patient disability. It has been found to compare well with the HRQoL questionnaire SF-36 [11, 18], which is considered the gold standard for health assessment [10, 7, 6]. The SF-36, however, is more complicated to score, and it takes longer to complete the questionnaire than the NDI. There was a significant correlation between the NDI and SF-36, which corresponds well with previous studies by McCarthy and colleagues [11] and Grevitt and coworkers [7].
There was also a significant correlation between increasing NDI and higher HAD-D scores in the present study. Based on our results, it seems that NDI captures the patients’ level of depression, but not anxiety. Anxiety, however, is partly captured by the SF-36 MCS score and correlates with HAD-A. The present results correspond with a previous study [27] demonstrating that symptoms of depression, using the Modified Self-rating Depression Scale Zung questionnaire [29], were significantly associated with NDI scores in patients with cervical radiculopathy.
Strengths of our study
Previous studies have assessed the correlation between NDI and HRQoL among patients with a variety of disorders of the cervical spine. However, to the best of our knowledge, no studies have focused on the correlation between NDI and HRQoL and NDI and mental health in patients with single-level cervical radiculopathy scheduled for surgery. This is also the first study to demonstrate the relationship between the mental component score of SF-36 and HAD-A and HAD-D among patients with single-level cervical disc disease.
Limitations
Somewhat few patients preclude firm conclusions about the study results. Former mental disorder that made the patient unsuitable for participation in the study was one of the exclusion criteria. Mental disorder could have been emphasized more specifically since the phrase “unsuitable for participation” gives the interviewer an opportunity for a broad interpretation of what is not a suitable affliction. Thus, some patients may have had symptoms of anxiety and/or depression regardless of their cervical radiculopathy and self-rated disability.
The questionnaires were answered 1 to 3 days prior to surgery, and anxiety about the operation itself may have influenced the responses among some of the patients. The HADS questionnaire was introduced approximately 1 year after patient enrollment started as additional outcome variable. Thus, only 92 out of 136 included patients answered this questionnaire.
Conclusion
In conclusion, our study demonstrates that a higher NDI score significantly correlates with poorer quality of life and increasing symptoms of depression in patients with single-level cervical radiculopathy. In addition to providing a number for the severity of neck and arm pain, the NDI also provides information about the patients overall health status.
References
Brooks RG, Jendteg S, Lindgren B, Persson U, Björk S (1991) EuroQol: health-related quality of life measurement. Results of the Swedish questionnaire exercise. Health Policy 18:37–48
Carreon LY, Bratcher KR, Das N, Nienhuis JB, Glassman SD (2014) Estimating EQ-5D values from the neck disability index and numeric rating scales for neck and arm pain. J Neurosurg Spine 6:1–6
Cohen JW (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale, NJ
Coric D, Nunley PD, Guyer RD, Musante D, Carmody CN, Gordon CR, Lauryssen C, Ohnmeiss DD, Boltes MO (2011) Prospective randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 15:348–358
Fairbank JCT, Couper J, Davies JB, O'Brien JP (1980) The Oswestry low back pain disability index. Physiotherapy 66:2713
Garratt AM, Ruter DA, Abdalla MI, Buckingham JK, Russell IT (1993) The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS. Br Med J 306:1440–1443
Grevitt M, Khazim R, Webb JK, Mulholland R, Shepperd J (1997) The short form-36 health survey questionnaire in spine surgery. Br J Bone Joint Surg 79:48–52
Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK (2009) Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled clinical trial. Spine (Phila Pa 1976) 34:101–107
http://clinicaltrials.gov/show/NCT00735176 Accessed 1 June 2015
Jenkinson C, Coulter A, Wright L (1993) Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. Br Med J 306:1437–1440
McCarthy MJH, Grevitt MP, Silcocks P, Hobbs G (2007) The reliability of the Vernon and Mior neck disability index, and its validity compared with the short form-36 health survey questionnaire. Eur Spine J 16:2111–2117
Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA (2007) Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 6:198–209
Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9:275–286
Peolsson A, Hedlund R, Vavruch L, Oberg B (2003) Predictive factors for the outcome of anterior cervical decompression and fusion. Eur Spine J 12:274–280
Peolsson A, Peolsson M (2008) Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. Eur Spine J 17:406–414
Peolsson A, Vavruch L, Oberg B (2006) Predictive factors for arm pain, neck pain, neck specific disability and health after anterior cervical decompression and fusion. Acta Neurochir 148:167–173
Radhakrishnan K, Litchy WJ, O′Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population based study from Rochester, Minnesota, 1976 through 1990. Brain 117:325–335
Riddle D, Stratford P (1998) Use of generic versus region-specific functional status measures on patients with cervical spine disorders. Phys Ther 78:951–963
Rodi RJ, Vernon H (2012) Cervical radiculopathy: a systematic review on treatment by spinal manipulation and measurement with the neck disability index. J Can Chiropr Assoc 56:18–28
Salemi G, Savettieri G, Meneghini F, Di Benedetto ME, Ragonese P, Morgante L, Reggio A, Patti F, Grigoletto F, Di Perri R (1996) Prevalence of cervical spondylotic radiculopathy: a door-to-door survey in a Sicilian municipality. Acta Neurol Scand 93:184–188
Sampath P, Bendebba M, Davis JD, Ducker T (1999) Outcome in patients with cervical radiculopathy. Prospective multicenter study with independent clinical review. Spine 24:591–597
Sasso RC, Anderson PA, Riew KD, Heller JG (2011) Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am 93:1684–1692
The EuroQol Group (1990) EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Vernon H, Mior S (1991) The Neck Disability Index: a study of reliability and validity. J Manip Physiol Ther 14:409–415
Ware JE, Sherbourne CD (1992) The MOS 36-Item Short Form Health Survey (SF- 36). I: Conceptual framework and item selection. Med Care 30:473–483
Wewers ME, Lowe NK (1990) A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 13:227–236
Wibault J, Oberg B, Löfgren H, Zsigmond P, Persson L, Peolsson A (2014) Individual factors associated with neck disability in patients with cervical radiculopathy scheduled for surgery: a study on physical impairments, psychosocial factors, and life style habits. Eur Spine J 23:599–605
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67:361–370
Zung WW (1965) A self-rating depression scale. Arch Gen Psychiatry 12:63–70
Acknowledgments
The authors would like to thank Vigdis Skogli, Torun Gillebo, Jorund Roos, Camilla Seif and Monica Finkirk for efforts to convene the patients, coordination of investigations and follow-up of the study.
Conflict of interest
The study committee has received a grant from DePuy Synthes Spine (325 Paramount Drive Raynham, MA 02767) for the project to be completed. The study sponsor was not involved in the study design, conduct of the trial, or writing or review of the manuscript. The prostheses implanted were solely financed by the individual hospitals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sundseth, J., Kolstad, F., Johnsen, L.G. et al. The Neck Disability Index (NDI) and its correlation with quality of life and mental health measures among patients with single-level cervical disc disease scheduled for surgery. Acta Neurochir 157, 1807–1812 (2015). https://doi.org/10.1007/s00701-015-2534-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2534-1