Abstract
Background
Homocysteine (tHcy) has been known over the last few decades for its putative impact on vascular diseases, but has not been evaluated much in patients with subarachnoid hemorrhage (SAH). This study was carried out to assess its prognostic impact on the neurological outcome following SAH.
Methods
Admission plasma tHcy was evaluated in 90 SAH patients and prospectively studied in relation to various factors and the Glasgow Outcome Scale (GOS) at 3 months. Univariate and multivariate analyses were performed using SPSS 21.
Results
tHcy was significantly higher following SAH compared to matched controls [median (IQR): 25.7 (17.3–35.9) vs. 14.0 (9.8–17.6) μmol/l, p < 0.001]. It was significantly higher in younger patients. However, systemic disease, WFNS and Fisher grades did not have a significant impact on its levels. tHcy was significantly lower among patients who died [median (IQR): 16.0 (14.4–20.6) vs. 29.7 (21.8–40.2) μmol/l, p < 0.001] and those with unfavorable outcome (GOS 1–3) [median (IQR): 21.6 (14.5–28.2) vs. 30.3 (20.4–40.7) μmol/l, p = 0.004] compared to others, with a significant continuous positive correlation between tHcy and GOS (p = 0.002). The beneficial association of tHcy with outcome was homogeneous with no significant subgroup difference. Multivariate analysis using binary logistic regression adjusting for the effects of age, systemic disease, WFNS grade, Fisher grade, site of aneurysm, clipping or coiling revealed higher tHcy to have a significant independent association with both survival (p = 0.01) and favorable outcome (p = 0.04).
Conclusions
Higher homocysteine levels following SAH appear to have a significant association with both survival and favorable neurological outcome, independent of other known prognostic factors, apparently exemplifying “reverse epidemiology paradox” in which a conventional risk factor seems to impart a survival advantage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH), constituting 5 % of strokes, occurs predominantly in productive middle age. In spite of immense changes in its management in the last decade, the case fatality rate is around 30–50 %, with a third of survivors having major neurological deficits and only a third of survivors able to return to their profession [5, 6, 14]. The outcome is even more dismal among the elderly and those with a poor clinical-radiological grade and in the presence of serious systemic diseases [5, 6, 14]. In spite of the considerable health-economic burden of disability following SAH on society, outcome prediction overall has been enigmatic because of the complex interplay of various pathophysiological mechanisms beyond mere vascular spasm [21, 28]. Patients with SAH can have poor neurological outcomes without vasospasm, and those with good outcomes might have had vasospasm [21]. This necessitates the identification of biochemical prognostic markers for the cardinal components of ischemia, inflammation, microthrombi, deranged microcirculation, oxidative damage and apoptosis in addition to vasospasm, potentially helpful in recognizing patients at high risk for unfavorable outcome even before their deterioration [4, 13, 21, 28]. Yet no biomarkers have been predictive of outcome after SAH.
Total homocysteine (tHcy), a sulfhydryl non-protein α-amino acid and branch-point intermediate of methionine metabolism, has been implicated by several observational studies in coronary artery disease, ischemic stroke, venous thrombosis, retinal artery and vein occlusion, and anterior ischemic optic neuropathy because of its predominant atherothrombogenic properties and its effect on a plethora of mechanisms encompassing vascular remodeling, decreased NO, platelet activation, endothelial dysfunction and apoptosis, which invariably are also part of the pathophysiology of SAH [11, 20, 24, 29, 31, 33]. However, its role in SAH has not been studied much.
This is probably the first prospective study on the correlation of admission plasma total homocysteine (tHcy) levels with neurological outcome following SAH.
Methods
Study design and procedures
All patients with spontaneous SAH admitted within 5 days of ictus at the Neurosurgery Department of the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, underwent plasma tHcy level assessment at admission and were taken up for the study, with ethics committee approval. Those with Glasgow Coma Scale (GCS) scores of 3/15 were not considered for the study.
SAH patients with a good clinical grade or those with large lobar bleeds underwent urgent computed tomography angiography (CTA). Poor grade patients were stabilized and then taken up for CTA. Ventriculoperitoneal shunt or external ventricular drainage was performed in poor grade patients with hydrocephalus, depending on the clinical status and intraventricular bleed. Patients underwent surgical clipping or endovascular coiling as per their choice and feasibility as early as possible. Poor grade patients were preferentially offered coiling. The management protocol included phenytoin, nimodipine, cardiovascular monitoring, fluid and electrolyte homeostasis. Induced hypertension was employed during symptomatic vasospasm after aneurysm occlusion.
The admission EDTA blood samples of patients were analyzed post-centrifugation for plasma total homocysteine (tHcy) levels by competitive immunoassay using direct, chemiluminescent technology with the ADVIA Centaur Immunoassay System (Siemens AG, Munich, Germany). It was primarily considered as a continuous variable, but also classified as low (<5 μmol/l), normal (5 to less than 15 μmol/l), moderate (15–30 μmol/l) and intermediate (30–100 μmol/l) elevation categories [20, 33]. The tests were also performed on 20 (age- and gender-matched) normal volunteers from the same community to arrive at a local control range. The clinical team was blinded to the tHcy levels for at least 3 months following ictus.
Basic demographic data of patients, associated serious systemic disease (inadequately treated or severe hypertension or diabetes mellitus), admission World Federation of Neurosurgical Societies (WFNS) grade [30], admission computed tomography (CT) Fisher grade [9], site of aneurysm, treatment details and adverse events were entered in a pre-planned prospective database and were followed up. New onset neurological impairment, not apparent immediately after aneurysm occlusion, not due to other causes based on clinico-radiological and laboratory findings, was noted as delayed ischemic neurological deficit or delayed cerebral ischemia [5, 21].
Outcomes
The Glasgow Outcome Scale (GOS) [16] was adopted because of its simplicity and more lucid categorization of outcome and was assessed at 3 months after the bleed, either directly or over the telephone. Good recovery (GOS 5) or moderate disability (GOS 4) was considered a favorable outcome, and severe disability (GOS 3), persistent vegetative state (GOS 2) or death (GOS 1) was considered an unfavorable outcome. Patients who had died because of any cause were considered as GOS 1 or mortality.
Statistical analyses
Continuous variables were assessed for normality with the Shapiro-Wilk test. Normally distributed (parametric) data were reported as a mean with standard deviation (SD). Nonparametric data were reported as a median with interquartile range (IQR). Categorical data were reported as counts and proportions in each group. SPSS 21 software (IBM Corp., New York, USA) was used for the statistical analyses. Univariate analyses of continuous variables across binary categories were compared using the independent samples T test (parametric) or Mann–Whitney U test (nonparametric) and across multiple categories using ANOVA (parametric) or the Kruskal-Wallis test (nonparametric). The bivariate relationship between two continuous variables was assessed using the Pearson (parametric) or Spearman (nonparametric) correlation coefficient. Proportions were compared using chi-square or Fisher’s exact test wherever appropriate, and subgroup analyses were done using the Breslow-Day test of homogeneity of odds ratios on parameters found significant in univariate analysis. Two-sided significance tests were used throughout, and the significance level was kept at p < 0.05. Multivariate analyses were conducted on both mortality and unfavorable neurological outcome using binary logistic regression with mandatory significance of the model coefficient being less than 0.05 for validity of outcome prediction after adjusting for known prognostic factors such as age, serious systemic disease, WFNS grade, Fisher grade, site of aneurysm and definitive treatment in relation to tHcy levels as continuous variables.
Results
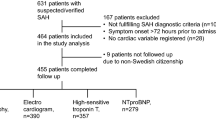
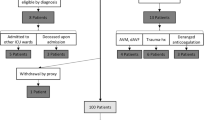
There were a total of 90 patients included in our study. Their ages were normally distributed ranging from 20 to 76 years. The mean age was 49 years, and there were 22 patients aged 60 years or more. There were 45 males and 45 females. There were 20 (10 male and 10 female) matched controls with a mean age of 50 years.
Out of the total 90 patients with SAH, 29 (32 %) had clinical evidence of inadequately treated or severe systemic disease (hypertension or diabetes). Fifty-six (62 %) patients had presented in good clinical grade (WFNS grade 1-III), while the rest had presented in poor grade. There were 45 (50 %) and 43 (48 %) patients in admission CT Fisher grades 3 and 4, respectively, and the remaining 2 (2 %) patient in grade 2. Out of 76 patients who were clinically stable enough to undergo CT angiography, 65 (86 %) had aneurysms in the anterior circulation (26 in the anterior communicating artery, 4 in the distal anterior cerebral artery, 19 in the internal carotid segments, 16 in the middle cerebral artery), 5 (7 %) had aneurysms in the posterior circulation, and 6 (8 %) had severe vasospasm precluding identification of any aneurysm. Of the total 90, 47 (52 %) underwent surgical clipping, and 13 (14 %) underwent endovascular coiling, while the rest were in poor clinical status on supportive medical management.
Admission plasma tHcy levels were significantly higher in patients with SAH compared to matched controls [median (IQR): 25.7 (17.3–35.9) vs. 14.0 (9.8–17.6) μmol/l, p value < 0.001] (Fig. 1). Of the 90, 2 had low (<5 μmol/l), 18 had normal (5 to less than 15 μmol/l), 37 had moderate (15–30 μmol/l) and 33 had intermediate (>30 μmol/l) hyperhomocysteinemia. Younger patients had significantly higher tHcy levels (median of 28.5 vs. 20.1 μmol/l, p value = 0.03). Patients with ruptured anterior cerebral artery aneurysms had significantly greater and those with ruptured middle cerebral artery aneurysms had significantly lower levels of tHcy (p value = 0.04) compared to others. WFNS grade had a significant inverse correlation with tHcy as continuous data (p value = 0.01) and nonsignificant association with tHcy levels as categorical data. Serious systemic disease, Fisher grade and multiplicity of aneurysms did not have any significant impact on tHcy levels. Patients who underwent clipping or coiling did not differ significantly in tHcy levels and in comparison to those who could not undergo definitive treatment because of poor clinical status. Patients with delayed ischemic neurological deficits had statistically nonsignificantly lower tHcy levels compared to others (Table 1).
The outcome could only be assessed for 73 patients at 3 months. The admission tHcy levels were significantly lower among patients who died [median (IQR): 16.0 (14.4–20.6) vs. 29.7 (21.8–40.2) μmol/l, p value < 0.001] and those with unfavorable neurological outcome (GOS 1–3) [median (IQR): 21.6 (14.5–28.2) vs. 30.3 (20.4–40.7) μmol/l, p value = 0.004] compared with those who were alive and with favorable outcome, respectively (Table 1). As continuous data, there was a significant positive correlation between admission plasma tHcy levels and GOS at 3 months (Spearman ρ = 0.36, p value = 0.002) (Fig. 2).
As categorical data, WFNS and Fisher grades had a significant univariate impact on neurological outcome (p value = 0.001). Patients with intermediate tHcy (>30 μmol/l) levels had even significantly better outcome compared to those with moderate tHcy (15–30 μmol/l) and normal levels (79 % vs. 53 % vs. 40 % favorable outcome, respectively, p value = 0.03) (Fig. 3). Only age, WFNS grade and tHcy had a significant categorical univariate impact on mortality (p values 0.04, <0.001 and 0.001 respectively). Sex, serious systemic disease, site of aneurysm, multiplicity of aneurysms, and clipping or coiling did not have any significant association with either mortality or neurological outcome.
Significant association of tHcy with neurological outcome both as a continuous variable as well as ordinal categories prompted subgroup analyses of various factors across different tHcy levels. Patients with tHcy elevation overall had significantly less mortality (12 vs. 47 %) (p value = 0.01) compared with the rest. The inverse association of tHcy elevation with mortality was uniform and homogeneous across all subgroups with no significant subgroup difference. However, the association of tHcy elevation on neurological outcome was less marked among younger patients compared with the elderly (Table 2).
Multivariate analyses of mortality and neurological outcome using binary logistic regression model were found to be significant, adjusting for the effects of age, systemic disease, admission WFNS grade, Fisher grade, site of aneurysm, clipping or coiling, and admission plasma tHcy levels. Higher plasma tHcy levels were noted to have a significant association with both survival (p value = 0.01) and favorable neurological outcome (p value = 0.04), while a higher Fisher grade had a significant association with unfavorable outcome (p value = 0.01), independent of other known confounding factors (Fig. 4).
Discussion
Despite homocysteine (tHcy) emerging as a key prognostic tool to assess metabolic imbalance in cardiovascular diseases and ischemic stroke [11, 20, 24, 29, 31, 33], it has not been studied much in patients with subarachnoid hemorrhage.
In our study, plasma tHcy levels were significantly higher at admission in patients with SAH compared to matched controls. In a smaller comparative study of tHcy in SAH and controls, McEvoy et al. noted no significant difference between them [25]. This might be because many patients in their study had been assessed at a later stage following SAH. Higher levels of tHcy in the acute setting in patients with SAH have not been reported previously. These increased levels may be due to either SAH occurring more in those with higher levels of tHcy or elevation of tHcy in response to SAH. Though the former explanation was considered probable for a while in cardiovascular diseases and ischemic stroke at least, the results of many studies of tHcy measurement before the onset of vascular disease were inconsistent, leading to the coexistent latter possibility of “reverse causality,” in which the disease results in increased tHcy levels as a result of metabolic stress response [1, 3, 12, 17, 23, 24]. The difference in tHcy levels at admission in relation to the site of aneurysm rupture may be due to greater metabolic response in ACA bleeds, probably because of the proximity to the hypothalamic axis.
Regardless of the causality, there is abundant epidemiological evidence implicating tHcy as an independent prognostic marker in cardiovascular disease and ischemic stroke [20, 24, 29, 33]. Surprisingly, we noted higher admission tHcy levels to be significantly associated with survival and favorable outcome, independent of other confounding factors such as age, clinical-radiological grade, presence of a significant systemic disease, site of aneurysm, and clipping or coiling and of each other.
Plasma tHcy comprises protein-bound homocysteine, homocysteine dimer (homocystine), cysteine-homocysteine disulfide, free homocysteine and homocysteine thiolactone [20, 23, 33]. tHcy resulting solely from dietary methionine predominantly undergoes transmethylation by methionine synthase, capturing the methyl group to be transferred further to various biomolecules including DNA and proteins [2, 23, 29]. There is an additional transsulfuration pathway by cystathionine β-synthase (CBS), stimulated by oxidative stress, which gives rise to hydrogen sulfide (H2S) and cysteine-dependent metabolites such as glutathione (GSH), sulfate and taurine, having antilipid peroxidative effects [10, 22, 33].
The traditional harmful effects of tHcy in cardiovascular diseases and ischemic stroke were attributed to its oxidative metabolism to homocystine (Hcy-Hcy) and homocysteine thiolactone (HCTL), causing endothelial dysfunction, platelet activation, increased proliferation of vascular smooth muscle cells, decreased nitric oxide, homocysteinylation of proteins, atherothrombogenesis, excitotoxicity and apoptosis [15, 20, 23, 29, 33]. However, Grobelny et al. found no correlation of tHcy levels with cerebral vasospasm following SAH [10]. The apparent contrarian and protective association of tHcy noted by us has never been reported previously, except in patients of end-stage renal disease on dialysis [19, 22]. This so-called “malnutrition inflammation complex syndrome” (MICS) in dialysis patients demonstrates a “reverse epidemiology” or “survival paradox” in which the conventional risk factors such as homocysteine seem to be protective, imparting a survival advantage [18, 26]. MICS is considered to be due to other superimposed dominant factors such as nutritional status impacting survival to a greater degree in the short term in these patients compared to the long-term harmful effects of tHcy [7, 19, 26].
Though tHcy levels were much lower in patients with a poorer admission WFNS grade in our study, suggesting the baseline impact of SAH-induced early brain injury, its association with outcome independent of WFNS grade and across different WFNS grades indicates the role of tHcy on evolving mechanisms following SAH [4, 21, 28]. The protective effect of tHcy in SAH may be due to a combination of microvascular dilatation because of H2S, regulation of neuronal ion channels and cellular signaling pathways, augmented detoxification-scavenging attributes by metabolites of cysteine such as GSH and methyl group transfers mediating cell repair as well as its thrombogenic nature precluding massive bleed [10, 22, 29, 33]. Watanabe et al. noted an increase in serum glutathione peroxidase activity in SAH as a response to counter-oxidative free-radical stress of vasopasm, implying enhanced Hcy transulfuration [32]. Okomoto et al. used parenteral glutathione, resulting in a significantly better outcome following SAH, indicating the beneficial effect of Hcy [27]. Grobelny et al. noted that gain of function polymorphisms in the CBS gene reduced the risk of delayed cerebral ischemia, but with no effect on angiographic vasospasm [10]. The intricate metabolic balance between the long-term harmful effects and acute protective effects of tHcy probably determines the outcome being tilted to either side, exemplifying the viability of the “reverse epidemiology paradox” in SAH (Fig. 5). During acute stress following SAH, the beneficial intermediates of tHcy, such as H2S and GSH, result in various protective pathophysiological responses resulting in better outcome. This probably masks the chronic ill effects of tHcy in this setting. The similarity of this phenomenon to MICS indicates the burden of hypercatabolism and inflammation in the pathophysiology of SAH [8, 19, 26, 27]. The variability of the homocysteine increase following SAH due to endogenous as well as dietary habits may also explain the racial and ethnic differences in outcome following SAH [1, 5, 6, 14].
Hypothesis of the reverse epidemiology paradox in SAH [Hcy playing a pivotal intermediary role in methionine metabolism following long-term accumulation results in vascular remodeling and decreased NO and platelet activation, causing atherosclerosis, endothelial dysfunction and apoptosis, thereby imparting risk in several vascular pathologies. Hcy mainly undergoes transmethylation by methionine synthase (MS), capturing the methyl group to be transferred further to various biomolecules for cell repair. The supplementary transsulfuration pathway by cystathionine β-synthase (CBS) gives rise to many acute beneficial intermediates, such as H2S enhancing cerebral blood flow, and various antioxidants, probably tilting the metabolic balance toward a favorable outcome in SAH)
The limitations of our study are the greater proportion of patients who were elderly, with a poor clinical-radiological grade and with serious systemic disease in whom ischemia might have played a role in influencing the homocysteine levels. Also we had a relatively smaller sample size, loss to follow-up and no longitudinal assessments of tHcy, which may have precluded any definitive inference. However, considering the potential therapeutic importance of a protective association between higher levels of tHcy and favorable neurological outcome, this observation needs to be corroborated further in a larger, more homogeneous patient group probably of a different community. Studies with longitudinal assessments of tHcy following SAH in comparison with pre-ictus tHcy levels would be ideal to verify the causality or bystander effect in relation to the acute pathophysiological insult.
In conclusion, plasma tHcy elevation following SAH appears to have a significant association with both survival and favorable neurological outcome, independent of other confounding factors, exemplifying a “reverse epidemiology paradox” in SAH. The putative protective role of tHcy may be due to acute beneficial intermediates of tHcy such as H2S and GSH prevailing over the known long-term harmful effects of tHcy, probably by causing enhanced microvascular blood flow and a better response to oxidative stress.
References
Al-Delaimy WK, Rexrode KM, Hu FB, Albert CM, Stampfer MJ, Willett WC, Manson JE (2004) Folate intake and risk of stroke among women. Stroke 35:1259–1263
Banecka-Majkutewicz Z, Sawuła W, Kadziński L, Węgrzyn A, Banecki B (2012) Homocysteine, heat shock proteins, genistein and vitamins in ischemic stroke–pathogenic and therapeutic implications. Acta Biochim Pol 59:495–499
Brattström L, Wilcken DE (2000) Homocysteine and cardiovascular disease: cause or effect? Am J Clin Nutr 72:315–323
Carr KR, Zuckerman SL, Mocco J (2013) Inflammation, cerebral vasospasm, and evolving theories of delayed cerebral ischemia. Neurol Res Int 2013:506584
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM, Ogilvy CS, Patel AB, Thompson BG, Vespa P, American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737
Dhandapani S, Pal SS, Gupta SK, Mohindra S, Chhabra R, Malhotra SK (2013) Does the impact of elective temporary clipping on intraoperative rupture really influence neurological outcome after surgery for ruptured anterior circulation aneurysms?–A prospective multivariate study. Acta Neurochir (Wien) 155:237–46
Dhandapani SS, Manju D, Sharma BS, Mahapatra AK (2007) Clinical malnutrition in severe traumatic brain injury: factors associated and outcome at 6 months. Indian J Neurotrauma 4:35–39
Dhandapani SS, Manju D, Vivekanandhan S, Agarwal M, Mahapatra AK (2010) Prospective longitudinal study of biochemical changes in critically ill patients with severe traumatic brain injury: factors associated and outcome at 6 months. Indian J Neurotrauma 7:23–27
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6:1–9
Grobelny BT, Ducruet AF, DeRosa PA, Kotchetkov IS, Zacharia BE, Hickman ZL, Fernandez L, Narula R, Claassen J, Lee K, Badjatia N, Mayer SA, Connolly ES Jr (2011) Gain-of-function polymorphisms of cystathionine β-synthase and delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. J Neurosurg 115:101–107
Hasan N, McColgan P, Bentley P, Edwards RJ, Sharma P (2012) Towards the identification of blood biomarkers for acute stroke in humans: a comprehensive systematic review. Br J Clin Pharmacol 74:230–40
Holmes MV, Newcombe P, Hubacek JA, Sofat R, Ricketts SL, Cooper J, Breteler MM, Bautista LE, Sharma P, Whittaker JC, Smeeth L, Fowkes FG, Algra A, Shmeleva V, Szolnoki Z, Roest M, Linnebank M, Zacho J, Nalls MA, Singleton AB, Ferrucci L, Hardy J, Worrall BB, Rich SS, Matarin M, Norman PE, Flicker L, Almeida OP, van Bockxmeer FM, Shimokata H, Khaw KT, Wareham NJ, Bobak M, Sterne JA, Smith GD, Talmud PJ, van Duijn C, Humphries SE, Price JF, Ebrahim S, Lawlor DA, Hankey GJ, Meschia JF, Sandhu MS, Hingorani AD, Casas JP (2011) Effect modification by population dietary folate on the association between MTHFR genotype, homocysteine, and stroke risk: a meta-analysis of genetic studies and randomised trials. Lancet 378:584–594
Hong CM, Tosun C, Kurland DB, Gerzanich V, Schreibman D, Simard JM (2014) Biomarkers as outcome predictors in subarachnoid hemorrhage—a systematic review. Biomarkers 19:95–108
Hop JW, Rinkel GJ, Algra A, van Gijn J (1997) Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke 28:660–664
Jakubowski H (2000) Homocysteine thiolactone: metabolic origin and protein homocysteinylation in humans. J Nutr 130(Suppl):377S–381S
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1:480–484
Ji Y, Tan S, Xu Y, Chandra A, Shi C, Song B, Qin J, Gao Y (2013) Vitamin B supplementation, homocysteine levels, and the risk of cerebrovascular disease: a meta-analysis. Neurology 81:1298–1307
Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD (2003) Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 63:793–808
Kalantar-Zadeh K (2005) Recent advances in understanding the malnutrition-inflammation-cachexia syndrome in chronic kidney disease patients: what is next? Semin Dial 18:365–369
Kang SS, Wong PW, Malinow MR (1992) Hyperhomocyst(e)inemia as a risk factor for occlusive vascular disease. Annu Rev Nutr 12:279–298
Lee Y, Zuckerman SL, Mocco J (2013) Current controversies in the prediction, diagnosis, and management of cerebral vasospasm: where do we stand? Neurol Res Int 2013:373458
Lord RS, Fitzgerald K (2005) Significance of Low Plasma Homocysteine: Hypohomocysteinemia. Metametrix white paper; Norcross, GA, USA
Manolescu BN, Oprea E, Farcasanu IC, Berteanu M, Cercasov C (2010) Homocysteine and vitamin therapy in stroke prevention and treatment: a review. Acta Biochim Pol 57:467–477
Martí-Carvajal AJ, Solà I, Lathyris D, Karakitsiou DE, Simancas-Racines D (2013) Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev 1, CD006612
McEvoy AW, Marras C, Kitchen ND, Briddon A (2001) Plasma total homocysteine and subarachnoid haemorrhage in a co-factor replete population. Amino Acids 21:237–241
Nurmohamed SA, Nubé MJ (2005) Reverse epidemiology: paradoxical observations in haemodialysis patients. Neth J Med 63:376–381
Okamoto H, Takeuchi H, Tanabe M, Akatsuka K, Nishiyama M, Watanabe T, Hori T (1998) Ameliorated outcome of subarachnoid hemorrhage patients treated with reduced form glutathione. Yonago Acta Medica 41:73–81
Østergaard L, Aamand R, Karabegovic S, Tietze A, Blicher JU, Mikkelsen IK, Iversen NK, Secher N, Engedal TS, Anzabi M, Jimenez EG, Cai C, Koch KU, Naess-Schmidt ET, Obel A, Juul N, Rasmussen M, Sørensen JC (2013) The role of the microcirculation in delayed cerebral ischemia and chronic degenerative changes after subarachnoid hemorrhage. J Cereb Blood Flow Metab 33:1825–1837
Schalinske KL, Smazal AL (2012) Homocysteine imbalance: a pathological metabolic marker. Adv Nutr 3:755–762
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, de Villiers JC (1988) A universal subarachnoid hemorrhage scale: report of a committee of the world federation of neurosurgical societies. J Neurol Neurosurg Psychiatry 51:1457
Wu XQ, Ding J, Ge AY, Liu FF, Wang X, Fan W (2013) Acute phase homocysteine related to severity and outcome of atherothrombotic stroke. Eur J Intern Med 24:362–7
Watanabe T, Sasaki T, Asano T, Takakura K, Sano K, Fuchinoue T, Watanabe K, Yoshimura S, Abe K (1988) Changes in glutathione peroxidase and lipid peroxides in cerebrospinal fluid and serum after subarachnoid hemorrhage–with special reference to the occurrence of cerebral vasospasm. Neurol Med Chir (Tokyo) 28:645–649
Welch GN, Loscalzo J (1998) Homocysteine and atherothrombosis. N Engl J Med 338:1042–1050
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dhandapani, S., Goudihalli, S., Mukherjee, K.K. et al. Prospective study of the correlation between admission plasma homocysteine levels and neurological outcome following subarachnoid hemorrhage: A case for the reverse epidemiology paradox?. Acta Neurochir 157, 399–407 (2015). https://doi.org/10.1007/s00701-014-2297-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2297-0