Abstract
Background
Lesions initially presenting as a scalp mass are quite common entities with a wide spectrum of causes. They may be directly related to the scalp itself or may be secondary stigmata of an underlying process in the skull. The rate and clinical significance of the differential diagnosis of these lesions are not well studied in the adult population.
Methods
Three hundred sixty patients were operated on for scalp masses at our hospital between January 2011 and February 2014. The patients were defined retrospectively by using the hospital coding system for scalp lesions. Among these patients, 15 were excluded for being younger than 16 years old.
Results
A total of 345 patients, consisting of 172 females (49.9 %) and 173 males (50.1 %), were included in the study. The mean age at diagnosis was 44.3 (16–89). There were no mortalities during the follow-up period (mean 17.99 months). Mean numbers of scalp lesions and surgeries were 1.25 and 1.18, respectively. There were 32 distinct histopathological diagnoses, the 5 most common being trichilemmal cyst, epidermal cyst, lipoma, nevus and sebaceous cyst in order of frequency. The rate of “clinically significant” pathologies, meaning malignancies or those needing follow-up, was around 7.8 %. The incidence of correct preoperative diagnosis with respect to the departments was 13–27 %.
Conclusions
Our series indicated that generally scalp masses were underestimated and detailed preoperative diagnostic workup or interdisciplinary consultations were not performed regularly. The overall incidence of clinically significant lesions warrants a high degree of vigilance for accurate diagnosis and management of these lesions, because their etiology can be so variable and challenging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients presenting with a scalp mass are frequently encountered in daily practice. The spectrum of causes is comprehensive. They may be directly related to the scalp itself or may be secondary stigmata of an underlying process in the skull. Moreover, intracranial lesions may extend into the extracranial region, even causing bony defects, rendering a noticeable lesion long before causing neurological deficits. Being unaware of the involvement of the cerebral structures creates a great challenge to the surgeon [8].
The differential diagnosis and management strategies for scalp masses have not been described in detail, nor has their clinical significance. In the literature, the overall incidence of particular diagnoses and rates of clinically significant lesions presenting as scalp masses are not well defined. There are some reports in the pediatric population including congenital lesions [10]; however, the topic has not been well evaluated in adults.
The study was inspired by our experiences with several cases with challenging management, such as cranial vault lymphoma, eccrine cell carcinoma or dermatofibrosarcoma protuberans, which were quite unfamiliar to the authors. The paucity of information in the literature encouraged us to present our experience with scalp masses in order to highlight their clinical significance and evaluation strategies.
This study aims to determine the etiology of scalp masses, the frequency of the causes, their clinical implications, and the concordance between the clinical and histopathological diagnosis.
Materials and methods
A total of 360 patients were operated on for scalp masses in our hospital between January 2011 and February 2014. The patients were defined retrospectively from the hospital coding system, retrieved according to the diagnosis and surgical interventions for scalp lesions. Among these patients, 15 were excluded for being younger than 16 years old. A total of 410 surgeries was performed for 345 patients. The informed consent of each and every patient was obtained before the procedures. The patient charts were retrospectively investigated for (1) surgery departments and repeated surgeries, (2) demographic features, (3) pathology reports, (4) surgical notes and number of surgeries, (5) preoperative and postoperative diagnosis, (6) laterality and location of the lesions, if noted, (7) radiological studies and (8) further managements.
The final diagnosis was based on histolopathological findings in all cases in this study.
The laterality and locations could not be determined in most of the patients (74.2 %) because of inadequate filling in of files; these were classified as “undefined” in our study. Presence of multiple involvements and the number of lesions in a patient were basically acquired from the number of pathology specimens; however, if this information had been noted in the patient charts or could be obviously determined from the radiological images, it was recorded accordingly. Moreover, pathology reports were examined for the presence of calcification, keratinization, proliferation, differentiation, rupturing or necrosis, if noted.
Results
A total of 345 patients, consisting of 172 females (49.9 %) and 173 males (50.1 %), were included in the study. The mean age at diagnosis was 44.3 (16–89). There were no mortalities during the follow-up period (mean 17.99 months, range 7–44 months). General characteristics of the patient demographics and lesions are presented in Table 1. The number of patients over 67 years was quite low compared to other decades.
The locations of the lesions had usually not been specified properly in the documents (74.2 %). The lesions were defined by location (frontal, parietal, etc.) in 94 % of the cases operated on by neurosurgeons; however, this percentage was 10.4 % for plastic surgeons and 9.4 % for general surgeons. The left and right specifications could not be determined in the documents in the majority of the patients.
The mean number of lesions was 1.25 (1–10) for our patient group. Forty patients (11.6 %) had two or more lesions. Five patients (1.4 %) were operated on more than four times; the diagnoses were trichilemmal cyst, squamous cell carcinoma (SCC), actinic keratosis and angiosarcoma in these patients. Moreover, one patient with multiple lesions (over 10 masses) was evaluated for associated pathologies, and two intracranial deep-seated meningiomas were detected (Fig. 1). This elderly patient was examined for neurofibromatosis; however, the scalp lesions were diagnosed as trichilemmal cysts and epidermal cysts with calcifications. The medical reports revealed the presence of neither neurofibromas nor café-au-lait spots. The intracranial meningiomas were operated on, and the pathological diagnoses were WHO grade 1 meningotheliomatous and psammomatous types. Two patients with unexpected diagnoses were operated on three times; their diagnoses were eccrine cell carcinoma and sebaceous carcinoma. Both patients were further evaluated following their first histopathological reports. The mean number of surgeries per patient was 1.18 in this study.
MR scans of the patient with multiple scalp masses; T2-weighted axial (a and b) and sagittal MR (c) images revealed a mass lesion (meningioma) at the frontal base with bilaterally dispersed multiple scalp masses. Moreover, a coronal postcontrast MR image showed another mass lesion (meningioma) at the medial sphenoid wing with associated scalp masses at the vertex (d)
The list of histological diagnoses is presented in Table 2. The most common diagnosis was trichilemmal cyst, followed by epidermal cyst, lipoma, nevus and sebaceous cyst. These five diagnoses constituted about 77.1 % of the cases. The tumors originating from cutaneous appendages (trichilemmal cyst, pilomatrixoma, sebaceous cyst, sebaceous carcinoma, apocrine mixed tumor, syringocystadenoma, hidradenoma, eccrine cell carcinoma, nevus sebaceous) constituted almost half of the cases (49 %). A total of 82.3 % (284/345) of the lesions originated from skin components, the epidermis or cutaneous appendages. The rest were tumors of fat tissue (lipomas), muscles, cartilage, bones (osteoma and bone lesions), neuronal and neuroendocrine components (neurofibroma, Merkel cell carcinoma), vascular tissue (hemangioma, angiosarcoma), proliferation of fibrous or related tissues (dermatofibrosarcoma protuberans), cutaneous metastases or cutaneous lymphoid infiltrations (lymphoma).
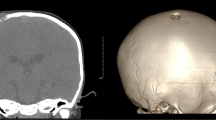
The patients with eccrine cell carcinoma and dermatofibrosarcoma protuberans were primarily operated on by neurosurgeons according to an initial preoperative diagnosis of lipoma. Then, plastic surgery consultations were performed as the pathological diagnoses were made. Two patients had cranial vault lymphoma in the series; one was initially operated on by plastic surgeons and the other by general surgeons. Then, both patients were consulted to neurosurgery. One of the meningioma cases was referred from the general surgery department because of a large, immobile mass in the frontal region. Further radiological evaluations showed this mass lesion was growing over the dura toward the skull; the histopathological diagnosis was meningioma (Figs. 2 and 3).
Overall, there was a large discrepancy between the initial and histopathologically confirmed diagnoses of the lesions (Tables 3 and 4). In the series, preoperative diagnoses were not even specified by the surgeons in 53 % of the patients. On the other hand, if specified, the preoperative diagnoses were correct in just 13–27 % of the cases with respect to the departments (Table 3).
From the histopathological perspective, there were 32 distinct diagnoses in the pathological reports; however, 19 (59.3 %) of the diagnoses were not suspected even once in 345 patients in the preoperative period (Table 4). In the five most common lesions, the rate of correct preoperative diagnosis was 16.1 %. The figure was increased in dermatological malignancies such as SCC and basal cell carcinoma (BCC), which were correctly diagnosed in 83.3 % (5/6) and 40 % (4/10) of the cases at the preoperative period, respectively.
The series included some pathologies needing further follow-up, such as BCC (10 cases), SCC (6 cases), lymphoma (2 cases), meningioma (2 cases), dermatofibrosarcoma protuberans (1 case), eccrine cell carcinoma (1 case), fibrous dysplasia (1 case), Merkel cell carcinoma (1 case), metastases (1 case), sebaceous carcinoma (1 case) and angiosarcoma (1 case). The overall rate of these lesions was 7.8 % (27/ 345).
Discussion
Scalp masses, although very common in daily practice, are one of the ignored types of pathologies with respect to management. Not much consideration is given before intervening with these potentially troublesome lesions. Careful examination and even radiological evaluation in selected cases are warranted because the external appearance can mislead doctors, who think that they are dealing with a benign entity.
Sudhakar et al. presented the case of a 42-year-old female patient with two separate lesions (supposedly a sebaceous cyst), one in the canthal area and the other in the right temporoparietal region of the scalp. The lesion was operated on with a resulting intracerebral hematoma because of the unknown skull defect of an epidermal cyst.
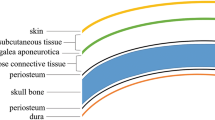
The etiology of a scalp mass can mainly be evaluated under two headings with respect to the site of origin: “superficial” causes including lesions arising from cutaneous and subcutaneous tissues such as BCC and lipoma or “deeper” causes such as a bone tumor or intracranial pathology. Thus, a clinician should take this perspective into consideration when dealing with a scalp mass, which can be a reflection of a clinically significant pathology in the intracranial region such as meningioma.
In the present series, 82.3 % of the lesions originated from skin components; trichilemmal cysts (also known as pilar cysts) constituted almost half of these lesions (40.6 %) in our study. This result was not surprising because trichilemmal cysts are reported to affect 5–10 % of the population and mostly occur on the scalp with a benign nature [4, 9]. However, the rate of preoperative correct diagnosis was still 7.14 %.
Moreover, there are some distinct pathological subtypes for these common lesions such as “proliferating” trichilemmal cyst, observed in 2 % of the cases. In this subtype, gradual enlargement and locally aggressive behavior with recurrences and seldom with metastases can be seen [11]. Although we could not define any association, some carcinomas, e.g., Merkel cell carcinoma, were correlated to trichilemmal cysts [7]. With respect to our series, the proliferating subtype was seen in 3.5 % (5/140) of the trichilemmal cysts. The incidence is a little higher than in the literature. This may be related to geographical and ethnic differences.
Besides, malignant skin tumors may also arise from the surface epithelium or its cutaneous appendages. In a report of 25 scalp carcinomas, almost half were BCCs (48 %), followed by SCCs (32 %), adnexal carcinoma, Merkel cell carcinoma and metastases [6]. These tumors occur rarely in the scalp; however, in general, unless promptly identified and managed, tumors of the scalp will grow rapidly and infiltrate the underlying cranium and occasionally the dura.
In our series, eccrine cell carcinoma, apocrine tumors and dermatofibrosarcoma protuberans were initially operated on by neurosurgeons. One patient with BCC and two patients with SCC were operated on by general surgeons at first. These figures show that various scalp lesions can be operated on by surgeons in different departments. However, particularly for malignant lesions, aggressive surgical removal of the lesion with its surrounding soft tissues, skull and dura might be the best management [6]. Therefore, even if it seems trivial to discuss, scalp masses originating from skin components, even trichilemmal cysts, should be familiar to neurosurgeons and other involved departments; a multidisciplinary approach is warranted.
Scalp masses may also raise suspicion for an underlying process involving the skull and intracranial compartment. There were 11 cases (3.2 %) (2 lymphomas, 2 meningiomas, 1 fibrous dysplasia, 1 angiosarcoma and 1 metastasis) in the series that initially presented as a scalp mass before causing symptoms related to the primary process (Figs. 2 and 3).
Lymphoma cases were operated on by plastic and general surgeons before neurosurgeons. Lymphoma in the central nervous system is familiar to neurosurgeons. However, primary lymphoma in the cranial vault is quite rare. The overall reported rate of non-Hodgkin lymphoma originating from bone tissue is 3–4 % [2, 3]. Fukushima presented a review reporting 15 cases. In six (40 %) of these patients, the initial presenting symptom was only a mass on the scalp [2]. Similar to the literature, our patients also presented with painless scalp masses without any neurological deficits [1, 2, 5]. However, since the preoperative unawareness of the diagnosis, the second patient has undergone an aggressive surgery with removal of both extracranial and intracranial components. This patient had an early recurrence of scalp lesions in 3 weeks and received chemotherapy and radiotherapy afterwards. In this case, the authors questioned whether preoperative awareness of the diagnosis would have changed the initial management strategy. This patient may exemplify the importance of a preoperative multidisciplinary approach, helping the surgical team in accurate management of the patient [1–3].
The overall incidence of “clinically significant” lesions was around 7.8 % in our series. Among these, some cases did not even resemble a significant lesion at the preoperative period. Information about the personal history (such as presence of a known malignancy, duration of the lesion), physical examination, particularly the external appearance (such as a punctum of an epidermal cyst, telangiectasia of BCC), mobility, consistency and number of lesions is important. Further diagnostic studies (radiological imaging) and consultations with a multidisciplinary vision may be crucial. Radiological evaluation would be best for defining any bone involvement and other associated lesions in patients having multiple or extensive scalp masses with firm consistency and immobile on palpation. Our empirical experience suggested that the preoperative workup including radiological evaluation is important in all cases of scalp masses in order to avoid many problems such as multiple surgical interventions.
In this study, we observed that more than half of the diagnoses (19/32, 59.3 %) were not considered among the possible preoperative diagnoses even once in 345 patients. This might indicate the unfamiliarity of the surgeons with the differential diagnosis of scalp masses. Moreover, high rates of initial misdiagnosis might be associated with underestimation of the clinical significance of these lesions. The surgeons involved in the management of scalp masses should be familiar with the differential diagnosis of these lesions, which can be variable and sometimes challenging, necessitating a multidisciplinary approach.
Indications for surgery when dealing with a scalp mass should be clearly determined. Necessary consultations should be considered with respect to the preoperative diagnosis. An algorithmic approach might be useful in accurate management. Future studies are needed in this regard.
In this study, the number of metastases was quite low, and some pathologies such as malignant melanoma were even not encountered. This may be attributed to the specific outlook of malignant melanoma rendering an initial diagnosis other than a scalp mass. In case of metastases, although the scalp is one of the most common sites for metastasis, our study detected only one case with a metastasis. This was questioned by the authors; however, the exact cause could not been determined. Still, the authors believe that the possibility of metastasis should always be kept in mind when considering a mass in the scalp, especially at an older age. The metastasis can present as dermal or subcutaneous nodules, which can be solitary or multiple. Moreover, another limitation of our study is that only scalp masses that were thought to be eligible for surgical removal or necessary for histopathological examination could be reached because of the design of this study. Thus, there is also a need for a prospective study in order to determine the exact frequency of causes of scalp masses.
References
Duyndam DA, Biesma DH, van Heesewijk JP (2002) Primary non-Hodgkin’s lymphoma of the cranial vault; MRI features before and after treatment. Clin Radiol 57:948–950
Fukushima Y, Oka H, Utsuki S, Nakahara K, Fujii K (2007) Primary malignant lymphoma of the cranial vault. Acta Neurochir 149:601–604
Herkes GK, Partington MD, O’Neil BP (1991) Neurological features of cranial vault lymphomas: report of two cases. Neurosurgery 29:898–901
James WD, Berger TG, Elston DM (2011) Andrews’ Diseases of the Skin: Clinical Dermatology. Saunders Elsevier, Philadelphia, PA
Kanai M, Kawano K, Murakami T, Saitou M, Kikumoto N (2003) A case of malignant lymphoma of the cranial vault. No Shinkei Geka 31:419–424
Soma PF, Chibbaro S, Makiese O, Marsella M, Diemidio P, Fricia M, Passanisi M, Catania V, Sirago P, Ventura F (2008) Aggressive scalp carcinoma with intracranial extension: A multidisciplinary experience of 25 patients with long-term follow-up. J Clin Neurosci 15:988–992
Su W, Kheir SM, Berberian B, Cockerell CJ (2008) Merkel cell carcinoma in situ arising in a trichilemmal cyst: a case report and literature review. Am J Dermatopathol 30:458–461
Sudhakar N, Stephenson GC (2004) Swelling on the head, a forgotten lesson: a case report of an intradiploic epidermal cyst with an iatrogenic complication. Br J Oral Maxillofac Surg 42:155–7
Thomas VD, Snavely NR, Lee KK, Swanson NA (2012) Benign Epithelial Tumors, Hamartomas, and Hyperplasias. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K (eds) Fitzpatrick’s Dermatology in General Medicine. McGraw-Hill, New York, NY, p 1334
Yoon SH, Park SH (2008) A Study of 77 cases of surgically excised scalp and skull masses in pediatric patients. Childs Nerv Syst 4:459–465
Weiss J, Heine M, Grimmel M, Jung EG (1995) Malignant proliferating trichilemmal cyst. J Am Acad Dermatol 32:870–873
Conflicts of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership or other equity interest; and expert testimony or patent-licensing arrangements) or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Türk, C.Ç., Bacanlı, A. & Kara, N.N. Incidence and clinical significance of lesions presenting as a scalp mass in adult patients. Acta Neurochir 157, 217–223 (2015). https://doi.org/10.1007/s00701-014-2266-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2266-7