Abstract
Purpose
This study identified the relationship between postoperative pneumonia and preoperative sarcopenia as well as the factors for preoperative sarcopenia in patients with esophageal cancer.
Methods
In this retrospective, single-center, observational study, we evaluated the data of 274 patients who were scheduled for thoracoscopic-laparoscopic esophagectomy. Sarcopenia was defined using the skeletal muscle index, handgrip strength, and gait speed. The physical activity and nutritional status were evaluated. A multivariate logistic regression analysis was performed to confirm the association between sarcopenia and postoperative pneumonia and identify sarcopenia-related factors. A Spearman’s correlation analysis was used to identify the relationship between physical activity and nutritional status.
Results
Age, male sex, sarcopenia, and postoperative recurrent laryngeal nerve palsy were significantly associated with postoperative pneumonia. Age, male sex, physical activity, and nutritional status were significantly associated with preoperative sarcopenia. There was a significant correlation between physical activity and nutritional status.
Conclusions
Preoperative sarcopenia was confirmed to be a predictor of postoperative pneumonia. Furthermore, age, sex, physical activity, and nutritional status were significantly associated with preoperative sarcopenia. Physical activity and nutritional status are closely associated with each other in patients with esophageal cancer. A multidisciplinary approach to preoperative sarcopenia, taking exercise and nutrition into account, is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer is one of the most common malignancies and has a poor prognosis despite advancements in treatment [1, 2]. Esophagectomy is the mainstay of curative therapy for locoregional diseases. Although the adoption of minimally invasive esophagectomy (MIE), such as thoracoscopic–laparoscopic esophagectomy (TLE), is increasing, postoperative pulmonary complications continue to occur [3], among which postoperative pneumonia adversely affects overall survival [4]. Therefore, preventing postoperative pneumonia is essential.
Previous studies have demonstrated that age, the pulmonary function, and recurrent laryngeal nerve palsy are associated with postoperative pneumonia [5,6,7]. However, in recent years, studies have demonstrated that preoperative sarcopenia, defined as a progressive and generalized skeletal muscle disorder characterized by an accelerated loss of muscle mass and function [8], is also associated with postoperative pneumonia [9, 10]. Reports involving MIE are lacking, and limited studies have used the revised criteria proposed by the 2019 Asian Working Group for Sarcopenia (AWGS) [11], as recommended in the assessment of sarcopenia. Therefore, further studies are necessary to address these limitations.
Sarcopenia is caused by advanced age, malnutrition, inactivity, comorbid diseases, and iatrogenic problems [8]. A previous study described the clinical characteristics of sarcopenia, including advanced age, advanced cancer, histopathology, low albumin levels, presence of pulmonary disease, and the type of neoadjuvant treatment, in patients with esophageal cancer [9]. However, that study only reported the characteristics of patients with preoperative sarcopenia and did not perform a factor analysis. Furthermore, no studies, to our knowledge, have evaluated preoperative sarcopenia in patients with esophageal cancer with consideration of physical activity, which is considered a reversible factor. Therefore, effective interventions for preoperative sarcopenia in patients with esophageal cancer remain unclear.
Given the above, the present study explored whether or not sarcopenia, as defined by the AWGS 2019, is a predictor of pneumonia after MIE and identified significant factors associated with preoperative sarcopenia that might aid in establishing effective strategies for the management of preoperative sarcopenia in patients with esophageal cancer.
Methods
Study design and population
This retrospective, single-center, observational study was conducted at the National Cancer Center Hospital (NCCH). Ethical approval was obtained from the Institutional Review Board of the NCCH (approval number: 2017–061). All procedures performed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the 1964 Declaration of Helsinki and its later versions. Informed consent for inclusion in this study or an equivalent alternative was obtained from all patients.
Patients with esophageal cancer who were scheduled for TLE between May 2017 and December 2020 were enrolled in this study. The inclusion criteria were as follows: (1) a diagnosis of esophageal cancer, (2) scheduled for TLE, and (3) available for an evaluation. Patients unable to undergo scheduled TLE were excluded from the analysis.
Measurements
General and clinical information (age, sex, body mass index [BMI], histopathology, clinical stage, neoadjuvant treatment, C-reactive protein [CRP] and hemoglobin levels, pulmonary function, and smoking history) was collected from the patients’ medical records. The percentage of forced expiratory volume in 1 s (FEV1.0%) was used to evaluate pulmonary function. The smoking status was defined as being either a current smoker (cessation within one year before the surgery) or a noncurrent smoker (cessation more than one year before the surgery or never smoked). The comorbidities included chronic pulmonary diseases (chronic obstructive pulmonary disease, asthma, or interstitial lung disease), diabetes mellitus, cardiovascular disease, hepatobiliary disease, and chronic kidney disease. The clinical stage was categorized as IA–IIB or IIIA–IV based on the seventh tumor-node-metastasis classification of the Union for International Cancer Control. Neoadjuvant treatment was chemotherapy or chemoradiotherapy. Postoperative pneumonia was defined as the presence of new or progressive infiltrates on chest radiographs or computed tomography (CT) and meeting at least two of the following three criteria: body temperature > 38 °C, leukopenia or leukocytosis (white blood cell count < 4 × 109/L or > 10 × 109/L), and purulent sputum. Postoperative complications occurring within 30 days of the surgery were coded as a Clavien–Dindo grade ≥ 2. As an exception, recurrent laryngeal nerve palsy, including Clavien–Dindo complications, was classified as grade ≥ 1 [12].
The participants were evaluated for sarcopenia, the nutritional status, and physical activity before TLE.
Sarcopenia definition
Sarcopenia was diagnosed based on an algorithm from a previous study [13]. Muscle strength and physical performance were determined according to the AWGS 2019 criteria [11]. Muscle strength was measured by handgrip strength using a digital dynamometer (T.K.K.5401; Takei Scientific Instruments Co., Ltd., Niigata, Japan). Low muscle strength was defined as a handgrip strength of < 28 kg in males and < 18 kg in females. Low physical performance was measured according to the usual gait speed with a cut-off of < 1.0 m/s [11]. Skeletal muscle mass was measured using CT, which is often performed in patients with esophageal cancer. Skeletal muscle mass was calculated using the Image J software program, a free public domain program developed by the National Institutes of Health. Calculations were based on cross-sectional CT images taken at the level of the third lumbar vertebra (L3) before TLE was performed. The skeletal muscle at the L3 level correlates with appendicular skeletal muscle mass [14]. The skeletal muscle index (SMI) was calculated by normalizing the cross-sectional areas for height (cm2/m2). A low muscle mass was defined as an SMI ≤ 52.4 cm2/m2 for males and ≤ 38.5 cm2/m2 for females [15]. In the present study, moderate sarcopenia was defined as (1) low skeletal muscle mass or (2) low handgrip strength and/or low gait speed. Severe sarcopenia was defined as a low skeletal muscle mass, low muscle strength, and low physical performance.
Nutritional status
A two-step approach was selected for the diagnosis of the nutritional status according to the Global Leadership Initiative in Malnutrition (GLIM) criteria [16]. First, patients at risk of malnutrition were identified using a subjective global assessment [17]. Second, the diagnosis of malnutrition was confirmed when at least one of the three phenotypic criteria (non-volitional weight loss, low BMI, and reduced muscle mass) and one of the two etiologic criteria (reduced food intake or assimilation and inflammation or disease burden) were met. Regarding the phenotypic criteria, a low BMI was defined as < 20 kg/m2 for subjects < 70 years old and < 18.5 kg/m2 for those ≥ 70 years old, according to a consensus report. Weight loss was defined as a reduction of > 5% within 6 months before the surgery or > 10% beyond 6 months [16]. The cut-off value for a reduced muscle mass was based on the SMI in a previous study [15]. Regarding the etiologic criteria, a reduced food intake or assimilation was defined as consuming 50% of the energy requirements for > 1 week, any reduction in food intake for > 2 weeks, or any chronic gastrointestinal condition that adversely affects food assimilation or absorption. Finally, inflammation was defined as a CRP level of > 0.5 mg/dL [16, 18]. The severity of malnutrition was classified as moderate or severe, according to the phenotypic criteria [16].
Thus, the nutritional status of the patients was classified into three groups: well-nourished, moderate malnutrition, and severe malnutrition according to the GLIM criteria.
Physical activity
A study reported that 150–300 min/week of moderate-intensity aerobic activity or 75–150 min/week of vigorous-intensity aerobic activity is recommended [19]. In the present study, the participants were preoperatively classified into two groups (high and low physical activity). Patients who achieved ≥ 150 min of moderate-intensity aerobic activity per week were placed in the high physical activity group, while those who did not meet the cut-off were placed in the low physical activity group.
Statistical analyses
Data were analyzed using the IBM SPSS Statistics version 26.0 software program (IBM Corp., Armonk, NY, USA). The characteristics of the non-sarcopenia, moderate sarcopenia, and severe sarcopenia groups were compared. Data were analyzed using the Kruskal–Wallis test with the Bonferroni test. Categorical data were analyzed using the chi-square test for between-group comparisons. A univariate logistic regression analysis was performed to identify the association between various factors and moderate or severe sarcopenia. Variables with significance in the univariate analysis were included in the multivariate model. The factors affecting postoperative pneumonia were also analyzed using univariate and multivariate logistic regression analyses. A Spearman’s correlation analysis was performed to identify the relationship between physical activity and nutritional status. Statistical significance was set at P < 0.05.
Data are expressed as the median (interquartile range [IQR]) or number and percentage of participants.
Results
Patient demographic and clinical characteristics
A total of 274 patients with esophageal cancer participated in this study. Table 1 shows their demographic and clinical characteristics. The median age was 65.5 (58.0–71.0) years old. Of these patients, 198 (72.3%) and 2 (0.7%) received neoadjuvant chemotherapy and chemoradiotherapy, respectively. Postoperative pneumonia occurred in 55 patients (20.1%). There were 55 patients with malnutrition (moderate malnutrition, n = 27, 9.9%; severe malnutrition, n = 28, 10.2%), and 95 (34.7%) had low physical activity. The median handgrip strength was 33.1 (26.5–38.4) kg, gait speed was 1.24 (1.09–1.39) m/sec, and SMI was 47.0 (41.4–51.8) cm2/m2. The patients were classified into groups of non-sarcopenia (n = 70, 25.5%), moderate sarcopenia (n = 166, 60.6%), and severe sarcopenia (n = 38, 13.9%). Compared with the patients in the non-sarcopenia and moderate sarcopenia groups, the patients with severe sarcopenia were significantly older; had a significantly lower FEV1.0%, hemoglobin levels, handgrip strengths, and gait speeds; and had significantly higher CRP levels. Patients with severe and moderate sarcopenia had significantly lower BMI and SMI values than those without sarcopenia. Physical activity levels, fulfillment of the GLIM criteria, and occurrences of postoperative pneumonia were significantly different among the three groups.
Factors associated with postoperative pneumonia
In the univariate logistic regression analysis, age, sex, sarcopenia, and postoperative recurrent laryngeal nerve palsy were identified as potentially significant factors (P < 0.05). In the multivariate logistic regression analysis of these significant variables, age, sex, sarcopenia, and postoperative recurrent laryngeal nerve palsy were also significantly associated with postoperative pneumonia (Table 2).
Factors associated with sarcopenia
In the univariate logistic regression analysis, age, sex, hemoglobin level, nutritional status, and physical activity were identified as potentially significant factors (P < 0.05). We included these variables in the multivariate logistic regression analysis, which revealed that age, sex, nutritional status, and physical activity were significantly associated with sarcopenia (Table 3).
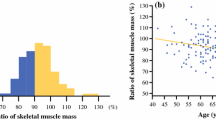
Relationship between physical activity and the nutritional status
A Spearman’s correlation analysis revealed a significant correlation between physical activity and nutritional status (r = 0.245, P < 0.001). The levels of physical activity were significantly different among the three groups classified by nutritional status using the GLIM criteria (P < 0.001). Among well-nourished patients, 156 (71.2%) and 63 (28.8%) had high and low physical activity, respectively. In contrast, among patients with moderate malnutrition, 11 (40.7%) and 16 (59.3%) had high and low levels of physical activity, respectively. Among patients with severe malnutrition, 12 (42.9%) and 16 (57.1%) had high and low physical activity levels, respectively (Fig. 1).
Discussion
Preoperative sarcopenia in esophageal cancer is a well-known predictor of postoperative pneumonia [9, 10]. However, few reports have involved MIE, and fewer still have employed the AWGS 2019 criteria [11], which are recommended for the assessment of sarcopenia. Furthermore, which factors lead to preoperative sarcopenia in patients with esophageal cancer is unclear. To our knowledge, this is the first study to evaluate the factors associated with preoperative sarcopenia in patients with esophageal cancer. We found that physical activity and nutritional status were independent factors significantly associated with preoperative sarcopenia.
Given the lack of studies focusing on MIE and the prevalent use of single assessments of muscle mass for diagnosing sarcopenia, in this study, we evaluated sarcopenia in patients who were scheduled for TLE using the cut-off specified by AWGS 2019 [9]. Our results showed that preoperative sarcopenia is an independent predictor of postoperative pneumonia. A previous study demonstrated that sarcopenia, as defined by the AWGS 2019, is an independent risk factor for pneumonia after MIE [13], which supports our results. It is clear that sarcopenia is a useful predictor of pneumonia after MIE, even when a systematic approach to sarcopenia assessment is used. These findings emphasize the importance of perioperative management of sarcopenia, even in patients undergoing minimally invasive procedures.
The factors that contribute to sarcopenia are generally related to age, malnutrition, inactivity, disease, and iatrogenic factors [8]. Patients with cancer are exposed to various cancer- and noncancer-specific degenerative factors that cause sarcopenia characterized by muscle dysfunction [20]. In particular, in patients with preoperative esophageal cancer, several possible factors, such as cancer and its symptoms, malnutrition, and preoperative treatment, may cause sarcopenia. Among these factors, we found that age, sex, nutritional status, and physical activity were independently associated with preoperative sarcopenia. Sarcopenia is common in older patients with cancer given their susceptibility to the effects of cancer progression and treatment [21]. Previous studies on patients with cancer have also reported that the male sex influences the development of sarcopenia [22]. Although the reasons for this association are unclear, these previous results support our findings.
Physical inactivity accelerates the loss of muscle mass and strength through disuse-induced muscle fiber loss and decreased activation of the motor units [23]. Physical activity is often reduced in patients with cancer. Kong et al. showed that sarcopenia was associated with low physical activity in patients with preoperative lung cancer [24]. Although the importance of physical activity for sarcopenia has already been demonstrated, the effect of physical activity on sarcopenia in patients with preoperative esophageal cancer has not been elucidated. One study on esophageal cancer reported that systemic inflammatory markers were significantly associated with sarcopenia in patients undergoing definitive radiotherapy [15]. However, no studies have focused on patients scheduled for surgery, which is the standard treatment for esophageal cancer. Furthermore, there are no multifaceted studies that include physical activity. Therefore, our finding that physical activity is a significant factor associated with preoperative sarcopenia is novel.
Malnutrition is common in patients with cancer [25]. Esophageal cancer is a malignancy with one of the highest risks of malnutrition [26]. Before their diagnosis, 80% of patients with esophageal cancer experience unintentional weight loss of over 10%–15% caused by reduced food intake resulting from dysphagia [27]. In addition, increased energy consumption caused by tumor-induced systemic inflammation enhances weight loss [28]. This is a potential cause of malnutrition in patients with esophageal cancer, and malnutrition and sarcopenia are closely related [29]. The nutritional status has been reported to be an independent factor for muscle strength [30], muscle mass [31], and gait speed [32]. These studies support our finding that malnutrition is a significant factor in preoperative sarcopenia.
Establishing an effective intervention strategy for sarcopenia, a predictor of postoperative pneumonia, is crucial. Based on our results, a low physical activity and poor nutritional status are important factors to take into account when considering intervention, as they are reversible. Furthermore, it is worth noting that a significant correlation was found between physical activity and nutritional status, and low physical activity was prevalent in patients with malnutrition. Previous studies have not shown an association between physical activity and the nutritional status in patients with esophageal cancer before surgery, so we believe that the present results will prove useful for planning preoperative intervention and provide a basis for intervention. Physical activity and nutrition being separately extracted as risk factors suggest the need for interventions that consider both factors. Although the level of evidence is low, preoperative nutritional assessment/intervention and rehabilitation for esophageal cancer are moderate to strongly recommend [33]. Regarding nutrition, nutritional assessments should be performed on all patients to detect and optimize nutritional status before surgery. Nutritional intervention should be based on the level of risk. Those perceived to be at low risk should be given dietary advice. Moderate-risk patients should be given protein and energy supplements, and enteral support should be considered for those at high risk, commonly with tube feeding. These measures have been shown to improve patient outcomes [34]. Regarding rehabilitation, exercise therapy combining aerobic and resistance exercises has been shown to have an impact on physical function [35]. Furthermore, it is suggested that an approach that includes instructions and patient education that directly improves physical activity is also important. We were unable to establish a causal relationship between physical activity and nutritional status in this study. However, it is important to adopt a multidisciplinary approach to address preoperative sarcopenia [36], considering both nutrition and exercise, as this will improve the perioperative outcomes.
Several limitations associated with the present study warrant mention. First, this was a retrospective, observational study involving patients from a single institution, which might have caused patient selection bias. Second, physical activity was not evaluated using objective devices, such as pedometers. Therefore, details regarding the duration and type of physical activity were not available. Third, we measured the L3 CT-based SMI to estimate the skeletal muscle mass, even though the AWGS criteria advocate performing such measurements using a bioelectrical impedance analysis.
Conclusion
Preoperative sarcopenia in esophageal cancer was confirmed to be a predictor of postoperative pneumonia in this study. Furthermore, age, sex, physical activity level, and nutritional status were demonstrated to be significantly associated with sarcopenia. Malnutrition and physical inactivity are closely associated with each other in patients with esophageal cancer. A multidisciplinary approach to preoperative sarcopenia, taking nutrition and exercise into account, was suggested.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–36.
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. 2014;260:259–66.
Fujishima S, Tsujimoto H, Nagata K, Sugasawa H, Nomura S, Ito N, et al. Postoperative pneumonia causes the loss of skeletal muscle volume and poor prognosis in patients undergoing esophagectomy for esophageal cancer. Gen Thorac Cardiovasc Surg. 2021;69:84–90.
Scholtemeijer MG, Seesing MFJ, Brenkman HJF, Janssen LM, van Hillegersberg R, Ruurda JP. Recurrent laryngeal nerve injury after esophagectomy for esophageal cancer: incidence, management, and impact on short- and long-term outcomes. J Thorac Dis. 2017;9:S868–78.
Law S, Wong KH, Kwok KF, Chu KM, Wong J. Predictive factors for postoperative pulmonary complications and mortality after esophagectomy for cancer. Ann Surg. 2004;240:791–800.
Avendano CE, Flume PA, Silvestri GA, King LB, Reed CE. Pulmonary complications after esophagectomy. Ann Thorac Surg. 2002;73:922–6.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Wang PY, Xu LD, Chen XK, Xu L, Yu YK, Zhang RX, et al. Sarcopenia and short-term outcomes after esophagectomy: a meta-analysis. Ann Surg Oncol. 2020;27:3041–51.
Kurita D, Oguma J, Ishiyama K, Hirano Y, Kanamori J, Daiko H. Handgrip strength predicts postoperative pneumonia after thoracoscopic-laparoscopic esophagectomy for patients with esophageal cancer. Ann Surg Oncol. 2020;27:3173–81.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 Consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300-7.e2.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Wang PY, Chen XK, Liu Q, Yu YK, Xu L, Liu XB, et al. Highlighting sarcopenia management for promoting surgical outcomes in esophageal cancers: Evidence from a prospective cohort study. Int J Surg. 2020;83:206–15.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
Liang H, Peng H, Chen L. Prognostic value of sarcopenia and systemic inflammation markers in patients undergoing definitive radiotherapy for esophageal cancer. Cancer Manag Res. 2021;13:181–92.
Jensen GL, Cederholm T, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. JPEN J Parenter Enteral Nutr. 2019;43:32–40.
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987;11:8–13.
Einarsson S, Laurell G, Tiblom EY. Mapping the frequency of malnutrition in patients with head and neck cancer using the GLIM criteria for the diagnosis of malnutrition. Clin Nutr ESPEN. 2020;37:100–6.
Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, et al. American college of sports medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc. 2019;51:2391–402.
Christensen JF, Jones LW, Andersen JL, Daugaard G, Rorth M, Hojman P. Muscle dysfunction in cancer patients. Ann Oncol. 2014;25:947–58.
Ligibel JA, Schmitz KH, Berger NA. Sarcopenia in aging, obesity, and cancer. Transl Cancer Res. 2020;9:5760–71.
Pamoukdjian F, Bouillet T, Lévy V, Soussan M, Zelek L, Paillaud E. Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: a systematic review. Clin Nutr. 2018;37:1101–13.
Kawakami Y, Akima H, Kubo K, Muraoka Y, Hasegawa H, Kouzaki M, et al. Changes in muscle size, architecture, and neural activation after 20 days of bed rest with and without resistance exercise. Eur J Appl Physiol. 2001;84:7–12.
Kong S, Shin S, Lee JK, Lee G, Kang D, Cho J, et al. Association between sarcopenia and physical function among preoperative lung cancer patients. J Pers Med. 2020;10:166.
Zhang X, Edwards BJ. Malnutrition in older adults with cancer. Curr Oncol Rep. 2019;21:80.
Steenhagen E, van Vulpen JK, van Hillegersberg R, May AM, Siersema PD. Nutrition in peri-operative esophageal cancer management. Expert Rev Gastroenterol Hepatol. 2017;11:663–72.
Riccardi D, Allen K. Nutritional management of patients with esophageal and esophagogastric junction cancer. Cancer Control. 1999;6:64–72.
Martin L, Lagergren P. Long-term weight change after oesophageal cancer surgery. Br J Surg. 2009;96:1308–14.
Souza BU, Souza NCS, Martucci RB, Rodrigues VD, Pinho NB, Gonzalez MC, et al. Factors associated with sarcopenia in patients with colorectal cancer. Nutr Cancer. 2018;70:176–83.
Norman K, Stobäus N, Smoliner C, Zocher D, Scheufele R, Valentini L, et al. Determinants of hand grip strength, knee extension strength and functional status in cancer patients. Clin Nutr. 2010;29:586–91.
Fukushima T, Nakano J, Ishii S, Natsuzako A, Sato S, Sakamoto J, et al. Factors associated with muscle function in patients with hematologic malignancies undergoing chemotherapy. Support Care Cancer. 2020;28:1433–9.
Mendes J, Borges N, Santos A, Padrão P, Moreira P, Afonso C, et al. Nutritional status and gait speed in a nationwide population-based sample of older adults. Sci Rep. 2018;8:4227.
Low DE, Allum W, De Manzoni G, Ferri L, Immanuel A, Kuppusamy M, et al. Guidelines for perioperative care in esophagectomy: Enhanced recovery after surgery (ERAS®) society recommendations. World J Surg. 2019;43:299–330.
Ligthart-Melis GC, Weijs PJ, te Boveldt ND, Buskermolen S, Earthman CP, Verheul HM, et al. Dietician-delivered intensive nutritional support is associated with a decrease in severe postoperative complications after surgery in patients with esophageal cancer. Dis Esophagus. 2013;26:587–93.
Minnella EM, Awasthi R, Loiselle SE, Agnihotram RV, Ferri LE, Carli F. Effect of exercise and nutrition prehabilitation on functional capacity in esophagogastric cancer surgery: a randomized clinical trial. JAMA Surg. 2018;153:1081–9.
Stephens MR, Lewis WG, Brewster AE, Lord I, Blackshaw GR, Hodzovic I, et al. Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus. 2006;19:164–71.
Acknowledgements
The authors thank the members of the Department of Musculoskeletal Oncology and Rehabilitation and Esophageal Surgery, National Cancer Center. This research would not have been possible without their leadership and cooperation.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Fukushima T, Watanabe N, Okita Y, Yokota S, Kojima K, Matsuoka A, Kurita D, Ishiyama K, Oguma J, Kawai A, and Daiko H declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fukushima, T., Watanabe, N., Okita, Y. et al. The evaluation of the association between preoperative sarcopenia and postoperative pneumonia and factors for preoperative sarcopenia in patients undergoing thoracoscopic-laparoscopic esophagectomy for esophageal cancer. Surg Today 53, 782–790 (2023). https://doi.org/10.1007/s00595-022-02620-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02620-6