Abstract
Purpose
To evaluate the efficacy and safety of the enhanced recovery after surgery (ERAS) protocol and quantify the impact of each ERAS item on postoperative outcomes.
Methods
We used a generalized linear model to compare 289 colorectal cancer patients treated with the ERAS protocol between June, 2015 and April, 2021, with 99 colorectal cancer patients treated with the conventional colorectal surgery pathway between April, 2014 and June, 2015.
Results
The median length of hospital stay (LOHS) was significantly shorter in the ERAS group, at 9 days (range 3–104 days) vs. 14 days (range 4–44 days) (p < 0.001), but the complication rates (Clavien–Dindo grade 2 or more) were similar (16.6% vs. 22.2%; p = 0.227). However, in the ERAS group, the higher the compliance with ERAS items, the lower the complication rate and LOHS (both p < 0.001). Multiple regression analysis demonstrated that "Discontinuation of continuous intravenous infusion on POD1" and "Avoidance of fluid overload" were significantly associated with the LOHS (p < 0.001 and p = 0.008).
Conclusion
The ERAS protocol is safe and effective for elective colorectal cancer surgery, and compliance with the ERAS protocol contributes to shorter LOHS and fewer complications. Items related to perioperative fluid management had a crucial impact on these outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The enhanced recovery after surgery (ERAS) protocol is a comprehensive treatment plan that incorporates a set of techniques proven to maintain physiological function and promote the recovery of postoperative patients. Previous studies have shown that the ERAS protocol facilitates a smooth transition to discharge without increasing postoperative complication rates [1]. ERAS compliance is related to complication rates and length of hospital stay (LOHS) [1,2,3,4,5,6], but the relevance and contribution of each item on the ERAS is unclear. It is understood that as many items as possible promote postoperative recovery, but which ERAS items play a more important role has not been elucidated. Thus, a detailed analysis of the independent contributions of ERAS items to postoperative outcomes is necessary. In this study, we evaluated the efficacy and safety of the ERAS protocol, as well as the impact of compliance with each ERAS item, on postoperative outcomes, especially complication rates and LOHS.
Methods
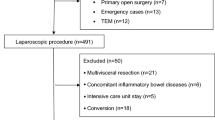
Patient eligibility
We compared the results of 289 colorectal cancers treated with the ERAS protocol between June, 2015 and April, 2021, with those of 99 colorectal cancers treated with the conventional colorectal surgery pathway between April, 2014 and June, 2015.
Items in perioperative routines from the ERAS protocol
Table 1 lists the items from the ERAS that were applied in perioperative routines. Postoperative nausea and vomiting (PONV) measures were originally based on the four major risk factors proposed by Apfel et al. [7]: female gender, history of motion sickness and PONV, non-smoker, and postoperative opioid use. We implemented PONV countermeasures based on the "Consensus guidelines for the management of postoperative nausea and vomiting" [8], which evolved from that proposal. ERAS protocol deviations were defined as an inability to recommence oral food intake on postoperative day (POD) 1, discontinuation of food intake once started, and resumption of continuous infusion [1]. Patients who deviated from the ERAS protocol were also included in the statistical analysis as part of the ERAS protocol group.
Propensity score (PS) matching
A higher proportion of laparoscopy was expected in the ERAS group. Because the laparoscopic surgery group was more recent than the open surgery group, an imbalance in crucial covariates related to outcomes could have biased the estimation of the effect of laparoscopic surgery. To address the selection bias, we performed a PS analysis. The PS included 12 effective covariates, including age, sex, surgical approaches, procedure classification, pathological stage, cardiovascular disease or hypertension, respiratory disease, liver disease, urinary tract disease, diabetes mellitus, cerebral vascular disease, and American Society of Anesthesiologists physical status (ASA-PS). The PS for each patient was estimated using a logistic regression model, and we used the PS to match patients who were treated by the ERAS protocol with corresponding control patients who were treated conventionally. For more plausible matching, we applied one-to-one pair matching. The caliper width for PS matching was 0.2.
Statistical analysis
Data are presented as means and standard deviation or median and range. The Mann–Whitney U test, Pearson’s chi-squared test, or Fisher’s exact test were used to investigate the relationship between the ERAS protocol and conventional care. The association between the clinical variables and LOHS was examined using multiple regression analysis. Logistic regression analysis was also used to examine the association of the clinical variables with complications. Factors were included in the models based on existing knowledge of the factors related to LOHS and with p < 0.05 in the univariate regression analysis. We selected the factors using the forced entry method and likelihood ratios. Multicollinearity among the included variables was examined using variance inflation factors. Factors with p < 0.05 were also considered significant in the multivariate analysis. We conducted this analysis using version 28.0.0 of SPSS software (IBM, NY, USA). To examine the relationship between compliance and overall complications, or between compliance and LOHS, trend analyses were performed using the Jonckheere-Terpstra trend test.
Results
Patient characteristics and perioperative outcomes
Table 2 compares the patient characteristics and perioperative outcomes between the ERAS group and the conventional care group. We found no significant differences in age, gender, colectomy rate, comorbidity, or ASA grade between the groups, but the ERAS group had a significantly higher rate of laparoscopy and a significantly lower median volume of intraoperative fluid. In terms of postoperative outcomes, we found no significant difference in Clavien–Dindo grade, time to first flatus, or time to first stool between the groups, although food intake recommenced significantly earlier in the ERAS group. We also found no significant differences between the groups in the rates of postoperative death, reoperation, or readmission within 30 days after surgery.
As the percentage of laparoscopic surgery was significantly higher in the ERAS group than in the conventional care group, we performed PS matching to compare the perioperative outcomes of 73 patients from both groups with a percentage of laparoscopy of 87.7%. Even after matching, the volume of intraoperative fluid given was significantly less in the ERAS group (median 765 ml [range 80–3800 ml] vs. 1600 ml [500–3400 ml], p < 0.001). In terms of postoperative outcomes, we found no significant difference in Clavien–Dindo grade between the two groups (p = 0.314), although the infusion was discontinued significantly earlier in the ERAS group, on POD 1 [range POD 1–34] vs. POD 3 [1–77]; p < 0.001). LOHS was significantly shorter in the ERAS group at a median of 9 days [range 3–43 days] vs. 12 days [4–44 days]; p < 0.001), and there were no significant differences in the rates of postoperative death, reoperation, or readmission within 30 days after surgery between the groups (p = 1.000, 1.000, and 0.366, respectively).
The accomplishment rate of the ERAS protocol was 77.2% (223/289). Table 3 lists the complications in the two groups. There were no significant differences in the incidences of the major complications of paralytic ileus (p = 0.139), anastomotic leakage (p = 0.769), outlet obstruction (p = 1.000), or port site hernia (p = 0.574).
Compliance with each ERAS intervention
Figure 1 compares compliance with each ERAS intervention between the ERAS protocol and conventional care groups. Compliance rates were much higher in the ERAS group for all items except the use of routine postoperative laxatives because some items that were not part of conventional care were included. These comprised preadmission education, PONV measures, no preoperative mechanical bowel preparation, taking Elental on the day of surgery, sitting upright on the day of surgery, oral intake of 500 ml water on the day of surgery, use of chewing gum on the day of surgery, and giving an oral nutritional supplement on POD1. Giving laxatives from POD1 was forgone in the left-sided colon surgery or rectal surgery in the ERAS group, based on evidence that severe diarrhea on POD1 may cause anastomotic leak.
Relationship between compliance rate and complication rate or LOHS
We compared the complication rate (Fig. 2) and median LOHS (Fig. 3) with the extent to which patients could comply with the ERAS items (< 70% compliance, 70–80%, 80–90%, and > 90%). The higher compliance rate showed a significantly lower complication rate and shorter LOHS (both p < 0.001). To examine the influence on compliance of age, ASA-PS, or surgical procedure, we conducted a subgroup analysis of compliance rates for colectomy ERAS (n = 208) and proctectomy ERAS (n = 81), non-elderly ERAS (< 75 years old, n = 151) and elderly ERAS (≥ 75 years old, n = 138), and ASA-PS of 1 (n = 45) and ASA-PS of 2 or higher (n = 244). We found significant differences between colectomy ERAS and proctectomy ERAS (89.2% vs. 75.0%, p < 0.001), but not between non-elderly ERAS and elderly ERAS patients (85.0% vs. 85.4%, p = 0.991) or ASA-PS of 1 and ASA-PS of 2 or higher (85.5% vs. 85.2%, p = 0.628).
Factors related to complications
Table 4 shows univariate and multivariate analyses of the association between factors and complications. Univariate analysis identified sex, procedure classification (%colectomy), surgical approach (%laparoscopy), operation time ≥ 300 min, discontinuation of the intravenous infusion (c.i.v.) on POD 1, avoidance of fluid overload (intraoperative fluid < 2000 ml), no drain, oral nutritional supplementation on POD 1, routine postoperative laxative, removal of urethral catheter on POD 1, and ambulation on POD 1 as significantly associated with complications. According to binomial logistic regression analysis, "Discontinuation of c.i.v. on POD1" alone was significantly associated with complications (odds ratio = 0.025; 95% confidence interval [CI] 0.009, 0.067; p < 0.001).
Factors related to LOHS
Table 5 shows univariate and multivariate analyses of the association of various factors with the LOHS. Univariate analysis identified sex, procedure classification (%colectomy), surgical approach (%laparoscopy), cerebral vascular disease, operation time ≥ 300 min, discontinuation of c.i.v. on POD1, avoidance of fluid overload (intraoperative fluid < 2000 ml), no drain, oral intake of 500 ml water on the day of surgery, routine postoperative laxative, and removal of the urethral catheter on POD1 as significantly associated with LOHS. Multiple regression analysis was performed in the same way. "Discontinuation of c.i.v. on POD1" and "Avoidance of fluid overload" were significantly associated with LOHS (coefficient = -5.43; 95% CI − 6.74, − 4.12; p < 0.001; and coefficient = − 3.89; 95% CI − 6.76, − 1.01; p = 0.008, respectively). "Discontinuation of c.i.v. on POD1" had a greater impact than "Avoidance of fluid overload" (β = − 0.43 and − 0.17, respectively). The residuals had normal distribution.
Discussion
The findings of this study demonstrated that the ERAS protocol at our hospital was safe and effective for elective colorectal cancer surgery and that greater compliance contributed to shorter LOHS and fewer complications. While these results reconfirm general evidence from previous reports, we also identified the most important ERAS items. Notably, compliance with ERAS items related to perioperative fluid management had a strong influence on these outcomes. We think that identifying this will help facilitate successful implementation of the ERAS protocol in colorectal surgery.
Ota et al. reported that the ERAS protocol can promote early discharge without increasing the complication rate, more effectively than conventional care [1]. Despite reports that stoma creation interfered with postoperative recovery from rectal cancer surgery [9, 10], there was no difference in the proportion of patients in the ERAS group and in the conventional care group, who had a stoma created after PS matching (11 of 73 patients in each group, data not shown). In the present study, compliance with ERAS items correlated with complication rates and LOHS, but the compliance rate may be influenced by other factors, such as age, ASA-PS, or proctectomy. Although proctectomy had a significantly worse compliance rate than colectomy, there was no difference in terms of age and ASA-PS. A detailed analysis of the impact of such factors on compliance rate, accomplishment rate, complication rate, and LOHS will be the subject of future studies.
Although we did not investigate the issue of cost in our study, other reports have shown that the application of ERAS not only shortens the LOHS, but it also reduces costs for patients after colorectal surgery [11] and laparoscopic cholecystectomy [12]. Some studies have focused on the importance of perioperative nutritional management [13], whereas others have focused on perioperative fluid management [14,15,16,17,18,19,20]. The ERAS Compliance Group [2] reported that LOHS can be shortened by preoperative carbohydrate drinks, optimal fluid loading, and intravenous anesthesia instead of epidural anesthesia.
Our results showed that the discontinuation of c.i.v. on POD 1 contributed to reducing the complication rate, and that the avoidance of fluid overload and discontinuation of c.i.v. on POD 1 helped minimize the LOHS. Both of these items are associated with perioperative infusion management. Intraoperative infusion tends to vary among anesthesiologists, probably in consideration of postoperative outcomes [14]. It is thought that administering the appropriate amount of IV fluids without excess or deficiency can shorten the LOHS, reduce costs, and prevent postoperative ileus [15]. In this study, the most prevalent complication was paralytic ileus, which also tended to be more frequent in the conventional care group than in the ERAS group, although the complication rates did not differ significantly between the two groups, being 6.9% vs. 12.1% in the ERAS protocol vs. conventional care groups, respectively; p = 0.139; Table 3). We emphasized the importance of restriction to optimize perioperative fluid infusion. Within the ERAS group, paralytic ileus occurred in only 2 of 226 patients (0.9%) for whom "Discontinuation of c.i.v on POD 1" was achieved, but in 18 of 63 patients (28.6%) for whom it was not achieved (p < 0.001, data not shown). These data suggest that excessive or unnecessary fluid infusion postoperatively may cause bowel edema, leading to reduced bowel peristalsis. Because of the small number of patients in this series, it was not possible to evaluate whether achieving "Discontinuation of c.i.v. on POD1" affected the incidence of other complications.
According to our analysis, avoidance of fluid overload (intraoperative fluid < 2000 ml) was significantly associated with a shorter LOHS (Table 5). As shown in Table 1, the ERAS protocol generally recommends 3 ml/kg/h of intraoperative crystalloid and colloid fluid for low-risk surgery, so there may be skepticism about 2000 ml of intraoperative fluid being the boundary between optimal fluid and volume overload. However, we consider > 2000 ml intraoperative fluid to be excessive, because even when following the 3 ml/kg/h guideline, the intraoperative fluid volume for a 7-h operation on a patient weighing 100 kg, would be 2100 ml. Most of the patients in this series weighed less than 100 kg and the operation times were less than 7 h, so 2000 ml was used as the boundary and > 2000 ml was defined as fluid overload in this study. The multivariate analysis also included an operation time ≥ 300 min as an independent variable, which mitigates the bias by operation time. Fluid overload was unable to be avoided in 15 patients, with a median infusion rate of 4.87 ml/kg/h (range 2.26–8.65 ml/kg/h) and exceeding 4 ml/kg/h in 12. Complications of Clavien–Dindo grade 2 or higher occurred in 10 of these 15 patients, all of which were related to paralytic ileus (data not shown). Considering that the incidence of paralytic ileus in the entire ERAS protocol group was 6.9% (Table 3), the incidence was much higher in patients given intraoperative fluid > 2000 ml. Although maintaining an infusion rate of 3 ml/kg/h for low-risk patients according to the ERAS protocol is ideal, considering the reality of clinical practice, we think that our proposed fluid overload boundary can serve as a simple indicator to prevent excessive infusion in general colorectal cancer surgery.
This study has some limitations. First, it was a single-center retrospective study, and the data collected in the conventional care group (April, 2014 to June, 2015) were in a different period to the data for the ERAS protocol group (June, 2015 to April, 2021). Therefore, the ERAS protocol group could have had a higher implementation rate of laparoscopic surgery than the conventional care group and, naturally, had better postoperative outcomes [21]. Although we eliminated that bias by performing PS matching, even after matching, the ERAS group had better postoperative outcomes than the conventional care group. As surgical techniques improve over time, it is undeniable that they will have had some influence on postoperative outcomes.
In conclusion, this study showed that the ERAS protocol can be implemented safely for elective colorectal cancer surgery without increasing the complication rate, and that a higher compliance rate with the ERAS protocol is dose-dependently associated with a lower complication rate and shorter LOHS. Among the ERAS items, perioperative fluid management had a crucial impact on lowering complication rates and shortening the LOHS.
References
Ota H, Ikenaga M, Hasegawa J, Murata K, Miyake Y, Mizushima T, et al. Safety and efficacy of an “enhanced recovery after surgery” protocol for patients undergoing colon cancer surgery: a multi-institutional controlled study. Surg Today. 2017;47:668–75.
ERAS Compliance Group. The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an International Registry. Ann Surg. 2015;261:1153–9.
Fujie Y, Ota H, Ikenaga M, Hasegawa J, Murata K, Miyake Y, et al. Evaluation of the feasibility of an “enhanced recovery after surgery” protocol for older patients undergoing colon cancer surgery. J Anus Rectum Colon. 2018;2:83–9.
Owodunni OP, Hampton J, Bettick D, Sateri S, Magnuson T, Wick E, et al. High compliance to an enhanced recovery pathway for patients >/=65 years undergoing major small and large intestinal surgery is associated with improved postoperative outcomes. Ann Surg. 2019;270:1117–23.
Hampton JP, Owodunni OP, Bettick D, Chen SY, Sateri S, Magnuson T, et al. Compliance to an enhanced recovery pathway among patients with a high frailty index after major gastrointestinal surgery results in improved 30-day outcomes. Surgery. 2019;166:75–81.
Pisarska M, Pedziwiatr M, Malczak P, Major P, Ochenduszko S, Zub-Pokrowiecka A, et al. Do we really need the full compliance with ERAS protocol in laparoscopic colorectal surgery? A prospective cohort study. Int J Surg. 2016;36:377–82.
Apfel CC, Heidrich FM, Jukar-Rao S, Jalota L, Hornuss C, Whelan RP, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012;109:742–53.
Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118:85–113.
Anderin K, Gustafsson UO, Thorell A, Nygren J. The effect of diverting stoma on postoperative morbidity after low anterior resection for rectal cancer in patients treated within an ERAS program. Eur J Surg Oncol. 2015;41:724–30.
Van Butsele J, Bislenghi G, D’Hoore A, Wolthuis AM. Readmission after rectal resection in the ERAS-era: is a loop ileostomy the Achilles heel? BMC Surg. 2021;21:267.
Jochum SB, Ritz EM, Bhama AR, Hayden DM, Saclarides TJ, Favuzza J. Early feeding in colorectal surgery patients: safe and cost effective. Int J Colorectal Dis. 2020;35:465–9.
Akhtar MS, Khan N, Qayyum A, Khan SZ. Cost difference of enhanced recovery after surgery pathway vs. conventional care in elective laparoscopic cholecystectomy. J Ayub Med Coll Abbottabad. 2020;32:470–5.
Bisch S, Nelson G, Altman A. Impact of nutrition on enhanced recovery after surgery (ERAS) in gynecologic oncology. Nutrients. 2019;11:1088.
Lilot M, Ehrenfeld JM, Lee C, Harrington B, Cannesson M, Rinehart J. Variability in practice and factors predictive of total crystalloid administration during abdominal surgery: retrospective two-centre analysis. Br J Anaesth. 2015;114:767–76.
Thacker JK, Mountford WK, Ernst FR, Krukas MR, Mythen MM. Perioperative fluid utilization variability and association with outcomes: considerations for enhanced recovery efforts in sample US surgical populations. Ann Surg. 2016;263:502–10.
Zhu AC, Agarwala A, Bao X. Perioperative fluid management in the enhanced recovery after surgery (ERAS) pathway. Clin Colon Rectal Surg. 2019;32:114–20.
Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, et al. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97:820–6.
Rollins KE, Lobo DN. Intraoperative goal-directed fluid therapy in elective major abdominal surgery: a meta-analysis of randomized controlled trials. Ann Surg. 2016;263:465–76.
Brandstrup B, Svendsen PE, Rasmussen M, Belhage B, Rodt SA, Hansen B, et al. Which goal for fluid therapy during colorectal surgery is followed by the best outcome: near-maximal stroke volume or zero fluid balance? Br J Anaesth. 2012;109:191–9.
Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–8.
Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP, et al. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014;32:1804–11.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hiromichi Sato, Hirofumi Ota, Koji Munakata, Yusuke Matsuura, Makoto Fujii, Noriko Wada, Daisuke Takiuchi, Naoki Hama, Kou Takachi, and Masao Yukawa declare that they have no conflicts of interest.
Ethical statement
The protocol for this research project was approved by the Institutional Review Board of Ikeda City Hospital and conforms to the provisions of the Helsinki Declaration of 1964 and later versions. Approval no. A21011. The requirement for acquisition of informed consent from patients was waived because of the retrospective design of this study and anonymized data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sato, H., Ota, H., Munakata, K. et al. Perioperative fluid management influences complication rates and length of hospital stay in the enhanced recovery after surgery (ERAS) protocol for patients with colorectal cancer. Surg Today 53, 242–251 (2023). https://doi.org/10.1007/s00595-022-02568-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02568-7