Abstract
Purpose
The Endoscopic Surgical Skill Quantification System for qualified surgeons (QSs) was introduced in Japan to improve surgical outcomes. This study reviewed the surgical outcomes after initial experience performing laparoscopic distal gastrectomy (LDG) and evaluated the improvement in surgical outcomes following accreditation as a QS.
Methods
Eighty-seven consecutive patients who underwent LDG for gastric cancer by a single surgeon were enrolled in this study. The cumulative sum method was used to analyze the learning curve for LDG. The surgical outcomes were evaluated according to the two phases of the learning curve (learning period vs. mastery period) and accreditation (non-QS period vs. QS period).
Results
The learning period for LDG was 48 cases. Accreditation was approved at the 67th case. The operation time and estimated blood loss were significantly reduced in the QS period compared to the non-QS period (230 vs. 270 min, p < 0.001; 20.5 vs. 59.8 ml, p = 0.024, respectively). Furthermore, the major complication rate was significantly lower in the QS period than in the non-QS period (0 vs. 10.6%, p = 0.044).
Conclusions
Experience performing approximately 50 cases is required to reach proficiency in LDG. After receiving accreditation as a QS, the surgical outcomes, including the complication rate, were improved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic distal gastrectomy (LDG) for early gastric cancer has been widely performed as a standard procedure since the first case was reported in 1994 [1]. LDG is reportedly safe and feasible and leads to reduced postoperative pain, a faster recovery, and a shorter postoperative hospital stay than open gastrectomy [2, 3]. However, the acquisition of adequate surgical skills for LDG remains difficult compared to open surgery. To improve the quality of laparoscopic surgical techniques, the Japan Society for Endoscopic Surgery (JSES) established the Endoscopic Surgical Skill Quantification System (ESSQS) in 2001, which consists of expert laparoscopic surgeons from various surgical specialties [4, 5]. In the laparoscopic gastrectomy field, unedited video of LDG with lymph node (LN) dissection for gastric cancer is assessed by two referees in a double-blind fashion. For the video evaluation, two referees review the video using a score sheet along with detailed check points that consist of common criteria and organ-specific criteria. In colorectal surgery, a laparoscopic procedure performed by an ESSQS-qualified surgeon (QS) reportedly leads to improved surgical outcomes, including a better operation time, blood loss, and local recurrence rate than that performed by a non-ESSQS-QS [6, 7]. Furthermore, LDG performed by trainees supervised by an ESSQS-QS is a safe and appropriate procedure, similar to that performed by an ESSQS-QS [8].
The accreditation rate in LDG has hovered around 25% each year. The low accreditation rate is attributable to the strict assessment of surgical skills, perioperative conduct, and overall performance of the surgical team and leadership of the primary surgeon. While this type of accreditation system is expected to improve surgical outcomes and reduce complications, it is original to Japan and has not been implemented elsewhere. Although the reliability of the assessment is essential for this system to work, it has been reported that interrater agreement is relatively low [4].
In the present study, the surgical results of LDG performed by a single surgeon and the results of accreditation examinations to evaluate the board ESSQS for QS were investigated.
Materials and methods
Patients
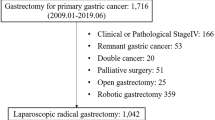
This was a retrospective study using data obtained from December 2013 to February 2020 at Okayama University Hospital, Okayama, Japan, and a single surgeon (Surgeon A, S Kikuchi) performed LDG with D1+ LN dissection for early-stage gastric cancer in 87 patients. The data of another surgeon (Surgeon B, T Kagawa) who had performed same surgical procedure from November 2014 to April 2020 at Okayama University Hospital and Shikoku Cancer Center, Matsuyama, Japan, were also analyzed.
Before this period, the surgeons had no experience performing LDG. Patients with a history of upper abdominal surgery were excluded from the analysis. All Roux en Y reconstructions were performed intracorporeally without a small incision in the epigastrium. In Surgeon A, the patients from the 1st case to the 19th case with Billroth-I reconstruction were operated on extracorporeally, with a small incision made at the epigastrium, while the patients from the 20th to the 87th case with Billroth-I reconstruction underwent intracorporeal triangle reconstruction [9]. In Surgeon B, all patients with Billroth-I reconstruction underwent intracorporeal reconstruction. QSs participated in all operations as an assistant or the scopist to supervise.
All patients underwent esophagogastroduodenoscopy with a biopsy and abdominal computed tomography (CT) for the preoperative diagnosis and staging. Endoscopic ultrasonography and chest CT were performed in select patients. The indication for LDG with D1+ LN dissection was cStage I gastric cancer, which was outside the indication for endoscopic resection. The extent of the LN dissection was determined using the 2017 Japanese gastric cancer treatment guidelines (Ver. 4) [10].
The study was approved by the Institutional Review Board of Okayama University Hospital (No. 2101-021), and Shikoku Cancer Center (Rin2020-92).
Data collection
The patients’ demographic and clinical characteristics as well as their perioperative outcomes, including the operating time, estimated blood loss (EBL), number of retrieved LNs, complications, and postoperative hospital length of stay, were evaluated. Nine of the 87 (10.3%) cases in Surgeon A and none in Surgeon B underwent LDG with laparoscopic cholecystectomy for gallstones or chronic cholecystitis. The time for cholecystectomy was excluded from the total operating time by a retrospective video review to avoid operative heterogeneity. Complications were graded by the Clavien-Dindo classification [11]. A major complication was defined as requiring surgical, endoscopic, or radiological intervention (grade ≥ IIIa).
The cumulative sum (CUSUM) method and statistical analyses
The CUSUM method is a sequential analysis technique typically used to detect a small shift in an overall process [12]. In the current study, the cases were numbered sequentially from the first to the last case. The formula for the CUSUM of the operation time was as follows:
where allowable slack (k) = 0.5 × σ, action limit = ± 4 × σ, and σ = \(\overline{R}\)/1.128. \(\overline{R}\) is the average of the moving range of Xi. Xi is an individual operation time (i = 1, 2, …, 87), and the Target value was set to 240 min, which was the average time of the successful candidates of ESSQS for QS in LDG. k is a constant representing the allowable slack in the process and setting the magnitude of the shift to be detected. There were two fluctuating lines; the upper line indicated that the individual operation time was longer than the population mean and the lower line indicated that it was shorter, and therefore, it was not necessary to include these findings in the analysis. Therefore, the upper line was defined as the learning curve for LDG related to the operation time The CUSUM charts were plotted using the Excel software program (Microsoft, Redmond, WA, USA).
The χ2 test was used to analyze categorical variables. Welch’s or Student’s t-test was used to analyze continuous variables. All p values were two-sided, and those less than 0.05 were considered to be statistically significant. Statistical analyses was performed using the JMP software program, ver. 11.2 (SAS Institute, Cary, NC, USA).
Results
LDG learning curve by a CUSUM analysis
The operation time for 87 consecutive cases of LDG is shown in Fig. 1a. The moving average of the operation time for groups of five patients was plotted. The operation time reached a temporary plateau after approximately 10 cases; subsequently, the curve of the operation time increased and plateaued again after approximately 53 cases.
Sequential operation time and learning curve for LDG in surgeon A. a Sequential operation time for LDG. The moving average of the operation time in a group of five cases is plotted. b Learning curve for LDG. The CUSUM chart shows a gradual decrease at the 49th case, which is defined as the learning curve, and the cases are divided into two periods at the 49th case. Accreditation as a QS was approved at the 67th case. LDG, laparoscopic distal gastrectomy; QS, qualified surgeon; SH, high side cumulative sum; SL, low side cumulative sum; UCL, upper control; LCL, lower control
The CUSUM analysis for the operation time was performed to analyze the learning curve for LDG according to the cases performed. The parameters of the CUSUM chart were as follows: \(\overline{R}\) = 41.2, σ = 36.5, allowable slack (k) = 18.3, action limit = 146. The upper control limit (UCL) and lower control limit (LCL) were set based on the action limit. The CUSUM chart showed a gradual increase until the 48th case and then subsequently decreased to the 87th case (Fig. 1b). The learning curve for LDG was defined as the 49th case in the present study according to the CUSUM chart for the operation time, and the cases were then divided into two phases (learning period, 1st–48th case; mastery period, 49th–87th case). The CUSUM analysis for the operation time of another surgeon (surgeon B) who had been accredited as an ESSQS-QS with fewer cases experienced (by the 25th case) was also performed. The learning curve for LDG in Surgeon B was not defined (Supplementary Fig. S1).
The comparison of the characteristics and surgical outcomes according to the learning curve
Patients’ characteristics and surgical outcomes are shown in Table 1. There were no significant differences in the age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) Physical Status classification, or reconstruction procedure between the two phases. However, more cases were performed by intracorporeal anastomosis in the mastery period than in the learning period (100% vs. 60.4%, p < 0.001), as intracorporeal triangle reconstruction using the endoscopic linear stapler for Billroth-I reconstruction was introduced at the 20th case in our institution.
The operation time was significantly shorter and the EBL lower in the mastery period than in the learning period (226 vs. 288 min, p < 0.001; 26.8 vs. 69.4 ml, p = 0.027, respectively). There were no significant differences in the rate of major complications (Clavien-Dindo ≥ IIIa), number of retrieved LNs, or length of the postoperative hospital stay between the two phases.
The comparison of the characteristics and surgical outcomes according to ESSQS accreditation
Accreditation as a QS by ESSQS using the unedited video review of LDG with LN dissection for gastric cancer was approved at the 67th case of which video has been submitted to JSES and passed the examination. The cases were divided into two phases according to ESSQS accreditation (non-QS period, 1st–66th case; QS period, 67th–87th case).
There were no significant differences in patients’ characteristics or surgical procedures between the two phases, except for in the rate of intracorporeal anastomosis (Table 2). The operation time was significantly shorter, and the EBL was lower in the QS period than in the non-QS period (230 vs. 270 min, p < 0.001; 20.5 vs. 59.8 ml, p = 0.024, respectively). The rate of major postoperative complications (pancreatic fistula 2, anastomotic leakage 1, intra-abdominal abscess 1, pneumonia 1, pulmonary embolism 1, postoperative hemorrhage 1) was significantly lower in the QS period than in the non-QS period (0% vs. 10.6%, p = 0.044), although there were no significant differences in the number of retrieved LNs or the length of the postoperative hospital stay. In the additional analysis of Surgeon B, the postoperative complication rate was also significantly lower in the QS period than in the non-QS period (Supplementary Table S1), although there were no significant differences in the operation time or EBL between the two phases due to the small number of cases.
Discussion
The frequency of performing LDG for early-stage gastric cancer patients has been increasing rapidly because a laparoscopic approach is less invasive than open surgery, and its oncological safety compared with conventional open distal gastrectomy (ODG) has also been confirmed [2, 3, 13, 14]. However, the incidence of postoperative pancreatic fistula was reportedly higher in LDG than in ODG according to a review of a national clinical database in Japan, as these LDG procedures were performed by various surgeons, including trainees and non-QSs [15]. In Japan, the ESSQS has been established to assess and improve the quality of laparoscopic surgical skill, since laparoscopic surgery requires more experience than open surgery to obtain sufficient surgical and management skill. In the current study, the significance of the ESSQS for QSs was evaluated by investigating the surgical outcomes of consecutive LDG procedures starting from the initial case performed by a single surgeon.
The CUSUM chart plots the cumulative sum of the deviation of the raw value of each sample from the target or mean value [16]. It is more useful for monitoring performance and defining a learning curve for a surgical procedure than the moving average [16, 17]. In our CUSUM analysis of the learning curve, a plateau was reached at the 5th case, decreasing until the 17th case but then gradually increasing again until the 48th case. Therefore, the learning curve was considered to require 48 cases in the present study. Several reports have shown that the operation time of trainees became almost equal to that of the trainers after performing 5–10 cases under the trainers’ assistance and supervision [18,19,20]. They also suggested that standardization of surgical procedures and sufficient experience as a first assistant and scopist were required to ensure the safety and successful accomplishment of LDG for trainees. Kaito and Kinoshita noted that learning using operative videos, daily practice using a dry box, and actual surgical experience were necessary to master the LDG procedure for trainees [21]. Surgeon B was accredited as a QS with less experience (at the 25th case), and the complication rate was improved after ESSQS-QS accreditation (Supplementary Table S1).
However, trainees might require more surgical experience (approximately 50 cases) to reach proficiency in LDG because the CUSUM chart did not show a decrease in Surgeon B Supplementary Fig. S1) although trainees can perform LDG safely under the excellent trainers’ assistance and supervision. Several reports have suggested that trainees require surgical experience with at least 30–90 LDG procedures before achieving optimal outcomes, as LDG includes complex procedure, such as LN dissection and intracorporeal reconstruction [22,23,24]. The rates of intracorporeal anastomosis were significantly higher in the later periods than in the earlier periods. The time for extracorporeal anastomosis was not so different from that for intracorporeal anastomosis. However, totally laparoscopic gastrectomy with intracorporeal gastroduodenostomy was introduced at the 20th case. The learning curve for intracorporeal anastomosis reportedly plateaued after 15–20 cases [9, 25], which might affect the total operation time and the increase in the learning curve of the CUSUM chart at the 19th case.
A surgeon was considered accredited as a QS after performing the case in which a surgical video was submitted to JSES and passed the examination. The timing of accreditation as a QS might be affected by there being only one examination conducted per year. However, the accredited surgical video in the present case was performed approximately 11 months before the examination deadline, and other submitted surgical videos did not result in accreditation in previous years. Therefore, the definition of accreditation as a QS seems appropriate in this study.
On comparing the learning and mastery periods, the major complication rate was not significantly different, although the operation time was significantly shorter, and the EBL was lower in the mastery period than in the learning period. However, the major complication rate was lower in the QS period than in the non-QS period, in addition to the operation time being shorter and the EBL lower. The acceptance criteria of the board of ESSQS for a QS include whether or not the surgeon has sufficient endoscopic surgical skill and performs the LDG safely, independent of the tutor. The results of the present study suggest that the ESSQS for QSs in LDG is appropriate because all surgical outcomes, including postoperative complications, improved in the QS period, suggesting that both sufficient surgical experience and accreditation as an ESSQS-QS are required to achieve better surgical outcomes of LDG. However, an effective education system will shorten the time to achieve QS qualification, similar to the operation time.
The number of retrieved LNs was slightly smaller in the QS period than in the non-QS period although there was no significant difference between two periods. Although the small case number in the QS period might affect the results, the quality of surgery in the QS period was not inferior to that in the non-QS period as the number of retrieved LNs in the QS period was larger than 15, which was recommended by the 8th edition TNM classification for gastric cancer to guarantee accurate optimal staging [26].
Several limitations associated with the present study warrant mention. First, this study was retrospective, and all LDG procedures in this study were performed by a single surgeon. Further analyses including multiple surgeons and multiple institutions will improve the quality of this study in the future. Second, several surgeons worked as assistants. LDG performed by a trainee supervised by a QS has been reported to be appropriate and safe [8], and who acts as the assistant affects the operation time and surgical outcomes. However, we do not think this will cause major problems, as QSs acted as the assistant or scopist in all cases in this study.
Conclusions
Experience performing approximately 50 cases is required to reach proficiency in the laparoscopic surgical technique for LDG, although the precise number depends on an individual’s ability and the training environment. Accreditation with the ESSQS for QSs in LDG was found to improve surgical outcomes and reduce complications. Further analyses including multiple surgeons and multiple institutions will be needed to clarify the implications of the board accreditation system of the ESSQS.
References
Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4:146–8.
Katai H, Mizusawa J, Katayama H, Takagi M, Yoshikawa T, Fukagawa T, et al. Short-term surgical outcomes from a phase III study of laparoscopy-assisted vs. open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer. 2017;20:699–708.
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016;263:28–35.
Kimura T, Mori T, Konishi F, Kitajima M. Endoscopic surgical skill qualification system in Japan: five years of experience in the gastrointestinal field. Asian J Endosc Surg. 2010;3:66–70.
Tanigawa N, Lee SW, Kimura T, Mori T, Uyama I, Nomura E, et al. The endoscopic surgical skill qualification system for gastric surgery in Japan. Asian J Endosc Surg. 2011;4:112–5.
Ichikawa N, Hommma S, Funakoshi T, Ohshima T, Hirose K, Yamada K, et al. Impact of technically qualified surgeons on laparoscopic colorectal resection outcomes: results of a propensity score-matching analysis. BJS Open. 2020. https://doi.org/10.1002/bjs5.50263.
Aoyama S, Inoue Y, Ohki T, Itabashi M, Yamamoto M. Usefulness of the endoscopic surgical skill qualification system in laparoscopic colorectal surgery: short-term outcomes: a single-center and retrospective analysis. BMC Surg. 2019;19:90. https://doi.org/10.1186/s12893-019-0528-2.
Yamada T, Kumazu Y, Nakazono M, Hara K, Nagasawa S, Shimoda Y. Feasibility and safety of laparoscopy-assisted distal gastrectomy performed by trainees supervised by an experienced qualified surgeon. Surg Endosc. 2020;34:429–35.
Oki E, Tsuda Y, Saeki H, Ando K, Imamura Y, Nakashima Y. Book-binding technique for Billroth I anastomosis during totally laparoscopic distal gastrectomy. J Am Coll Surg. 2014;219:e69-73.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver.4). Gastric Cancer. 2017;20:1–19. https://doi.org/10.1007/s10120-016-0622-4.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of survey. Ann Surg. 2004;240:205–13.
Page ES. Continuous inspection schemes. Biometrika. 1954;41:100–15.
Katai H, Mizusawa J, Katayama H, Morita S, Yamada T, Bando E, et al. Survival outcomes after laparoscopy-assisted distal gastrectomy vs. open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol Hepatol. 2020;5:142–51.
Kim HH, Han SU, Kim MC, Kim W, Lee HJ, Ryu SW, Korean Laparoendoscopic Gastrointestinal Surgery Study (KLASS) Group, et al. Effect of laparoscopic distal gastrectomy vs. open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol. 2019;5:7506–13.
Yoshida K, Honda M, Kumamaru H, Kodera Y, Kakeji Y, Hiki N, et al. Surgical outcomes of laparoscopic distal gastrectomy compared to open distal gastrectomy: a retrospective cohort study based on a nationwide registry database in Japan. Ann Gastroenterol Surg. 2017;22:55–64.
Wang B, Son SY, Shin HJ, Hur H, Han SU, et al. The learning curve of linear-shaped gastroduodenostomy associated with totally laparoscopic distal gastrectomy. J Gastrointest Surg. 2019. https://doi.org/10.1007/s11605-019-04329-3.
Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, Cho YK, et al. Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc. 2017;21:28–33.
Tokunaga M, Hiki N, Fukunaga T, Miki A, Nunobe S, Ohyama S, et al. Quality control and educational value of laparoscopy-assisted gastrectomy in a high-volume center. Surg Endosc. 2009;23:289–95.
Nunobe S, Hiki N, Tanimura S, Nohara K, Sano T, Yamaguchi T, et al. The clinical safety of performing laparoscopic gastrectomy for gastric cancer by trainees after sufficient experience in assisting. World J Surg. 2013;37:424–9.
Kuroda S, Kikuchi S, Hori N, Sakamoto S, Kagawa T, Watanabe M, et al. Training system for laparoscopy-assisted distal gastrectomy. Surg Today. 2017;47(7):802–9. https://doi.org/10.1007/s00595-016-1439-9.
Kaito A, Kinoshita T. Educational system of laparoscopic gastrectomy for trainee-how to teach, how to learn. J Vis Surg. 2017;13(3):16. https://doi.org/10.21037/jovs.2016.12.13.
Kim MG, Kim KC, Yook JH, Kim BS, Kim TH, Kim BS. A practical way to overcome the learning period of laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2011;25:3838–44.
Kunisaki C, Makino H, Yamamoto N, Sato T, Oshima T, Nagano Y, et al. Learning curve for laparoscopy-assisted distal gastrectomy with regional lymph node dissection for early gastric cancer. Surg Laparosc Endosc Percutan Tech. 2008;18:236–41.
Zhang X, Tanigawa N. Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomybased analysis. Surg Endosc. 2009;23:1259–64.
Jeong O, Jung MR, Park YK, Ryu SY. Safety and feasibility during the initial learning process of intracorporeal Billroth I (delta-shaped) anastomosis for laparoscopic distal gastrectomy. Surg Endosc. 2015;29:1522–9.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9. https://doi.org/10.3322/caac.21388.
Acknowledgements
This work was supported by JSPS Early Career Scientists, Grant number 18K16362.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest for this study.
Ethical statement
The study was approved by the Institutional Review Board of Okayama University Hospital (No. 2101-021) and Shikoku Cancer Center (Rin2020-92). The research reported in this paper was in compliance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kikuchi, S., Kagawa, T., Kuroda, S. et al. Accreditation as a qualified surgeon improves surgical outcomes in laparoscopic distal gastrectomy. Surg Today 51, 1978–1984 (2021). https://doi.org/10.1007/s00595-021-02309-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02309-2