Abstract
Purpose
There are few data available on the outcomes of postoperative recurrent thymic carcinoma (TC) and thymic neuroendocrine carcinoma (TNEC). The aim of this study is to evaluate the treatment and survival in patients with recurrent TC and TNEC after undergoing surgical resection.
Methods
A retrospective chart review was performed using our multicenter database to identify patients with a postoperative recurrence of TC and TNEC from 1995 to 2018. The clinicopathological factors were reviewed and the survival outcomes were analyzed.
Results
Sixty patients were identified among 152 patients who underwent resection of TC and TNEC. The median follow-up period from the first recurrence was 14.8 months (range 0–144). The 5-year post-recurrence survival was 23% for the whole cohort. According to a univariable analysis, advanced stage [hazard ratio (HR) 2.81, 95% confidence interval (CI) 1.09–9.54], interval between primary surgery and recurrence (HR 0.97, 95% CI 0.95–0.99), any treatment for recurrence (HR: 0.27, 95% CI 0.13–0.58) and chemotherapy for recurrence (HR: 0.46, 95% CI 0.22–0.95) were significant factors related to post-recurrence survival.
Conclusions
Chemotherapy rather than surgery appears to be the mainstay treatment for managing patients with postoperative recurrent TC and TNEC and it may also be considered in multidisciplinary management. Further studies with a larger sample size are required to confirm our findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Thymic epithelial neoplasms are classified as thymoma, thymic carcinoma (TC), and thymic neuroendocrine carcinoma (TNEC). The prevalences of TC and TNEC among all thymic neoplasms are around 15–20% and 2–3%, respectively [1, 2]. In the European Society of Thoracic Surgeons (ESTS) thymic database, in which 1122 patients were registered from 2007 to 2017, 28% of surgical cases had TC and 6.6% had TNEC [3]. In Japan, there were 2340 cases of resection of thymic epithelial neoplasms in 2016, including 314 TC (13%) and 40 TNEC (2%) [4]. In addition to limited data, TC and TNEC have a high rate of recurrence of 30–40% at 5 years, even after complete resection [5,6,7,8]; and the incidence of distant recurrence after surgery for TC and TNEC is almost as high as that of locoregional recurrence [8, 9], whereas this is not seen for recurrent thymoma.
Surgical resection for thymic epithelial neoplasms is the treatment of choice and it also has a significant impact on survival and recurrence [10,11,12]. In TC, complete resection, early pathological stage at the first surgery, and postoperative radiotherapy are significant prognostic factors for a lower rate of recurrence [5, 6, 11, 13,14,15]. The survival and recurrence rates of completely resected TNEC are similar to those for TC [6, 14]. A literature search suggested that little is known about the therapeutic strategy for postoperative recurrence of TC and TNEC. A recent report from the Mayo Clinic on long-term outcomes of treatment for recurrent thymic epithelial tumors proposed surgery for resectable and locoregional recurrent tumors, but a multimodal approach is often used including repeat surgery for recurrent TC and TNEC [9]. In a limited number of patients with recurrent TC, chemotherapy was associated with a prolonged progression-free interval [9].
To the best of our knowledge, few studies have so far examined the association of background factors and treatment on the outcomes of recurrent TC and TNEC. Therefore, the aim of this study is to examine these relationships in patients with a recurrence of these tumors.
Methods
Patients and data collection
This study was approved by the Kyoto University Hospital Institutional Review Board (IRB) (reference number: R1872) and the IRBs at Nishi-Kobe Medical Center, Fukuoka University Hospital, Kobe City Medical Centre General Hospital, Kitano Hospital, Shizuoka Municipal Hospital, Tenri Hospital, Shiga Medical Center for Adults, Nagara Medical Center, Takatsuki Red Cross Hospital, Osaka Red Cross Hospital, St. Luke’s International Hospital, Kyoto-Katsura Hospital, and Otsu Red Cross Hospital, all of which granted a waiver of consent for the study. A retrospective chart review was performed to identify patients who underwent thymectomy for TC and TNEC with a curative intent in the databases of the above twelve hospitals between May 1995 and December 2018. Data were collected regarding background (age and sex), intra- and perioperative data (surgical approach, extent of resection, completeness of resection, neoadjuvant therapy, and adjuvant therapy), pathological findings (histology, maximum diameter of the specimen, lymph node metastasis, and Masaoka stage), and follow-up (recurrence site, treatment for recurrence, and cause of death). In a case with an incomplete resection at initial resection, a complete disappearance of the disease was confirmed by the first postoperative surveillance chest computed tomography and a new discrete lesion by imaging modalities was regarded as recurrence. Surgery for recurrent disease was typically performed in patients with an intrathoracic, solitary, and resectable lesion based on the findings of CT with or without PET.
Statistical analysis
Categorical variables were compared by Fisher exact test, and continuous variables by Wilcoxon signed-rank test. Post-recurrence survival was calculated as the time from the date of recurrence until the date of death from any cause or the date on which the patient was last known to be alive. The diagnosis of recurrence was confirmed radiologically, including use of computed tomography (CT) with or without positron emission tomography (PET). Post-recurrence survival was analyzed using the Kaplan–Meier method with a log-rank test, and with a Cox proportional hazard model, with p < 0.05 considered to be significant. All analyses were performed using JMP® 14 software program (SAS Institute Inc., Cary, NC, USA).
Results
From our multi-institutional database, 60 recurrent cases (37 males, 23 females) were identified among 152 patients who underwent resection. The demographic data, tumor characteristics, and perioperative therapy for these cases are shown in Table 1. The median age was 63 (range 19–89) years. The median interval from the initial operation to recurrence was 17.5 (1.8–142) months. Complete resection at the initial operation was achieved in 45 patients (75%). Treatment for recurrence was performed in 42 patients (70%), including chemotherapy in 30 patients (50%), surgery in 16 (27%), and radiotherapy in 10 (17%); with 15 patients (25%) receiving more than one treatment. In the chemotherapy cases, the treatment was chemotherapy alone (n = 18) and in combination with surgery (n = 5), radiotherapy (n = 3), and surgery and radiotherapy (n = 2).
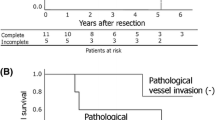
The median follow-up period from the initial operation was 44.2 (5.87–181) months, and this period after recurrence was 14.8 (0.1–153) months. The 5-year OS after recurrence was 23%. In the whole cohort, median post-recurrence survival was 14.8 months. According to a univariable analysis, advanced stage (HR 2.81, 95% CI 1.09–9.54), the interval between primary surgery and recurrence (HR 0.97, 95% CI 0.95–0.99), any treatment for recurrence (HR 0.27, 95% CI 0.13–0.58) and chemotherapy for recurrence (HR 0.46, 95% CI 0.22–0.95) were significant factors related to post-recurrence survival (Table 2). According to a multivariable analysis, the interval between primary surgery and recurrence (HR 0.98, 95% CI 0.95–1.01) and any treatment for recurrence (HR 0.23, 95% CI 0.04–1.16) tended to show a prolonged post-recurrence survival, although it was not statically significant. (Table 2). The survival curve comparing treatment and best supportive care (BSC) is shown in Fig. 1a. The 5-year post-recurrence survival rates after any treatment and BSC were 32% and 0%, respectively. In patients with any treatment after recurrence (n = 42), the 5-year post-recurrence survival rates after chemotherapy and non-chemotherapy were 33% and 28%, respectively (Fig. 1b). The patterns of recurrence in each treatment pattern are shown in Table 3.
Survival and treatment in patients with recurrence
A comparison of the demographic data, tumor characteristics, and perioperative therapy between BSC and any treatment is shown in Table 4. There was no significant difference between the two groups, but there were tendencies towards a higher age (p = 0.15), more advanced Masaoka stage (p = 0.19) at the initial operation, and a shorter interval between primary surgery and recurrence (p = 0.05) in patients who received BSC.
Surgical resection for recurrence was performed in 16 patients (27%) (Table 5), and 11 of these patients received further therapy after this surgery, with chemotherapy only (n = 5), radiotherapy only (n = 3), and chemoradiotherapy (n = 3). Five patients received no additional therapy after surgery. Repeated surgical resection was performed in 2 patients (4 and 2 times, respectively). The survival curves comparing surgery and non-surgery for recurrence in patients with treatment after recurrence (n = 42) are shown in Fig. 2a. The 5-year post-recurrence survival rates in the surgery and non-surgery groups were 30% and 33%, respectively.
Post-recurrence survival in a subgroup analysis. a Survival curves comparing surgery and non-surgery for recurrence in patients with treatment after recurrence (n = 42). Non-surgical patients consisted of patients undergoing chemotherapy, radiotherapy, or both for recurrent thymic carcinoma and neuroendocrine carcinoma. b Survival curves comparing surgery and non-surgery for recurrence of thymic carcinoma (n = 42). Non-surgical patients consisted of patients undergoing chemotherapy, radiotherapy, or both or best supportive care for recurrent thymic carcinoma
Chemotherapy for recurrence was performed in 30 patients (50%), with regimens of carboplatin and paclitaxel (n = 11), carboplatin and etoposide (n = 3), cisplatin and etoposide (n = 2), cisplatin, doxorubicin, vincristine, and cyclophosphamide (n = 2), and others (n = 8). Repeated chemotherapy was performed in 13 patients.
Radiotherapy for recurrence was performed in 10 patients (17%), including 2 treated with radiotherapy alone. One of these cases received radiotherapy for local recurrence and died of pneumonia at 5.7 months after recurrence. The other patient received palliative radiotherapy for multiple bone metastases and died of an unknown cause at 24.5 months after recurrence.
Subgroup information and analysis
Of the 60 patients, 42 were diagnosed with TC, 16 with TNEC, and 2 with TNEC combined with squamous cell carcinoma. According to a univariable analysis for TC cases (n = 42) (Table 6), chemotherapy for recurrence was significantly associated with improved post-recurrence survival after recurrence (HR 0.33, 95% CI 0.14–0.78), and surgery for recurrence (HR 0.44, 95% CI 0.10–1.28) tended to show a prolonged post-recurrence survival, although it was not statistically significant. According to a multivariable analysis, chemotherapy for recurrence was significantly associated with an improved post-recurrence survival (HR 0.32, 95% CI 0.13–0.76), and surgery for recurrence (HR 0.42, 95% CI 0.10–1.22) tended to show this association. In thymic carcinoma cases (n = 42), the survival curve comparing surgery and non-surgery is shown in Fig. 2b. The 5-year post-recurrence survival rates in the surgery and non-surgery groups were 27% and 19%, respectively. According to a univariable analysis for TNEC cases (n = 18) (Table 6), radiotherapy for recurrence was significantly associated with a worse post-recurrence survival after recurrence (HR 11.5, 95% CI 1.63–230).
Discussion
There is relatively little information on management of recurrent TC and TNEC after the initial resection of the primary lesion. Using the database of the Japanese Association for Research on the Thymus, Mizuno et al. found that more than 70% of patients with postoperative recurrent TC were managed non-surgically; however, detailed treatment information was scarce for all of the patients [16]. In the current study, we found that heterogenous treatment combinations are used for postoperative recurrent TC and TNEC, but with chemotherapy playing a major role in the multidisciplinary treatment.
Evidence-based guidelines for the management of recurrence are lacking, presumably due to the rarity of TC and the limited sample sizes of the published studies. Both NCCN [17] and ESMO (18) guidelines discuss the management of “advanced and recurrent” diseases, instead of making separate recommendations for advanced disease without prior treatment and recurrent disease after prior treatment. The Japanese Lung Cancer Society guidelines [19] recommend surgical resection in a multidisciplinary setting for resectable recurrent thymic epithelial tumors (including thymoma and other histologies). For TC alone, chemotherapy is recommended in patients with performance status 0–2 and recurrent disease, but information on the regimen, number of cycles, and no recurrence criteria have been established in the above guidelines.
In our literature search of chemotherapy for thymic carcinoma, we found several studies that included patients with advanced disease without treatment and with recurrent disease after treatment. In all identified studies, including three clinical trials [22, 24, 25] and two using real world data [21, 23], patients were treated with chemotherapy without radiotherapy or surgical resection. Lemma et al. [20], Furugen et al. [21], and Kim et al. [22] did not include cases with recurrent disease, Igawa et al. [23] had no cases with postoperative recurrence, and Hirai et al. [24] included 8 cases with postoperative recurrence, which accounted for 20% of all cases. The median progression-free survival (PFS) in the whole cohort was 7.5 (6.2–12.3) months. Inoue et al. [25] included 10 cases with postoperative recurrence, which accounted for 30% of all cases with TC. The median PFS was 7.6 months. These results cannot be compared to our study, given the heterogeneity of the treatment patterns in our patients. In addition, no previous study has so far examined the short- or long-term outcomes limited to patients with recurrent disease after prior treatment.
A suitable chemotherapy regimen can sometimes be selected based on the results of animal experiments, and there are a few thymoma-related animal models [26, 27], but none for TC or TNEC. Therefore, the selection of the optimal regimen has to be based on previous reports for related diseases. In a systematic review of 55 articles, Berghmans et al. evaluated the efficacy of different systemic therapies in thymoma and TC [28], and found that carboplatin plus amrubicin, carboplatin plus paclitaxel, and cisplatin plus docetaxel are favorable regimens [28, 29]. However, the efficacy of these regimens for recurrent TC and TNEC is uncertain.
Unlike surgical management of recurrent thymoma, the role of surgery in recurrent TC and TNEC is undetermined, and little information is available on surgical resection of these tumors [30, 31]. Okumura et al. [30] described a single patient who underwent resection for recurrent TC, who died 2 years later from TC. Yen et al. [31] reported 7 patients with surgical resection of recurrent TC, but the site, completeness of resection, and the number of lesions were not available, and all the patients underwent subsequent chemotherapy, which appeared to be associated with more favorable post-recurrence survival compared to radiotherapy plus chemotherapy [30]. In our series, 16 patients underwent surgical resection of recurrent TC, of whom 8 (50%) received subsequent chemotherapy with or without radiotherapy. In multivariable analysis, the significance of chemotherapy after surgery for recurrence was undetermined and this, therefore, requires a further study.
Resection of recurrent TC and TNEC, as well as the initial resection, should aim to achieve a complete resection; however, 6 patients of all surgical patients (n = 16) in our series ended up with only a debulking resection. One of the interpretations would be that we may unexpectedly encounter disseminated lesions that were not detected radiologically prior to surgery. In the current literature, there has been no study supporting debulking resection for recurrent TC and TNEC. Our findings suggested that debulking resection should be followed by chemotherapy, as was administered in 5 of 6 patients undergoing debulking resections.
A subgroup analysis of recurrent TNEC included 18 patients. The only significant factor associated with post-recurrence survival was radiotherapy, which was presumably performed in a more palliative setting. The small number of patients with recurrent TNEC did not allow us to identify any other significant factors and the management of recurrent TNEC is thus considered to be similar to those of recurrent TC.
There is also limited information on the utility of radiotherapy alone for recurrent TC. In a 2012 report from the Mayo Clinic [9], one of 9 patients with recurrent TC underwent radiotherapy alone for multiple bone metastasis, presumably for palliative purposes, without a response. Three of these 9 patients underwent radiotherapy for supraclavicular lymph node metastases (partial response); multiple bone lesions (stable disease), and liver and multiple mediastinal lymph node metastases (partial response). In our study, radiotherapy for recurrence tended to be associated with a poor prognosis, and only 2 of 10 patients received radiotherapy alone after recurrence. These findings suggest that radiotherapy as a monotherapy is essentially palliative in recurrent TC and TNEC.
There are several limitations associated this study, including the retrospective design; the relatively small sample size, which probably affected the power of the study; little information is available on the performance status and renal functions in our database; insufficient follow-up for thorough evaluation of the treatment outcome in each patient; and inconsistencies in decision-making about treatment. Patient selection and confounding factors presumably affected the results and thus were associated with some bias. Therefore, further and ideally prospective studies with a large sample size and more information are required to confirm our findings.
In conclusion, chemotherapy rather than surgery appears to be the mainstay treatment in managing patients with postoperative recurrent TC and TNEC. Long-term and careful follow-up after the initial resection is recommended. Multidisciplinary treatment including chemotherapy may, therefore, be most effective treatment modality for postoperative recurrent TC and TNEC.
References
Cardillo G, Rea F, Lucchi M, Paul MA, Margaritora S, Carleo F, et al. Primary neuroendocrine tumors of the thymus: a multicenter experience of 35 patients. Ann Thorac Surg. 2012;94(1):241–5 discussion 5–6.
Filosso PL, Yao X, Ahmad U, Zhan Y, Huang J, Ruffini E, et al. Outcome of primary neuroendocrine tumors of the thymus: a joint analysis of the international thymic malignancy interest group and the European Society of Thoracic Surgeons databases. J Thorac Cardiovasc Surg. 2015;149(1):103–9.e2.
Ruffini E, Guerrera F, Brunelli A, Passani S, Pellicano D, Thomas P, et al. Report from the European Society of Thoracic Surgeons prospective thymic database 2017: a powerful resource for a collaborative global effort to manage thymic tumours. Eur J Cardiothorac Surg. 2019;55(4):601–9.
Committee for Scientific Affairs TJAfTS, Shimizu H, Endo S, Natsugoe S, Doki Y, Hirata Y, et al. Thoracic and cardiovascular surgery in Japan in 2016: annual report by the Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg. 2019;67(4):377–411.
Hishida T, Nomura S, Yano M, Asamura H, Yamashita M, Ohde Y, et al. Long-term outcome and prognostic factors of surgically treated thymic carcinoma: results of 306 cases from a Japanese nationwide database study. Eur J Cardiothorac Surg. 2016;49(3):835–41.
Filosso PL, Yao X, Ruffini E, Ahmad U, Antonicelli A, Huang J, et al. Comparison of outcomes between neuroendocrine thymic tumours and other subtypes of thymic carcinomas: a joint analysis of the European Society of Thoracic Surgeons and the international thymic malignancy interest group. Eur J Cardiothorac Surg. 2016;50(4):766–71.
Park IK, Kim YT, Jeon JH, Kim HS, Hwang Y, Seong YW, et al. Importance of lymph node dissection in thymic carcinoma. Ann Thorac Surg. 2013;96(3):1025–32 discussion 32.
Ruffini E, Detterbeck F, Van Raemdonck D, Rocco G, Thomas P, Weder W, et al. Thymic carcinoma: a cohort study of patients from the European Society of Thoracic Surgeons database. J Thorac Oncol. 2014;9(4):541–8.
Hamaji M, Allen MS, Cassivi SD, Nichols FC 3rd, Wigle DA, Deschamps C, et al. The role of surgical management in recurrent thymic tumors. Ann Thorac Surg. 2012;94(1):247–54 discussion 54.
Fiorelli A, D’Andrilli A, Vanni C, Cascone R, Anile M, Diso D, et al. Iterative surgical treatment for repeated recurrences after complete resection of thymic tumors. Ann Thorac Surg. 2017;103(2):422–31.
Hamaji M, Shah RM, Ali SO, Bettenhausen A, Lee HS, Burt BM. A meta-analysis of postoperative radiotherapy for thymic carcinoma. Ann Thorac Surg. 2017;103(5):1668–75.
Miyata R, Hamaji M, Omasa M, Nakagawa T, Sumitomo R, Huang CL, et al. Survival outcomes after minimally invasive thymectomy for early-stage thymic carcinoma. Surg Today. 2019;49(4):357–60.
Filosso PL, Guerrera F, Rendina AE, Bora G, Ruffini E, Novero D, et al. Outcome of surgically resected thymic carcinoma: a multicenter experience. Lung Cancer. 2014;83(2):205–10.
Zhao Y, Gu H, Fan L, Han K, Yang J, Zhao H. Comparison of clinical features and survival between thymic carcinoma and thymic carcinoid patients. Eur J Cardiothorac Surg. 2017;52(1):33–8.
Omasa M, Date H, Sozu T, Sato T, Nagai K, Yokoi K, et al. Postoperative radiotherapy is effective for thymic carcinoma but not for thymoma in stage II and III thymic epithelial tumors: the Japanese Association for Research on the Thymus Database Study. Cancer. 2015;121(7):1008–166.
Mizuno T, Okumura M, Asamura H, Yoshida K, Niwa H, Kondo K, et al. Surgical management of recurrent thymic epithelial tumors: a retrospective analysis based on the Japanese nationwide database. J Thorac Oncol. 2015;10(1):199–205.
NCCN clinical practice guidelines in Oncology. Thymomas and Thymic Carcinomas, Available at NCCN, www.nccn.org/professionals/physician_gls/pdf/thymic_blocks.pdf Accessed Apr 14, 2017.
Girard N, Ruffini E, Marx A, Faivre-Finn C, Peters S, Committee EG. Thymic epithelial tumours: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v40–55.
JLCS clinical practice guidelines in Thymic Epithelial Tumors, Available at JLCS, www.haigan.gr.jp/guideline/2019/3/2/190302030100.html#3-2 Accessed Feb 18, 2020.
Lemma GL, Lee JW, Aisner SC, Langer CJ, Tester WJ, Johnson DH, et al. Phase II study of carboplatin and paclitaxel in advanced thymoma and thymic carcinoma. J Clin Oncol. 2011;29(15):2060–5.
Furugen M, Sekine I, Tsuta K, Horinouchi H, Nokihara H, Yamamoto N, et al. Combination chemotherapy with carboplatin and paclitaxel for advanced thymic cancer. Jpn J Clin Oncol. 2011;41(8):1013–6.
Kim HS, Lee JY, Lim SH, Sun JM, Lee SH, Ahn JS, et al. A prospective phase ii study of cisplatin and cremophor EL-free paclitaxel (Genexol-PM) in patients with unresectable thymic epithelial tumors. J Thorac Oncol. 2015;10(12):1800–6.
Igawa S, Murakami H, Takahashi T, Nakamura Y, Tsuya A, Naito T, et al. Efficacy of chemotherapy with carboplatin and paclitaxel for unresectable thymic carcinoma. Lung Cancer. 2010;67(2):194–7.
Hirai F, Yamanaka T, Taguchi K, Daga H, Ono A, Tanaka K, et al. A multicenter phase II study of carboplatin and paclitaxel for advanced thymic carcinoma: WJOG4207L. Ann Oncol. 2015;26(2):363–8.
Inoue A, Sugawara S, Harada M, Kobayashi K, Kozuki T, Kuyama S, et al. Phase II study of Amrubicin combined with carboplatin for thymic carcinoma and invasive thymoma: North Japan lung cancer group study 0803. J Thorac Oncol. 2014;9(12):1805–9.
Moore RR, Nagai H, Miller RA, Hardisty JF, Allison N, Shockley KR, et al. Comparative incidences and biological outcomes for thymoma in various rat strains in national toxicology program studies. Toxicol Pathol. 2019;47(7):833–41.
Lee SS, Park WY, Chi JG, Seo JW, Kim JI, Kim CW, et al. Thymic epithelial tumor progression in an SV40T transgenic mouse model. Cortical thymoma-thymic carcinoma sequence Virchows Arch. 1998;432(1):33–42.
Berghmans T, Durieux V, Holbrechts S, Jungels C, Lafitte JJ, Meert AP, et al. Systemic treatments for thymoma and thymic carcinoma: a systematic review. Lung Cancer. 2018;126:25–31.
Hirai F, Toyozawa R, Nosaki K, Seto T. Are anthracycline-based regimens truly indicated to be the standard chemotherapy regimen for thymic carcinoma? J Thorac Oncol. 2016;11:115–21.
Okumura M, Shiono H, Inoue M, Tanaka H, Yoon HE, Nakagawa K, et al. Outcome of surgical treatment for recurrent thymic epithelial tumors with reference to world health organization histologic classification system. J Surg Oncol. 2007;95(1):40–4.
Yen YT, Lai WW, Chang KW, Chang KC, Lee SC, Lin SH, et al. Factors predicting recurrence and postrecurrence survival in completely resected thymic carcinoma. Ann Thorac Surg. 2014;97(4):1169–75.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
RM and MH designed the study, contributed to the analysis and interpretation of data, and wrote the initial draft of the manuscript. HD assisted in the preparation of the manuscript. All other authors contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflicts of interest
All authors declared that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyata, R., Hamaji, M., Omasa, M. et al. The treatment and survival of patients with postoperative recurrent thymic carcinoma and neuroendocrine carcinoma: a multicenter retrospective study. Surg Today 51, 502–510 (2021). https://doi.org/10.1007/s00595-020-02102-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02102-7