Abstract
Purpose
There are many treatment choices for hepatocellular carcinoma (HCC), one of which is proton beam therapy (PBT). The purpose of this study was to compare surgical resection (SR) and PBT to clarify the prognostic factors for operable HCC based on a single institution’s database.
Methods
Patients with single primary nodular HCC ≤ 100 mm without vessel invasion on pretreatment imaging were divided into the SR group and PBT group. In the PBT group, the patients with unresectable HCC due to their liver function and/or performance status were excluded.
Results
There were 314 and 31 patients who underwent SR and PBT, respectively. The median survival time in the SR group was significantly better than in the PBT group (104.1 vs. 64.6 months, p = 0.008). Regarding the relapse-free survival (RFS), there was no significant difference between the SR and PBT groups (33.8 vs. 14.0 months, p = 0.099).
Conclusion
The RFS was comparable between the PBT and SR groups. However, the PBT group had a significantly worse overall survival than the SR group. SR may therefore be favorable as an initial treatment for HCC compared to PBT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common and deadly cancers as the fifth-most common cause of cancer-related death worldwide [1, 2]. There are many treatment choices for HCC, including surgical resection (SR), liver transplantation, radiofrequency ablation (RFA), transarterial chemoembolization (TACE), molecular-targeted drugs [3], radiation therapy, and proton beam therapy (PBT). PBT has a Bragg peak peculiar to a charged particle beam that enables the delivery of a conformal high dose to a localized target volume, which improves the local control rate and reduces the rate of normal tissue impairment [4]. Some reports have shown a 5-year local tumor control rate of over 80% and a 5-year survival rate of 24–45% in patients with locoregional HCC [5,6,7]. The efficacy and safety of PBT for HCC are being increasingly recognized, and PBT may be considered a curative treatment similar to SR and RFA in selected patients [7, 8]. However, most previous reports suggesting the efficacy of PBT targeted cases of HCC that were unresectable due to a poor liver function and/or performance status (PS) [9]. No report has compared the long-term outcomes between PBT and SR for HCC.
The present study compared PBT and SR to clarify the prognostic factors for operable HCC based on a single institution’s database.
Methods
The clinical records of patients who received primary treatment for HCC between August 2003 and November 2017 were reviewed. Patients who received SR or PBT for single nodular HCC ≤ 100 mm without vessel invasion on pretreatment imaging (potential candidates for PBT) were extracted, and those who were eligible for both SR and PBT were identified. Indications for therapies of HCC were determined at a weekly cancer board meeting. HCC was diagnosed before treatment by typical findings of computed tomography or magnetic resonance imaging or pathological findings of a fine-needle biopsy in cases for which a pretreatment diagnosis was difficult to determine by imaging. The patients had the details of HCC treatment, including the therapeutic benefits, risks, and outcomes of different treatment modalities, explained to them. Shared decisions were made between patients and clinicians after the delivery of this detailed explanation.
The patients’ background information and laboratory results were collected and analyzed retrospectively. The variables used in this study were as follows: age, sex, viral infection, blood cell counts, blood biochemistry, tumor markers, tumor status, and Child–Pugh grade. PBT-related toxicities and complications of SR were graded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 5 (National Cancer Institute, Bethesda, MD, USA), and Clavien–Dindo (CD) Classification, respectively [10].
This study was retrospective, and we obtained approval (No. 1856) from the Institutional Review Board of Shizuoka Cancer Center for the exception of patients’ consent. In addition, the content of this study was presented in the ethical disclosure section of our institution’s website (https://www.scchr.jp/clinicaltrial/wp-content/uploads/sites/13/2016/11/keizi30-8-12.pdf), and all patients had opportunity to opt out of the study. This study was conducted in accordance with the ethical standards of the Declaration of Helsinki. All patients were informed of the details of the standard therapies and PBT for HCC.
SR procedure
The suitability of SR was determined according to Makuuchi’s criteria [11]. The hepatic reserve was assessed using the Child–Pugh classification [12] and liver damage criteria [13], including the indocyanine green retention rate at 15 min (ICG R15). The details of the SR strategy and procedure have been previously reported [14]. The types of hepatectomies were defined according to the Brisbane 2000 terminology as minor (two liver segments or fewer) or major (three liver segments or more) [15].
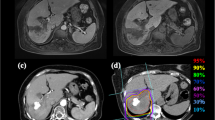
Proton beam irradiation
In this study, patients selected PBT therapy after being informed that they were eligible for both SR and PBT therapies. Patients were deemed eligible for PBT if they had a single nodular HCC ≤ 100 mm without vessel invasion on pretreatment imaging. Before treatment planning, metallic fiducial markers were implanted in the vicinity of the target tumor as landmarks. The clinical target volume involved the tumor volume with a 5–10-mm margin in all directions. The schedule of fractionated PBT was selected from among three options depending on the tumor location according to the proposal of the Japanese Society for Radiation Oncology. A total dose of 66.0 GyE in 10 fractions was selected for peripheral liver tumors, 72.6–76.0 GyE in 20–22 fractions was selected for hepatic hilar tumors, and 74.0–76.0 GyE in 37–38 fractions was selected for tumors that were adjacent to the gastrointestinal tract [16, 17].
Statistical analyses
Continuous variables are presented as the median and range and were compared using the Mann–Whitney U test. The categorical variables were compared using the Chi-square test or Fisher’s exact test, as appropriate. The overall survival (OS) and relapse-free survival (RFS) were estimated using the Kaplan–Meier method. The survival period was defined as the time between the day of SR or PBT conclusion and the event date (any death for the OS and recurrence for the RFS). Differences in the survival and relapse-free time between the two groups were evaluated using the log-rank test. Factors affecting the survival and recurrence were identified by a multivariate analysis using the Cox proportional hazards model. A p value < 0.05 was considered statistically significant. To minimize the influence of potential confounders on the selection bias, propensity scores were generated using binary logistic regression. Independent variables entered into the propensity model included the performance status, platelet count and viral infection. One-to-one matching between the groups was accomplished using the nearest-neighbor matching method. All statistical analyses were performed using the EZR software program (Saitama Medical Center, Jichi Medical University, Saitama, Japan).
Results
Patients
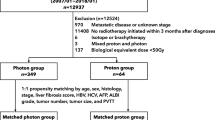
During the study period, 799 patients underwent primary treatment for HCC. We extracted 540 patients with single nodular HCC ≤ 100 mm without vessel invasion. We excluded 120 patients receiving radiofrequency ablation. Among the 106 patients in the PBT group, we extracted 31 who were eligible for both SR and PBT but refused SR and ultimately elected to undergo PBT. The present study ultimately included 314 patients as the SR group and 31 as the PBT group (Fig. 1).
Patient characteristics
The patient and tumor characteristics are shown in Table 1. This study included 269 men and 76 women with a median age of 71 years (range 39–87 years). The median tumor size was 35 mm (7–100 mm). The SR group included significantly fewer patients with a poor PS than the PBT group. The platelet count in the SR group was significantly higher than in the PBT group. In the PBT group, all of the patients completed PBT with a total median dose of 73.5 GyE (range 47.6–78.4 GyE). The prescribed dose was administered at the discretion of the treating physician.
Results of univariate and multivariate analyses to identify the prognostic factors and predictors of recurrence
In the SR group and PBT group, the median length of follow-up was 64.2 months (95% CI 56.1–71.8) and 56.3 months (95% CI 22.2–82.3), respectively (Kaplan–Meier estimate), with no significant differences between periods (p = 0.070). The 3- and 5-year survival rates and median survival time were significantly better in the SR group than in the PBT group (84.5% vs. 69.2%, 75.8% vs. 51.1% and 104.1 vs. 64.6 months, respectively: p = 0.008) (Fig. 2a). A univariate analysis of the OS is shown in Table 2. A multivariate analysis showed that PBT for HCC (hazard ratio [HR] 2.188, 95% confidence interval [CI] 1.185–4.038, p = 0.008), alpha-fetoprotein (AFP) (HR 2.054, 95% CI 1.372–3.076, p = 0.003), the PS (HR 2.039, 95% CI 1.261–3.297, p = 0.004) and age (HR 1.787, 95% CI 1.187–2.691, p = 0.027) were independent prognostic factors (Table 2).
Conversely, the 3- and 5-year RFS rates of the SR vs. PBT groups were 47.9% vs. 38.9% and 37.3% vs. 31.1%, respectively, and the median RFS was 33.8 vs. 14.0 months with no significant difference between the groups (p = 0.099) (Fig. 2b). Furthermore, a multivariate analysis showed that higher AFP (HR 1.606, 95% CI 1.205–2.141, p < 0.001) and aspartate aminotransferase levels (HR 1.466, 95% CI 1.092–1.967, p = 0.011) were independent prognostic factors (Table 2).
A comparison of complications after treatment
In the SR group, complications of CD [10] Grade ≥ IIIa were confirmed in 34 patients (10.8%). One patient (3.2%) experienced grade 3 toxicity (CTCAE) of gastric ulcer in the PBT group, and the rates of toxicities or complications were not significantly different between the SR and PBT groups (p = 0.343). The median postoperative hospital stay in the SR group was 10 days (range 3–103 days), whereas, in principle, PBT was conducted at the outpatient clinic, so hospitalization was not necessary. The Grade ≥ IIIa complications in the SR group were bile leakage (20 cases), postoperative bleeding (4 cases), refractory ascites (4 cases), aspiration pneumonia (3 cases), arrhythmia (2 cases), pleural effusion (2 cases), wound dehiscence (1 case), intraabdominal abscess (1 case) and stomach ulcer (1 case).
A comparison of recurrence sites, therapy for recurrence and causes of death
There was no significant difference in the recurrence rate between the SR and PBT groups (52.9% vs. 51.6%, p = 1.000). However, the PBT group had local recurrence significantly more frequently than the SR group (19.4% vs. 2.2%, p < 0.001) (Table 3). In addition, there was a significant difference among the kinds of therapy for recurrence (SR, PBT and RFA vs. others), as one SR, one PBT and no RFA therapies tended to be selected for recurrence lesions in the PBT group (p = 0.031). Furthermore, the PBT group had significantly larger proportion of patients who died of pneumonia than the SR group (25.0% vs. 3.3%, p = 0.020) (Table 3).
Results of univariate and multivariate analyses to identify the prognostic factors after therapy for recurrence
The median survival after recurrence in the SR and PBT groups was 63.0 and 40.2 months, respectively (p = 0.196). In a multivariate analysis of the OS after recurrence, the PS (≥ 1) (HR 3.508, 95% CI 2.207–6.069, p < 0.001) and therapy for recurrent tumors (others vs. SR, PBT and RFA) (HR 2.016, 95% CI 1.261–3.224, p = 0.003) were prognostic factors (Table 1, supplementary material).
Results of univariate and multivariate analyses to identify the prognostic factors and predictors of recurrence limited to patients with a PS of 0
A multivariate analysis of the OS showed PBT as the therapy for HCC (HR 2.493, 95% CI 1.182–5.257, p = 0.016) and elevated AFP levels (HR 1.956, 95% CI 1.243–3.076, p = 0.004) were independent prognostic factors for the patients with a PS of 0 (Table 4). Regarding the RFS, elevated AFP levels (HR 1.713, 95% CI 1.260–2.330, p < 0.001) were the only independent prognostic factor for the patients with a PS of 0 (Table 4).
A comparison of the patient characteristics, OS and RFS after propensity score matching
The pretreatment factors became balanced between the 2 groups after propensity score matching (PSM) (Table 5). The 3- and 5-year survival rates of the SR vs. PBT groups were 81.0% vs. 69.2% and 61.8% vs. 51.1%, respectively, and median survival was 63.5 vs. 64.6 months, with no significant difference between the groups (p = 0.481). The median RFS was 25.7 and 14.0 months in the SR and PBT groups, respectively, which did not reach statistical significance (p = 0.643).
Discussion
The present study showed that PBT had an RFS comparable to that of SR, although PBT was an independent poor prognostic factor for the survival in patients with primary HCC. However, it remains difficult to draw definitive conclusions regarding the superiority of SR or PBT, as the backgrounds of the two groups in the present study differed markedly. SR may be favorable as an initial treatment for HCC compared to PBT in patients with a good liver function and PS. In contrast, PBT should be considered in patients with a poor PS based on our post-PSM analysis, as the advantage of SR disappeared when there was no significant difference in the PS.
Previous reports showed that PBT was associated with excellent local control rates for HCC [7, 8]. One reason for this excellent local control is that PBT can target HCCs, including microsatellite lesions, by securing adequate safety irradiation margins despite the presence of microsatellite lesions that can cause recurrence in approximately 50% of HCC cases. However, the present study showed that SR was better than PBT with respect to achieving local control. Although some studies have reported that the survival rates of patients undergoing PBT for HCC may be comparable to those of SR and RFA [7, 8], there have been no reports directly comparing the long-term outcomes between PBT and SR for HCC.
In the present study, the RFS rate did not differ significantly between the SR and PBT groups; however, the OS rate in the SR group was significantly better than in the PBT group. We propose two hypotheses for why SR achieved a better survival time than PBT. First, the therapy for recurrent lesions differed significantly between the SR group and the PBT group. A previous study comparing SR and RFA for HCC reported that SR achieves a significantly better RFS rate, whereas the rate of OS after recurrence is not significantly different between SR and RFA [18]. These results imply that tumor recurrence may not crucially determine the prognosis after SR and RFA. The kind of treatment for recurrent lesions may affect the survival time after recurrence. In the present study, the multivariate analysis of the OS after recurrence showed that the type of therapy for recurrent tumors (SR, PBT and RFA vs. others) and the PS were independent prognostic factors. The patients in the PBT group underwent SR and PBT in one case each and no RFA for recurrent tumors because recurrent tumors cannot be detected by ultrasonography, have vascular invasion and are located under the diaphragm. Second, a poor PS has been reported as a prognostic factor for the survival in HCC patients [8, 19]. In the present study, the PS was again confirmed to be an independent prognostic factor for the survival. Based on the patients’ background characteristics in the present study, the rate of a poor PS in the PBT group was higher than in the SR group. We also found that the PBT group had a significantly greater proportion of patients who died of pneumonia than the SR group. A previous study showed a poor PS was associated with the severity and mortality of pneumonia [20]. The high rate of a poor PS in the PBT group may therefore have influenced the survival duration being worse than in the SR group.
After PSM, there were no significant differences in the OS or RFS between the SR and PBT groups. The rate of a poor PS was much higher in the SR group after PSM (35.5%) than before PSM (14.4%). A poor PS may have resulted in the OS and RFS rates being comparable between the SR and PBT groups. The present study suggested that the PS of patients was a very important factor to consider when deciding on the treatment strategy for HCC.
In addition to the treatment outcomes, the quality of life of patients who undergo treatment for HCC is important. Dermatitis, gastrointestinal toxicities (bleeding or ulceration) and hepatic insufficiencies were reported as major possible adverse events after PBT for HCC [9, 21,22,23]. Hong et al. reported that 4.8% patients of PBT experienced grade 3 radiation-induced toxicity of the hepatic function or gastrointestinal ulcers. Kimura et al. [23] reported that PBT achieved high response rates for HCC over 5 cm without accompanying severe toxicity. In the present study, the rates of toxicities or complications were not significantly different between the SR and PBT groups; however, the SR group had more cases of complications than the PBT group. The patients with a poor PS may be better suited to PBT, as PBT is minimally invasive with an RFS comparable to that of SR.
Finally, several limitations associated with the present study should be mentioned. First, there were significant differences in the patient background characteristics. However, the authors believe that the results of the present study reflect the actual clinical situation, which is also an important finding. Furthermore, to avoid such biases, PSM was performed to match the background characteristics between the groups. Another limitation is the small number of subjects due to the retrospective nature of the study and single-institution setting, so further studies in a large population will be needed to verify our findings in the future. A direct comparison between PBT and surgery for HCC is difficult for several reasons, none of which have been reported. However, the Japanese Clinical Oncology Group is now planning a non-randomized prospective concurrent control study between surgery and PBT for HCC [9].
In conclusion, the present findings suggest that patients with a single primary nodular HCC ≤ 100 mm without vessel invasion should undergo SR if they have a good liver function and PS, whereas PBT may be considered in patients with a poor PS. To our knowledge, the present study, while not a prospective one, is the first to compare SR and PBT for HCC.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- PBT:
-
Proton beam therapy
- SR:
-
Surgical resection
- PS:
-
Performance status
- RFS:
-
Relapse-free survival
- RFA:
-
Radiofrequency ablation
- TACE:
-
Transarterial chemoembolization
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- CD:
-
Clavien–Dindo
- ICG R15:
-
Indocyanine green retention rate at 15 min
- OS:
-
Overall survival
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- AFP:
-
Alpha-fetoprotein
- PSM:
-
Propensity score matching
References
El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365(12):1118–27.
Abe T, Saitoh J, Kobayashi D, Shibuya K, Koyama Y, Shimada H, et al. Dosimetric comparison of carbon ion radiotherapy and stereotactic body radiotherapy with photon beams for the treatment of hepatocellular carcinoma. Radiat Oncol (Lond Engl). 2015;10:187.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90.
Bortfeld T, Schlegel W. An analytical approximation of depth-dose distributions for therapeutic proton beams. Phys Med Biol. 1996;41(8):1331–9.
Matsuzaki Y, Osuga T, Saito Y, Chuganji Y, Tanaka N, Shoda J, et al. A new, effective, and safe therapeutic option using proton irradiation for hepatocellular carcinoma. Gastroenterology. 1994;106(4):1032–41.
Chiba T, Tokuuye K, Matsuzaki Y, Sugahara S, Chuganji Y, Kagei K, et al. Proton beam therapy for hepatocellular carcinoma: a retrospective review of 162 patients. Clin Cancer Res. 2005;11(10):3799–805.
Nakayama H, Sugahara S, Tokita M, Fukuda K, Mizumoto M, Abei M, et al. Proton beam therapy for hepatocellular carcinoma: the University of Tsukuba experience. Cancer. 2009;115(23):5499–506.
Fukuda K, Okumura T, Abei M, Fukumitsu N, Ishige K, Mizumoto M, et al. Long-term outcomes of proton beam therapy in patients with previously untreated hepatocellular carcinoma. Cancer Sci. 2017;108(3):497–503.
Igaki H, Mizumoto M, Okumura T, Hasegawa K, Kokudo N, Sakurai H. A systematic review of publications on charged particle therapy for hepatocellular carcinoma. Int J Clin Oncol 2017;23:423–33
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Makuuchi M, Kosuge T, Takayama T, Yamazaki S, Kakazu T, Miyagawa S, et al. Surgery for small liver cancers. Semin Surg Oncol. 1993;9(4):298–304.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–9.
Ikai I, Arii S, Kojiro M, Ichida T, Makuuchi M, Matsuyama Y, et al. Reevaluation of prognostic factors for survival after liver resection in patients with hepatocellular carcinoma in a Japanese nationwide survey. Cancer. 2004;101(4):796–802.
Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K. Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma: a case-controlled study with propensity score matching. J Gastrointest Surg. 2014;18(11):1994–2002.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepato-biliary-pancreatic Surg. 2005;12(5):351–5.
Kawashima M, Furuse J, Nishio T, Konishi M, Ishii H, Kinoshita T, et al. Phase II study of radiotherapy employing proton beam for hepatocellular carcinoma. J Clin Oncol. 2005;23(9):1839–46.
Mizumoto M, Okumura T, Hashimoto T, Fukuda K, Oshiro Y, Fukumitsu N, et al. Proton beam therapy for hepatocellular carcinoma: a comparison of three treatment protocols. Int J Radiat Oncol Biol Phys. 2011;81(4):1039–45.
Liu PH, Hsu CY, Hsia CY, Lee YH, Huang YH, Chiou YY, et al. Surgical resection versus radiofrequency ablation for single hepatocellular carcinoma %3c/= 2 cm in a propensity score model. Ann Surg. 2016;263(3):538–45.
Hsu CY, Lee YH, Hsia CY, Huang YH, Su CW, Lin HC, et al. Performance status in patients with hepatocellular carcinoma: determinants, prognostic impact, and ability to improve the Barcelona Clinic Liver Cancer system. Hepatol (Baltim MD). 2013;57(1):112–9.
Ishiguro T, Kagiyama N, Uozumi R, Odashima K, Kurashima K, Morita S, et al. Risk factors for the severity and mortality of pneumococcal pneumonia: importance of premorbid patients' performance status. J infect Chemother. 2016;22(10):685–91.
Bush DA, Hillebrand DJ, Slater JM, Slater JD. High-dose proton beam radiotherapy of hepatocellular carcinoma: preliminary results of a phase II trial. Gastroenterology. 2004;127(5 Suppl 1):S189–S193193.
Bush DA, Kayali Z, Grove R, Slater JD. The safety and efficacy of high-dose proton beam radiotherapy for hepatocellular carcinoma: a phase 2 prospective trial. Cancer. 2011;117(13):3053–9.
Kimura K, Nakamura T, Ono T, Azami Y, Suzuki M, Wada H, et al. Clinical results of proton beam therapy for hepatocellular carcinoma over 5 cm. Hepatol Res. 2017;47(13):1368–74.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tamura, S., Okamura, Y., Sugiura, T. et al. A comparison of the outcomes between surgical resection and proton beam therapy for single primary hepatocellular carcinoma. Surg Today 50, 369–378 (2020). https://doi.org/10.1007/s00595-019-01888-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-019-01888-5