Abstract
Purpose
A congenital extrahepatic portosystemic shunt (CEPS) associated with hyperammonemia requires occlusion of the shunt vessels. We evaluated the effectiveness and safety of laparoscopic ligation of a CEPS in children with hyperammonemia.
Methods
The subjects of this retrospective study were seven children with hyperammonemia who underwent laparoscopic ligation of a CEPS. Their median age was 5.2 years (range 1–16 years). Before the laparoscopic procedure, a catheter was inserted through the femoral vein and placed in the portal vein via the shunt vessel. The shunt vessel was dissected and taped laparoscopically. After measuring the portal vein pressure under temporal occlusion, the shunt vessels were ligated.
Results
The types of shunts according to location were patent ductus venosus (n = 2), splenorenal shunt (n = 2), gastrorenal shunt (n = 2), and superior mesenteric vein–inferior vena cava shunt (n = 1). Laparoscopic ligation of the shunt vessel was completed uneventfully in all patients. The median portal vein pressure was 19 mmHg after ligation. The median preoperative blood ammonia level was 94 µg/dL (range 71–259 µg/dL), which decreased after ligation in all patients. There was no incidence of postoperative liver failure.
Conclusion
Laparoscopic ligation of a CEPS is safe and effective for children with hyperammonemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A congenital portosystemic shunt (CPSS) is a rare malformation that leads to hyperammonemia, hypermanganesemia, hepatic encephalopathy, pulmonary hypertension, hepatopulmonary syndrome, and liver tumor [1]. CPSSs are divided into intrahepatic- and extrahepatic shunts [2]. Congenital extrahepatic portosystemic shunts (CEPSs) have been further classified into two types: type I—the liver is not perfused with portal blood; and type II— the liver is perfused with portal blood [2].
A portosystemic shunt causing symptoms requires occlusion of the shunt vessels to alleviate or prevent other symptoms [1, 3, 4]. A type II CEPS can be closed surgically or through an interventional radiological procedure [1, 3, 5]. We prefer surgical closure to minimize the risk of migration of embolic material. At our institution, laparoscopic surgical ligation is the procedure of choice for occlusion of a type II CEPS because it is minimally invasive and reliable. We conducted this study to evaluate the usefulness, safety, and effectiveness of laparoscopic ligation of a type II CEPS for children with hyperammonemia.
Methods
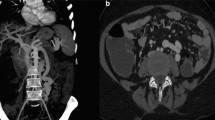
We analyzed, retrospectively, seven cases of laparoscopic ligation of a type II CEPS performed at our institution between January, 2003 and December, 2016. Two of these cases (cases 3 and 5) were reported in 2004 [6]. The study protocol was approved by our institutional review board (protocol no. 15191). We reviewed the medical records and noted the patients’ age at diagnosis, sex, course of laboratory data, shunt location, imaging findings, operative findings, portal vein pressure, treatments, complications related to treatment, and prognosis. The blood ammonia levels were assessed before surgery, then within 1 month, and 6 months to 1 year after surgery. Portal vein pressure was assessed before surgery and at surgery, before and after the ligation. Surgery was indicated when patients had hyperammonemia. Before the laparoscopic procedure, a catheter was inserted through the femoral vein and placed in the portal vein via the shunt vessel. The portal vein pressure was measured using this catheter. The shunt vessel was dissected and taped laparoscopically (Fig. 1). After measuring the portal vein pressure under 15 min of temporal shunt occlusion, the shunt vessels were ligated. The criteria for indicating primary ligation at our institution were as follows: portal vein pressure < 25 mmHg after ligation, pressure gradient < 5 mmHg at ligation, and absence of signs of intestinal wall edema and redness as would accompany intestinal congestion.
Results
We performed laparoscopic ligation of a type II CEPS in seven patients during the study period. Table 1 summarizes their demographic characteristics. There were five boys and two girls, with a median age at diagnosis of 1.5 years (range 0–14 years) and a median age at surgery of 5.2 years (range 1–16 years). The triggers for diagnosis were hypergalactosemia (n = 4), hyperammonemia (n = 2), and liver function disorder (n = 1). Two patients were also being treated for cardiopulmonary disease. The other patients had no relevant medical history or complications. The types of shunt according to location were a patent ductus venosus shunt (n = 2), a splenorenal shunt (n = 2), a gastrorenal shunt (n = 2), and a superior mesenteric vein–inferior vena cava shunt (n = 1). The median preoperative blood ammonia level was 94 µg/dL (range 71–259 µg/dL; normal blood ammonia level, 5–43 µg/dL). There were no cases of hepatopulmonary syndrome or pulmonary hypertension. Two patients were found to have a liver tumor, diagnosed as focal nodular hyperplasia (FNH) in both. The size of the FNH had decreased by 2 years after surgery in patient no. 6 and was unchanged 6 months after surgery in patient no. 7. There was no sign of hepatic encephalopathy or intracerebral disorder caused by CEPS in any patient. Although one patient (no. 6) had a pervasive developmental disorder, with parkinsonism and hallucinations, it was not clear whether these conditions were related to hyperammonemia.
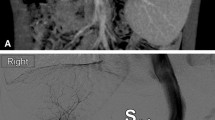
We performed primary ligation in all patients in accordance with the institutional criteria mentioned above. Table 2 shows the surgical findings. The median operative time was 157 min (range 126–182 min). Laparoscopic ligation of the shunt vessel was completed without complications. The median portal vein pressure was 18 mmHg (range 13–20 mmHg) before ligation and 19 mmHg (range 13–23 mmHg) after ligation. The median pressure gradient was 2 mmHg (range 0–3 mmHg). Blood ammonia levels decreased after ligation in all patients and normalized in five patients (Fig. 2). The two patients with cardiovascular disease (nos. 6 and 7) continued to take oral lactulose because of a mild elevation in their blood ammonia level. The median follow-up time was 6.7 years (range 1.4–14.7 years). There was no recurrence of hyperammonemia or postoperative liver failure.
Discussion
CPSS is classified into various types according to the location of the shunt and the presence of intrahepatic portal flow [1,2,3,4, 7]. In this study, we treated type II CEPSs, in which the shunt vessels existed in the extrahepatic lesion and intrahepatic portal flow was perfused with portal blood. Patients with CPSS present with a wide spectrum of symptoms and complications that may develop during their lifetime. In pediatric patients, hyperammonemia or hypergalactosemia is usually diagnosed [1, 4]. Galactosemia without enzyme deficiency may be diagnosed by the routine screening of neonates [1, 4, 8]. Hepatic encephalopathy, hepatopulmonary syndrome, and pulmonary hypertension are the prominent manifestations of long-term portosystemic shunting and are most often observed in children [1, 3, 5]. Although the optimal timing of treatment for children with CEPS has not been established, some review papers suggest that all patients with extrahepatic shunts should receive early intervention regardless of the symptoms, as early treatment has been shown to prevent hepatopulmonary syndrome and other pulmonary complications, and may allow the progress of intellectual and psychosocial development [1, 3, 4]. The likelihood of encephalopathy increases with age and is related to the shunt flow [1, 5]. Children whose condition is undiagnosed or who are placed under long-term surveillance for mild symptoms and remain untreated may develop clinical symptoms at a later age [1, 9, 10]. Unusual findings such as parkinsonism and spastic paraparesis have also been described in association with hyperammonemia [1, 9]. Considering these facts, early intervention for hyperammonemia and CEPS may be important to prevent encephalopathy, hepatopulmonary syndrome, and intellectual and psychosocial disorders. Therefore, surgery is now indicated at our institution when patients have hyperammonemia uncontrolled by non-surgical treatment.
A high portal vein pressure after ligation may induce postoperative liver failure [1, 8, 11, 12]. We measure the intraoperative portal vein pressure routinely, before and after temporal ligation, to allow us to decide whether primary ligation is possible according to our institutional criteria. The criteria for primary ligation are controversial and not yet established. The criteria at our institution mentioned in “Methods” section are based on our preliminary experiences and previous reports [3, 4, 6, 13, 14]. As there was no incidence of postoperative liver failure in this series, we consider that our criteria were adequate.
For type II CEPS, shunt occlusion is usually performed using a surgical or interventional radiological approach [1, 3,4,5,6,7, 11,12,13,14,15,16]. Although interventional radiology is a less invasive method, the choice between a radiological or surgical approach depends on local expertise, shunt anatomy and size, and the patient’s general condition [1, 3, 7, 16]. If the shunt is wide and short, or embolization has failed, the surgical approach is preferred [1, 13]. At our institution, surgical intervention, especially laparoscopic intervention, is the treatment of choice for patients with type II CEPS [6, 14]. The laparoscopic approach is as minimally invasive as the interventional radiological approach. With the laparoscopic approach, it is possible not only to measure the portal vein pressure, but also to check, under direct view, for intestinal congestion and the liver appearance at the time of ligation, which is impossible with the interventional radiological approach. In our study, laparoscopic ligation of type II CEPS was possible for various shunts in children aged 1–16 years, without complications or recurrence of hyperammonemia.
The limitation of laparoscopic shunt ligation is that it is not suitable for patients with intrahepatic CPSS. Moreover, the limitations of this study were the small number of patients, the single-institution design, and the short follow-up.
Conclusions
We performed laparoscopic ligation of type II CEPS at various locations in children aged 1–16 years. Our ligation criteria proved useful for preventing postoperative liver failure. Laparoscopic ligation of type II CEPS carries no risk of inadvertent migration or pulmonary embolization of embolic agents, unlike interventional radiology. Furthermore, it is a safe and effective method for reducing serum ammonia levels and preventing hepatopulmonary syndrome, pulmonary complications, and intellectual or developmental disorders.
Abbreviations
- CPSS:
-
Congenital portosystemic shunt
- CEPS:
-
Congenital extrahepatic portosystemic shunt
References
Papamichail M, Pizanias M, Heaton N. Congenital portosystemic venous shunt. Eur J Pediatr. 2018;177:285–94.
Morgan G, Superina R. Congenital absence of the portal vein: two cases and a proposed classification system for portasystemic vascular anomalies. J Pediatr Surg. 1994;29:1239–41.
Sokollik C, Bandsma RH, Gana JC, van den Heuvel M, Ling SC. Congenital portosystemic shunt: characterization of a multisystem disease. J Pediatr Gastroenterol Nutr. 2013;56:675–81.
Bernard O, Franchi-Abella S, Branchereau S, Pariente D, Gauthier F, Jacquemin E. Congenital portosystemic shunts in children: recognition, evaluation, and management. Semin Liver Dis. 2013;32:273–87.
Hara Y, Sato Y, Yamamoto S, Oya H, Igarashi M, Abe S, et al. Successful laparoscopic division of a patent ductus venosus: report of a case. Surg Today. 2013;43:434–8.
Kimura T, Soh H, Hasegawa T, Sasaki T, Kuroda S, Yuri E, et al. Laparoscopic correction of congenital portosystemic shunt in children. Surg Laparosc Endosc Percutaneous Tech. 2004;14:285–8.
Kanazawa H, Nosaka S, Miyazaki O, Sakamoto S, Fukuda A, Shigeta T, et al. The classification based on intrahepatic portal system for congenital portosystemic shunts. J Pediatr Surg. 2015;50:688–95.
Yagi H, Takada Y, Fujimoto Y, Ogura Y, Kozaki K, Ueda M, et al. Successful surgical ligation under intraoperative portal vein pressure monitoring of a large portosystemic shunt presenting as an intrapulmonary shunt: report of a case. Surg Today. 2004;34:1049–52.
Lautz TB, Tantemsapya N, Rowell E, Superina RA. Management and classification of type II congenital portosystemic shunts. J Pediatr Surg. 2011;46:308–14.
Siegel D, Marder R, Palvanov A. Asymptomatic intrahepatic portosystemic venous shunt: to treat or not to treat? Int J Angiol. 2015;25:193–8.
Matsuura T, Takahashi Y, Yanagi Y, Yoshimaru K, Yamamura K, Morihana E, et al. Surgical strategy according to the anatomical types of congenital portosystemic shunts in children. J Pediatr Surg. 2016;51:2099–104.
Sanada Y, Urahashi T, Ihara Y, Wakiya T, Okada N, Yamada N, et al. The role of operative intervention in management of congenital extrahepatic portosystemic shunt. Surgery. 2011;151:404–11.
Kamimatsuse A, Onitake Y, Kamei N, Tajima G, Sakura N, Sueda T, et al. Surgical intervention for patent ductus venosus. Pediatr Surg Int. 2010;26:1025–30.
Kamata S, Kitayama Y, Usui N, Kuroda S, Nose K, Sawai T, et al. Patent ductus venosus with a hypoplastic intrahepatic portal system presenting intrapulmonary shunt: a case treated with banding of the ductus venosus. J Pediatr Surg. 2000;35:655–7.
Passalacqua M, Lie KT, Yarmohammadi H. Congenital extrahepatic portosystemic shunt (Abernethy malformation) treated endovascularly with vascular plug shunt closure. Pediatr Surg Int. 2011;28:79–83.
Papamichail M, Ali A, Quaglia A, Karani J, Heaton N. Liver resection for the treatment of a congenital intrahepatic portosystemic venous shunt. Hepatobiliary Pancreat Dis Int HBPD INT 2016;15:329–333
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yuichi Takama and his co-authors have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Takama, Y., Ueno, T., Umeda, S. et al. Laparoscopic ligation of a congenital extrahepatic portosystemic shunt for children with hyperammonemia: a single-institution experience. Surg Today 49, 323–327 (2019). https://doi.org/10.1007/s00595-018-1731-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1731-y