Abstract
Purpose
The Frey procedure is an effective surgery for chronic pancreatitis (CP) patients who have pancreatic head lesions with dilation of the main pancreatic duct. However, pancreatic tail lesions can cause relapsing pancreatitis after the procedure. Therefore, additional distal pancreatectomy (DP) might complement the therapeutic effect of the Frey procedure in controlling inflammation of the pancreatic tail. The Frey procedure with DP (Frey + DP) is indicated for inflammatory lesions in the pancreatic head and tail. In this study, we assessed the usefulness of Frey + DP using the retrospective clinical data of our cases.
Methods
The clinical outcomes were compared between CP patients who underwent the Frey procedure (N = 44) and Frey + DP (N = 13) from January 2005 to April 2016.
Results
Frey + DP showed similarly good therapeutic effects to the Frey procedure with regard to the postoperative stay, morbidity, mortality, pain relief and nutrition, although the Frey + DP had a longer operative time, more bleeding and higher incidence of diabetes mellitus than the Frey procedure because of the additional DP. One patient in the Frey group received additional DP because of recurrent pain due to the tail lesion.
Conclusion
Frey + DP can be a promising treatment for CP patients with pancreatic head and tail lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pancreatitis (CP) refers to chronic inflammation of the pancreas caused by the activation of pancreatic enzymes, mostly due to alcohol consumptions. The major symptom of CP is abdominal or back pain, and, as the disease progresses, pancreatic exocrine and endocrine insufficiency induce digestive malabsorption and diabetes mellitus (DM) [1].
The primary treatments for CP are lifestyle improvements, such as alcohol cessation, and pain control using analgesics. Endoscopic or surgical intervention is indicated when these conservative treatments fail. Surgical intervention is particularly useful for patients with severe symptoms [2] and is classified into two strategies for CP: pancreatic duct drainage and resection of the inflammatory lesion (pancreatectomy). Pancreatojejunostomy with distal pancreatectomy (Puestow procedure) and longitudinal pancreatojejunostomy (Partington procedure) are considered pancreatic duct drainage, and pancreatoduodenectomy (PD), distal pancreatectomy (DP) and duodenum-preserving pancreatic head resection (Beger procedure) are considered pancreatectomy [3,4,5]. Pancreatic duct drainage is useful for the preservation of the pancreatic function, but it is less effective for cases requiring the control of inflammation in the pancreatic head or tail, in which an inflammatory mass has formed [6]. In contrast, pancreatectomy is suitable for removing local lesions but carries a high risk of pancreatic exocrine and endocrine insufficiency [7].
The Frey procedure, which involves longitudinal pancreatojejunostomy with coring-out of the pancreatic head, theoretically shares the advantages of both pancreatic duct drainage and pancreatectomy [8]. The Frey procedure has been conducted for CP since the 1990s in Japan and has achieved good therapeutic outcomes in terms of pain relief and preservation of the exo- and endocrine functions at our and other Japanese institutions [9,10,11]. Patients with pancreatic head lesions and a dilated main pancreatic duct are good candidates for the Frey procedure. However, the procedure is not effective for patients with severe pancreatic tail lesions, especially when the main pancreatic duct in the pancreatic tail is not dilated. Indeed, we have experienced a few cases of CP with pancreatic tail lesion that recurred after the Frey procedure and then required additional DP [9].
Based on these experiences, we currently perform Frey procedure with DP (Frey + DP) as a novel surgical strategy for CP patients with both pancreatic head and tail lesions. Theoretically, Frey + DP is suitable for those cases, but the therapeutic effect is not fully discussed. We herein report our comparison of the clinical outcomes between the Frey procedure alone and Frey + DP, and show typical cases of CP with both pancreatic head and tail lesions.
Materials and methods
Ethics
The present study protocol was performed in accordance with the ethical standards of the Declaration of Helsinki and approved by the Ethics Committee of Tohoku University Hospital (2017-1-733, 2015-1-790, 2014-1-544).
Patients and study outline
This study was a retrospective and observational study. Consecutive CP patients who underwent the Frey procedure or Frey + DP at our institution from January 2005 to April 2016 were identified using our medical information database and enrolled into the study. Patients who underwent other surgical procedures except for cholecystectomy in addition to these surgeries and who had already undergone DP previously were excluded. Sixty-three CP patients were enrolled in this study initially (50 Frey procedures alone and 13 Frey + DP), and six cases were excluded from the Frey procedure alone group due to undergoing an additional procedure (n = 4) or having undergone preceding DP (n = 2) (Fig. 1).
The perioperative outcomes, including patient characteristics, and perioperative data, including operative time, hemorrhaging volume, postoperative hospital stay, morbidity and mortality, were compared between the Frey procedure and Frey + DP. Complications were defined as grade IIIa or more according to the Clavien–Dindo classification [12, 13]. Long-term outcomes, such as the nutritional status and pain, were assessed at 1 year after surgery. The nutritional status was assessed by the body weight (BW) and serum albumin (Alb) before and 1 year after surgery. Pain before or 1 year after surgery was defined by the regular use of oral analgesics. Postoperative new-onset DM was also monitored. In this study, DM was defined by HbA1c ≥ 6.5% or the administration of antidiabetic drug or insulin. Fourteen patients who did not receive postoperative follow-up were excluded from the analysis: 11 from the Frey procedure alone group and 3 from Frey + DP. One patient who developed pancreatic cancer within 1 year after Frey + DP was also excluded from the analysis. Finally, the long-term outcomes were assessed in 33 CP patients who underwent the Frey procedure alone and 9 patients who underwent Frey + DP (Fig. 1).
Operative procedures
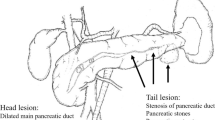
The Frey procedure has been described in detail elsewhere [8, 10]. In brief, the main pancreatic duct was opened along the long axis, and the frontal part of the pancreatic head was cored-out. The proximal jejunum was then longitudinally anastomosed to the opened main pancreatic duct and cored-out pancreatic head. The Frey procedure is indicated for cases with lesions in the pancreatic head and dilatation of the main pancreatic duct.
For cases with severe inflammation and calcification or a symptomatic cyst in the pancreatic tail in addition to the pancreatic head lesion and dilatation of the main pancreatic duct, we performed Frey + DP as a primary surgery [9]. In Frey + DP, the pancreatic tail was resected first, and then the main pancreatic duct was opened from the pancreatic stump. Some patients received additional splenectomy based on whether or not their splenic vessels were preservable. After opening the main pancreatic duct of the body and tail, the pancreatic head was cored-out, as in the Frey procedure. The jejunum was then opened to an appropriate length to cover the pancreatic stump and duct, and anastomosed longitudinally.
Statistical analyses
All statistical analyses were performed with the JMP Pro® software program, ver. 12.2.0, for Macintosh (SAS Institute Inc., Cary, NC, USA). Wilcoxon’s signed-rank test or Wilcoxon’s rank sum test was applied for continuous variables, and Fisher’s exact test or chi-square test was used for categorical data. A p value < 0.05 was considered to indicate statistical significance. All representative values are expressed as the median ± quartile deviation unless otherwise noted.
Results
Characteristics of the patients
The characteristics of the enrolled patients are shown in Table 1. In the Frey procedure alone group, the median age of the 44 patients was 54.0 ± 8.6 years old. The great majority of the patients were male (86.4%), and the causes of CP were alcohol in 38 cases (86.4%) and idiopathic in 6 cases (13.6%). Preoperative pain was reported in 34 cases (77.3%), and preoperative DM was noted in 18 cases (40.9%). The duration from the onset of CP to surgery was 3.5 ± 3.67 years. Preoperative endoscopic treatment was performed 1.0 ± 1.1 times. A history of acute exacerbation was noted in 31 cases (70.5%). In the Frey + DP group, the median age was 52.0 ± 4.0 years old, and the great majority of the patients were male (84.6%). The causes of CP were alcohol in 11 cases (84.6%) and idiopathic and hereditary in 1 case each. All patients suffered from pain, and 6 (46.2%) had DM before surgery. The duration from the onset of CP to surgery was 2.6 ± 2.6 years. Preoperative endoscopic treatment was performed 1.0 ± 1.0 times. A history of acute exacerbation was noted in eight cases (61.5%). There were no significant differences in the clinical backgrounds between the two groups.
Perioperative outcomes
The perioperative data are shown in Table 2. Frey + DP resulted in good therapeutic effects with regard to the postoperative hospital stay, morbidity, mortality, pain relief and nutritional status, just as with the Frey procedure alone (no significant differences in the factors), although Frey + DP had a longer operative time (p < 0.01) and greater bleeding (p < 0.01) than the Frey procedure alone because of the additional DP. In the Frey + DP group, the major morbidities were intraperitoneal abscesses and respiratory disorders, whereas those in the Frey procedure alone group were intraperitoneal abscess, pancreatic fistulas and postoperative bleeding. All patients were free from pain at the time of discharge in both groups, although some patients received oral analgesics.
One patient in the Frey procedure alone group developed recurrent abdominal pain due to a lesion in the pancreatic tail 9 months after the Frey procedure and eventually underwent DP (described in detail later).
Long-term outcomes
Table 3 shows the changes in the BW, Alb, DM and abdominal or back pain before and 1 year after these procedures. There was no significant decrease in the BW or increase in the incidence of DM before and 1 year after either surgery, and the Alb was significantly improved after both (Frey procedure alone; p < 0.01, Frey + DP; p = 0.036). Ten patients who underwent the Frey procedure alone and one who underwent Frey + DP had recurrent abdominal pain 1 year after surgery. Except for one patient who underwent DP for a lesion of the pancreatic tail after the Frey procedure, the symptoms were controlled by oral analgesics in all cases.
Table 4 shows a comparison of the long-term operative outcomes, such as the pancreatic exo- and endocrine functions, between the two procedures. Frey + DP and the Frey procedure had comparable results with regard to the changes in the BW (p = 0.62) and Alb (p = 0.82). However, Frey + DP showed a higher rate of new-onset DM than the Frey procedure alone (p = 0.026).
Case reports
We herein report two CP patients with pancreatic head and tail lesions. One received the Frey procedure as a primary surgery and additional DP due to recurrence of CP (Case 1). Recurrence of CP was able to be prevented in the other by simultaneous Frey + DP (Case 2).
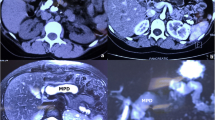
Case 1 was a 31-year-old male with idiopathic CP who underwent the Frey procedure due to persistent pain lasting 7 years. Preoperative abdominal computed tomography (CT) showed pancreatic tail lesions, dilation of the main pancreatic duct and pancreatic stones throughout the entire pancreas (Fig. 2a). The lesion of the pancreatic tail had been detected before the primary surgery, but DP was not performed at that time because we believed that opening the main pancreatic duct to the pancreatic tail and longitudinal anastomosis would relieve the inflammation in the pancreatic tail. The operative time was 267 min, and the bleeding amount was 355 ml. The postoperative course was uneventful, and he was discharged on the 17th postoperative day. However, he developed recurrent abdominal pain due to a lesion in the pancreatic tail 9 months after the Frey procedure (Fig. 2b). We eventually performed DP, and he was released from the symptoms.
Abdominal CT scan of a recurrent case with pancreatic tail lesions after the Frey procedure. a Before the Frey procedure. There were pancreatic stones throughout the entire pancreas with a dilated main pancreatic duct. In addition, the patient had pancreatic tail lesions before the primary Frey procedure. b Recurrent pancreatitis after the Frey procedure. Abdominal pain recurred due to lesions of the pancreatic tail 9 months after the Frey procedure
Case 2 was a 77-year-old male suffering from alcoholic CP who underwent Frey + DP about 2 years after the onset of CP. Preoperative abdominal CT showed pancreatic tail lesions and dilation of the main pancreatic duct (Fig. 3). The operative time was 335 min, and the bleeding amount was 1030 ml. He had grade IIIa respiratory complications, but he was discharged on the 17th postoperative day. He reported no recurrence of pain at 1 year after the surgery.
Discussion
The Frey procedure is recommended for CP patients with pancreatic head lesions and dilation of the main pancreatic duct, and it has become a standard surgery for CP in Japan [1]. However, it has limited efficacy in patients with stenosis of the bile duct or the duodenum and severe lesions in the pancreatic tail [9, 14, 15]. For such cases, additional procedures are combined with the Frey procedure at our institution, according to the complications and location of the CP lesions. For example, choledochojejunostomy can be added to the Frey procedure for cases with bile duct obstruction, and Frey + DP is performed for cases with pancreatic tail lesions.
In the present study, we compared the clinical outcomes of Frey + DP with those of the Frey procedure alone and showed that Frey + DP tended to be performed in cases with severe symptoms (Table 1). In addition, the recurrence rate of pain was lower after Frey + DP (11.1%) than with the Frey procedure alone (38.5%) at 1 year after surgery (Table 3). The feasibility of Frey + DP is equivalent to that of the Frey procedure alone with regard to the postoperative hospital stay, morbidity and mortality. Although Frey + DP showed a significantly longer operative time and larger bleeding amount than the Frey procedure alone because of additional DP, the addition of DP did not markedly affect the postoperative outcomes of the Frey procedure. The postoperative nutritional status, which reflects the exocrine pancreatic function, was similarly improved in the two groups. We already clarified that the nutritional status after the Frey procedure is superior to that of pancreatic resection [16], and the results of this study also indicated that the feasibility of Frey + DP is comparable to that of the Frey procedure.
The main disadvantage of Frey + DP is the increased rate of new-onset DM compared with the Frey procedure alone. Indeed, 50% (3/6) of the patients in the Frey + DP group showed new-onset DM in our study. Despite the resected area being limited to only part of the pancreatic tail and most of the pancreatic parenchyma being preserved in Frey + DP, half of the patients developed DM after surgery. The high rate of new-onset DM after Frey + DP indicated the impaired endocrine function of the remnant pancreas in CP. Since pancreatectomy reduces the volume of the pancreas, it theoretically impairs the exocrine and endocrine pancreatic functions and can lead to DM, known as pancreatic DM [7]. In the present study, two of the three patients with new-onset DM have maintained a good endocrinal condition under the administration of antidiabetic drugs and a small amount of insulin usage, but the other patient who was unable to quit drinking alcohol showed severe DM due to alcohol abuse. Based on these results, abstinence from alcohol also seems to be important for ensuring the preservation of the postoperative pancreatic function and preventing recurrence of CP.
Two-step surgery, as shown in Case 1 (the Frey procedure as the first surgery, followed by DP when the Frey procedure was ineffective), may be a therapeutic strategy for CP patients to reduce the rate of new-onset DM after Frey + DP. However, performing a second surgery is much more difficult than performing the first surgery due to adhesion, and whether or not a second surgery can be performed safely cannot be confirmed at the time of the first surgery, as the general condition of CP patients is usually impaired. We consider Frey + DP to be an acceptable procedure because new-onset pancreatic DM can be managed by lifestyle improvements and the administration of antidiabetic drugs and insulin. The merits of the procedure for controlling intolerable pain and improving the quality of life outweigh the demerit of postoperative pancreatic DM.
This study was limited by its sample size. Although our institution is a high-volume center for CP in Japan, there were only four patients each year who underwent the Frey procedure at our institution [10]. Therefore, it is difficult to plan a prospective study to compare the Frey procedure alone and Frey + DP for CP patients with head and tail lesions.
There are certain patients with severe lesions in the pancreatic tail who need additional DP after the Frey procedure [9]. Because the therapeutic effects of Frey + DP are supposed to be similar to those of the Frey procedure, simultaneous Frey + DP may be indicated for those patients. At present, we perform simultaneous Frey + DP on patients with severe lesions in the pancreatic tail, such as intense calcification or cystic lesions, especially those with a partially undilated pancreatic duct in the tail that is difficult to open and anastomose.
The reliability of the therapeutic effect of Frey + DP is expected to be clarified with the accumulation of further cases and examinations such as joint research with other institutions.
Conclusion
Frey + DP is a tolerable and useful operation for CP with dilation of the main pancreatic duct and symptomatic lesions in the pancreatic head and tail. It should be considered when performing the Frey procedure for CP patients with pancreatic tail lesions.
References
The Japanese Society of Gastroenterology. Evidence-based clinical practice guidelines for chronic pancreatitis 2015. 2nd edn. Nankodo: The Japanese Society of Gastroenterology; 2015 (in Japanese).
Cahen DL, Gouma DJ, Nio Y, Rauws EA, Boermeester MA, Busch OR, et al. Endoscopic versus surgical drainage of the pancreatic duct in chronic pancreatitis. N Eng J Med. 2007;356:676–84.
Puestow CW, Gillesby WJ. Retrograde surgical drainage of the pancreas for chronic relapsing pancreatitis. Ann Surg. 1958;69:898–907.
Partington PF, Rochelle RL. Modified Puestow procedure for retrograde of the pancreatic duct. Ann Surg. 1969;152:1037–43.
Beger HG, Krautzberger W, Bittner R, Büchler M, Limmer J. Duodenum-preserving resection of the head of the pancreas in patients with severe chronic pancreatitis. Surgery. 1985;97:467–73.
Izbicki JR, Bloechle C, Broering DC, Knoefel WT, Kuechler T, Broelsch CE. Extended drainage versus resection in surgery for chronic pancreatitis: a prospective randomized trial comparing the longitudinal pancreaticojejunostomy combined with local pancreatic head excision with the pylorus-preserving pancreatoduodenectomy. Ann Surg. 1998;228:771–9.
Park JW, Jang JY, Kim EJ, Kang MJ, Kwon W, Chang YR, et al. Effects of pancreatectomy on nutritional state, pancreatic function and quality of life. Br J Surg. 2013;100:1064–70.
Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas. 1987;2(6):701–7.
Egawa S, Motoi F, Sakata N, Kitamura Y, Nakagawa K, Ohtsuka H, et al. Assessment of Frey procedures: Japanese experience. J Hepatobiliary Pancreat Sci. 2010;17(6):745–51.
Sakata N, Egawa S, Motoi F, Goto M, Matsuno S, Katayose Y, et al. How much of the pancreatic head should we resect in Frey’s procedure? Surg Today. 2009;39(2):120–7.
Suzumura K, Hatano E, Okada T, Asano Y, Uyama N, Nakamura I, et al. Short- and long-term outcomes of the Frey procedure for chronic pancreatitis: a single-center experience and summary of outcomes in Japan. Surg Today. 2018;48(1):58–65.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien–Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Sudo T, Murakami Y, Uemura K, Hashimoto Y, Kondo N, Nakagawa N, et al. Short- and long-term results of lateral pancreaticojejunostomy for chronic pancreatitis: a retrospective Japanese single-center study. J Hepatobiliary Pancreat Sci. 2014;21:426–32.
Ueda J, Miyasaka Y, Ohtsuka T, Takahata S, Tanaka M. Short- and long-term results of the Frey procedure for chronic pancreatitis. J Hepatobiliary Pancreat Sci. 2015;22:211–6.
Sato H, Ishida M, Motoi F, Sakata N, Aoki T, Kudoh K, et al. Frey’s procedure for chronic pancreatitis improves the nutritional status of these patients. Surg Today. 2018;48(1):80–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hideaki Sato and the other co-authors have no conflicts of interest to declare in association with this study.
Rights and permissions
About this article
Cite this article
Sato, H., Ishida, M., Motoi, F. et al. Combination of longitudinal pancreaticojejunostomy with coring-out of the pancreatic head (Frey procedure) and distal pancreatectomy for chronic pancreatitis. Surg Today 49, 137–142 (2019). https://doi.org/10.1007/s00595-018-1720-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1720-1