Abstract
Purpose
The surgical sheets that are currently used for congenital cardiovascular surgery have several drawbacks, including material deterioration, calcification, and pseudo-intimal proliferation resulting in hemodynamic disturbance. The aim of this study was to evaluate a newly developed sheet made from a combination of silk fibroin (SF) and a synthetic polymer, thermoplastic polyurethane (TPU), for surgical use.
Methods
The hybrid SF/TPU sheet was a non-woven fabric with nanofibers that was made using the electrospinning method. The mechanical properties of the SF/TPU sheet were characterized. To determine its biocompatibility, part of the wall of the canine descending aorta was replaced with a SF/TPU sheet as a patch. The patches were removed after 3 months and a histological examination was performed.
Results
The flexibility, water permeability, and suture retention strength of the SF/TPU sheet were excellent and equivalent to those of existing sheets. The SF/TPU sheet had excellent handling properties and fit well into the vascular wall without needle hole bleeding. The histological examination revealed that the intimal tissue was restored well over the intraluminal surface of the explanted SF/TPU sheet, the absence of calcium deposition, and minimal inflammatory reaction, without signs of degradation.
Conclusion
The SF/TPU sheet had excellent mechanical properties and tissue biocompatibility. These favorable features and possible biodegradability of the SF portion warrant a long-term follow-up study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the surgical treatment of congenital cardiovascular diseases, surgical sheets are often placed as a patch to correct various anatomical abnormalities. Both an expanded polytetrafluoroethylene (ePTFE) sheet and glutaraldehyde-treated bovine pericardium are currently used for cardiac repair throughout the world. However, these existing products are associated with various problems. For example, when using an ePTFE sheet, it is difficult to prevent or stop a large amount of bleeding from the suture holes at the sites of anastomosis, and thus blood transfusions and the use of hemostatic materials are required in many cases [1]. The use of a bovine pericardium inevitably evokes a host response to a foreign material, and induces both deterioration and calcification-induced involution over time, which may result in new hemodynamic disturbances [2]. Thus, expansion by either catheter intervention or surgical replacement of the patch is often needed. On the other hand, although glutaraldehyde-treated autologous pericardium is frequently used in children, the amount of material is limited. Many improvements and studies of artificial patch materials have been performed to solve these problems, but products with decisive advantages have yet to be developed [3, 4].
Silk fibroin is a promising biocompatible polymer that has long been used as a surgical material, including suture thread [5]. Silk fiber is composed of two types of protein, sericin and fibroin. Silk fiber can be used as a polymer source by removing sericin, which causes type I hypersensitivity, to derive biocompatible silk fibroin (SF) [6, 7].
SF can be used in various forms as a water solution, film, or sponge. In recent years, SF has shown potential as a scaffold for cells in regenerative medicine [8, 9]. Despite its strength, SF alone is not appropriate as a surgical material for reconstructive procedures in cardiovascular surgery, because of its poor flexibility. Thus, we hypothesized that a new sheet for cardiovascular repair could be developed to solve this problem by mixing flexible thermoplastic polyurethane (TPU) with SF. In this study, we determined a proof of concept by evaluating various properties of this new sheet material.
Methods
Preparation of a sheet made from a combination SF and TPU (Fig. 1)
SF was obtained from Bombyx mori silk cocoons and prepared as a sponge-like material, as previously reported [10]. Briefly, a 6% (W/V) SF/TPU solution with a ratio by weight of 1:1 was made from the solution of the obtained SF sponge and TPU (Pellethane®: 2363-80AE, Dow Chemical Co. Michigan, USA) dissolved in 1,1,1,3,3,3-hexafluoro-2-propanol (HFIP). Using this mixture, a sheet with a thickness of 100–500 µm was made using the electrospinning (ES) method [11]. The conditions of the ES method were as follows: (1) applied voltage, 16–20 kV; (2) injection velocity, 12 µl/min; (3) syringe transportation (traverse), 5.0 mm/min; (4) distance between the syringe and the target, 10 cm; (5) temperature 25–30 °C; and (6) relative humidity, 30–50%. The sheet was then allowed to stand for 24 h at 38 °C with a relative humidity of 100% after air-drying. Next, the sheet was immersed in purified water for 72 h to remove the HFIP, and sterilized in a medical package with gamma rays (25 kGy) before implantation in animals.
In a previous study using a rat model (11), SF/TPU sheets of varying ratios were implanted in the abdominal aorta. The SF/TPU = 0:10 (pure TPU) sheet was not acceptable for surgical use because of its extreme flexibility. On the other hand, the SF/TPU = 10:0 (pure SF) sheet showed sufficient strength but little elasticity and was not acceptable for surgical use. Surprisingly, the in vitro mechanical properties and in vivo histological characteristics did not differ among the SF/TPU composite sheets of various mixtures, including 3:7, 5:5 (1:1), and 7:3. Thus, the mixing ratio of SF/TPU = 1:1 was selected for this study.
The evaluation of the physical properties of the SF/TPU sheet
Measurement of the modulus of elasticity
A stress–strain curve was obtained by measuring the relationship between changes in both stress and strain to the sheet. The measurements were performed by stretching both ends of a rectangular piece of sample sheet (15 × 3 mm in width) at the velocity of 2 mm/min for SF alone, TPU alone, and SF/TPU sheets using a tensile apparatus (EZ-test: Shimadzu Seisakusho Co., Ltd., Japan). The measurement was carried out until the elongation reached 100%. The modulus of elasticity (Young’s modulus) was calculated from the elongation 1–2% section of the obtained stress–strain curve (n = 6).
The measurement of blood leakage from needle holes
Suture holes were created by passing a 6-0 polypropylene suture (6-0 Prolene TF-1, ETHICON, Inc. New Jersey, USA) through both the SF/TPU and the ePTFE sheets (0.4 mm ePTFE sheet: W.L Gore & Associates, Inc. New Jersey, USA) and were observed by a magnification scope. In addition, the amount of blood leakage from the suture holes was measured when a fixed pressure (100 mmHg) was continuously applied to the sheets attached to an airtight container filled with heparinized canine blood.
A one-way analysis of variance (ANOVA) for Young’s modulus and a two-way ANOVA multiple comparison test for needle hole leakage were performed. Tukey’s post hoc test was then performed to analyze the significance of the differences. These data were presented as the mean ± standard deviation (SD). P values of < 0.01 were considered to indicate statistical significance.
Implantation of the SF/TPU patch in the canine descending thoracic aorta
A SF/TPU patch was implanted in the descending aorta of beagle dogs to evaluate surgical handling and the biological reaction.
Beagle dogs (male, weight: 9.9 ± 1.1 kg) were anesthetized by the intravenous administration of a short-acting barbiturate (200 mg), followed by inhaled isoflurane (1.5–5%), and were placed on a ventilator. Electrocardiogram readouts and oxygen saturation were continuously monitored during surgery. Cefazolin (0.5 g) was intravenously administered before the skin incision to prevent surgical infection. With the dog in a right lateral position, the descending aorta was exposed via left thoracotomy through the 4th intercostal space. After systemic heparinization, a temporal bypass between the aortic arch and the lower descending aorta was established. Then, after cross-clamping the aorta, an oval-shaped defect was made in the upper descending aorta. Using 6–0 polypropylene continuous suture thread, the defect was filled with a patch (2 cm × 1 cm in size) trimmed from either a SF/TPU sheet or an ePTFE small graft (Gore-Tex. EPTFE Graft II. W.L Gore & Associates, Inc. New Jersey, USA). The animal was extubated after chest closure and received all necessary care until sacrifice.
The evaluation of the biocompatibility of the SF/TPU sheet (early-stage evaluation)
At 3 months after implantation, the animals were euthanized under general anesthesia (according to the above-described method) with the intravenous injection of a fatal dose of thiamylal sodium. The chest was entered through the previous thoracotomy, and the patch with the surrounding native vascular wall was removed en bloc for a histological examination. After careful macroscopic observation, the excised tissue block was fixed with 4% paraformaldehyde. A tube-shaped sample was cut open with a longitudinal incision made on the opposite side of the patch. A sample slice was cut from the center of the patch along the circumferential direction of the aorta and embedded in paraffin. Slices of 5 µm thickness were prepared by microtome sectioning and stained with hematoxylin and eosin (HE) for general histology. Other stains included elastica van Gieson (EVG) for differential staining of collagen, elastin, and other connective tissues and alizarin red (AR) for calcification. Immunohistochemistry was performed with von Willebrand factor (vWF) staining and alpha smooth muscle actin (SMA) staining to detect endothelial cells and neo-arteries, respectively. Briefly, a 1:2000 dilution of anti-vWF rabbit polyclonal antibody (ab6994, Abcam, Cambridge, UK) and a 1:500 dilution of anti-alpha-SMA mouse monoclonal antibody (clone 1A4, Dako, Glostrup, Denmark) were reacted with tissue sections at 4 °C overnight in a refrigerator (MR-CL38NF-W; Mitsubishi Electric, Tokyo, Japan). HRP-conjugated anti-mouse IgG goat polyclonal antibody (Histofine #424134, Nichirei, Tokyo, Japan) and anti-rabbit IgG goat polyclonal antibody (#424144, Nichirei) were then reacted with the tissue sections as a secondary antibody for 30 min at room temperature. Finally, 3,3′-diaminobenzidine (DAB) was used to visualize the positive cells, which were stained brownish-red. Counterstaining of nuclei was performed with Mayer’s hematoxylin; the nuclei were stained pale-purple.
The study was approved by the Animal Research Committee of Osaka Medical College (approval ID #27018). The animals received humane care in accordance with the guidelines of this committee and with the National Institutes of Health Guidelines for the Care and Use of Laboratory Animals.
Results
Preparation of the SF/TPU sheet
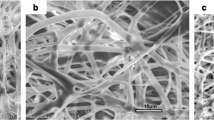
The scanning electron microscope (SEM) of SF/TPU and the commercially available ePTFE sheet are shown in Fig. 2. The SF/TPU sheet is made up of a nonporous and non-woven fabric with layered uniform nano-microfibers. A previous study, in which a structural analysis was performed using solid-state nuclear magnetic resonance, showed that SF and TPU had excellent compatibility with each other on a molecular level [12]. This compatibility allows the SF/TPU electrospinning fiber to be homogenous.
On the other hand, although the ePTFE sheet is also a non-woven fabric constructed from nano-microfibers, the fibers are irregular with islands and micropores (Fig. 2).
The physical properties of the SF/TPU sheet
Figure 3 a shows the stress–strain curves of ePTFE, SF, TPU and SF/TPU composite sheets, while Fig. 3b shows the modulus of elasticity (Young’s modulus) as a numerical constant of solidity and elasticity. The curve and Young’s modulus indicated that the strength of the sheet constructed from TPU alone was too flexible. On the other hand, the sheet constructed from SF alone had sufficient strength, but its elastic property was poor. However, Young’s modulus of the SF/TPU composite sheet was equivalent to that of the ePTFE sheet, indicating that the beneficial properties of SF and TPU (i.e., favorable strength and flexibility) were retained in the composite sheet, suggesting that it was usable as a surgical material.
Measurement of the physical properties of the SF/TPU composite sheet. a The stress–strain relationships of various sheets. Measurement conditions: cross head speed = 2 mm/min, sample size = 15 × 3 mm. b Modulus of elasticity of each sheet (Young’s modulus: Mpa). SF silk fibroin, TPU thermoplastic polyurethane, ePTFE expanded polytetrafluoroethylene
The diameter of the suture hole was larger than that of the suture thread in the ePTFE sheet. On the other hand, the diameters of the suture hole and the thread were same in the SF/TPU sheet (Fig. 4a). The amount of blood leakage from the suture hole in the SF/TPU sheet was significantly smaller than that in the ePTFE sheet, and was equivalent to that in the bovine pericardium (Fig. 4b).
The intraoperative findings of the SF/TPU sheet
Surgical handling, the passing of the surgical suture through the patch, and the fitting of the patch to the native aortic wall were excellent (Fig. 5a). Additional hemostasis was not required to control the bleeding from the suture holes in the SF/TPU sheet. In contrast, the use of a hemostatic collagen sheet was required for 30 min to control the bleeding in the ePTFE sheet (Fig. 5d).
The macroscopic and histological assessment of the excised sheet 3 months after implantation
Macroscopic findings: the SF/TPU and ePTFE patch appeared integrated with the native aortic wall without either stenosis or aneurysmal change at 3 months after implantation (Fig. 5b, e). The luminal surface of the patch was covered with a smooth neointimal layer without thrombus (Fig. 5c, f).
Microscopic findings: the SF/TPU patch was stained light pink by HE and contained fine fibers that were interlaced at a relatively high density (Fig. 6a, b). Minimal inflammatory cell infiltration was found on the outer surface of the patch, especially at the site of anastomosis. Foreign-body giant cells, neutrophil infiltration, bleeding, and tissue necrosis were not observed. Although modest cellular infiltration was found on the surface of the patch and in the space of the electrospinning layers at the edge of the patch (Fig. 6b), damage to the patch structure and self-assembled displacement were generally minimal. A thin layer of smooth muscle and collagen fibers with endothelial cells covered the luminal surface of the patch with seamless continuity from the native aortic wall (Fig. 6b, f). Visible restoration of elastin had yet to occur in the implanted region (Fig. 6c). No calcification was detected in the patch by alizarin red staining (Fig. 6d). Micro-vessel hyperplasia was observed at the edge of the patch (Fig. 6e).
The histological findings of the SF/TPU patch at 3 months after implantation. The upper side of each photo indicates the luminal side of the aorta. a Hematoxylin and eosin staining (low-power field). b Hematoxylin and eosin staining (high-power field). c Elastica van Gieson staining. d Alizarin red staining. e von Willebrand factor immunostaining. f α-Smooth muscle actin immunostaining. SF Silk fibroin, TPU thermoplastic polyurethane
On the other hand, the neointimal tissue that developed on the ePTFE patch was thinner than that on the SF-TPU patch (Fig. 7a, b). Modest inflammatory cell infiltration was found on the outside surface of the ePTFE patch (Fig. 7a, b). Although extracellular matrix was found as an exudate in the spongy space on the surface of the ePTFE patch, there were no viable connections between the matrix and the newly developed tissue surrounding the ePTFE patch. Visible restoration of elastin had yet to occur in the implanted region (Fig. 7c). No calcification was detected in the patch by alizarin red staining (Fig. 7d). A well-developed endothelial layer covered the luminal surface of the neo-intima (Fig. 7e), and a very thin layer of smooth muscle covered the luminal surface of the patch (Fig. 6f).
The histological findings of the ePTFE patch at 3 months after implantation. The upper side of each photo indicates the luminal side of the aorta. a Hematoxylin and eosin staining (low-power field). b Hematoxylin and eosin staining (high-power field). c Elastica van Gieson staining. d Alizarin red staining. e von Willebrand factor immunostaining. f α-Smooth muscle actin immunostaining
Discussion
Three major findings on this proof-of-concept study are as follows. First, the non-woven fabric sheet consisting of electrospun uniform nano-microfiber made from a mixture of SF and TPU achieved excellent flexibility and strength in surgical use. Second, the surgical handling of the sheet was equivalent to that of existing products and the amount of bleeding from the suture holes was significantly less than that observed with the ePTFE sheet. Third, the SF/TPU sheet showed good biological stability with a modest inflammatory response, no calcification, and early-stage tissue regeneration of layered smooth muscle cells and collagen.
Silk fibroin has been used clinically as a promising biomaterial in various forms, including liquid, gel, powder, string, sheets, and tubes [7, 8, 13]. In the cardiovascular field, a small-diameter artificial tube has been tested by various techniques using SF alone [14]. SF has shown excellent tissue compatibility in vivo in all studies, especially in the replacement of the abdominal aorta of rats with a small tube [15]. The endothelial cell layer with the underlying smooth muscle cells was well formed on the luminal surface of the implanted SF tube and the 1-year patency rate was favorable. Moreover, the SF tube was replaced with autologous tissues indicating the biodegradability of SF [15]. Based on the favorable tissue compatibility of the SF tube, we created an electrospun non-woven sheet for a cardiovascular patch using SF alone. However, the results were disappointing because the sheet constructed from SF alone was inflexible and easily torn by surgical sutures. Thus, we hypothesized that adding another polymer to SF would solve these problems while maintaining the benefits of SF. We selected thermoplastic polyurethane because we considered its flexibility to sufficient to improve surgical handling, placement in the tissue, and strength to maintain surgical sutures.
TPU has good biostability and flexibility, and has been used in clinical practice as a covering material for implantable pacemaker leads and for a coronary artery intervention device [16, 17]. In the present study, we selected the ES method to assemble the SF/TPU sheets because various polymers can be widely used with this ES method without any processing required as opposed to other methods that require processing (i.e., knitting or weaving) [18, 19]. In the structural analysis using solid NMR, the SF and TPU showed higher compatibility and stability in fibers of the SF/TPU sheet in comparison to the values reported in previous studies investigating other patch types [12, 20]. The combination of the ES method and the addition of TPU to SF improved the flexibility and strength to the sheet. Finally, this SF/TPU sheet showed improved surgical handling and reduced suture hole bleeding.
Although various types of treatment have been used to enhance biocompatibility and to extend the life span of bovine and porcine tissue materials [21, 22], retraction and hardening due to primary tissue deterioration and calcification as a consequence of calcium deposition are inevitable because of chronic inflammation at the grafts. It should be noted that even ePTFE products are widely known to have calcification resulting in hardening [2]. The histological findings of the explanted SF/TPU patch from the canine aorta demonstrated a modest inflammatory response, no structural deterioration, and no calcium deposition on the patch. Early autologous tissue restoration on the luminal surface of the patch developed, this was especially noticeable when compared to that in the ePTFE patch. This might resolve the problems associated with existing ePTFE products, such as infection and thrombogenesis.
To maintain the viability of the restored tissue on the implanted sheet and the expansion of the sheet in growing children, the sheet needs to be degraded and replaced by autologous tissues. In a previous experiment in which the rat abdominal aorta was replaced with a small-diameter graft composed of SF alone, the biodegradability of SF and the replacement of the graft with autologous tissues were clearly confirmed at 1 year after implantation [14]. Thus, the biodegradability of the SF/TPU sheet was also expected. However, such biodegradability was not been seen histologically within the 3 months after the implantation of the SF/TPU patch in the canine aorta. Additional long-term follow-up studies or further improvements in the production process will be needed to elucidate the biodegradability of the SF/TPU patch and tissue replacement.
Conclusion
This proof-of-concept study showed a new cardiovascular surgical sheet that was made from a combination of SF and TPU using the ES method. When implanted, the SF/PLT sheet had excellent mechanical properties for both surgical handling and the prevention of suture hole bleeding as well as good tissue compatibility. These favorable features and the possible biodegradability of the SF/TPU sheet warrant a long-term follow-up study.
References
Martin P, Mahmood A, Smith SRG, Simms MH, Vohra RK. Randomized trial comparing quixil surgical sealant with kaltostat hemostatic dressing to control suture line bleeding after carotid endarterectomy with ePTFE patch reconstruction. World J Surg. 2005;29:1259–62.
Hayabuchi Y, Mori K, Kitagawa T, Sakata M, Kagami S. Polytetrafluoroethylene graft calcification in patients with surgically repaired congenital heart disease: evaluation using multidetector-row computed tomography. Am Heart J. 2007;153:806.e1–8.
Woo JS, Fishbein MC, Reemtsen B. Histologic examination of decellularized porcine intestinal submucosa extracellular matrix (CorMatrix) in pediatric congenital heart surgery. Cardiovasc Pathol. 2016;25(1):12 – 7.
Iwai S, Sawa Y, Ichikawa H, Taketani S, Uchimura E, Chen C, et al. Biodegradable polymer with collagen microsponge serves as a new bioenginnered cardiovascular prosthesis. J Thorac Cardiovasc Surg. 2004;128:472–9.
Moy RL, Lee A, Zalka A. Commonly used suture materials in skin surgery. Am Fam Physician. 1992;44:2123–8.
Hollander DH. Interstitial cystitis and silk allergy. Med Hypotheses. 1994;43:155–6.
Nakazawa Y, Asakura T. Development of tissue engineering materials based on silk fibroin. Jpn J Silk Sci Tech. 2014;22:23–9. (Japanese).
Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J, et al. Silk based biomaterials. Biomaterials. 2003;24:401–16.
Kim U-J, Park J, Kim HJ, Wada M, Kaplan DL. Three-dimensional aqueous-derived biomaterial scaffolds from silk fibroin. Biomaterials. 2005;26:2775–85.
Ohgo K, Zhao C, Kobayashi M, Asakura T. Preparation of non-woven nanofibers of Bombyx mori silk, Samia cynthia ricini silk and recombinant hybrid silk with electrospinning method. Polymer. 2003;44:841–6.
Shimada K, Higuchi A, Kubo R, Murakami T, Nakazawa Y, Tanaka R. The effect of a silk fibroin/polyurethane blend patch on rat vessels. Organogenesis. 2017;13(4):115–124.
Nakazawa C, Higuchi A, Asano A. Solid-state NMR studies for the development of non-woven biomaterials based on silk fibroin and polyurethane. Polymer J. 2017;49:583–586.
Tamada Y, Kobayashi K, Sumi N. Fibroin sponge safety evaluations (in Japanese). Jpn J Silk Sci Tech. 2015;23:71–3.
Nakazawa Y, Sato M, Takahashi R, Aytemiz D, Takabayashi C, Tamura T, et al. Development of small-diameter vascular grafts based on silk fibroin form Bombyx mori for vascular regeneration. J Biomater Sci Polym Ed. 2011;22:195–206.
Enomoto S, Sumi M, Kajimoto K, Nakazawa Y, Takahashi R, Takabayashi C. Long-term patency of small-diameter vascular graft made from fibroin, a silk-based biodegradable material. J Vasc Surg. 2010;51:155–64.
Szyche MR: Biostability of polyurethane elastomers: a critical review. J Biomater Appl 1988; 3:297–402.
Stokes K, McVenes R, Anderson J. Polyurethane elastomer biostability. J Biomater Appl. 1995;9:321–54.
Dan K, Molamma PP, Guorui J, Seeram R. Guided orientation of cardiomyocytes on electrospun aligned nanofibers for cardiac tissue engineering. J Biomed Mater Res Part B. 2011;98B:379–86.
Vaz CM, van Tuijl S,.Bouten CV, Baaijens FP. Design of scaffolds for blood vessel tissue engineering using a multi-layering electrospinning technique. Acta Biomater. 2005;1(5):575–82.
Nakazawa Y, Asano A, Nakazawa TC, Tsukatani T, Asakura T. Structural characterization of silk-polyurethane composite material for biomaterials using solid-state NMR. Polym J. 2012;44:802–7.
Strange G, Brizard CP, Karl TR, Neethling L. An evaluation of Admedus’ tissue engineering process-treated (ADAPT) bovine pericardium patch (CardioCel) for the repair of cardiac and vascular defects. Expert Rev Med Devices. 2015;12(2):135–41.
Nowocin AK, Southgate A, Gabe SM, Ansari T. Biocompatibility and potential of decellularized porcine small intestine to support cellular attachment and grow. J Tissue Eng Regen Med. 2016;10(1):E23–E33.
Acknowledgements
We would like to express our sincere gratitude to Ms. Atsuko Ueda and to Ms. Madoka Omura for their careful management and surgery of the animal experiments in this study. This work is supported by a Scientific technique research promotion program of agriculture, forestry, fishery and food industry (26051A) from the Japanese Ministry of Agriculture, Forestry and Fisheries and a Grant-in-aid for Scientific Research (KAKENHI: 26462094 and 15H03020) from the Japanese Ministry of Education, Culture, Sports, Science and Technology Japan.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Rights and permissions
About this article
Cite this article
Shimada, R., Konishi, H., Ozawa, H. et al. Development of a new surgical sheet containing both silk fibroin and thermoplastic polyurethane for cardiovascular surgery. Surg Today 48, 486–494 (2018). https://doi.org/10.1007/s00595-017-1615-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1615-6