Abstract
Purpose
To compare the outcomes of laparoscopic surgery vs. open surgery after insertion of a colonic stent for obstructive colorectal cancer.
Methods
Between April 2005 and August 2013, 58 patients underwent surgery after the insertion of a colonic stent for obstructive colorectal cancer. We analyzed the outcomes of the patients who underwent laparoscopic surgery vs. those who underwent open surgery.
Results
We compared blood loss, operative time, hospital stay, and complications in 26 patients who underwent laparoscopic surgery and 32 patients who underwent open surgery. Blood loss was significantly less in the laparoscopic surgery group, but operative time was significantly shorter in the open surgery group. The length of hospital stay was shorter in the laparoscopic surgery group than in the open surgery group, but the difference was not significant. There was no significant difference in postoperative surgical complications between the groups.
Conclusion
The patients who underwent laparoscopic resection had less blood loss, although no significant difference was found in postoperative morbidity or mortality. Thus, laparoscopic resection after stent insertion is a feasible and safe option for patients with obstructive colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is reported that colon cancer develops in the ileus in 10–20 % of cases. Operations such as Hartmann’s procedure and colostomy construction are usually performed as emergency surgery, but the occurrence of complications and mortality is higher than that of elective surgery. As a result, emergency surgery is associated with prolonged hospital stay and high cost [1–6].
In Japan, self-expanding metallic stent (SEMS) treatment for obstructive colorectal cancer was approved for cover by national health insurance in 2012, since when it has been used proactively to treat many malignant colonic obstructions to avoid the need for colostomy. The insertion of an SEMS for colonic obstruction was first reported in Japan in 1991 by Dohmoto, as a palliative treatment for obstructive rectal cancer [7]. Thereafter, stent insertion became the optimal treatment for obstruction in patients with advanced or disseminated malignancies. In recent years, patients with obstructive colorectal cancer who need emergency surgery have undergone temporary insertion of a colonic stent preoperatively [8].
By using a colonic stent for obstructive colorectal cancer it is possible to preoperatively decompress the intestinal tract transanally and perform elective surgery as a bridge to surgery (BTS) without compromising the patient’s quality of life (QOL). Furthermore, laparoscopic surgery can be performed if intestinal tract expansion is sufficiently achieved by the colonic stent insertion [6]. In our department, we have been inserting colonic stents preoperatively for obstructive colorectal cancer since 1993. In this study, we compared the outcomes of laparoscopic surgery vs. open surgery after the insertion of a colonic stent for obstructive colorectal cancer.
Patients and methods
The subjects of this study were 58 patients who underwent surgery after the insertion of a colonic stent for obstructive colorectal cancer between April 2005 and August 2013, at Toho University Ohashi Medical Center.
All patients presented with clinical features of colonic obstruction, and the diagnosis was confirmed with abdominal radiography and/or computed tomography. The colorectal obstruction scoring system (CROSS) classification score was 0 in all patients. Table 1 shows the CROSS classifications: Score 0 signifies obstruction requiring continuous decompression [9].
Patients who presented with features of peritonitis, bowel ischemia, or perforation were deemed unsuitable for stent insertion and underwent emergency surgery without delay. Stents were inserted in eligible patients under endoscopic and fluoroscopic control by colorectal surgeons after obtaining written informed consent. After confirming the site of the obstruction by colonoscopy, a guide wire was passed through the working channel of the endoscope to the proximal part of the colon under fluoroscopic guidance. The guide wire was inserted past the obstruction and followed by a catheter. Water-soluble contrast solution was infused via the catheter to assess the extent of the lesion. After confirming the position of the catheter, the guide wire was inserted through the channel of the endoscope and positioned in the proximal part of the colon. The metallic stent (WallFlex Colonic Stent, Boston Scientific Corporation, Massachusetts, United States and Niti-S, Taewoong Medical, Seoul, South Korea) was inserted over the guide wire under fluoroscopic guidance. The stent type was chosen by an endoscopist. Elective surgery was performed later after the colonic obstruction had been resolved. All patients underwent mechanical bowel preparation with polyethylene glycol solution (Niflec®, Ajinomoto Pharmaceuticals Co., Ltd. Tokyo, Japan) 1 day before surgery and colorectal resection was performed using the stent. Subsequently, those patients whose intestinal tract expansion was sufficiently improved were selected to undergo laparoscopic resection.
The results were evaluated and compared between patients who underwent laparoscopic surgery and those who underwent open surgery. Comparisons between both groups of categorical variables were made using the t test and the Chi square test. A p value of <0.05 was considered significant.
Results
When colonic stents were first introduced, most patients subsequently underwent open surgery. The use of laparoscopic surgery for colon cancer has gradually increased and expanded its application to patients with obstructive colon cancer after stent insertion. In the early phase after stent introduction, laparoscopic surgery was limited to patients with sigmoid colon cancer because of its relative ease in that situation; however, its use has expanded to include most patients now (19 of 21 cases over 2 years) with subsequent improvements in the operative technique. In our department, we have not encountered any case that required conversion from laparoscopic surgery to open surgery. During the period from April 2005 to August 2013, 58 patients who presented with obstructive colorectal cancer underwent the insertion of a metallic stent as a BTS.
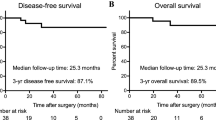
Table 2 summarizes the patient outcomes of the laparoscopic and open surgery groups. We compared blood loss, operative time, hospital stay, and complications in 26 patients who underwent laparoscopic surgery and 32 patients who underwent open surgery. The median age of the laparoscopic surgery group was 65 years old (range 37–93 years), and there were 15 men and 11 women. The median age of the open surgery group was 75 years old (range 40–91 years) and there were 21 men and 11 women. The tumor was located in the right colon in 5 (19.2 %) and 3 (9.3 %) patients and in the left colon in 21 (80.8 %) and 29 (90.7 %) patients from the laparoscopic and open surgery groups, respectively. There were 12 cases of stageIIA, 6 cases of stageIIIB, 2 cases of stageIIIC, 4 cases of stageIVA, and 2 cases of stageIVB in the laparoscopic group and 12 cases of stageIIA, 7 cases of stageIIIB, 1 case of stageIIIC, 8 cases of stageIVA, and 4 cases of stageIVB in the open surgery group.
Blood loss was significantly less in the laparoscopic surgery group (45.6 mL) than in the open surgery group (203 mL; p < 0.05). However, operative time was significantly shorter in the open surgery group (175 min) than in the laparoscopic surgery group (225 min; p < 0.05). The length of hospital stay was shorter in the laparoscopic surgery group (17.8 days) than in the open surgery group (30 days), but the difference was not significant (p = 0.12).
Table 3 lists the postoperative complications. We defined complications according to the JCOG postoperative complications criteria of grade 2 or more [10]. There was no significant difference in postoperative surgical complications between the groups.
Discussion
The management of colonic obstruction varies according to the patient and institutional practice. The conventional 2-stage operation; namely, the emergency Hartmann’s operation, involving resection of the primary lesion and subsequent colostomy closure, has a higher mortality rate than elective surgery [11–13] However, the treatment of acute colonic obstruction has changed dramatically since the introduction of the colonic stent following the first report in 1991 [7]. The use of a metallic stent for colonic obstruction can avoid the need for emergency surgery and is suited to elective surgery. Moreover, because the decompression of the obstructed section of the colon can be achieved and eating becomes possible after stent insertion, elective surgery can improve the nutritional status of patients.
The efficacy and safety of using a metallic stent in acute colonic obstruction have been extensively evaluated. Watt et al. reported technical and clinical success rates of stent insertion of 96.2 and 92 % in 1785; patients with malignant colonic obstruction [14]. In our department, the success rate of colonic stent insertion is 92 %, with good short-term and long-term outcomes and low morbidity [15]. According to a meta-analysis of 601 patients in eight comparative studies of SEMS insertion as a BTS in emergency surgery for acute obstructive colon cancer (SEMS group = 232; emergency surgery group = 369), the SEMS group had a shorter intensive care unit stay, a lower stoma creation rate, and a lower rate of postoperative complications (including leakage) [16]. However, there was no significant difference in mortality or long-term outcomes between the two groups [8, 17]. We previously reported on the high success rate of colonic stents after confirming the safety and feasibility of stent insertion for obstructive colon cancer [9]. Therefore, based on our experience and current evidence, we conclude that stent insertion before surgery, as BTS, is effective and safe, with a high success rate and low complication rate.
Another benefit of the colonic stent as a BTS is its relative ease of use in laparoscopic surgery. Laparoscopic resection for colorectal cancer is associated with satisfactory short-term outcomes, although generally, colonic obstruction is contraindicated for laparoscopic surgery. However, if sufficient intestinal decompression is performed before surgery, it is possible for patients with colonic obstruction to undergo laparoscopic resection.
We are usually able to perform laparoscopic surgery for obstructed colorectal cancer, although the procedure can be made difficult by edema, which can occur around the tumor, or tumor invasion to other organs.
Law et al. were the first to report successful stent insertion followed by laparoscopic resection in a patient with obstructive sigmoid colon cancer. They found laparoscopic resection after stent insertion to be safer than open resection [6]. Stipa et al. compared the clinical effect differences between 16 patients who underwent open resection and 6 patients got treated with laparoscopic resection after stent insertion [18]. The postoperative complication rate for the laparoscopic surgery group was significantly lower than that for the open resection group (0 and 20 %, respectively). Furthermore, the length of hospital stay was shorter after laparoscopic surgery than after open surgery (17.8 vs. 30.0 days, respectively).
Cheung et al. conducted a comparative study on left-sided colonic obstruction of emergency surgery and elective laparoscopic surgery after endoscopic stent insertion. Twenty of 24 patients in the elective laparoscopic surgery group underwent successful laparoscopic treatment. Primary anastomosis was possible in all of the elective laparoscopic surgery patients, although four required temporary stomas. They demonstrated that elective laparoscopic surgery decreased the need for a permanent stoma and increased chance for single-stage surgery, and that laparoscopic resection for obstructive colorectal cancer can be performed safely after the insertion of a metallic stent [19].
In conclusion, the patients in our laparoscopic resection group had less blood loss, although no significant difference was found in postoperative morbidity or mortality. Thus, laparoscopic resection after metallic stent insertion is a feasible and safe option for patients with obstructive colorectal cancer.
References
Abdussamet Bozkurt M, Gonenc M, Kapan S, Kocatass A, Temizgönül B, Alis H. Colonic stent as bridge to surgery in patients with obstructive left-sided colon cancer. JSLS. 2014;18(4). doi:10.4293/JSLS.2014.00161.
Abdussamet van den Berg MW, Ledeboer M, Dijkgraaf MG, Fockens P, ter Borg F, van Hooft JE. Long-term results of palliative stent placement for acute malignant colonic obstruction. Surg Endosc. 2014;29:1580–5.
McArdle CS, McMillan DC, Hole DJ. The impact of blood loss, obstruction and perforation on survival in patients undergoing curative resection for colon cancer. Br J Surg. 2006;93:483–8.
Smothers L, Hynan L, Fleming J, Turnage R, Simmang C, Anthony T. Emergency surgery for colon carcinoma. Dis Colon Rectum. 2003;46:24–30.
van den Berg MW, Sloothaak DA, Dijkkgraaf MG, van der Zaag ES, Bemelman WA, Tanis PJ, et al. Bridge-to-surgery stent placement versus emergency surgery for acute malignant colonic obstruction. BJS. 2014;101:867–73.
Law WL, Poon JT, Fan JK, Lo OS. Colorectal resection after stent insertion for obstructing cancer: comparison between open and laparoscopic approaches. Surg Laparosc Endosc Percutan Tech. 2013;23:29–32.
Dohmoto M. New method—endoscopic implantation of rectal stent in palliative treatment of colorectal neoplastic obstructions. Endosc Dig. 1991;3:1507–12.
Saida Y, Sumiyama Y, Nagao J, Takase M. Stent endoprosthesis for obstructing colorectal cancers. Dis Colon Rectum. 1996;39:552–5.
Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, et al. A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015;82:697–707.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2015. doi:10.1007/s00595-015-1236-x.
Anderson JH, Hole D, McArdle CS. Elective versus emergency surgery for patients with colorectal cancer. Br J Surg. 1992;79:706–9.
Ascanelli S, Navarra G, Tonini G, Feo C, Zerbinati A, Pozza E, et al. Early and late outcome after surgery for colorectal cancer: elective versus emergency surgery. Tumori. 2003;89:36–41.
Alvarez JA, Baldonedo RF, Bear IG, Truán N, Pire G, Alvarez P. Presentation, treatment, and multivariate analysis of risk factors for obstructive and perforative colorectal carcinoma. Am J Surg. 2005;190:376–82.
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ. Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg. 2007;246:24–30.
Saida Y, Enomoto T, Takabayashi K, Otsuji A, Nakamura Y, Nagao J, et al. Outcome of 141 cases of self-expandable metallic stent placements for malignant and benign colorectal strictures in a single center. Surg Endosc. 2011;25:1748–52.
Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2012;26:110–9.
Matsuda A, Miyashita M, Matsumoto S, Matsutani T, Sakurazawa N, Takahashi G, et al. Comparison of long-term outcomes of colonic stent as “bridge to surgery” and emergency surgery for malignant large-bowel obstruction: a meta-analysis. Ann Surg Oncol. 2015;22:497–504.
Stipa F, Pigazzi A, Bascone B, Cimitan A, Villotti G, Burza A, et al. Management of obstructive colorectal cancer with endoscopic stenting followed by single-stage surgery: open or laparoscopic resection? Surg Endosc. 2008;22:1477–81.
Cheung HY, Chung CC, Tsang WW, Wong JC, Yau KK, Li MK. Endolaparoscopic approach vs. conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg. 2009;144:1127–32.
Acknowledgments
Assistant Professor R.J. Turner of the Faculty of Medicine of Toho University, Tokyo, Japan edited this manuscript and formatted the references.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Toshiyuki Enomoto and his co-authors have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Enomoto, T., Saida, Y., Takabayashi, K. et al. Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. Surg Today 46, 1383–1386 (2016). https://doi.org/10.1007/s00595-016-1331-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1331-7