Abstract
Aim
We aimed to investigate the combined impact of liver enzymes and alcohol consumption on the diabetes risk.
Methods
Data on 5972 non-diabetic participants aged 30–79 years from the Suita study were analyzed. Diabetes incidence was surveyed every 2 years. Current daily alcohol consumption was defined as light drinking (< 23.0 g ethanol/day in men and < 11.5 g in women), moderate drinking (23.0–45.9 g and 11.5–22.9 g), and heavy drinking (≥ 46.0 g and ≥ 23.0 g). The nondrinkers category included both never-drinkers and former drinkers.
Results
During the median follow-up of 13 years, 597 incident diabetes cases were diagnosed. Higher levels of γ-glutamyltransferase (GGT), alanine aminotransferase (GPT), and aspartate aminotransferase (GOT) were associated with an increased diabetes risk, and current light drinkers had a lower risk of diabetes than nondrinkers. No sex differences were observed in these associations. Compared to nondrinkers having the lowest quartiles of liver enzymes, nondrinkers and current moderate/heavy drinkers having the highest quartiles had an increased risk of diabetes. However, no association was observed for current light drinkers having the highest quartiles of liver enzymes; the multivariable hazard ratios (95% CIs) in current light drinkers with the highest quartile of liver enzymes were 1.27 (0.68–2.37) for GGT, 1.05 (0.59–1.89) for GPT, and 0.76 (0.40–1.47) for GOT, respectively.
Conclusion
High liver enzymes were associated with an increased diabetes risk. No increased diabetes risk was observed in current light drinkers, even in these who had high levels of liver enzymes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High levels of liver enzymes such as γ-glutamyltransferase (GGT), alanine aminotransferase (GPT), and aspartate aminotransferase (GOT) are considered markers of liver dysfunction. These enzymes could indicate fat accumulation in the liver and are known to be elevated in those with insulin resistance [1,2,3]. Previous population-based studies have shown that these enzymes of liver function were associated with an increased risk of diabetes, independent of obesity and daily alcohol consumption [4,5,6,7,8,9]. The reported associations were evident even within normal ranges of liver enzymes. GPT represents the most specific marker of liver function because it is mainly observed in the liver, whereas GGT and GOT are less specific markers because they are also correlated to other conditions. Two meta-analyses of population-based studies showed that both GGT and GPT are independent predictors of diabetes [4, 5]. A Mendelian randomized study showed causal evidence for the association of GPT and GOT with the risk of diabetes [6].
Alcohol consumption has a dose-dependent impact on liver enzymes, and elevated GGT is the most typical biomarker of excess alcohol use [10]. In a meta-analysis of 20 cohort studies, light alcohol consumption was reported to have a protective role against incident diabetes [11]. The combined impact of liver enzymes and alcohol consumption on the risk of diabetes is rarely investigated, despite its potential utility for risk classification for primary prevention of diabetes among the general population.
In this study, we analyzed the data from the Suita study to investigate the combined impact of liver enzymes and alcohol consumption on the risk of diabetes. We hypothesized that liver enzymes are positively associated with the risk of diabetes, but that these associations would likely be altered by daily alcohol consumption.
Methods
Study population
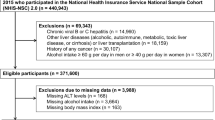
The Suita study is a population-based study of urban residents launched more than 30 years ago, in 1989 [12,13,14]. Residents aged 30–79 years were randomly selected from the municipality population registry and were stratified by sex and 10-year age groups, and ultimately, 8360 men and women underwent at least one health check-up in the National Cerebral and Cardiovascular Center. Participants were enrolled from the original cohort between 1989 and 1996, a secondary cohort between 1996 and 1998, and a volunteer group between 1992 and 2006. After excluding 2,388 participants who had histories of cardiovascular diseases and diabetes, no follow-up data, or age greater than 79 years, 5972 participants were available for this analysis. Informed consent was obtained from all study participants, and the institutional review board approved this study of the National Cerebral and Cardiovascular Center (R21024).
Follow-up and ascertainment of cases
Participants were followed up to (1) the date of first diagnosis with diabetes; (2) the date of the last health examination and medical records; or (3) December 31, 2015 (date of censorship). The median follow-up was 12.6 years with an interquartile range of 5.9–19.2 years. Participants were invited to have a health check-up every 2 years. Diabetes was defined as a fasting blood glucose level ≥ 126 mg/dL, non-fasting blood glucose level ≥ 200 mg/dL, or the use of diabetes medication.
Measurement of liver enzymes and covariates
Blood tests, including liver enzymes, total cholesterol, high-density lipoprotein cholesterol, and blood glucose, were performed as part of the regular health check-up. After at least 5 min of rest, blood pressure was measured in a seated position using a mercury sphygmomanometer and a suitable-sized cuff according to the standard protocol. Body mass index was calculated as weight (kg) divided by height in meters squared (m2). Details regarding lifestyles such as smoking, drinking (status and daily alcohol consumption in current drinkers), and medications use were obtained using a standard-format interview. Participants were grouped by drinking status, first as never-drinkers, former drinkers, and current drinkers; then the category “nondrinkers” was created to encompass both never-drinkers and former drinkers whereas the “current drinkers” group members were further defined by daily alcohol consumption as light drinkers (< 23 g ethanol/day in men and < 11.5 g in women), moderate drinkers (23–45.9 g and 11.5–22.9 g), and heavy drinkers (≥ 46 g and ≥ 23 g). Impaired glucose tolerance was defined as fasting plasma glucose levels of 100–125 mg/dL or non-fasting glucose levels of 140–199 mg/dL. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease equation modified by the Japanese coefficient:
eGFR = 0.881 × 186 × age−0.203 × serum creatinine −1.154 × 0.742 (for women) [15].
Statistical analysis
Analysis of variance was used to compare mean values, and chi-square test was used to compare proportions of baseline characteristics. Cox proportional hazard regression model was used to calculate hazard ratio with 95% confidence interval (CI) according to quartile of liver enzymes or drinking status. Potential confounding factors included age (years), body mass index groups (< 18.5, 18.5–24.9, or ≥ 25.0 kg/m2), systolic blood pressure (mmHg), antihypertensive medication use (no or yes), total cholesterol (mg/dL), high-density lipoprotein cholesterol (mg/dL), antihyperlipidemic medication use (no or yes), eGFR (mL/min/1.73 m2), impaired glucose tolerance (no or yes), exercise habits (no or yes), current smoking (no or yes), drinking status (nondrinkers, light drinkers, moderate drinkers, and heavy drinkers) or alcohol consumption (g/day), and other liver enzymes (U/L). We also calculated the hazard ratio with 95% CI according to 1 SD increment of liver enzymes and clinical threshold, which was defined as more than 50 U/L for men and 30 U/L for women for γ-GTP, and more than 40 U/L for GPT and GOT. P for interaction was calculated by a cross-product term that sex (dichotomous) was multiplied by liver enzymes levels or drinking status (categories). All analyses were performed with SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC, USA).
Results
Baseline characteristics of participants are shown in Table 1. There were 5972 participants, of whom 2735 (45.8%) were men; their mean age was 54.3 years with a standard deviation of 12.4 years. On average, the participants who developed diabetes during follow-up were younger and had more likely to be men compared to that who did not. Also, the participants with diabetes had higher levels of liver enzymes, blood pressure levels, and body mass index, a higher proportion of impaired glucose tolerance, current smokers, moderate and heavy drinkers, and lower levels of serum HDL cholesterol compared to those who did not develop diabetes.
During the 76,793 person-years of follow-up, a total of 597 diabetes cases were diagnosed. The incidence rate of diabetes was 7.8 per 1000 person-years. Hazard ratios (95% CIs) for incident diabetes according to liver enzymes or drinking status are shown in Table 2. Liver enzyme levels were positively associated with the age-adjusted risk of diabetes. After controlling for traditional risk factors, the association remained statistically significant: the multivariable hazard ratios (95% CIs) of the highest versus lowest quartile were 1.98 (1.44–2.72) for GGT, 2.02 (1.48–2.74) for GPT, and 1.47 (1.12–1.95) for GOT. No sex difference was observed; P for sex–interactions were 0.20 for GGT, 0.55 for GPT, and 0.34 for GOT. The corresponding hazard ratios (95% CIs) of 1 SD increment were 1.11 (1.03–1.19), 1.15 (1.03–1.29), and 0.95 (0.83–1.08), respectively. The association between daily alcohol consumption and diabetes took the form of a U-shaped curve; the multivariable hazard ratios (95% CIs) were 0.61 (0.43–0.86) for light drinkers, 0.80 (0.63–1.03) for moderate drinkers, and 0.97 (0.68–1.39) for heavy drinkers compared to nondrinkers, with nonsignificant sex–interactions (P = 0.58).
Multivariable hazard ratios and 95% confidence intervals for incident diabetes according to cross groups between liver enzymes and daily alcohol consumption are shown in Table 3. Compared to nondrinkers with the lowest quartiles of liver enzymes, nondrinkers and current moderate/heavy drinkers with the highest quartiles had increased risk of diabetes. However, current light drinkers with the highest quartiles of liver enzymes had no significant risk of diabetes; the corresponding multivariable hazard ratio (95% CI) was 1.27 (0.68–2.37) for GGT, 1.05 (0.59–1.89) for GPT, and 0.76 (0.40–1.47) for GOT.
Discussion
In this study, we observed a positive association between liver enzymes and the risk of diabetes and a U-shaped association between daily alcohol consumption and the risk of diabetes. The associations between GGT and GPT and diabetes were evident in nondrinkers and moderate/heavy alcohol drinkers, but not in light drinkers.
In a meta-analysis of seven population-based studies, GGT and GPT were positively associated with the risk of diabetes; the pooled hazard ratios of the highest versus lowest quartile were 2.94 (95% CI, 1.98–3.88; I2 = 20% and P = 0.26) for GGT and 2.02 (95% CI, 1.59–2.58; I2 = 27% and P = 0.19) for GPT [4]. The association for GOT was not reported in that study. Another meta-analysis of 17 population-based studies showed a consistent result for GPT (pooled hazard ratio = 1.66; 95% CI, 1.31–2.09; I2 = 88% and P < 0.001). However, this result showed considerable heterogeneity, and no explanation could be found among the study characteristics. Besides, publication bias was reported [5]. These unexplained heterogeneities limited meta-analytic results. In this situation, a separate prospective study based on a local general population may provide better evidence for clinical practice guidelines. The pooled association for GOT was first investigated in a meta-analysis of nine population-based studies; the pooled hazard ratio of the highest versus lowest tertile was 1.03 (95% CI, 0.98–1.09; I2 = 65% and P = 0.003), with a similar high heterogeneity [5]. That study of population-based studies of GOT associations was expanded from 9 to 13 in a subsequent meta-analysis performed by the same research team; the revised pooled hazard ratio of the highest versus lowest tertile was 1.09 (95% CI, 1.03–1.14; I2 = 73% and P < 0.001), whereas the statistical significance disappeared in the six studies that GGT and GPT were adjusted [7].
A bidirectional Mendelian randomization study showed associations of GPT and GOT with an increased risk of diabetes; the odds ratios (95% CIs) were 1.45 (1.10–1.92) for GPT, 1.25 (1.14–1.38) for GOT. Fasting insulin, but not diabetes, was associated with increased GPT. However, unlike previous observational studies, weak causal evidence was observed for GGT (odds ratio = 0.92; 95% CI, 0.80–1.06) [6], which was consistent with another Mendelian randomization study (odds ratio = 1.01; 95% CI, 0.99–1.02) [8].
Several mechanisms have been proposed to explain the apparent association between serum liver enzymes and incident diabetes. It is well-known that increased liver enzymes, especially GPT, reflect liver fat accumulation, which contributes to pathophysiological changes that are relevant to the development of diabetes [16, 17]. Besides, GPT is considered a marker of both insulin resistance and atherosclerotic vascular disease [18]. GGT is an enzyme responsible for the extracellular catabolism of antioxidant glutathione and its high value reflects oxidative stress [19]. Data from 3,086 women without diabetes, GPT, and GGT were positively associated with fasting glucose, fasting insulin, and HbA1c. These correlations were not substantially changed after excluding hyperinsulinemic women, and similar findings were observed in both obese and non-obese non-diabetic women [2]. Data from 1309 non-diabetic participants showed that GGT and GPT were inversely associated with insulin sensitivity, and GGT and GPT were positively associated with higher insulin secretion rates and reduced endogenous clearance of insulin and liver insulin extraction during the oral glucose tolerance test in both sexes [3]. Given that GGT is a non-specific marker and is correlated to many conditions, it could more reflect the potential intermediary related to diabetes pathogenesis. GOT was shown to reflect fat accumulation although the association was much weaker than that for GPT [20].
Increased liver enzymes are observed in current drinkers. GGT, in particular, is a classical biomarker of daily alcohol consumption. However, a meta-analysis of 20 population-based studies showed the protective role of moderate alcohol consumption against the risk of diabetes in both sexes [11]. The reduced diabetic risk could be explained by improved insulin sensitivity with moderate alcohol consumption [21, 22]. Data from 8576 non-diabetic male employees aged 40–55 years showed that both nondrinkers and heavy drinkers with the highest tertiles of liver enzymes had higher risks of diabetes than moderate drinkers with the lowest tertiles after a 4-year follow-up [9]. These findings were similar to ours here, with some exceptions. That study found an inverse linear association between daily alcohol consumption and diabetes; the multivariable odds ratio (95% CI) was 0.93 (0.71–1.22) for light drinkers, 0.69 (0.53–0.89) for moderate drinkers, and 0.71 (0.54–0.93) for heavy drinkers, compared to nondrinkers. The almost liner association was inconsistent with the U-shaped findings both in a previous meta-analysis [11], and in the present study. The difference could be due to the different population characteristics. Our study consisted of both sexes and enrolled participants from the general population so that our findings in turn could be extrapolated to the general population.
The strength of our study was the cohort design and cohort quality control. Cohort members were randomly enrolled from the population registry with stratified sex and age groups so that the possibility of selection bias should be small. However, the study also had several limitations. First, we could not classify the types of diabetes because we did not have sufficient diagnosis basis. However, the incidence of type 1 diabetes in Japan is very low [23], and most participants in our study were older than 40 years, so the cases of type 1 diabetes might be small. Second, we could not rule out the possibility of recall bias in drinking status because it was surveyed by a standard-form interview. However, we have a team of well-trained nurses and staff to perform the interview. Third, physical activity was not fully investigated. We controlled for the impact of physical activity by exercise habits only, not by exercise and/or type of daily work. Finally, residual confounding cannot be excluded because of the observational study design.
In conclusion, higher levels of liver enzymes were associated with an increased risk of diabetes in the general population. An excessive diabetic risk was observed in nondrinkers and current moderate/heavy alcohol drinkers with high levels of liver enzymes, whereas no increased diabetic risk was observed in current light drinkers, even in these with high levels of liver enzymes. The findings of our study highlight the impact of daily alcohol consumption on the association of liver enzymes with diabetic risk, and provide evidence for clinical guidance on how best to classify individuals’ diabetes risk when they have high levels of liver enzymes.
Availability of data and materials
Research data are not publicly available on legal or ethical grounds.
References
Vozarova B, Stefan N, Lindsay RS et al (2002) High alanine aminotransferase is associated with decreased liver insulin sensitivity and predicts the development of type 2 diabetes. Diabetes 51:1889–1895
Fraser A, Ebrahim S, Smith GD, Lawlor DA (2007) A comparison of associations of alanine aminotransferase and gamma-glutamyltransferase with fasting glucose, fasting insulin, and glycated hemoglobin in women with and without diabetes. Hepatology 46:158–165
Bonnet F, Ducluzeau PH, Gastaldelli A et al (2011) RISC Study Group Liver enzymes are associated with liver insulin resistance, insulin secretion, and glucagon concentration in healthy men and women. Diabetes 60:1660–1667
Fraser A, Harris R, Sattar N, Ebrahim S, Davey Smith G, Lawlor DA (2009) Alanine aminotransferase, gamma-glutamyltransferase, and incident diabetes: the British Women’s Heart and Health Study and meta-analysis. Diabetes Care 32:741–750
Kunutsor SK, Apekey TA, Walley J (2013) Liver aminotransferases and risk of incident type 2 diabetes: a systematic review and meta-analysis. Am J Epidemiol 178:159–171
De Silva NMG, Borges MC, Hingorani AD et al (2019) Liver function and risk of type 2 diabetes: bidirectional Mendelian randomization study. Diabetes 68:1681–1691
Kunutsor SK, Abbasi A, Apekey TA (2014) Aspartate aminotransferase: Risk marker for type-2 diabetes mellitus or red herring? Front Endocrinol 5:189
Lee YS, Cho Y, Burgess S et al (2016) Serum gamma-glutamyl transferase and risk of type 2 diabetes in the general Korean population: a Mendelian randomization study. Hum Mol Genet 25:3877–3886
Sato KK, Hayashi T, Nakamura Y et al (2008) Liver enzymes compared with alcohol consumption in predicting the risk of type 2 diabetes: the Kansai Healthcare Study. Diabetes Care 31:1230–1236
Agarwal S, Fulgoni VL III, Lieberman HR (2016) Assessing alcohol intake & its dose-dependent effects on liver enzymes by 24-h recall and questionnaire using NHANES 2001–2010 data. Nutr J 15:62
Baliunas DO, Taylor BJ, Irving H et al (2009) Alcohol as a risk factor for type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 32:2123–2132
Kokubo Y, Okamura T, Watanabe M et al (2010) The combined impact of blood pressure category and glucose abnormality on the incidence of cardiovascular diseases in a japanese urban cohort: the Suita study. Hypertens Res 33:1238–1243
Kokubo Y, Watanabe M, Higashiyama A, Nakao YM, Nakamura F, Miyamoto Y (2018) Impact of intima-media thickness progression in the common carotid arteries on the risk of incident cardiovascular disease in the Suita study. J Am Heart Assoc 7:e007720
Li J, Kokubo Y, Arafa A, et al (2021) Mild hypertensive retinopathy and risk of cardiovascular disease: the Suita study. J Atheroscler Thromb. Epub ahead of print
Imai E, Horio M, Nitta K et al (2007) Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin Exp Nephrol 11:41–50
Marchesini G, Brizi M, Bianchi G et al (2001) Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 50:1844–1850
Westerbacka J, Cornér A, Tiikkainen M et al (2004) Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia 47:1360–1369
Ceriello A, Motz E (2004) Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol 24:816–823
Turgut O, Yilmaz A, Yalta K, Karadas F, Birhan YM (2006) Gamma-glutamyltransferase is a promising biomarker for cardiovascular risk. Med Hypotheses 67:1060–1064
Kim CH, Park JY, Lee KU, Kim JH, Kim HK (2009) Association of serum gamma-glutamyltransferase and alanine aminotransferase activities with risk of type 2 diabetes mellitus independent of fatty liver. Diabetes Metab Res Rev 25:64–69
Mayer EJ, Newman B, Quesenberry CP Jr, Friedman GD, Selby JV (1993) Alcohol consumption and insulin concentrations: role of insulin in associations of alcohol intake with high-density lipoprotein cholesterol and triglycerides. Circulation 88:2190–2197
Facchini F, Chen YD, Reaven GM (1994) Light-to-moderate alcohol intake is associated with enhanced insulin sensitivity. Diabetes Care 17:115–119
Kawasaki E, Matsuura N, Eguchi K (2006) Type 1 diabetes in Japan. Diabetologia 49:828–836
Acknowledgements
We would like to express our deepest gratitude to Drs. Kawanishi and Misaki, the former and current presidents of the Suita Medical Association, respectively, and to all the Suita City Health Center members and staff of Preventive Cardiology and Preventive Healthcare Departments for performing medical examinations and follow-ups. We also would like to express our special gratitude to Professor Hiroyasu Iso from Osaka University and all cohort members.
Funding
This study was supported by the Intramural Research Fund (20-4-9) for cardiovascular diseases of the National Cerebral and Cardiovascular Center, JST Grant Number JPMJPF2018, and by Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare of Japan (20FA1002). This study was also supported by the Meiji Yasuda Research Institute, Inc. and Meiji Yasuda Life Insurance Company.
Author information
Authors and Affiliations
Contributions
JL and YK contributed to initial concept; YK provided resources; YK acquired funding; JL and YK contributed to literature review; JL contributed to draft writing; JL analyzed the data; YK contributed to supervision; all authors contributed to critical revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Consent for publication
Informed consent was obtained from all study participants.
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of the National Cerebral and Cardiovascular Center, Osaka, Japan (R21024). The study was conducted per the Declaration of Helsinki. Written informed consent was obtained from all participants for their anonymized information in the Suita study.
Additional information
Managed By Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, J., Arafa, A., Kashima, R. et al. Liver enzymes, alcohol consumption and the risk of diabetes: the Suita study. Acta Diabetol 59, 1531–1537 (2022). https://doi.org/10.1007/s00592-022-01949-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-022-01949-1