Abstract
In the last ten years, knowledge on pathophysiology of type 2 diabetes (T2DM) has significantly increased, with multiple failures (decreased incretin effect, increased lipolysis, increased glucagon secretion, neurotransmitters dysfunction) recognized as important contributors, together with decreased insulin secretion and reduced peripheral glucose uptake. As a consequence, the pharmacologic therapy of T2DM has been progressively enriched by several novel classes of drugs, trying to overcome these defects. The last, intriguing compounds come into the market are SGLT2 inhibitors, framing the kidney in a different scenario, not as site of a harmful disease complication, but rather as the means to correct hyperglycemia and fight the disease. This review aims to offer a short, updated overview of the role of these compounds in the treatment of T2DM, focusing on efficacy, ancillary albeit relevant clinical effects, safety, potential cardiovascular protection, positioning in common therapeutic algorithms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mechanism of action
In the presence of normal glucose concentrations, glomeruli of a healthy individual filter approximately 180 g glucose per day, almost entirely reabsorbed through the proximal tubule into the bloodstream. In this condition, therefore, glycosuria is virtually zero. In face of a normal renal function, approximately 90 % of the tubular load of glucose is reabsorbed by an active mechanism mediated by the SGLT2 plasma membrane cotransporter [1], characterized by a low affinity, high capacity for glucose, almost exclusively localized in the early portion (S1 and S2 segments) of renal tubule, and reabsorbing glucose/Na in a 2:1 ratio. Glucose skipping this process (about 10 %) is reabsorbed more distally, by the SGLT1 transporter (Fig. 1), with high affinity and low capacity, much more represented in the gut, where it is the main responsible for glucose and galactose absorption [2].
Once into the tubular cell, glucose is passively released at the level of basolateral membrane with a mechanism of facilitated transport requiring GLUT2, going back into the bloodstream. The activity of these two transporters is fully independent upon insulin action.
When plasma glucose concentration raises and sustained hyperglycemia occurs, tubular reabsorption increases accordingly, till its maximum capacity (approximately 350 mg/min/1.73 m2, corresponding to glucose values of 180–200 mg/dl) is reached, and overcome, with the exceeding glucose passing into urine. In the realty, there is not a precise point beyond which that happens, and the so-called splay represents urinary glucose excretion that is evident before Tmax is reached. This can be explained considering that a certain number of nephrons may release glucose even at a lower level, others at a higher level, as well as by the relatively low affinity of the transporters [3]. This concept is recalled in Fig. 2.
In several animal models of diabetes, there is a strict correlation between glucose levels and renal SGLT2 expression that can be down-regulated by an insulin infusion [4, 5]; however, data in humans are scanty. The most convincing evidence is, perhaps, that reporting an increased expression and activity of this transporter in tubular cells collected from urines of a few T2DM patients vs controls [6].
Theoretically, what would you expect blocking these transporters? You would expect that, of the filtered glucose, very low or nothing is reabsorbed and a vast majority is excreted. Therefore, modulation of renal glucose reabsorption is a precise therapeutic target: by a SGLT2 inhibition, we may induce a relevant glycosuria, able to reduce the glucotoxicity that marks T2DM patients and represents an important determinant of organ damage [7].
The precursor of the modern SGLT2 inhibitors was phlorizin, derived from the apple tree root [8]; more than 20 years ago, Rossetti et al. [9] brilliantly demonstrated as partially pancreasectomised rats receiving phlorizin showed a strong improvement of glucose levels and insulin resistance. However, the experimental work on this compound was then abandoned due to the scarce bioavailability after oral administration, the relevant gastrointestinal side effects and the putative interference with brain transporters. Clinical research in this field has proceeded, and today we have the availability of several selective SGLT2 inhibitors. The full clinical meaning, implications and consequences of such extreme selectivity, even configuring an undoubted advantage in terms of efficacy and safety, is far from being fully understood and requires investigation.
Pharmacokinetic and pharmacodynamic
The three main SGLT2 inhibitors in terms of available preclinical and clinical studies are, in order of selectivity, empagliflozin, dapagliflozin and canagliflozin, whose pharmacokinetic is comparable [10]. The minimal dapagliflozin dose able to induce urinary glucose excretion in healthy individuals is 0.3 mg, but the daily amount of glycosuria is variable, ranging between 18 and 62 g [11]. In T2DM, the pharmacokinetic does not significantly differ from controls: fast absorption, t max of about 1.5–2 h and t 1/2 of 16–18 h, with a steady state reached after 4 days of treatment [12]. However, in T2DM individuals, at therapeutic doses, SGLT2 inhibitors induce a higher glucose excretion (about 80 g/day), likely due to the increased tubular load of these patients [13, 14]. It has been calculated that such excretion approximately corresponds to an inhibition of 36 % in T2DM and of 20–30 % in healthy volunteers; with repeated doses, the mean inhibition raises up to 40–45 % in T2DM and 15–50 % in non-diabetic individuals, again unveiling an ample individual variability [15]. In simple words, despite the current hypothesis of an increased presence and activity of these transporters in T2DM [6], differences between glycosuria obtained in healthy subjects after a series of single, increasing SGLT2 inhibitor doses only slightly differ from those observed in T2DM patients after repeated doses, and this is confirmed by clinical trials. Several hypotheses have been formulated to explain this phenomenon: we might hypothesize that the amount of glucose reaching renal tubule is too much for the number of transporters, or that other non-SGLT2 transporters might be present, or that transporters cannot be adequately reached by the inhibitor for anatomic reasons. Other possibilities are the presence of a strong protein link, with only a small free fraction of the inhibitor, or, in the presence of a SGLT2 inhibition, the occurrence of an increased expression and activity of SGLT1 transporters. Again, drug might be secreted in a more distal site, or a higher SGLT2 expression at the tubular level in humans (respect to that expected on the basis of animal data) is conceivable, making not sufficient the doses of the inhibitors. Lastly, the inhibitor might be excessively reabsorbed proximally, or many of these mechanisms might coexist [16]. Alternatively, an easier and more direct explanation can be drawn comparing the dynamicity of the nephron, where pre-urine flows through the tubule, and the phenomenon of trans-capillary filtration of solutes: in an in silico model of rat nephron challenged with a 95 % inhibition of SGLT2, the prediction is that, in a normoglycemic state, only 40 % of filtered glucose will appear in urines [17].
An intriguing pharmacokinetic characteristic is an effect of “desincronization” between plasma levels of the drug and its glycosuric effect; in other words, a remarkable glucose excretion persists along the time despite reduced plasma drug levels. If we assume that SGLT2 inhibitors would be actively secreted (beside filtered) in the proximal renal tubule, it is clear that high drug concentrations may reach the segment where SGLT2 transporters are, therefore contributing to maintain the effect, especially when plasma levels decline [16].
Race does not seem to significantly affect pharmacologic profile of these compounds, except for a greater oral absorption rate in Asian patients [18, 19]; interactions with other drugs commonly used in diabetic patients (statins, warfarin, digoxin) are not reported [20, 21].
Clinical efficacy
Effect on glucose control
SGLT2 inhibitors are effective when used in monotherapy or in initial combination with other agents, or as add-on to already ongoing therapies. For each one of the three agents, there is availability of several studies showing their efficacy in improving metabolic control of the patients. Mean HbA1c reduction was −0.8 % (−9 mmol/mol) [22], even higher when baseline HbA1c values are above 9 % (75 mmol/mol). Significantly higher, respect to placebo, is also the percentage of patients reaching the therapeutic goal: for example, 24 weeks of monotherapy with dapagliflozin 10 mg led to 51 % of patients achieving HbA1c <7.0 % (53 mmol/mol) versus 32 % of those in the placebo group [23]. After 26 weeks of treatment with canagliflozin, 44.5 and 62.4 % of subjects receiving 100 mg and 300 mg, respectively, achieved HbA1c <7.0 % versus 20.6 % of those on placebo [24]. Similar performances are reported when compared with active treatments: for example, empagliflozin monotherapy given for 24 weeks led to HbA1c <7.0 % in 35.3 and 43.6 % of subjects receiving 10 and 25 mg, respectively, versus 37.5 % for the active comparator group (sitagliptin 100 mg), and 12.0 % in the placebo group [25]. SGLT2 inhibition is effective in reducing HbA1c even in combination with insulin, stabilizing insulin dosing and reducing weight without increasing the number of major hypoglycemic episodes [26, 27].
T2DM is a chronic disease with an inevitable progressive course; this implies frequent, necessary therapeutic variations and/or dose adjustments, to maintain the ideal glycemic target for the patient. In this view, availability of drugs able to guarantee a certain durability of their clinical efficacy along the time is of crucial importance. The SGLT2 inhibitors seem to have this capability: in pre-registrative studies, a stability of HbA1c until 2 years has been demonstrated [26, 28, 29]; post-marketing trials are confirming these results at 4 years [30].
It is interesting to point out as using SGLT2 inhibitors even before the clinical onset of diabetes has been hypothesized, given their efficacy in improving β cell function (largely due to reduced glucose toxicity) and insulin sensitivity (obtained by preventing a further deterioration of glucose tolerance) [31–33].
Effect on body weight
Treatment of obesity, a frequent comorbidity of T2DM, is a difficult and demanding task, and different therapeutic strategies (hypocaloric diets, promotion of physical activity, behavioral therapy, pharmacologic intervention) have a limited efficacy. SGLT2 inhibitors, either alone and as add-on to metformin, induce a relevant and stable weight loss [34, 35]; such effect is maximized in patients treated already with drugs usually inducing weight gain, like sulphonylureas or pioglitazone [36, 37]; conversely, weight loss favorably influences glucose and blood pressure control [38]. As by a recent metanalysis including ten trials with 6701 participants [39], canagliflozin led to greater body weight loss (−2.81 kg vs. placebo). Similarly to glucose control, body weight seems to remain relatively stable along the time [29].
A smart approach in preventing an undesired weight gain is combining SGLT2 inhibitors with insulin, especially when patients are overweight or obese: in such studies, a sustained weight loss has been obtained, together with a reduction in daily insulin requirement [40].
Weight loss induced by SGLT2 inhibitors is mainly due to a reduction in subcutaneous and visceral fat mass [41]; an adjunctive role in determining weight loss and maintaining it stable can be played by a diuretic effect exerted by these compounds. However, as recently and elegantly shown by Ferrannini et al. [42], when accounting for glycosuria but assuming no changes in energy intake, the model-predicted weight loss would be much larger than usually reported, with observed and predicted weight loss diverging approximately at 24 weeks. The authors conclude that energy intake must have increased to explain the attenuation of weight loss.
Effect on arterial blood pressure
SGLT2 inhibitors constantly induce a reduction in either systolic (SBP) or diastolic blood pressure (DBP) [43, 44], marginally due to weight loss and rather to an increased sodium excretion (even though sodium can be reabsorbed in the distal nephron by other channels) [45], and to the osmotic diuresis that follows glucose excretion. Even small, this sodium/volume loss leads to a stimulation of the renin–angiotensin–aldosterone system, thus triggering a counter-regulatory compensatory mechanism to maintain sodium homeostasis [45].
Which is the entity of the antihypertensive effect? Pooled analyses of data obtained with dapagliflozin show changes from baseline in SBP and DBP of −3.6 and −1.2 mm Hg, respectively, in hypertensive patients and −2.6 and −1.2 mmHg, respectively, in non-hypertensive patients [44]; similar reductions, confirmed by ambulatory blood pressure monitoring, were obtained with empagliflozin and canagliflozin [46, 47]. An ample metanalysis (twenty-seven randomized clinical trials, almost 13,000 participants) has shown a mean SBP reduction −4.0 mmHg vs baseline, and −1.6 mmHg for DBP [48].
Other metabolic effects
SGLT2 inhibitors administration results in a small increase in both LDL and HDL cholesterol [49, 50]; the mechanism responsible for this undesired (for LDL cholesterol), albeit clinically trivial effect, is still unclear. Recently, an opposite effect according to the baseline LDL levels (reduction when starting LDL cholesterol levels are >120 mg/dl, increase in those with baseline <120 mg/dl) has been reported with canagliflozin [51].
Another beneficial outcome of a prolonged treatment with SGLT2 inhibitors is a reduction in uric acid levels (mean of −40/50 μmol/l); such effect might assume relevance in light of a recent metanalysis suggesting an increased risk of CV mortality linked to hyperuricemia [52], even though the causal relationship between uric acid levels and CV risk needs further confirmation. The hypothesized mechanism is a glycosuria-dependent enhanced uric acid secretion at the proximal tubule and inhibition of uric acid uptake via GLUT9 isoform 2 at the level of the collecting duct [53].
Side effects and safety
This class of anti-hyperglycemic compounds is well tolerated. A point of strength in their favor is the very low risk to induce hypoglycemia, with a slightly higher frequency of hypoglycemic episodes only when they are used as add-on to SU [54].
The most common side effects occurring during long-term treatment with SGLT2 inhibitors concern the genito-urinary apparatus; however, recent meta-analyses deny an increased risk of urinary tract infections vs placebo or active comparators, confirming the increased incidence of genital mycotic infections, mainly in the female sex [55, 56]. The incidence of such infections seems also to vary with the ethnicity.
Another potential undesired effect is linked to the osmotic diuresis induced by these compounds, that might promote a reduction in intravascular volume (−8 to 12 %, like with thiazide diuretics), and a small rise in hematocrit value, back to normal (likely through compensatory mechanisms) during a prolonged SGLT2 inhibition [57]. Orthostatic hypotension rarely occurs; nevertheless, caution in using these compounds in elderly people at high risk of dehydration is advisable, and patients particularly sensitive to volume changes should be monitored for signs and symptoms of dehydration and electrolyte abnormalities when SGLT2 inhibitors are combined with diuretics.
Recently, cases of euglycemic ketoacidosis have been reported in patients treated with SGLT2 inhibitors; a detailed analysis of these cases, mainly occurred in canagliflozin registration studies, has pointed out as many of these patients were type 1 or insulin-treated T2DM with high alcohol consumption, in which insulin dosage had been inadequately reduced, or with a background diuretic therapy that might have magnified the risk of dehydration; there were also cases of latent autoimmune diabetes of adulthood. In this view, physicians and patients should be aware as such risk may increase in long-standing T2DM patients with severe β-cell failure, or during prolonged starvation, or concomitant acute illness, or after surgery procedures [58].
An increased cotransport of phosphate and sodium is intrinsically linked to SGLT2 inhibition; this might slightly increase serum phosphate and PTH levels, thereby favoring bone resorption [59]. PTH can also increase the secretion of FGF23 by osteocytes that has been associated with bone disease [60]. Increased levels of biochemical markers of bone resorption and formation, and a small reduction in mineral bone density, together with an increased risk of bone fractures, have been reported with canagliflozin [59, 61]; further studies are needed to point out whether such a detrimental effect should be considered a drug class effect or it is compound specific.
Overall, prolonged treatment with SGLT2 inhibitors is associated with a high health-related quality of life and a great treatment satisfaction [62].
The relationship between SGLT2 inhibitors and cancer risk remains inconclusive but warrants continued surveillance, particularly as the number of treated patients and duration of exposure increases. Updated data from trials performed with SGLT2 inhibitors show no overall imbalance of malignancies; however, some neoplasms were more common in dapagliflozin-treated individuals, like bladder and breast cancer [63], even though such imbalance might be the consequence of increased detection of preexisting cancer for the former, and a better detection following weight loss for the latter.
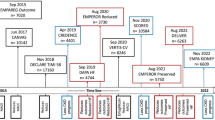
Cardiovascular safety
Pre-registrative and post-marketing data support a safe cardiovascular (CV) risk profile of SGLT2 inhibitors [64]; regarding the relationship between use of SGLT2 inhibitors and occurrence of major CV events, international regulatory authorities require post-marketing studies specifically addressing the non-inferiority of these novel anti-hyperglycemic drugs, respect to those in use since a longer time, in terms of long-term CV safety and potential beneficial effects on microvascular and macrovascular outcomes. Several trials are ongoing, but the EMPA-REG OUTCOME Study, performed with empagliflozin, has been concluded already, with the recent publication of its striking results [65]. Briefly, 7020 T2DM patients with previous personal history of CV disease (myocardial infarction, stroke or peripheral arterial disease) were randomized to either 10 mg empagliflozin, 25 mg empagliflozin, or placebo, assessing the occurrence of the primary (death from CV causes, non-fatal myocardial infarction and non-fatal stroke) and secondary endpoint (hospitalization for unstable angina in addition to the composite primary endpoint) along a median observation time of 3.1 years. A significant reduction in the primary endpoint (10.5 vs. 12.1 %) was observed in the empagliflozin group vs the placebo group, with a relative risk reduction (RRR) of 14 % (P = 0.04). Similarly, a RRR was noted in death from CV causes (RRR 38 %), hospitalization for heart failure (RRR 35 %) and all-cause death (RRR 32 %). The study has also confirmed the safety of empagliflozin, with no increase in bone fractures or cancer risk.
The EMPA-REG OUTCOME is a successful clinical study able to open novel scenarios but also leaving open and unsolved several questions, mainly regarding the mechanism(s) underlying such impressive CV benefit, and the question whether that is a class effect or should be regarded as exclusive of empagliflozin. Regarding the first point, several candidates might play a role: some of them are reported in Table 1. On the second point, the DECLARE-TIMI58 trial (ClinicalTrials.gov Identifier: NCT01730534), with dapagliflozin, more likely focusing on patients in primary prevention) and the CANVAS trial (NCT01032629), with canagliflozin, running in high CV risk individuals, whose results will be available within a few years, will be hopefully able to confirm the efficacy of SGLT2 inhibitors as a class of anti-hyperglycemic agents able to reduce residual risk of T2DM patients irrespective of glucose-lowering action.
SGLT2 inhibitors and the kidney: an intriguing relationship
The glycosuric efficacy of SGLT2 inhibitors has two main determinants: plasma glucose levels and glomerular filtration rate (GFR); as elegantly shown [66], at baseline, absorbed glucose linearly depends upon filtered glucose, and glycosuria occurs when glucose filtration rate is approximately 225–250 mg/min. After SGLT2 inhibition, we observe a reduced absorption and an increased excretion and that is true for the whole range of glomerular filtration. Both absorption and excretion increase in a parallel and linear fashion according to the increased GFR, without any clear evidence of a glycosuria threshold. Indeed, glycosuria increases as a function of GFR and glucose levels, and its amount can be reasonably predicted in each individual. As a consequence, the amount of glycosuria and the fractional glucose excretion is significantly lower in patients with GFR <60 ml/min/1.73 m2, even in the presence of a remarkable inter-individual variability. However, this does not seem to be the case for BP lowering effect, which is maintained and even magnified in people with CKD [67]; these patients encounter a beneficial effect on body weight too.
Apparently at odds with these clinical evidences are multiple recent reports of a nephroprotective effect of SGLT2 inhibitors [68]. SGLT2 administration seems to promote a recovery of glomerular hyperfiltration, a determinant of progressive renal disease in T2DM patients [69], likely through mechanisms of tubular–glomerular feedback [44]; data on albuminuria are less consistent [70].
Conclusive remarks
Based on the so far available data (clinical trial and post-marketing experience), SGLT2 inhibitors are effective in treating T2DM when used as either monotherapy or add-on to any other anti-hyperglycemic drug. Administered once daily, they are well tolerated and do not show relevant pharmacologic interactions. Their uniquely insulin-independent mechanism of action promotes a significant weight loss and a clinically relevant SBP reduction. Risk of hypoglycemia is low. For these reasons, such class of drugs is strongly recommended in treating obese and/or hypertensive T2DM individuals, pending a good renal function (if not, the drug would be simply less effective in correcting hyperglycemia) (Fig. 3). The more recent algorithm for treating T2DM, suggested last year by the American Diabetes Association and by the European Association for the Study of Diabetes, puts SGLT2 inhibitors after metformin, as any other therapeutic option, included insulin. Reinforcement of therapy is recommended anytime, despite 3 months of treatment with metformin at the maximal tolerated dosage, the ideal HbA1c target for the patient is not reached. SGLT2 inhibitors can be also considered as first-choice drugs in individuals who do not tolerate metformin, because, as GLP-1 analogues and DPP-IV inhibitors, they do not expose to the risk of hypoglycemia neither induce weight gain. As any other new drug, an adequate clinical experience on their long-term use is still lacking, mainly in terms of safety; the numerous post-marketing ongoing studies, as well as a growing clinical use, will contribute to enlarge the knowledge in this field.
To conclude, it should be pointed out as to combine a safe lifestyle with an adequate and constant adherence to therapy is of crucial importance to assure that the insertion of a novel drug in a whatever therapeutic scheme would be successful. The American Association of Diabetes Educators identifies seven critical behaviors in managing a T2DM patient: glycemic self- monitoring, physical activity, healthy diet, a quick facing and solving small daily problems of disease management, learning to manage stress and reducing risk factors [71]. Physicians, nurses and all sanitary personnel of diabetes world, together with patient’s family entourage, should play their own role to educate patients, informing them of benefits and risks of the therapy, sustaining them in difficult phases, encouraging them, all aiming at reaching and maintaining the expected metabolic control, reducing complications, ensure to these individuals a long and high-quality life.
References
Wright E, Loo D, Hirayama B (2011) Biology of human sodium glucose transporters. Physiol Rev 91:733–794
Dyer J, Daly K, Salmon KS et al (2007) Intestinal glucose sensing and regulation of intestinal glucose absorption. Biochem Soc Trans 35(Pt 5):1191–1194
Ferrannini E, Solini A (2012) SGLT2 inhibition in diabetes mellitus: rationale and clinical prospects. Nat Rev Endocrinol 8:495–502
Tabatabai NM, Sharma M, Blumenthal SS et al (2009) Enhanced expressions of sodium–glucose cotransporters in the kidneys of diabetic Zucker rats. Diabetes Res Clin Pract 83:e27–e30
Freitas HS, Anhe GF, Melo KF et al (2008) Na(+)-glucose transporter-2 messenger ribonucleic acid expression in kidney of diabetic rats correlates with glycemic levels: involvement of hepatocyte nuclear factor-1alpha expression and activity. Endocrinology 149:717–724
Rahmoune H, Thompson PW, Ward JM et al (2005) Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non-insulin-dependent diabetes. Diabetes 54:3427–3434
Campos C (2012) Chronic hyperglycemia and glucose toxicity: pathology and clinical sequelae. Postgrad Med 124:90–97
Ehrenkranz J, Lewis N, Kahn C et al (2005) Phlorizin: a review. Diabetes Metab Res Rev 21:31–38
Rossetti L, Smith D, Shulman GI et al (1987) Correction of hyperglycemia with phlorizin normalizes tissue sensitivity to insulin in diabetic rats. J Clin Invest 79:1510–1515
Scheen AJ (2014) Evaluating SGLT2 inhibitors for type 2 diabetes: pharmacokinetic and toxicological considerations. Expert Opin Drug Metab Toxicol 10:647–663
Komoroski B, Vachharajani N, Boulton D et al (2009) Dapagliflozin, a novel SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharmacol Ther 85:520–526
Devineni D, Curtin CR, Polidori D et al (2013) Pharmacokinetics and pharmacodynamics of canagliflozin, a sodium glucose co-transporter 2 inhibitor, in subjects with type 2 diabetes mellitus. J Clin Pharmacol 53:601–610
Heise T, Seewaldt-Becker E, Macha S et al (2013) Safety, tolerability, pharmacokinetics and pharmacodynamics following 4 weeks’ treatment with empagliflozin once daily in patients with type 2 diabetes. Diabetes Obes Metab 15:613–621
Kasichayanula S, Chang M, Hasegawa M et al (2011) Pharmacokinetics and pharmacodynamics of dapagliflozin, a novel selective inhibitor of sodium–glucose co-transporter type 2, in Japanese subjects without and with type 2 diabetes mellitus. Diabetes Obes Metab 13:357–365
List JF, Whaley JM (2011) Glucose dynamics and mechanistic implications of SGLT2 inhibitors in animals and humans. Kidney Int 120(Suppl):S20–27
Liu JJ, Lee T, DeFronzo RA (2012) Why do SGLT2 inhibitors inhibit only 30–50 % of renal glucose reabsorption in humans? Diabetes 61:2199–2204
Weinstein AM (2015) A mathematical model of the rat nephron: glucose transport. Am J Physiol Ren Physiol 308:F1098–F1118
Gavin JR 3rd, Davies MJ, Davies M et al (2015) The efficacy and safety of canagliflozin across racial groups in patients with type 2 diabetes mellitus. Curr Med Res Opin 31:1693–1702
Riggs MM, Staab A, Seman L et al (2013) Population pharmacokinetics of empagliflozin, a sodium glucose cotransporter 2 inhibitor, in patients with type 2 diabetes. J Clin Pharmacol 53:1028–1038
Macha S, Lang B, Pinnetti S et al (2014) Pharmacokinetics of empagliflozin, a sodium glucose cotransporter 2 inhibitor, and simvastatin following co-administration in healthy volunteers. Int J Clin Pharmacol Ther 52:973–980
Devineni D, Manitpisitkul P, Vaccaro N et al (2015) Effect of canagliflozin, a sodium glucose co-transporter 2 inhibitor, on the pharmacokinetics of oral contraceptives, warfarin, and digoxin in healthy participants. Int J Clin Pharmacol Ther 53:41–53
Berhan A, Barker A (2013) Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord 13:58
Ferrannini E, Ramos SJ, Salsali A et al (2010) Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care 33:2217–2224
Stenlof K, Cefalu WT, Kim KA et al (2013) Efficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetes Obes Metab 15:372–382
Roden M, Weng J, Eilbracht J et al (2013) Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol 1:208–219
Wilding JP, Woo V, Rohwedder K et al (2014) Dapagliflozin in patients with type 2 diabetes receiving high doses of insulin: efficacy and safety over 2 years. Diabetes Obes Metab 16:124–136
Ahmann A (2015) Combination therapy in type 2 diabetes mellitus: adding empagliflozin to basal insulin. Drugs Context 4:212288
Ridderstråle M, Andersen KR, Zeller C et al (2014) Comparison of empagliflozin and glimepiride as add-on to metformin in patients with type 2 diabetes: a 104-week randomised, active-controlled, double-blind, phase 3 trial. Lancet Diabetes Endocrinol 2:691–700
Leiter LA, Yoon KH, Arias P et al (2015) Canagliflozin provides durable glycemic improvements and body weight reduction over 104 weeks versus glimepiride in patients with type 2 diabetes on metformin: a randomized, double-blind, phase 3 study. Diabetes Care 38:355–364
Del Prato S, Nauck M, Durán-Garcia S et al (2015) Long-term glycaemic response and tolerability of dapagliflozin versus a sulphonylurea as add-on therapy to metformin in patients with type 2 diabetes: 4-year data. Diabetes Obes Metab 17:581–590
Merovci A, Mari A, Solis C et al (2015) Dapagliflozin lowers plasma glucose concentration and improves β-cell function. J Clin Endocrinol Metab 100:1927–1932
Polidori D, Mari A, Ferrannini E (2014) Canagliflozin, a sodium glucose co-transporter 2 inhibitor, improves model-based indices of beta cell function in patients with type 2 diabetes. Diabetologia 57:891–901
Merovci A, Solis-Herrera C, Daniele G et al (2014) Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest 124:509–514. Erratum in: J Clin Invest 2014;124:2287
Bailey CJ, Morales Villegas EC, Woo V et al (2015) Efficacy and safety of dapagliflozin monotherapy in people with type 2 diabetes: a randomized double-blind placebo-controlled 102-week trial. Diabet Med 32:531–541
Häring HU, Merker L, Seewaldt-Becker E et al (2014) Empagliflozin as add-on to metformin in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trial. Diabetes Care 37:1650–1659
Strojek K, Yoon KH, Hruba V et al (2014) Dapagliflozin added to glimepiride in patients with type 2 diabetes mellitus sustains glycemic control and weight loss over 48 weeks: a randomized, double-blind, parallel-group, placebo-controlled trial. Diabetes Ther 5:267–283
Kovacs CS, Seshiah V, Swallow R et al (2014) Empagliflozin improves glycaemic and weight control as add-on therapy to pioglitazone or pioglitazone plus metformin in patients with type 2 diabetes: a 24-week, randomized, placebo-controlled trial. Diabetes Obes Metab 16:147–158
Sjöström CD, Hashemi M, Sugg J et al (2015) Dapagliflozin-induced weight loss affects 24-week glycated haemoglobin and blood pressure levels. Diabetes Obes Metab 17:809–812
Yang XP, Lai D, Zhong XY et al (2014) Efficacy and safety of canagliflozin in subjects with type 2 diabetes: systematic review and meta-analysis. Eur J Clin Pharmacol 70:1149–1158
Rosenstock J, Jelaska A, Frappin G et al (2014) Improved glucose control with weight loss, lower insulin doses, and no increased hypoglycemia with empagliflozin added to titrated multiple daily injections of insulin in obese inadequately controlled type 2 diabetes. Diabetes Care 37:1815–1823
Bolinder J, Ljunggren Ö, Kullberg J et al (2012) Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab 97:1020–1031
Ferrannini G, Hach T, Crowe S et al (2015) Energy balance after sodium–glucose cotransporter 2 inhibition. Diabetes Care 38:1730–1735
Cefalu WT, Stenlöf K, Leiter LA et al (2015) Effects of canagliflozin on body weight and relationship to HbA1c and blood pressure changes in patients with type 2 diabetes. Diabetologia 58:1183–1187
Sjöström CD, Johansson P, Ptaszynska A et al (2015) Dapagliflozin lowers blood pressure in hypertensive and non-hypertensive patients with type 2 diabetes. Diab Vasc Dis Res 12:352–358
Cherney DZI, Perkins BA, Soleymanlou N et al (2014) Renal hemodynamic effect of sodium–glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 129:587–597
Tikkanen I, Narko K, Zeller C et al (2015) Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care 38:420–428
Townsend RR, Machin I, Ren J et al (2016) Reductions in mean 24-hour ambulatory blood pressure after 6-week treatment with canagliflozin in patients with type 2 diabetes mellitus and hypertension. J Clin Hypertens (Greenwich) 18:43–52
Baker WL, Smyth LR, Riche DM et al (2014) Effects of sodium–glucose co-transporter 2 inhibitors on blood pressure: a systematic review and meta-analysis. J Am Soc Hypertens 8(262–275):e9
Matthaei S, Bowering K, Rohwedder K et al (2015) Durability and tolerability of dapagliflozin over 52 weeks as add-on to metformin and sulphonylurea in type 2 diabetes. Diabetes Obes Metab 17:1075–1084
Stenlöf K, Cefalu WT, Kim KA et al (2014) Long-term efficacy and safety of canagliflozin monotherapy in patients with type 2 diabetes inadequately controlled with diet and exercise: findings from the 52-week CANTATA-M study. Curr Med Res Opin 30:163–175
Inagaki N, Goda M, Yokota S et al (2015) Effects of baseline blood pressure and low-density lipoprotein cholesterol on safety and efficacy of canagliflozin in Japanese patients with type 2 diabetes mellitus. Adv Ther 32:1085–1103
Zhao G, Huang L, Song M et al (2013) Baseline serum uric acid level as a predictor of cardiovascular disease related mortality and all-cause mortality: a meta-analysis of prospective studies. Atherosclerosis 23:61–68
Chino Y, Samukawa Y, Sakai S et al (2014) SGLT2 inhibitor lowers serum uric acid through alteration of uric acid transport activity in renal tubule by increased glycosuria. Biopharm Drug Dispos 35:391–404
Goring S, Hawkins N, Wygant G et al (2014) Dapagliflozin compared with other oral anti-diabetes treatments when added to metformin monotherapy: a systematic review and network meta-analysis. Diabetes Obes Metab 16:433–442
Liakos A, Karagiannis T, Athanasiadou E et al (2014) Efficacy and safety of empagliflozin for type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 16:984–993
Sinclair A, Bode B, Harris S et al (2014) Efficacy and safety of canagliflozin compared with placebo in older patients with type 2 diabetes mellitus: a pooled analysis of clinical studies. BMC Endocr Disord 14:37
Lambers Heerspink HJ, de Zeeuw D, Wie L et al (2013) Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab 15:853–862
Rosenstock J, Ferrannini E (2015) Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care 38:1638–1642
Taylor SI, Blau JE, Rother KI (2015) Possible adverse effects of SGLT2 inhibitors on bone. Lancet Diabetes Endocrinol 3:8–10
Quarles LD (2012) Skeletal secretion of FGF-23 regulates phosphate and vitamin D metabolism. Nat Rev Endocrinol 8:276–286
Watts NB, Bilezikian JP, Usiskin K et al (2016) Effects of canagliflozin on fracture risk in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 101:157–166
Grandy S, Sternhufvud C, Ryden A et al (2016) Patient-reported outcomes among type 2 diabetes mellitus patients treated with dapagliflozin in triple therapy regimen for 52 weeks. Diabetes Obes Metab 18:306–309
Lin HW, Tseng CH (2014) A review on the relationship between SGLT2 inhibitors and cancer. Int J Endocrinol 2014:719578
Leiter LA, Cefalu WT, de Bruin TW et al (2014) Dapagliflozin added to usual care in individuals with type 2 diabetes mellitus with preexisting cardiovascular disease: a 24-week, multicenter, randomized, double-blind, placebo-controlled study with a 28-week extension. J Am Geriatr Soc 62:1252–1262
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373:2117–2128
Ferrannini E, Veltkamp SA, Smulders RA et al (2013) Renal glucose handling: impact of chronic kidney disease and sodium–glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care 36:1260–1265
Barnett AH, Mithal A, Manassie J et al (2014) Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2:369–384
Solini A (2016) Extra-glycaemic properties of empagliflozin. Diabetes Metab Res Rev 32:230–237
Ruggenenti P, Porrini EL, Gaspari F et al (2012) Glomerular hyperfiltration and renal disease progression in type 2 diabetes. Diabetes Care 35:2061–2068
Kohan DE, Fioretto P, Tang W et al (2014) Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int 85:962–971
Powers MA, Bardsley J, Cypress M et al (2015) Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care 38:1372–1382
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Human and animal rights
This article does not contain studies with human or animal subjects performed by any of the authors.
Informed consent
None.
Additional information
Managed by Massimo Porta.
Rights and permissions
About this article
Cite this article
Solini, A. Role of SGLT2 inhibitors in the treatment of type 2 diabetes mellitus. Acta Diabetol 53, 863–870 (2016). https://doi.org/10.1007/s00592-016-0856-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-016-0856-y