Abstract
Aims
Severe hypoglycemia is one of the strongest predictors of adverse clinical outcomes in patients with type 2 diabetes. Our study addressed the question whether there is a relationship between hypoglycemic events (HE) and severe cardiac arrhythmias in type 2 diabetic patients with established clinical risk factors under real-world conditions.
Methods
We included 94 patients with type 2 diabetes and documented cardiovascular disease, in which interstitial glucose values and Holter ECG were recorded for 5 days in parallel. Patients received a stable treatment with insulin and/or sulfonylurea and were instructed to record symptoms of hypoglycemia or arrhythmias.
Results
Continuous glucose monitoring revealed 54 HE (interstitial glucose <3.1 mmol/l) in a total of 26 patients. Patients perceived only 39 % of HE during the day and 11 % of HE during the night. Patients with HE had a significantly higher number of severe ventricular arrhythmias [ventricular tachycardia (VT) 32.8 ± 60 vs. 0.9 ± 4.2, p = 0.019], and multivariate regression analysis revealed the duration of severe HE and TSH level as independent predictors of the occurrence of a VT.
Conclusions
In conclusion, our study suggests that hypoglycemia might be able to trigger at least under certain circumstances, such as low TSH, ventricular arrhythmias under real-world conditions. The large number of unrecognized HE and VT in vulnerable patients treated with insulin or sulfonylurea should encourage the practitioner to focus on stable glucose control and to search for silent HE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe hypoglycemia is one of the strongest predictors of macrovascular events, adverse clinical outcomes and mortality in patients with type 2 diabetes. However, it still remains to be clarified whether there is a direct pathophysiological link or whether hypoglycemia is only a marker of vulnerability to these events [1–5]. Secondary analyses of large clinical trials investigating risk and benefit of intensified glucose control on cardiovascular outcomes have shown that better glucose control was associated with better outcome despite the increased risk of hypoglycemia in the intervention arm [3, 6]. Nevertheless, there is a controversial debate whether or not the small beneficial effect on microvascular complications of reaching the target HbA1c might indeed outweigh the harmful effects of drug- induced hypoglycemia under real-world conditions [7]. Recent trials suggested an association between hypoglycemia and cardiac arrhythmias, but major limitations of these studies are either the small number of participants if gold standard methods for assessment of hypoglycemic events (HE) were used, or insufficient recording of HE if only symptomatic events were registered [1, 8–10].
In a pilot study, our group demonstrated an increased rate of both silent HE and asymptomatic ventricular tachycardia (VT) in a cohort of patients with type 2 diabetes and preexisting major macrovascular events treated with insulin and/or sulfonylurea compared to a treatment with metformin or DDP IV inhibitors [11]. The present study aimed at extending the observations in a larger cohort of patients with a broad spectrum of established clinical risk factors. Specifically, we addressed the question whether there is a temporal association between HE and ventricular arrhythmias during the day and/or night, whether there is a specific pattern of the ratio of asymptomatic vs. symptomatic events, and whether there are determinants of risk for both HE events and arrhythmias under real-world conditions. Finally, we also analyzed the putative relationship between HE and VT.
Materials and methods
This cross-sectional study included frail patients with type 2 diabetes with a proven cardiovascular event, e.g., coronary heart disease with previous myocardial infarction, coronary artery bypass grafting or PCI, cerebrovascular disease with previous stroke, surgical/endovascular procedures or advanced arteriosclerosis at the internal carotid artery or peripheral artery disease with limb amputation due to an ischemic event or surgical or endovascular procedures at the lower limb arteries. In addition, patients should be on a stable treatment with blood glucose lowering medication that is known to potentially cause hypoglycemia.
Exclusion criteria were type 1 diabetes, known atrial fibrillation or atrioventricular block > grade 1, previous implantation of a pacemaker or a defibrillator, known hypokalemia or thyroid disorders and treatment with antiarrhythmic drugs other than beta-blocker or calcium channel blocker.
We recorded interstitial glucose (iG) values every 5 min for 5 days using the continuous glucose monitoring (CGM) system (Medtronic ipro2®). In parallel, Holter ECG was registered and analyzed with the ECGpro® system (Amedtec). A HE was considered as iG value below 3.1 mmol/l during CGM—a threshold which indicates the onset of neurological symptoms. Patients were instructed to perform at least four measurements per day with a self-monitoring glucose system (FreeStyle®, Abbott) for calibration of CGM and to record all symptoms of hypoglycemia and arrhythmias with date and time using a diary.
Prior to the recording of iG and ECG, a blood sample was drawn for determination of HbA1c, thyroid stimulating hormone (TSH), creatinine, cholesterol levels, sodium and potassium concentrations.
Eligible patients were recruited between 2012 and 2014 in our outpatient department for metabolic diseases. Ninety-four patients were included into the analysis, 77 patients (82 %) were treated with insulin or a combination of insulin with any oral glucose lowering drug, 5 patients (5.3 %) were treated with sulfonylurea alone or in combination with other oral glucose lowering drugs and 12 patients (12.7 %) were treated with DPP 4 inhibitor in combination with metformin (n = 7) or metformin alone (n = 5). The remaining baseline characteristics and the proportions of cardiovascular diseases are displayed in Table 1. The study and all procedures were approved by the local ethical committee of the Saxony Association of Physicians. All patients gave written informed consent before inclusion into the study.
Statistical analysis
We calculated the following parameter from CGM recordings: average iG over 5 days and standard deviation of iG values; mean amplitude of glucose excursions (MAGE), the area under the glucose curve at the second day of CGM—at this day, patients received a standardized meal for adjustment of postmeal glucose excursions, and the frequency and time of HE. The standardized meal consisted of 72.3 g carbohydrates, 21.7 g protein and 23.1 g fat (energy content 593 kcal) and was consumed at breakfast. The ECG analysis included: mean, maximal and minimal heart rate (beats per minute), corrected QT time, numbers of ventricular extrasystoles (VES), couplets, triplets and ventricular tachycardia (VT). Heart rate variability as marker of cardiac autonomic neuropathy was assessed using the amplitude of R–R intervals and the standard deviation of normal R–R intervals (SDNN). We compared patients with versus without HE using T Test, or—if parameter were not normally distributed—Mann–Whitney test. Comparison of categorical variables was performed with Chi-square test. We calculated a stepwise regression analysis to evaluate independent parameter for the occurrence of VT and HE. Data are presented as mean ± SD if not indicated otherwise.
Results
Patients were divided according to the results of the 5-day CGM into a group of patients (n = 26) with at least one HE (iG < 3.1 mmol/l, HE group) and a group without such an event during the recording (n = 68, non-HE group). Fifty-four episodes of hypoglycemia were observed, corresponding to an average of 2.4 episodes per patient in the HE group. Eighteen events occurred during daytime and 36 during sleeping time (p = 0.004, Chi-square Test for the comparison of hypoglycemia frequency daytime vs. nighttime). However, only seven events during daytime (38.9 %) and four events during nighttime (11.1 %) were perceived by the patients.
As demonstrated in Table 1, age, diabetes duration, sex, cardiovascular events and cardiovascular risk factors as well as the treatment with beta-blocker were not significantly different between HE group and non-HE group, but we observed significant differences in parameters of glycemic control: HbA1c as well as average iG during 5 days of recording and the area under the interstitial glucose curve at the second day of recording were lower in patients with a severe HE (Table 1). In addition, there was a higher variability of recorded interstitial glucose values displayed as its standard deviation (Table 1). This might represent greater glucose excursions due to counter regulatory effects as a consequence of hypoglycemia. Proportions of glucose lowering treatments were not different between patient groups.
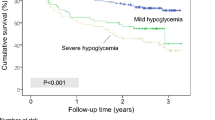
Parallel recording of ECG revealed a higher average number of ventricular arrhythmias in the HE group, especially ventricular tachycardias (VT) (Table 2). In addition, the proportion of patients who developed a VT was significantly higher in patients with severe hypoglycemia (50 vs. 16.1 %, Table 2). Only one patient perceived cardiac arrhythmias during the recording. Rate of polyneuropathy and SDNN as marker of cardiac autonomic neuropathy as well as the corrected QT interval as potential confounders were not significantly different between the two groups (Tables 1, 2). A comparison of the frequency of VT at daytime and during nighttime revealed no significant differences (0.66 ± 2.8 vs. 0.53 ± 2.1, p = 0.402). We analyzed the relationship between parameters of glycemic control and ventricular tachycardia using a stepwise regression analysis as shown in Table 3a. Only the time of interstitial glucose values below 3.1 mmol/l and TSH level were independent predictors of VT. Furthermore, we analyzed independent predictors of a HE by multivariate regression analysis (Table 3b) and identified HbA1c and SD of iG values.
Discussion
This case–control study of frail type 2 diabetic patients at high cardiovascular risk, which were treated with glucose lowering drugs associated with a risk of hypoglycemia, provides additional data on the clinical relevance of hypoglycemia and its possible association with critical ECG changes, in particular ventricular arrhythmias, under real-world conditions. By parallel CGM and Holter ECG recordings, we observed that even among trained patients with regular SMBG, the majority of critical HE remained asymptomatic. In particular, nocturnal episodes were not perceived by the majority of patients. In contrast to most clinical studies, CGM recording revealed that HE occurred more often during night than at daytime [5]. This is in accordance with other recently published CGM-based studies [7, 8, 12]. Even more important, the vast majority of VTs were not perceived by the patients.
We also addressed the question whether there are determinants of HE and arrhythmias in this study population. In contrast to previous studies [5], our groups with and without HE did not differ in regard to major clinical disease, such as coronary artery disease, diabetic polyneuropathy, chronic kidney disease, arterial hypertension and obesity. Therefore, we can largely exclude that the association between HE and arrhythmias in our cohort is merely a marker of vulnerability to these events. In contrast, we observed that patients with a HE were significantly more often treated with diuretics (65 vs. 29 %, Table 1), suggesting that potassium deficiency could contribute to the risk of ventricular arrhythmia. Potassium levels of our patients were within the normal range (as per inclusion criteria) and were not an independent predictor of VT in the multivariate analysis. However, we found a significant univariate inverse correlation between potassium levels and QTc (R = −0.228, p < 0.05) as widely accepted surrogate parameter and risk factor for developing ventricular fibrillation [13, 14]. Indeed, in our univariate analysis, QTc was significantly correlated with occurrence of VT (R = 0.223, p > 0.05), but the multivariate regression analysis revealed only time of HE and TSH level as independent predictors of VT. This confirms data from studies which demonstrated a prolongation of QT interval (as possible trigger for ventricular fibrillation) only after long-lasting HE of >30 min [9]. Accordingly, our findings suggest that long-lasting severe HE may be causally related to severe arrhythmic complications. Another interesting finding is the effect of low TSH levels on the occurrence of VT despite exclusion of patients with clinical manifest hyperthyroidism. These data indicate that latent hyperthyroidism or even low normal values may be an underestimated risk factor in patients which are likely to develop ventricular arrhythmias [15, 16]. This may also call into question the clinical practice to substitute hypothyroid patients in the upper normal range, especially when they are at risk of arrhythmias and hypoglycemia.
As independent predictors for severe HE, we observed SD of interstitial glucose and HbA1c (Table 3b); however, HbA1c in patients with and without HE was 7.1 versus 7.6 %—both values are within the recommended target range. By extrapolation, these findings suggest that low glycemic variability is an important parameter of safe diabetes control if HbA1c is within the target range [17]. Our data did not allow evaluating whether the SD might be either a cause of hypoglycemia (as it can reflect swinging glucose values due to inappropriate subcutaneous insulin administration) or a consequence due to counter regulatory effects with sympathetic activation after a HE.
A recent study reported prolonged bradycardia due to a suppressed sympathetic response after a HE as a possible trigger for the development of ventricular premature beats [8]. We did not analyze the ECG intervals before and after each HE in such detail. However, we could not demonstrate a close temporal association between VT and severe HE, since HE occurred most often during the night, whereas the frequency of VT was not different between daytime and nighttime. Renal function might influence the occurrence of HE in insulin-treated patients since the majority of exogenous insulin is metabolized by the kidney. Most of our patients had normal renal function, and creatinine levels were not different between patients with and without HEs.
Taken together, we observed a higher number of severe ventricular arrhythmias in patients with HEs that are at high cardiovascular risk. Of note, our large study cohort was well balanced for major comorbidities. Furthermore, our study revealed the duration of the HE as an independent predictor of the occurrence of VT and detected a TSH level within the lower range of normal as an additional independent risk factor for VT. The study design did not allow to clarify a causal relationship between HE and VT. However, the large number of subjects, the exclusion of typical confounding factors, such as major clinical disease, and the assessment of events with gold standard methods increased the quality of statistical analyses and suggests that hypoglycemia might be able to trigger, at least under certain circumstances, such as a low TSH, ventricular arrhythmias. It is questionable whether a prospective trial which could eventually clarify a causal relationship will ever been performed due to ethical reasons. Our findings under real-world conditions—the high number of unrecognized HE and VT in vulnerable patients treated with insulin or sulfonylurea—should encourage the practitioner to focus on stable glucose control and to search for silent HE in diabetic patients at high cardiovascular risk.
References
Bedenis R, Price AH, Robertson CM, Morling JR, Frier BM, Strachan MW, Price JF (2014) Association between severe hypoglycemia, adverse macrovascular events, and inflammation in the Edinburgh Type 2 Diabetes Study. Diabetes Care 37(12):3301–3308
McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA (2012) Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 35(9):1897–1901
Mellbin LG, Ryden L, Riddle MC, Probstfield J, Rosenstock J, Diaz R, Yusuf S, Gerstein HC (2013) Does hypoglycaemia increase the risk of cardiovascular events? A report from the ORIGIN trial. Eur Heart J 34(40):3137–3144
Nordin C (2014) The proarrhythmic effect of hypoglycemia: evidence for increased risk from ischemia and bradycardia. Acta Diabetol 51(1):5–14
Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S (2010) Severe hypoglycemia and risks of vascular events and death. N Engl J Med 363(15):1410–1418
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358(24):2560–2572
Clark AL, Best CJ, Fisher SJ (2014) Even silent hypoglycemia induces cardiac arrhythmias. Diabetes 63(5):1457–1459
Chow E, Bernjak A, Williams S, Fawdry RA, Hibbert S, Freeman J, Sheridan PJ, Heller SR (2014) Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes 63(5):1738–1747
Gill GV, Woodward A, Casson IF, Weston PJ (2009) Cardiac arrhythmia and nocturnal hypoglycaemia in type 1 diabetes—the ‘dead in bed’ syndrome revisited. Diabetologia 52(1):42–45
Nordin C (2010) The case for hypoglycaemia as a proarrhythmic event: basic and clinical evidence. Diabetologia 53(8):1552–1561
Stahn A, Pistrosch F, Ganz X, Teige M, Koehler C, Bornstein S, Hanefeld M (2014) Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: silent hypoglycemias and silent arrhythmias. Diabetes Care 37(2):516–520
Hay LC, Wilmshurst EG, Fulcher G (2003) Unrecognized hypo- and hyperglycemia in well-controlled patients with type 2 diabetes mellitus: the results of continuous glucose monitoring. Diabetes Technol Ther 5(1):19–26
Curione M, Di Bona S, Amato S, Turinese I, Tarquini G, Gatti A, Mandosi E, Rossetti M, Varrenti M, Salvatore S, Baiocco E, Morano S (2014) Lack of the QTc physiologic decrease during cardiac stress test in patients with type 2 diabetes treated with secretagogues. Acta Diabetol 51(1):31–33
Dumotier BM (2014) A straightforward guide to the basic science behind arrhythmogenesis. Heart 100(24):1907–1915
Collet TH, Gussekloo J, Bauer DC, den Elzen WP, Cappola AR, Balmer P, Iervasi G, Asvold BO, Sgarbi JA, Volzke H, Gencer B, Maciel RM, Molinaro S, Bremner A, Luben RN, Maisonneuve P, Cornuz J, Newman AB, Khaw KT, Westendorp RG, Franklyn JA, Vittinghoff E, Walsh JP, Rodondi N (2012) Subclinical hyperthyroidism and the risk of coronary heart disease and mortality. Arch Intern Med 172(10):799–809
Cooper DS, Biondi B (2012) Subclinical thyroid disease. Lancet 379(9821):1142–1154
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C (2006) Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295(14):1681–1687
Acknowledgments
The authors thank Medtronic for supplying the CGM equipment.
Conflict of interest
The authors declare that there are no potential conflicts of interest relevant to this study.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and Animal Rights disclosure
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Federici.
Rights and permissions
About this article
Cite this article
Pistrosch, F., Ganz, X., Bornstein, S.R. et al. Risk of and risk factors for hypoglycemia and associated arrhythmias in patients with type 2 diabetes and cardiovascular disease: a cohort study under real-world conditions. Acta Diabetol 52, 889–895 (2015). https://doi.org/10.1007/s00592-015-0727-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-015-0727-y