Abstract
Aim
Studies have identified the metabolically obese normal-weight (MONW) phenotype, which carries increased risk of diabetes and cardiovascular disease. We aimed to investigate the ability of lipid accumulation product (LAP) and visceral adiposity index (VAI), two markers of visceral obesity, to identify the MONW phenotype.
Methods
Normal-weight participants [body mass index (BMI) being of 18.5–23 kg/m2] (n = 3,552; 46.9 % men) in the 2009 nationwide China Health and Nutrition Survey were included in our analysis. Four different criteria that have been published were used to define the MONW phenotype. LAP and VAI were calculated according to published formula.
Results
Receiver operating characteristic (ROC) curve analysis revealed that, regardless of the definition used to define MONW phenotype, both LAP [area under the ROC curve (AUC) ranging from 0.606 to 0.807 depending on the criteria used for MONW phenotype] and VAI (AUC ranging from 0.611 to 0.835 depending on the criteria used for MONW phenotype) outperformed anthropometric parameters including BMI, waist circumference, waist-to-hip ratio, and waist-to-height ratio for identifying MONW phenotype. Both LAP and VAI were strongly related to the MONW phenotype, irrespective of the criteria used to define the MONW phenotype. The associations between the 4th quartile of LAP and the MONW phenotype or between the 4th quartile of VAI and the MONW phenotype were consistently seen in various subgroups.
Conclusion
Our study demonstrates that both LAP and VAI are effective markers for identifying the Chinese adults with MONW phenotype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The metabolically obese normal-weight (MONW) individuals, despite having normal body weight, but who, like people with obesity, are characterized by the presence of a cluster of cardiovascular risk factors including insulin resistance, impaired glucose tolerance, atherogenic lipid profiles, and hypertension [1, 2]. Evidence has shown that MONW individuals accounted for more than 20 % of the normal-weight population [2, 3]. Moreover, emerging evidence has indicated that the MONW phenotype exhibited increased incidences of diabetes, cardiovascular diseases, and all-cause mortality [4, 5]. The underlying etiology of the MONW phenotype is not well understood. Epidemiologic studies have indicated that increased visceral adipose tissue content is the main mechanism [6, 7]. Early identification of MONW individuals, who often elude screening as they are not perceived as high risk, is important to predict and prevent cardiovascular involvement, particularly in Chinese population, who, despite being generally less obese, are more prone to visceral fat accumulation and insulin resistance compared with western populations [8].
Imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), are currently the gold standard for measuring visceral adiposity. However, they are not suitable for routine clinical practice since performing MRI and CT scans is expensive, labor intensive, and poses a radiation hazard. We hypothesized that clinically measurable markers which can capture increased visceral adiposity may be useful in identifying the MONW phenotype. The lipid accumulation product (LAP), an index based on a combination of waist circumference (WC) and fasting triglyceride (TG), and visceral adiposity index (VAI), an index estimated with the use of both anthropometric (BMI and WC) and metabolic [TG and high-density lipoprotein cholesterol (HDL-C)] parameters, are two reliable markers of central lipid accumulation [9, 10]. Therefore, we aimed to investigate the usefulness of LAP and VAI for identifying individuals as having the MONW phenotype in normal-weight persons. In addition, to date, there is no uniform definition for the MONW phenotype, which may render findings difficult to compare. Thus, we further assessed whether there is consistency in the association of the visceral adiposity indicators with MONW phenotype using different definitions of metabolic obese.
Methods
Study design and participants
The China Health and Nutrition Survey (CHNS) is the only large-scale longitudinal, household-based survey in China. Full details of the study have been described elsewhere [11]. Briefly, the CHNS rounds were conducted in 1989, 1991, 1993, 1997, 2000, 2004, 2006, and 2009. For each round, a stratified multistage, random cluster process was employed to draw study sample from each of the nine provinces (Liaoning, Heilongjiang, Jiangsu, Shandong, Henan, Hubei, Hunan, Guangxi, and Guizhou), covering approximately 56 % of China’s population, that vary significantly in terms of geography, economic development, and health status. Each participant provided a written informed consent, and the study was approved by the institutional review committees of the University of North Carolina at Chapel Hill, the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention, and the China-Japan Friendship Hospital, Ministry of Health.
The present study examined data from CHNS 2009, from which fasting blood samples were available. Participants aged ≥18 years and with a BMI of 18.5–23 kg/m2 [according to the World Health Organization (WHO) criteria for Asians, normal weight is defined as BMI of 18.5–23 kg/m2] [12] were eligible for the current analysis. Exclusion criteria included pregnancy, no fasting before blood withdrawal, and with incomplete information on metabolic abnormalities that used to define MONW phenotype. The final sample for the present analysis consisted of 3,552 normal-weight participants. All participants were asked to complete a structured questionnaire which provided information on age, sex, urban/rural settings, regions (southern/northern), educational attainment, histories of current and previous illness, and medical treatment.
Measurements
BMI was calculated as weight (in kilograms) divided by the square of height (in meters). WC was measured with an inelastic tape at a midpoint between the bottom of the rib cage and the top of the iliac crest at the end of exhalation. Seated systolic/diastolic blood pressure (BP) was measured by trained technicians in triplicate after a 10-min rest, using mercury manometers. The three readings were averaged as the BP values in our data analysis.
Blood was collected after an overnight fast. Serum samples were stored at −86 °C for later laboratory analysis. All blood samples were analyzed in a national central laboratory in Beijing using the Hitachi 7600 automated analyzer (Hitachi Inc., Tokyo, Japan), with strict quality control. Fasting glucose was measured by the GOD-PAP method (Randox Laboratories Ltd, UK). Serum TG was measured by GPO-PAP method (Kyowa Medex Co., Tokyo, Japan). Low-density lipoprotein cholesterol (LDL-C) and HDL-C concentrations were measured enzymatically (Kyowa, Japan). Serum apolipoprotein A1 and apolipoprotein B were measured by immunoturbidimetric method (Randox Laboratories Ltd, UK). Hypersensitive C-reactive protein (hs-CRP) was determined by immunoturbidimetric method (Denka Seiken, Japan reagents). Serum uric acid (UA) was measured by enzymatic colorimetric method (Randox Laboratories Ltd, UK). Serum alanine aminotransferase (ALT) was measured enzymatically (Randox Laboratories Ltd, UK). Fasting insulin was measured using the radioimmunology assay (Gamma counter XH-6020, China). Insulin resistance was estimated by the homeostasis model assessment (HOMA-IR) formula: HOMA-IR = fasting insulin (micro-international units per milliliter) × FPG (millimoles per liter)/22.5. LAP and VAI were calculated using the published formula [9, 10]. LAP: [9] men: [WC (cm) − 65] × [TG (mmol/l)]; women: [WC (cm) − 58] × [TG (mmol/l)]. To avoid having nonpositive values for LAP, we reassigned any WC values for men/women that were <65/58 cm–66.0/59.0 cm. VAI: [10] men: [WC/39.68 + (1.88 × BMI)] × (TG/1.03) × (1.31/HDL); women: [WC/36.58 + (1.89 × BMI)] × (TG/0.81) × (1.52/HDL), where both TG and HDL levels are expressed in mM.
Definitions
Based on previous studies, we used four definitions to identify MONW phenotype: (1) Wildman criterion [2]: having more than two cardiometabolic abnormalities (systolic/diastolic BP ≥ 130/85 mmHg or use of antihypertensive drugs, TG ≥ 1.7 mmol/l or use of lipid-lowering drugs, fasting glucose ≥5.6 mmol/l or use of medications for diabetes, HOMA-IR > 5.13, hs-CRP > 0.1 mg/l, HDL-C ≥ 1.0/1.3 mmol/l for men/women); (2) Karelis criterion [13]: meeting more than two metabolic factors (HOMA ≥ 2.7, TG ≥ 1.7 mmol/l or use of lipid-lowering drugs, HDL-C ≥ 1.0/1.3 mmol/l for men/women, LDL-C ≥ 2.6 mmol/l, hs-CRP ≥ 3.0 mg/l); (3) the Adult Treatment Panel-III (ATP III) definition of metabolic syndrome [14]: having more than two metabolic abnormalities (WC ≥ 90/80 cm for men/women, systolic/diastolic BP ≥ 130/85 mmHg or use of antihypertensive drugs, TG ≥ 1.7 mmol/l or use of lipid-lowering drugs, fasting glucose ≥5.6 mmol/l or use of medications for diabetes, HDL-C ≥ 1.0/1.3 mmol/l for men/women); and (4) the HOMA index [15]: having HOMA-IR in upper quartile of the HOMA index.
Statistical analysis
All statistical analyses were conducted using SPSS software (version 12.0 for windows; SPSS, Chicago, IL, USA). Participants were categorized into two phenotypes: metabolically healthy normal-weight (MHNW) and MONW. Continuous variables were presented as medians (25th–75th percentiles) due to their skewed distribution. Mann–Whitney U test was applied to compare MHNW and MONW individuals. Categorical variables were expressed as percentages. A Chi-square test was used to assess differences in proportions between groups. A ROC curve analysis was performed for each adiposity measure to determine its ability to correctly discriminate MONW phenotype. The overall diagnostic accuracy was quantified using the area under the ROC curve (AUC). Odds ratios (OR) and corresponding 95 % confidence intervals (CI) were estimated with the use of logistic regression analysis. Significance was accepted at a two-tailed P < 0.05.
Results
The prevalence of MONW phenotype ranged from 28.2 to 47.9 % depending on the definition. Characteristics of the MONW and MHNW phenotype using Wildman criterion are presented in Table 1. MONW individuals were older than MHNW persons. Both groups were comparable for BMI, upper arm circumference, and triceps skin fold. However, WC, systolic and diastolic BP, TC, TG, LDL-C, apolipoprotein B, fasting glucose, fasting insulin, HOMA-IR, hs-CRP, UA, ALT, LAP, and VAI were significantly higher, whereas HDL-C and apolipoprotein A1 were lower in MONW than in MHNW participants (P < 0.001 for all these components). Not surprisingly, the prevalence of all components of the Wildman’s criterion as well as the prevalence of hyperuricemia was considerably higher in MONW than in MHNW participants (P < 0.001 for all these components).
ROC curves were generated to assess which obesity measures may serve as markers for predicting the MONW phenotype. We found that all adiposity measures including BMI, WC, waist-to-hip ratio, waist-to-height ratio, LAP and VAI were able to predict the MONW phenotype (Table 2). Comparing all these ROC curves, we observed that VAI exhibited the highest diagnostic accuracy for the MONW phenotype (AUC ranging from 0.611 to 0.835 depending on the criteria used for MONW phenotype), whatever the definition of MONW phenotype. LAP was the variable with the second highest diagnostic ability for the MONW phenotype (AUC ranging from 0.606 to 0.807 depending on the criteria used for MONW phenotype). To examine whether reassignment of WC values to avoid having nonpositive values would have impact on the above results, we repeated the ROC curve analysis after excluding men with WC < 65 cm and women with WC < 58 cm. The relevant results were largely replicated (Additional file 1). In the remaining analysis, we focus on the associations of MONW phenotype with LAP and VAI, since they are more accurate measures of adiposity and more predictive of MONW phenotype.
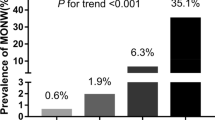
Both LAP and VAI were strongly related to MONW phenotype, irrespective of the criteria used to define the MONW phenotype (Fig. 1). The risk of MONW phenotype rose progressively with increasing values of LAP, with no evidence of a threshold. The crude ORs (95 % CIs) (model 1) for MONW phenotype using Wildman criteria were 1.46 (1.20–1.79) for the second, 2.37 (1.95–2.88) for the third, and 8.77 (7.07–10.87) for the fourth LAP quartile, in comparison with the first LAP quartile. This association was attenuated but still highly significant (P < 0.001) after adjustment for potential intermediate variables (model 3). A trend toward higher risk of MONW phenotype according to Wildman criteria was observed as VAI increased. Participants in the highest VAI quintile had a 10.50-fold (95 % CI 8.39–11.14) increased risk of MONW phenotype compared with those with a VAI in the lowest quintile (model1). This relation was persisted even after adjustment for potential confounding variables (model 3).
Odds ratios (OR) and 95 % confidence intervals (CI) for MONW phenotype associated with visceral obesity measures. Vertical bars are 95 % CIs. Metabolically obese normal-weight phenotype was defined using four different definitions: Wildman criterion (a), Karelis criterion (b), ATP III criterion (c), and HOMA index (d). Definitions of each criterion were defined in the “Definitions” section. Model 1 was an unadjusted model. Model 2 was adjusted for age, sex, socioeconomic status (rural/urban settings, region, and education level), smoking status, and alcohol use. Model 3 was adjusted for all variables in model 2 plus ALT, apolipoprotein A1, apolipoprotein B, and uric acid
Figure 2 shows the crude ORs for MONW phenotype according to Wildman criterion associated with the top quartiles of LAP and VAI compared with their first quartiles in various subgroups. The relations between these two adiposity markers and risk of MONW phenotype were consistently seen in both genders; all age-groups, irrespective of the presence of the cardiometabolic risk factors (hypertension, apolipoprotein B/apolipoprotein A1 ≥ 0.8, hyperuricemia). However, in all evaluated subgroups, except for the diabetes subgroup, the relations between the 4th quartile of VAI and MONW phenotype were consistently stronger than those between the 4th quartile of LAP and MONW phenotype (P < 0.001). The relations between LAP or VAI and MONW phenotype disappeared in the diabetes subgroup. Both LAP (11.05, 5.52–21.88) and VAI (28.71, 16.01–45.40) showed the strongest relation with MONW phenotype in the hyperuricemia subgroup. Results were replicated when other three criteria were used separately to define MONW phenotype (data not shown).
Odds ratios (OR) and 95 % confidence intervals (CI) for metabolically obese normal-weight phenotype according to Wildman criterion associated with 1 standard deviation increase in a specific visceral obesity measure in various subgroup. Definitions of Wildman criterion were defined in the “Definitions” section. Hypertension was defined as systolic/diastolic blood pressure ≥ 140/90 mmHg or use of antihypertensive drugs. Lipid disorder was defined as apolipoprotein B/apolipoprotein A1 ≥ 0.8. Hyperuricemia was defined as UA ≥ 6 mg/dl for women and ≥ 7 mg/dl for men. Diabetes was defined as fasting glucose ≥ 7.0 mmol/l or use of medications for diabetes
Discussion
The present study demonstrated that, despite having the same BMI as MHNW persons, the MONW individuals suffered from a worse cardiometabolic profile and had higher levels of LAP and VAI. The cardiometabolic disorders were also more prevalent in MONW individuals. Both LAP and VAI were much superior to anthropometric indicators of obesity such as BMI, WC, waist-to-hip ratio and waist-to-height ratio for identifying four different definitions of MONW phenotype. In addition, both LAP and VAI were highly related to MONW phenotype and the relationships were consistently seen in men and women, old and young, and those with or without hypertension, lipid disorder, or hyperuricemia (which are potential coexistence of obesity), indicating that both LAP and VAI were of value, even in those with low levels of other risk factors, for predicting MONW phenotype. Furthermore, of the two visceral adiposity indicators assessed, VAI outperformed LAP for predicting MONW phenotype. To the best of our knowledge, this is the first study evaluating the performance of LAP and VAI in identifying the MONW phenotype.
Our finding that approximately half of the sample had the MONW phenotype according to Wildman criteria supports the notion that Asians have a high risk of MONW [16]. A large abdominal fat accumulation in Asians [8] may explain the high prevalence. The significantly higher levels of LAP and VAI in MONW individuals compared with healthy normal-weight persons may mediate a worse cardiovascular risk profile through the increased visceral fat, that in turn confer a higher risk of cardiovascular involvement. The high prevalence of MONW individuals combined with a significantly increased risk of incidences of diabetes, cardiovascular disease, and all-cause mortality in MONW individuals observed in several prospective cohort studies [4, 5, 17] highlights the importance of screening for the MONW phenotype.
Emerging evidence shows that the MONW phenotype is characterized by increased visceral adiposity [6, 7]. Visceral fat accumulation is strongly associated with deleterious cardiometabolic profile [18]. Sophisticated imaging methods that directly measure the visceral fat are costly and complicated; thus, surrogate markers of visceral fat are more commonly utilized. Although BMI is the most frequently used indicator to provide a standardized definition of obesity, it lacks discriminatory power between fat and lean tissues, as evidenced by the occurrence of substantial variation in metabolic disturbance among individuals with similar levels of adiposity as measured by BMI [2]. This limited discriminatory power is especially pertinent for Asian populations, who have a greater amount of visceral adipose tissue compared with Europeans per given BMI value [8, 19]. Moreover, the association between BMI and the amount of visceral adiposity among elderly individuals is stronger than that among younger persons as aging is associated with a condition of sarcopenic obesity characterized by high body fat in the presence of reduced lean body mass [20]. Hence, grouping elderly individuals by BMI may incur greater potential error in assuming body fat content than the standard age-related underestimation associated with BMI. A similar limitation exists for anthropometric indicators of central obesity including WC, waist-to-hip ratio, and waist-to-height ratio [21, 22]. Therefore, greater emphasis should be placed on markers that can better capture excess visceral accumulation. The Quebec Cardiovascular Study group firstly introduced the hypertriglyceridemic waist phenotype (a combination of WC ≥ 90 cm along with fasting TG ≥ 2.0 mmol/l), a dichotomous index, as a marker of excess visceral adiposity and atherogenic metabolic triad (i.e., hyperinsulinemia, hyperapolipoprotein B and small, dense LDL particles) in men [23] and demonstrated that the hypertriglyceridemic waist phenotype was a good predictor of 5-year risk of cardiovascular disease [24]. The CHICAGO cohort showed that the hypertriglyceridemic waist phenotype could represent a simple marker of excess visceral fat in persons with type 2 diabetes [25]. However, visceral accumulation may not be adequately described by a dichotomous index as obesity itself is a continuous process. Alternatively, LAP has been developed as a continuous index to reflect the combined anatomic and physiological changes associated with visceral fat deposition [9]. Previous studies indicated that LAP was superior to BMI for identifying cardiovascular risk and diabetes [26]. Several prospective studies demonstrated that LAP outperformed BMI in predicting all-cause mortality [27, 28]. Our study showed for the first time that LAP had greater area under the ROC curve than anthropometric indexes including BMI, WC, waist-to-hip ratio, and waist-to-height ratio and thus illustrated superior performance of LAP in identifying MONW phenotype. Similarly, the Alkam Metabolic Syndrome Study firstly introduced the VAI as a good indicator of visceral adipose tissue (measured with MRI) and was inversely associated with insulin sensitivity (evaluated with a euglycemic-hyperinsulinemic clamp) [10]. Accumulating evidence showed that VAI is associated with increased risk of coronary heart disease [10, 29]. Our finding that VAI had the highest area under the ROC curve indicates the supremacy of VAI over LAP for detecting MONW phenotype.
Both LAP and VAI indicate close relations with the MONW phenotype, and the relations are consistent in all subgroups studied, except for the diabetes subgroup. These findings imply that LAP and VAI, offering advantages of a reduced economic burden and no radiation exposure, may serve as predictors of MONW phenotype. Interestingly, in our study, both LAP and VAI have stronger relations with MONW phenotype in nondiabetic than in diabetic subgroup. Coincidently, a recent study showed that LAP predicts mortality better in nondiabetic than diabetic patients [27]. Although explanations for this remains to be clarified, it is probably that early changes associated with lipid overaccumulation and reflected by increased LAP or VAI trigger a worse cardiovascular risk profile; however, once the diabetes occurs, other factors rather than visceral adiposity might become more important. Another explanation for the no significant relations between LAP or VAI and MONW phenotype in diabetic subgroup might due to small number of patients with diabetes (n = 168), which may incur low statistical power. In our study, relations between LAP or VAI and MONW phenotype were strongest in the hyperuricemia subgroup. This may be related to the fact that UA is a considerable discriminator between metabolically healthy and metabolically obese [30].
The limitations of the present study deserve comment. First, no direct measure of visceral adiposity was done. Second, since the present study was conducted only in Chinese population, extrapolating results to other populations should be interpreted cautiously. Third, estimates across subgroups should also be interpreted with caution because of limited sample size.
In conclusion, both LAP and VAI, easily obtainable indexes, performed better than usually applied anthropometric parameters for the assessment of MONW phenotype, which is of importance given the high prevalence of MONW phenotype in Chinese population. The early identification of MONW individuals who are predisposed to the developments of diabetes and cardiovascular disease will allow the introduction of early interventions to prevent or delay the progression to cardiovascular involvement.
References
Karelis AD, St-Pierre DH, Conus F, Rabasa-Lhoret R, Poehlman ET (2004) Metabolic and body composition factors in subgroups of obesity: what do we know? J Clin Endocrinol Metab 89:2569–2575
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, Sowers MR (2008) The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med 168:1617–1624
Pajunen P, Kotronen A, Korpi-Hyovalti E, Keinanen-Kiukaanniemi S, Oksa H, Niskanen L, Saaristo T, Saltevo JT, Sundvall J, Vanhala M, Uusitupa M, Peltonen M (2011) Metabolically healthy and unhealthy obesity phenotypes in the general population: the FIN-D2D Survey. BMC Public Health 11:754
Hamer M, Stamatakis E (2012) Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab 97:2482–2488
Kuk JL, Ardern CI (2009) Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care 32:2297–2299
Stefan N, Kantartzis K, Machann J, Schick F, Thamer C, Rittig K, Balletshofer B, Machicao F, Fritsche A, Haring HU (2008) Identification and characterization of metabolically benign obesity in humans. Arch Intern Med 168:1609–1616
Conus F, Allison DB, Rabasa-Lhoret R, St-Onge M, St-Pierre DH, Tremblay-Lebeau A, Poehlman ET (2004) Metabolic and behavioral characteristics of metabolically obese but normal-weight women. J Clin Endocrinol Metab 89:5013–5020
Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R, Massien C, Almeras N, Despres JP (2012) Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the international study of prediction of intra-abdominal adiposity and its relationship with cardiometabolic risk/intra-abdominal adiposity. Am J Clin Nutr 96:714–726
Kahn HS (2005) The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord 5:26
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, Galluzzo A (2010) Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33:920–922
Popkin BM, Du S, Zhai F, Zhang B (2010) Cohort profile: The China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol 39:1435–1440
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163
Karelis AD, Rabasa-Lhoret R (2008) Inclusion of C-reactive protein in the identification of metabolically healthy but obese (MHO) individuals. Diabetes Metab 34:183–184
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive summary of the third report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285:2486–2497
Meigs JB, Wilson PW, Fox CS, Vasan RS, Nathan DM, Sullivan LM, D’Agostino RB (2006) Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab 91:2906–2912
Gordon-Larsen P, Adair LS, Meigs JB, Mayer-Davis E, Herring A, Yan SK, Zhang B, Du S, Popkin BM (2013) Discordant risk: overweight and cardiometabolic risk in Chinese adults. Obesity 21:E166–E174
Arnlov J, Ingelsson E, Sundstrom J, Lind L (2010) Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation 121:230–236
Bays HE (2011) Adiposopathy is “sick fat” a cardiovascular disease? J Am Coll Cardiol 57:2461–2473
Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB (1996) How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 143:228–239
Roubenoff R (2004) Sarcopenic obesity: the confluence of two epidemics. Obes Res 12:887–888
Hill JO, Sidney S, Lewis CE, Tolan K, Scherzinger AL, Stamm ER (1999) Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Clin Nutr 69:381–387
Harris TB, Visser M, Everhart J, Cauley J, Tylavsky F, Fuerst T, Zamboni M, Taaffe D, Resnick HE, Scherzinger A, Nevitt M (2000) Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women: the health, aging and body composition study. Ann NY Acad Sci 904:462–473
Lemieux I, Pascot A, Couillard C, Lamarche B, Tchernof A, Almeras N, Bergeron J, Gaudet D, Tremblay G, Prud’homme D, Nadeau A, Despres JP (2000) Hypertriglyceridemic waist: a marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men? Circulation 102:179–184
Tanko LB, Bagger YZ, Qin G, Alexandersen P, Larsen PJ, Christiansen C (2005) Enlarged waist combined with elevated triglycerides is a strong predictor of accelerated atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation 111:1883–1890
Sam S, Haffner S, Davidson MH, D’Agostino RB Sr, Feinstein S, Kondos G, Perez A, Mazzone T (2009) Hypertriglyceridemic waist phenotype predicts increased visceral fat in subjects with type 2 diabetes. Diabetes Care 32:1916–1920
Taverna MJ, Martinez-Larrad MT, Frechtel GD, Serrano-Rios M (2011) Lipid accumulation product: a powerful marker of metabolic syndrome in healthy population. Eur J Endocrinol 164:559–567
Ioachimescu AG, Brennan DM, Hoar BM, Hoogwerf BJ (2010) The lipid accumulation product and all-cause mortality in patients at high cardiovascular risk: a PreCIS database study. Obesity (Silver Spring) 18:1836–1844
Wehr E, Pilz S, Boehm BO, Marz W, Obermayer-Pietsch B (2011) The lipid accumulation product is associated with increased mortality in normal weight postmenopausal women. Obesity (Silver Spring) 19:1873–1880
Zhang X, Shu XO, Li H, Yang G, Xiang YB, Cai Q, Ji BT, Gao YT, Zheng W (2013) Visceral adiposity and risk of coronary heart disease in relatively lean Chinese adults. Int J Cardiol 168:2141–2145
Mangge H, Zelzer S, Puerstner P, Schnedl WJ, Reeves G, Postolache TT, Weghuber D (2013) Uric acid best predicts metabolically unhealthy obesity with increased cardiovascular risk in youth and adults. Obesity (Silver Spring) 21:E71–E77
Acknowledgments
We thank the China Health and Nutrition Survey, supported by the NIH (R01-HD30880, DK056350, and R01-HD38700), and the National Institute of Nutrition and Food Safety, China Center for Disease Control and Prevention, Carolina Population Center, the University of North Carolina at Chapel Hill and the Fogarty International Center for providing the data used here. We also thank the China-Japan Friendship Hospital and Ministry of Health for support for CHNS 2009 survey.
Conflict of interest
Tingting Du, Xuefeng Yu, Jianhua Zhang, and Xingxing Sun declare that they have no conflict of interest.
Ethical standard
The study was approved by the institutional review committees of the University of North Carolina at Chapel Hill, the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention, and the China-Japan Friendship Hospital, Ministry of Health.
Human and Animal Rights disclosure
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Managed by Massimo Porta.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Du, T., Yu, X., Zhang, J. et al. Lipid accumulation product and visceral adiposity index are effective markers for identifying the metabolically obese normal-weight phenotype. Acta Diabetol 52, 855–863 (2015). https://doi.org/10.1007/s00592-015-0715-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-015-0715-2