Abstract
Aim
High glucose-induced oxidative stress has been suggested as one of the mediators of endothelial damage in diabetes. The major endothelial protein, endoglin, has been found overexpressed in the vessels during pathological situations, but little is known about its relation to diabetic vascular complications. To clarify the role of endoglin in endothelial injury, we sought to determine the effects of high and oscillating glucose on its expression.
Materials
Furthermore, the activation of the Krüppel-like factor 6 (KLF-6) and the hypoxia-inducible factor-1α (HIF-1α) as possible regulators of endoglin expression has been evaluated. The possible role of the oxidative stress has been studied evaluating the effects of the antioxidant alpha-lipoic acid (ALA) and the cellular antioxidant response mediated by NAD(P)H:quinine-oxido-reductase-1 (NQO-1) and heme oxygenase-1 (HO-1).
Results
Primary HUVECs were cultured for 21 days in normal, high and oscillating glucose (5, 25 and 5/25 mmol/l every 24 h, respectively) with/without ALA. In oscillating and high glucose total endoglin, its soluble form (sEng), KLF-6 and HIF-1α were significantly increased. Simultaneously, the oxidative DNA stress markers 8-OHdG and H2A.X were elevated. Moreover, ENG gene transcriptional rate increased during glucose exposures concomitantly with increased KLF-6 nuclear translocations. ALA significantly reduced all these phenomena. Interestingly, during oscillating and chronic high glucose, NQO-1 and HO-1 did not increase, but ALA induced their overexpression.
Conclusions
Together, these findings provide novel clue about endoglin in the regulation of high glucose-mediated vascular damage in HUVECs and the role of oxidative stress in this regulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is growing evidence that oxidative stress is involved in the pathogenesis of vascular disease in diabetes [1] and that hyperglycemia induces early endothelial damage through the generation of oxidative stress at mitochondrial level [2–4].
Endoglin (Eng, also known as CD105), a trans-membrane auxiliary receptor (TβRIII) that modulates multiple cellular response to members of TGF-beta signaling, is weakly expressed in resting endothelial cells, but is increased during angiogenesis [5, 6]. Numerous studies have reported a high expression of Eng on endothelial cells (ECs) in several vascular pathological situations, including active site of inflamed tissues, atherosclerosis, in response to arterial injury [7, 8] and in wound healing [9]. Besides membrane-bound Eng, also a soluble form (s-Eng) exists, resulting from the shedding of the membrane-bound receptor [10]. Although the mechanism by which s-Eng is released into the circulation has not been revealed yet, a recent study showed that Eng is proteolytically cleaved near the plasma membrane by matrix metalloproteinases (MMPs), and s-Eng is released into the blood stream [11–13]. Recently, elevated plasma levels of s-Eng have been observed in subjects with vascular diabetic complications [14].
In ECs, the response to vascular injury is mediated by Krϋppel-like factor-6 (KLF-6), a transcription factor that has recently been related to diabetic complication [15]. KLF-6 is considered an injury-response factor that trans-activates several target genes by direct binding to their promoters, as Eng gene among others [16]. A role for KLF-6 in transcriptional activation of Eng is suggested by its rapid induction in response to endothelial denudation during vascular injury [17]. However, KLF-6 mRNA results upregulated by oxidative stress [18] and in high glucose conditions [19, 20]. Oxidative stress activates the hypoxia-inducible factor 1α (HIF-1α), which is stabilized in cytoplasm by the inhibition of prolyl hydroxylases (PHDs), through the oxidation of the ferrous ion, essential for its catalytic mechanism [21]. HIF-1α binds to the hypoxia-responsive elements (HREs) of target genes and upregulates their transcriptions [7], among them, Eng gene [7]. Interestingly, it has already been reported that HIF-1α is overexpressed in high glucose [22]. In previous studies, we have reported that both oscillating glucose and constant high glucose are dangerous for ECs and that oxidative stress is one of the mediators of the damage [4]. With these premises, we have explored the regulation of Eng expression, the functional activation of KLF-6 and HIF-1α and the possible role of oxidative stress, in HUVECs, cultured in high glucose, both constant and oscillating. In order to evaluate the possible role of oxidative stress, the effect of alpha-lipoic acid (ALA) and the intracellular antioxidant response, NAD(P)H:quinine-oxido-reductase-1 (NQO-1) and heme oxygenase-1 (HO-1), has been studied. Furthermore, two markers of oxidative stress, 8-hydroxydeoxyguanosine (8-OHdG) and histone 2A variant (H2A.X), which have been proven to be increased in oxidative stress-associated disease [23] and in genotoxic events [24], have been evaluated.
Materials and methods
Materials and cells cultures
The primary pooled HUVECs were purchased from Lonza (Lonza Bioresearch LBS, Basel, Switzerland) and maintained for 3 weeks in endothelial basal medium (EBM-2), supplemented with 2 % heat-inactivated fetal bovine serum, hydrocortisone (0.04 %), basal fibroblastic growth factor (bFGF, 0.4 %), epidermal growth factor (rhEGF, 0.1 %), heparin (0.1 %) and gentamicin/amphotericin (GA-1000, 0.1 %) (all from Lonza) in a humified incubator with 5 % carbon dioxide added.
Experimental design and glucose exposures
HUVECs were seeded in 6-well plates (Corning, NY, USA) at a density of 1 × 105 cells/wells. Cells were exposed to three different glucose concentrations: (1) normal glucose (NG, 5 mmol/l), (2) oscillating glucose (OG, 5/25 mmol/l), (3) high glucose (HG, 25 mmol/l). In oscillating glucose condition, glucose concentration in the medium was changed alternatively every day (from 5 to 25 mmol/l) for 21 days [4]. Protein and mRNA were collected from oscillating conditions, while the cells were in NG medium. Experimental control was performed incubating the cells in any condition with mannitol at the same concentration of glucose. Cells were treated with/without alpha-lipoic acid (ALA, DL-6,8-thioctic acid, Sigma-Aldrich, St. Louis, MO, USA, 62.5 μmol/l) for the whole treatment [25]. α-Lipoic acid is an organosulfur compound derived from octanoic acid containing two sulfur atoms (at C6 and C8) connected by a disulfide bond and is thus considered to be a very good antioxidant [26].
Determination of 8-OHdG and sEng
8-OHdG in the HUVECs was determined using Bioxytech 8-OHdG-EIA Kit (OXIS Health Products, Portland, OR, USA). s-Eng in the culture supernatants was measured using specific ELISA Kits (R&D systems UK), following the manufacturer’s recommendation. Assays were repeated three times, and each sample was run in triplicate.
Western immunoblots
Cells were harvested, and whole cell lysates were prepared using RIPA buffer (150 mM NaCl, 10 mM Tris, pH 7.2, 0.1 % SDS, 1.0 % Triton X-100, 5 mM EDTA, pH 8.0) containing protease and phosphatase inhibitor cocktail. Protein content of the lysates was determined using the Bradford reagent (Sigma-Aldrich, St. Louis, MO, USA). Samples were subjected to 8–16 % Tris–glycine gradient (SDS-PAGE) gels in reducing conditions and blotted onto polyvinylidene fluoride (PVDF) membrane. After blocking with 5 % non-fat dry milk (NFDM) in 20 mM Tris–HCl (pH 7.5), 135 mM NaCl and 0.1 % Tween-20, blots were incubated with monoclonal antibodies against endoglin (D50G1), HIF-1α, phospho-histone 2AX; obtained from Cell Signaling (Beverly, MA, USA); washed with 20 mM Tris–HCl (pH 7.5), 135 mM NaCl and 0.1 % Tween-20; and incubated with a horseradish peroxidase-conjugated secondary antibody. Proteins were detected using ECL system (Pierce Chemical Co Rockford, IL, USA) according to the manufacturer’s instructions and revealed in CCD camera (ImageQuantLAS4000, GE Healthcare, UK). Antibodies against NQO-1 and HO-1 were obtained from BioVision (San Francisco, CA, USA) while against KLF-6 were obtained from Santa Cruz Biotechnology (R-173; Santa Cruz Biotechnology, CA, USA). The β-actin and α-tubulin (Sigma-Aldrich, St. Louis, MO, USA) and lamin-1B (Cell Signaling, Beverly, MA, USA) were used as loaded controls. Protein content quantification was performed using computer-assisted densitometry (www.imagej.nih.gov, ImageJ, NIH).
Subcellular protein extracts
Cytoplasmic and nuclear fraction extracts were prepared using Subcellular Protein Fractionation Kit for Cultured Cells (Pierce Chemical Co Rockford, IL, USA) as manufacturer described. Thus, HUVEC (1 × 106) cells were fractionated; equal amounts of extracts (10 µg) were separated in 4–20 % Tris–glycine gradient gels (Lonza Bioresearch LBS, Basel, Switzerland) and then run on SDS-PAGE in reducing conditions.
Real-time quantitative-PCR (q-PCR) analysis
Total RNA from HUVECs was extracted using RNA purification kit (Norgen Biotek, Thorold, ON, Canada). RNA was stored at −80 °C if not used immediately. RNA purity was assessed by spectrophotometric analysis (Nanodrop, Wilmington, DE, USA). One micrograms of total RNA was reverse-transcribed using the SuperScript III reverse transcriptase and random hexamers (Invitrogen, Life Technologies, Grand Island, NY, USA). Real-time q-PCR was performed using ABI 7900 HT thermo-cycler (Applied Biosystems, Zurich, Switzerland), in reaction buffer using TaqMan PCR Master Mix. Pre-optimized primers and probes gene expression assay were purchased from Applied Biosystems (ENG: Hs00923996_m1; HMOX1: Hs01110250_m1; NQO-1: Hs00168547_m1; KLF-6: Hs00810569_m1; HIF-1α: Hs00153153_m1; H2AFX: Hs00266783_s1). All q-PCR were normalized to 18 s ribosomal RNA expression provided as a pre-optimized control probe. Data were obtained as Ct values.
Statistical analysis
Results are expressed as mean ± SEM. Statistical analysis was performed using GraphPrism6.0® (www.graphpad.com). Differences between groups were evaluated using the one way ANOVA, followed by Tukey’s post hoc test or when appropriate, by Holm-Sidak’s multiple comparison test. Statistical significance was assumed at p < 0.05. For kinetic study, the interactions among the parts were evaluated using two-way ANOVA, followed by Bonferroni’s post hoc test. At least three different experiments were performed in triplicate to ensure reproducibility.
Results
Endoglin, HIF-1α and KLF-6 expression levels increased in oscillating and high glucose in HUVECs
To test whether high glucose (constant and oscillating) was able to activate Eng expression via HIF-1α and KFL-6 regulations, we have detected mRNA and protein expression levels. The results show increased Eng mRNA expression in OG (p < 0.001) and in HG conditions (p < 0.05; Fig. 1a). The effects were significantly lowest during ALA treatments (OG vs OG + ALA, p < 0.001; HG vs HG + ALA, p < 0.001; Fig. 1a).
High and oscillating glucose induce endoglin, HIF-1α and KLF-6 expression in HUVECs. Upregulation of endoglin, HIF-1α and KLF-6 expression revealed by mRNA q-PCR real time (a, b and c, respectively), densitometry analyses and one representative Western blot (b, d and f, respectively), during oscillating (OG), stable high (HG) and normal glucose (NG), with or without ALA. Data are expressed as mean (±SEM, n = 6–9). ‡ p < 0.05, ‡‡ p < 0.01, ‡‡‡ p < 0.001 vs control. Symbols over the bars refer to differences between the conditions shown under the bars, *p < 0.05, **p < 0.01, ***p < 0.001
HIF-1α mRNA (Fig. 1b) was upregulated in OG and HG conditions (OG, p < 0.01; HG, p < 0.05) compared to normal glucose (NG). ALA reduced the HIF-1α mRNA expression levels (OG vs OG + ALA, p < 0.01; HG vs HG + ALA, p < 0.01; Fig. 1b). The results of the densitometry (Fig. 1d) showed that OG and HG increased the Eng protein level compared to NG, an effect counterbalanced by ALA in both OG and HG (p < 0.001). The protein expression of HIF-1α was increased in high and oscillating conditions compared to NG (OG, p < 0.001; HG, p < 0.01; Fig. 1e). ALA reduced the HIF-1α protein expression in both the conditions (OG vs OG + ALA, p < 0.001, HG vs HG + ALA, p < 0.001; Fig. 1e). During glucose, the KLF6 expression increased in OG (p < 0.001) and HG (p < 0.01) compared to NG (Fig. 1c) and ALA counterbalanced these effects (HG vs H + , p < 0.01; OG vs OG + ALA, p < 0.001. Fig. 1c). The Western blot assay demonstrated that KLF-6 was induced coherently in high and oscillating glucose (HG, p < 0.01; OG, p < 0.001; Fig. 1f) and that with ALA its expression returned to basal condition (OG vs OG + ALA, p < 0.05; HG vs HG + ALA, p < 0.01. Fig. 1f).
Oxidative stress markers
In order to estimate the damage mediated by oxidative stress, we measured 8-OHdG contents and H2AX levels in HUVECs. Our results show increased 8-OHdG in both OG (p < 0.001) and HG (p < 0.01) compared to NG (Fig. 2a). ALA supplementation restored 8-OHdG generation to the basal levels in both HG (HG vs HG + ALA (p < 0.001) and OG (OG vs OG + ALA, p < 0.001, Fig. 2a). H2AX mRNA was upregulated in OG (p < 0.0001) and in HG (p < 0.05) compared to NG. In ALA-treated cells, the results show a significant reduction of the transcriptional activity (p < 0.001) respect to NG. Moreover, HG promoted increased double-strand breaks (DSBs) in the cells that could be demonstrated by γ-H2AX formation. Exposition to OG (p < 0.01) and HG (p < 0.05) resulted in a rapid phosphorylation of H2A.X at Ser139 level, which was suppressed with ALA (OG vs OG + ALA, p < 0.05; HG vs HG + ALA, p < 0.05; Fig. 2c).
Effects of high and oscillating glucose, with or without ALA, on the markers of oxidative stress in HUVECs. a 8-OHdG content (ng/ml) in HUVEC at 21 days of experiments, during oscillating (OG), stable high (HG) and normal glucose (NG), with or without ALA. b mRNA expression levels of H2A.X (histone 2A.X) in HUVEC at 21 days of experiments, during oscillating (OG), stable high (HG) and normal glucose (NG), with or without ALA. c Western blot of γ-H2AX, a marker of oxidative stress-induced double-strand breaks, in HUVEC at 21 days of experiments, during oscillating (OG), stable high (HG) and normal glucose (NG), with or without ALA. Data are expressed as mean (±SEM, n = 6). ‡ p < 0.05, ‡‡ p < 0.01, ‡‡‡ p < 0.001 vs control. Symbols over the bars refer to differences between the conditions shown under the bars, *p < 0.05, **p < 0.01, ***p < 0.001
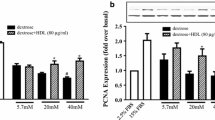
Intracellular antioxidant (NQO-1 and HO-1) response in high and oscillating glucose: the effect of ALA
Both NQO-1 and HO-1 were dysregulated at the transcriptional and protein level during exposure to OG and HG, leading to a lack of activation of cellular defense systems (Fig. 3a–d). ALA strongly induced mRNA levels of both NQO-1 (OG vs OG + ALA p < 0.001, HG vs HG + ALA p < 0.001, NG vs NG + ALA p < 0.001, respectively) and HO-1 (OG vs OG + ALA p < 0.001, HG vs HG + ALA p < 0.001, NG vs NG + ALA p < 0.001, respectively), even in NG (Fig. 3a–b). Consistently, ALA strongly induced the protein levels of both NQO-1 (OG vs OG + ALA p < 0.001, HG vs HG + ALA p < 0.001, NG vs NG + ALA p < 0.001, respectively) and HO-1 (OG vs OG + ALA p < 0.001, HG vs HG + ALA p < 0.001, NG vs NG + ALA p = NS, respectively; Fig. 3c–d).
Alpha-lipoic acid (ALA) induces expression of NQO-1 and HO-1 in high and oscillating glucose. NQO-1 (a, c) and HO-1 (b, d) expression in HUVEC at 21 days of experiments, during oscillating (OG), stable high (HG) and normal glucose (NG), with or without ALA. Data are expressed as mean (±SEM, n = 6). ‡ p < 0.05, ‡‡ p < 0.01, ‡‡‡ p < 0.001 vs control. Symbols over the bars refer to differences between the conditions shown under the bars. *p < 0.05, **p < 0.01, ***p < 0.001
High and oscillating glucose induce the activation of the transcription factor KLF-6 and HIF-1α in HUVECs
Functional activity of KLF-6 was demonstrated by Western blot analyses of cytoplasmic and nuclear fractions in both oscillating and high glucose conditions. Our results revealed that KLF-6 localized predominantly to the nuclear compartment in OG (fig. s1A; p < 0.001 vs OGcyt; p < 0.05 vs NGnuc) and HG (p < 0.001 vs HGcyt; p < 0.05 vs NGnuc). Moreover, the translocation in HG is higher than in OG (p < 0.05 HGnuc vs OGnuc).
To evaluate the potential role of KLF-6 or HIF-1α as activators of Eng transcription after glucose exposure, kinetic analyses were performed at different time points. mRNA expression after high glucose stimulation (25 mmol/l) was measured in real time. The expressions for Eng, KLF6 and HIF-1α are shown with a graphic summarizing the dynamic expressions during glucose exposure (fig. s1C). KLF-6 mRNA was rapidly induced within the third hour of injury. After the early induction of KLF-6, Eng mRNA expression increased approximately twofold at 6–12 h and decreased thereafter. The kinetics of Eng mRNA revealed a time delay of Eng respect to KLF-6 and HIF-1α. Two-way ANOVA reveals significant interactions between ENG and KLF-6 (3 h, p < 0.01; 12 h, p < 0.01; and 72 h, p < 0.05) and ENG and HIF-1α (12 h, p < 0.05 and 48 h, p < 0.001). KLF-6 induction in time-dependent manner is significantly consistent with the possibility that leads to the upregulation of Eng.
Effects of high and oscillating glucose on release of sEng in HUVEC
In order to assess the release of sEng into the media, we additionally performed ELISA quantification in the supernatants of HUVECs treated with/without ALA during 21 days of culture. The data revealed significant increased amounts in OG (p < 0.05 vs control) and HG (p < 0.001 vs control) (fig. s1B), whereas they were found reduced in ALA treatment (OG vs OG + ALA, p < 0.05; HG vs HG + ALA, p < 0.05).
Discussion
In the present study, we demonstrated that both oscillating glucose and high glucose induce Eng overexpression in ECs and that oxidative stress may be the potential mediator of this effect. Eng modulates the signaling of multiple members of the transforming growth factor-β (TGF-β) superfamily. Several published studies have reported that Eng negatively regulates TGF-β-mediated signaling in quiescent endothelium [27] and is involved in endothelial proliferation in response to an injury [10] and in the inflammation [28]. Recently, increased plasma levels of s-Eng have been associated with diabetic complications in diabetes [12, 29]. In this study, for the first time, we report that high glucose, both constant and oscillating, upregulates Eng expression and sEng release in ECs, suggesting a possible direct link between hyperglycemia and increased sEng in diabetes. Multiple mechanisms have been proposed to explain the release of sEng. Eng is an inducible gene, induced via the activation of KLF-6 and HIF-1 α in response to various factors [7, 16, 30–32]. We confirm that HIF-1α is overexpressed in HG [22], and for the first time, that is increased in OG. KLF-6 is a transcription factor having a crucial role in mediating the transcriptional activation of Eng upon vascular injury in vivo [16, 33]. Our study shows a possible role for KLF-6 in the transcriptional activation of Eng in high glucose, as suggested by its rapid induction within the third hour of glucose exposure. The study of the mRNA kinetics reveals a delay of Eng increase respect to KLF-6 and HIF-1α of about three–six hours. This effect probably is due to specific stimulus to high glucose. Moreover, the data demonstrate that the transcriptional level of Eng is accompanied by an increase in the translocation into the nucleus of KLF-6 after glucose stimuli.
The increase in 8-OHdG confirms the free radicals production in high glucose in ECs [4, 34, 35]. Consistently, we also found an increase in the γ-H2AX, a marker of oxidative stress-induced double-strand breaks [36], and in the histone 2AX, which is a critical DNA sensor that undergoes to phosphorylation on serine 139 upon genotoxic stress [36].
ALA has been shown to be effective in the treatment of several conditions in which oxidative injury is thought to be important, as diabetes [37] and, specifically, in the protection of various cell types exposed to HG and OG [25, 38]. The evidence, in our study, that ALA counterbalances the effects of HG and OG clearly suggests a role of oxidative stress in the described phenomena. These data are consistent with the evidence that reactive oxygen species lead to increased levels of s-Eng via the generation of oxysterols [12] and that previous studies have shown a link between endoglin deficiency and glucose metabolism by which endoglin modulates insulin levels [39].
The dysregulation of antioxidant response and the accumulation of ROS and oxidative damage are a causal factor in the development of several diseases [40]. It is worthy of interest that in both HG and OG, the mRNA and the intracellular protein levels of the antioxidant defenses NQO-1 and HO-1 are not changed respect to control. This is consistent with the report showing that HO-1 is downregulated in an animal model of diabetes [41]. The lack of an efficient defense against the oxidative stress generated by both HG and OG may explain the observed results. Cudmore et al. [42] demonstrated the capability of HO-1 to inhibit s-Eng release from endothelium in mice. It can be hypothesized that, in our study, ALA induces an efficient intracellular increase in both NQO-1 and HO-1, which in turn, protecting endothelial cells, counteracts the induction of Eng and the release of its soluble form.
In conclusion, our data suggest that, during hyperglycemia, oxidative stress is the possible mediator of the ECs damage, leading to the activation of KLF-6 and HIF-1α, which in turn could trans-activate Eng expression. However, the precise role of Eng in vascular complications of diabetes still remains to be elucidated.
References
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107:1058–1070
Ceriello A, Testa R (2009) Antioxidant anti-inflammatory treatment in type 2 diabetes. Diabetes Care 32(Suppl 2):S232–S236
Ceriello A (2010) Hyperglycaemia and the vessel wall: the pathophysiological aspects on the atherosclerotic burden in patients with diabetes. Eur J Cardiovasc Prev Rehabil 17(Suppl 1):S15–S19
Quagliaro L, Piconi L, Assaloni R, Martinelli L, Motz E, Ceriello A (2003) Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes 52:2795–2804
Zhu Y, Sun Y, Xie L, Jin K, Sheibani N, Greenberg DA (2003) Hypoxic induction of endoglin via mitogen-activated protein kinases in mouse brain microvascular endothelial cells. Stroke 34:2483–2488
Bernabeu C, Conley BA, Vary CP (2007) Novel biochemical pathways of endoglin in vascular cell physiology. J Cell Biochem 102:1375–1388
Sánchez-Elsner T, Botella LM, Velasco B, Langa C, Bernabéu C (2002) Endoglin expression is regulated by transcriptional cooperation between the hypoxia and transforming growth factor-beta pathways. J Biol Chem 277:43799–43808
Atkins GB, Jain MK (2007) Role of Krüppel-like transcription factors in endothelial biology. Circ Res 100:1686–1695
Torsney E, Charlton R, Parums D, Collis M, Arthur HM (2002) Inducible expression of human endoglin during inflammation and wound healing in vivo. Inflamm Res 51:464–470
Lopez-Novoa JM, Bernabeu C (2010) The physiological role of endoglin in the cardiovascular system. Am J Physiol Heart Circ Physiol 299:H959–H974
Hawinkels LJ, Kuiper P, Wiercinska E, Verspaget HW, Liu Z, Pardali E, Sier CF, ten Dijke P (2010) Matrix metalloproteinase-14 (MT1-MMP)-mediated endoglin shedding inhibits tumor angiogenesis. Cancer Res 70:4141–4150
Valbuena-Diez AC, Blanco FJ, Oujo B, Langa C, Gonzalez-Nuñez M, Llano E, Pendas AM, Díaz M, Castrillo A, Lopez-Novoa JM, Bernabeu C (2012) Oxysterol-induced soluble endoglin release and its involvement in hypertension. Circulation 126:2612–2624
Kaitu’u-Lino TJ, Palmer KR, Whitehead CL, Williams E, Lappas M, Tong S (2012) MMP-14 is expressed in preeclamptic placentas and mediates release of soluble endoglin. Am J Pathol 180:888–894
Blázquez-Medela AM, García-Ortiz L, Gómez-Marcos MA, Recio-Rodríguez JI, Sánchez-Rodríguez A, López-Novoa JM, Martínez-Salgado C (2010) Increased plasma soluble endoglin levels as an indicator of cardiovascular alterations in hypertensive and diabetic patients. BMC Med 8:86
Qi W, Chen X, Holian J, Tan CY, Kelly DJ, Pollock C (2009) Transcription factors Kruppel-like factor 6 and peroxisome proliferator-activated receptor-{gamma} mediate high glucose-induced thioredoxin-interacting protein. Am J Pathol 175:1858–1867
Botella LM, Sánchez-Elsner T, Sanz-Rodriguez F, Kojima S, Shimada J, Guerrero-Esteo M, Cooreman MP, Ratziu V, Langa C, Vary CP, Ramirez JR, Friedman S, Bernabéu C (2002) Transcriptional activation of endoglin and transforming growth factor-beta signaling components by cooperative interaction between Sp1 and KLF6: their potential role in the response to vascular injury. Blood 100:4001–4010
Cullingford TE, Butler MJ, Marshall AK, el Tham L, Sugden PH, Clerk A (2008) Differential regulation of Krüppel-like factor family transcription factor expression in neonatal rat cardiac myocytes: effects of endothelin-1, oxidative stress and cytokines. Biochim Biophys Acta 178:1229–1236
Stärkel P, Sempoux C, Leclercq I, Herin M, Deby C, Desager JP, Horsmans Y (2003) Oxidative stress, KLF6 and transforming growth factor-beta up-regulation differentiate non-alcoholic steatohepatitis progressing to fibrosis from uncomplicated steatosis in rats. J Hepatol 39:538–546
Holian J, Qi W, Kelly DJ, Zhang Y, Mreich E, Pollock CA, Chen XM (2008) Role of Kruppel-like factor 6 in transforming growth factor-beta1-induced epithelial-mesenchymal transition of proximal tubule cells. Am J Physiol Renal Physiol 295:F1388–F1396
Pan Y, Mansfield KD, Bertozzi CC, Rudenko V, Chan DA, Giaccia AJ, Simon MC (2007) Multiple factors affecting cellular redox status and energy metabolism modulate hypoxia-inducible factor prolyl hydroxylase activity in vivo and in vitro. Mol Cell Biol 27:912–925
Ke Q, Costa M (2006) Hypoxia-inducible factor-1 (HIF-1). Mol Pharmacol 70:1469–1480
Liu Z, Jia X, Duan Y, Xiao H, Sundqvist KG, Permert J, Wang F (2013) Excess glucose induces hypoxia-inducible factor-1α in pancreatic cancer cells and stimulates glucose metabolism and cell migration. Cancer Biol Ther 14:428–435
Wu LL, Chiou CC, Chang PY, Wu JT (2004) Urinary 8-OHdG: a marker of oxidative stress to DNA and a risk factor for cancer, atherosclerosis and diabetics. Clin Chim Acta 339:1–9
Schisano B, Tripathi G, McGee K, McTernan PG, Ceriello A (2011) Glucose oscillations, more than constant high glucose, induce p53 activation and a metabolic memory in human endothelial cells. Diabetologia 54:1219–1226
Ihnat MA, Thorpe JE, Kamat CD, Szabó C, Green DE, Warnke LA, Lacza Z, Cselenyák A, Ross K, Shakir S, Piconi L, Kaltreider RC, Ceriello A (2007) Reactive oxygen species mediate a cellular ‘memory’ of high glucose stress signalling. Diabetologia 50:1523–1531
Shay KP, Moreau RF, Smith EJ, Smith AR, Hagen TM (2009) Alpha-lipoic acid as a dietary supplement: molecular mechanisms and therapeutic potential. Biochim Biophys Acta 1790:1149–1160
Lebrin F, Goumans MJ, Jonker L, Carvalho RL, Valdimarsdottir G, Thorikay M, Mummery C, Arthur HM, ten Dijke P (2004) Endoglin promotes endothelial cell proliferation and TGF-beta/ALK1 signal transduction. EMBO J 23:4018–4028
Rossi E, Sanz-Rodriguez F, Eleno N, Düwell A, Blanco FJ, Langa C, Botella LM, Cabañas C, Lopez-Novoa JM, Bernabeu C (2013) Endothelial endoglin is involved in inflammation: role in leukocyte adhesion and transmigration. Blood 121:403–415
Abu El-Asrar AM, Nawaz MI, Kangave D, Abouammoh M, Mohammad G (2012) High-mobility group box-1 and endothelial cell angiogenic markers in the vitreous from patients with proliferative diabetic retinopathy. Mediators Inflamm 2012:697489
Docherty NG, López-Novoa JM, Arevalo M, Düwel A, Rodriguez-Peña A, Pérez-Barriocanal F, Bernabeu C, Eleno N (2006) Endoglin regulates renal ischaemia-reperfusion injury. Nephrol Dial Transplant 21:2106–2119
Ma X, Labinaz M, Goldstein J, Miller H, Keon WJ, Letarte M, O’Brien E (2000) Endoglin is overexpressed after arterial injury and is required for transforming growth factor-beta-induced inhibition of smooth muscle cell migration. Arterioscler Thromb Vasc Biol 20:2546–2552
van Laake LW, van den Driesche S, Post S, Feijen A, Jansen MA, Driessens MH, Mager JJ, Snijder RJ, Westermann CJ, Doevendans PA, van Echteld CJ, ten Dijke P, Arthur HM, Goumans MJ, Lebrin F, Mummery CL (2006) Endoglin has a crucial role in blood cell-mediated vascular repair. Circulation 114:2288–2297
Suzuki T, Aizawa K, Matsumura T, Nagai R (2005) Vascular implications of the Krüppel-like family of transcription factors. Arterioscler Thromb Vasc Biol 25:1135–1141
Piconi L, Quagliaro L, Assaloni R, Da Ros R, Maier A, Zuodar G, Ceriello A (2006) Constant and intermittent high glucose enhances endothelial cell apoptosis through mitochondrial superoxide overproduction. Diabetes Metab Res Rev 22:198–203
Quagliaro L, Piconi L, Assaloni R, Da Ros R, Szabó C, Ceriello A (2007) Primary role of superoxide anion generation in the cascade of events leading to endothelial dysfunction and damage in high glucose treated HUVEC. Nutr Metab Cardiovasc Dis 17:257–267
Wu CY, Kang HY, Yang WL, Wu J, Jeong YS, Wang J, Chan CH, Lee SW, Zhang X, Lamothe B, Campos AD, Darnay BG, Lin HK (2011) Critical role of monoubiquitination of histone H2AX protein in histone H2AX phosphorylation and DNA damage response. J Biol Chem 286:30806–30815
Packer L, Witt EH, Tritschler HJ (1995) Alpha-lipoic acid as a biological antioxidant. Free Radical Biol Med 19:227–250
Sun LQ, Chen YY, Wang X, Li XJ, Xue B, Qu L, Zhang TT, Mu YM, Lu JM (2012) The protective effect of alpha lipoic acid on Schwann cells exposed to constant or intermittent high glucose. Biochem Pharmacol 84:961–973
Beiroa D, Romero-Picó A, Langa C, Bernabeu C, López M, López-Novoa JM, Nogueiras R, Diéguez C (2013) Heterozygous deficiency of endoglin decreases insulin and hepatic triglyceride levels during high fat diet. PLoS one 8:e54591
Ungvari Z, Bailey-Downs L, Sosnowska D, Gautam T, Koncz P, Losonczy G, Ballabh P, de Cabo R, Sonntag WE, Csiszar A (2011) Vascular oxidative stress in aging: a homeostatic failure due to dysregulation of NRF2-mediated antioxidant response. Am J Physiol Heart Circ Physiol 301:H363–H372
Wang Y, Ying L, Chen YY, Shen YL, Guo R, Jin KK, Wang LX (2014) Induction of heme oxygenase-1 ameliorates vascular dysfunction in streptozotocin-induced type 2 diabetic rats. Vascul Pharmacol 61:16–24
Cudmore M, Ahmad S, Al-Ani B, Fujisawa T, Coxall H, Chudasama K, Devey LR, Wigmore SJ, Abbas A, Hewett PW, Ahmed A (2007) Negative regulation of soluble Flt-1 and soluble endoglin release by heme oxygenase-1. Circulation 115:1789–1797
Conflict of interest
Lucia La Sala, Gemma Pujadas, Valeria De Nigris, Silvia Canivell, Anna Novials, Stefano Genovese, Antonio Ceriello declare that they have no conflict of interest.
Human and animal rights statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Federici.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
La Sala, L., Pujadas, G., De Nigris, V. et al. Oscillating glucose and constant high glucose induce endoglin expression in endothelial cells: the role of oxidative stress. Acta Diabetol 52, 505–512 (2015). https://doi.org/10.1007/s00592-014-0670-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0670-3