Abstract
Aims
Glucagon is used as an emergency drug in hypoglycemia, mainly when the patient is unconscious. A few studies report on ineffectiveness of glucagon in relieving hypoglycemia. The present systematic review and meta-analysis evaluate the effectiveness of glucagon alone and in comparison with dextrose and the effectiveness of intranasal glucagon in comparison with injected glucagon.
Methods
Studies were grouped into three groups: (1) reports on glucagon ineffectiveness; (2) comparison of glucagon and dextrose; (3) comparison of intranasal glucagon and injected glucagon. In groups 2 and 3, only controlled studies were included in the analysis, whether randomized or non-randomized studies. Appropriate methodology (PRISMA statement) was adhered to, and publication bias was formally assessed. Sixteen studies, published in any language as full papers, were analysed to identify predictors of ineffectiveness, and they were included in a meta-analysis (random effects model) to study the effect of different strategies. Intervention effect (number of failures) was expressed as odds ratio (OR), with 95 % confidence intervals.
Results
Failure rate ranged from 0.0 to 2.31 %, to 7.6 %, to 14.4 %, and to 59 %. Comparing glucagon and dextrose, the OR was 0.53 (0.20–1.42); comparing intranasal and intramuscular glucagon, the OR was 1.40 (0.18–10.93). Heterogeneity was low and not statistically significant. Publication bias was absent.
Conclusions
These data indicate that ineffectiveness of glucagon is unfrequent, not different from dextrose; in addition, intranasal and injected glucagon are similarly effective. In the case of failure, a second dose can be administered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glycemic control is crucial for diabetes, as near-normoglycemia prevents or delays microvascular complications and macrovascular events in both type 1 and type 2 diabetes [1–3]. However, hypoglycemia is a common side effect of glucose-lowering therapy, and severe hypoglycemia (SH) is a clinically and economically [4] significant complication in patients receiving insulin [1–3], limiting lifetime maintenance of euglycemia in the vast majority of patients [5].
Approximately, 16–21 % of adults with type 2 diabetes (T2DM) (3.7–5.1 million) are on insulin therapy [6], and 30–60 % of insulin-treated patients have experienced symptoms of hypoglycemia. Hypoglycemia is common for people with type 1 diabetes (T1DM), who suffer an average of two episodes of symptomatic hypoglycemia per week and one episode of SH per year [1, 7]. The frequency of SH is lower in T2DM [6, 8]; the highest incidence of SH is observed in patients with intensive insulin treatment, T1DM or T2DM [9, 10], mainly the elderly [11], with a different risk of hypoglycemia depending on insulin administration regimens [12]. As glucose is an obligate metabolic fuel for the brain [13], prolonged hypoglycemia, if not managed promptly, can cause irreversible cerebral damage, seizure, and coma, and in patients with long-standing diabetes, it may increase cardiovascular and all-cause mortality [1, 4, 14–18].
During the past 10 years, the incidence of T1DM increased on average by 2.5–3 % per year worldwide [19] and so is for the number of patients treated with insulin or insulin plus oral antidiabetic agents [11, 20], and frequency of hypoglycemia is also raising [21].
Current guidelines advise that less stringent glycemic targets may be appropriate for patients with a history of SH in order to minimize the incidence of additional SH events [22].
Episodes of asymptomatic and most episodes of symptomatic hypoglycemia can be effectively self-treated by ingestion of oral carbohydrates [23]; nevertheless, during SH, patients are unable or unwilling to take carbohydrates orally, and therefore require assistance from a third party, through the administration of parenteral glucose or glucagon [13, 22, 24, 25].
Glucagon is a polypeptide produced by the alpha cells in pancreatic islets [26]. Glucagon modulates glycogen breakdown in the liver, and glucose uptake [27], thus increasing plasma glucose concentrations. For this reason, glucagon is critical to the homeostatic role of the liver during everyday life (exercise, fasting, and feeding) [28] and is thought to be the counterregulator of insulin to achieve a balance of plasma glucose concentration [26]. Intravenous (IV), subcutaneous (SC), and intramuscular (IM) glucagon are available for various clinical uses, such as premedication in radiological and endoscopic examinations of the alimentary tract, the insulin stimulation test, the diagnosis for insulinoma, and the glucagon-insulin therapy of fulminant hepatitis; its main use is treatment of mild to severe hypoglycemia. Glucagon, injected by the subcutaneous (SC) or the intramuscular (IM) route, is the treatment of choice for severe hypoglycemia outside of the hospital setting. Clinical studies [29–32] have shown its effectiveness in yielding a predictable rise in plasma glucose in both healthy volunteers and hypoglycemic patients in the pre-hospital and hospital setting. The use of glucagon has been reported to be safe and effective also in diabetic children [33–38], in infants affected by neonatal hypoglycemia non-responsive to IV dextrose infusions [39], and, in association with low-dose octreotide, in preventing hypoglycemic episodes in severe congenital hyperinsulinism [40].
Efficacy of intranasal (IN) glucagon has been proved in the 1980s [41–43], 2 mg of IN glucagon being as effective as 1 mg of IM glucagon [44]; the IN route seems to be a safer method of administration decreasing the hazard of accidental needle sticks and body fluid exposure [45, 46], especially in the emergency setting where an IV access may not always be rapidly achieved and the IM route may not be desirable. Unfortunately, the IN route is not yet commercially available.
While effective in most circumstances, glucagon will not be effective when hepatic glycogen stores are not sufficient (starvation, adrenal insufficiency, and alcoholic hypoglycemia) or when liver function is compromised [47–49]; therefore, efficacy is expected to be reduced when treating episodes of SH that may arise after prolonged exercise or inadequate caloric intake or ethanol abuse.
There are, however, reports indicating that glucagon was not effective, even in the absence of apparent impaired hepatic glycogen stores (Table 1). MacCuish et al. [50] showed that only 41 % of 100 consecutive diabetic patients admitted at the Emergency Department (ED) with insulin-induced SH responded to IM glucagon, and 59 % required treatment with IV glucose to recover. In contrast, Mulhauser et al. [51] reported four cases of failure among 53 diabetic patients treated with IM glucagon in the pre-hospital setting. Similarly, Slama et al. [52] observed a 14 % “non responder” rate among 20 children affected by type 1 diabetes mellitus during incident episodes of severe hypoglycemia; in experiments with a bi-hormonal artificial endocrine pancreas, Castle et al. [53] showed that glucagon administration failed to prevent hypoglycemia in 7 out of 19 episodes in diabetic subjects, and it was observed that circulating insulin levels at the start of glucagon delivery were significantly higher in failures compared to successes. Again, data from the National EMS Information System (NEMSIS) regarding the pre-hospital EMS response to diabetic emergencies in the United States indicated that, in 2011, glucagon was administered 18,483 times in runs listed in the dataset, with 436 times requiring a repeat dose [54]; the Food and Drug Administration (FDA), and Health Canada, reported 82 and 8 failures out of a total of 568 reports from 2011 to 2012 and of 20 reports from 1997 to 2012, respectively [55, 56]. Some authors, comparing IM glucagon to IV dextrose in the pre-hospital settings, showed a delay in recovering from an hypoglycemic event with glucagon [57–60], but with a steady increase in blood glucose [58]; in contrast, dextrose treated patients seemed to have more fluctuations of blood glucose.
The aim of this systematic review and meta-analysis is to evaluate studies reporting on failure of glucagon in relieving hypoglycemia in diabetes mellitus; therefore, we analyzed frequency of failures in any kind of report; in addition, we analyzed frequency of failure of glucagon in comparison with frequency of failure of dextrose; finally, we analyzed frequency of failure of intranasal glucagon in comparison with frequency of failure of glucagon injection (intramuscular, subcutaneous).
Methods
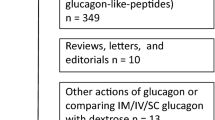
We considered all studies reporting data on glucose effects after IM, IV, and IN glucagon in diabetic patients during hypoglycemia episodes, whatever the duration of the study and the ethnic group, published as full reports in any language up to May 2014. A systematic literature search was conducted using the terms diabetes mellitus, hypoglycemia, insulin-induced hypoglycemia, and glucagon, limiting search to clinical studies and human studies. No exclusion was applied to studies concerning special populations, i.e., children or elderly. Measure of efficacy was the number/percentage of patients/subjects not responding to glucagon according to criteria pre-defined by the authors of each paper. All the data are tabulated in Tables 1 and 2. Sixteen studies fulfilled the inclusion criteria [33, 42, 44, 50–62]. Details of data source and searches, study selection, data extraction and quality assessment, data synthesis, and analysis have already been published [12]. Appropriate methodology according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [12] was adhered to, as shown in flow diagram (Fig. 1).
Flowchart of clinical trials included in the systematic review and meta-analysis; Asterisk most studies were dealing with glucagon-like-peptide 1 or with DPP-4 inhibitors and were excluded first; papers without original data (reviews, meta-analyses, commentaries, and duplicates) were excluded next; finally, studies without quantitative were excluded
For each study, the number of subjects evaluated, the number of subjects with increase in blood glucose (effective), and the number of subjects with no increase of blood glucose (failure), with either glucagon or dextrose, are reported. For each study, the number/percentage of patients/subjects not responding to glucagon was calculated. In studies in which both glucagon and glucose were used, the number/percentage of patients/subjects not responding to glucagon and to glucose was used to process the Forest plot using statistical program Stata 12 (Stata Corporation, College Station, Texas) to assess whether glucagon was more or less effective than glucose in treating hypoglycemia. Intervention effect (failure to respond) was expressed as odds ratio (OR), with 95 % confidence intervals (CIs). In each treatment group, difference in the treatment groups (1 for OR) was expressed as point estimates and 95 % CI. To explore the potential effect of patients or study characteristics on the pooled estimate of failure, a meta-regression analysis was also planned, taking into consideration that, since studies in each strategy were few, the meta-regression was possible only for the whole series of studies. The dependent variable was failure to respond from each study. The role of each covariate in heterogeneity was expressed by Wald test estimated by the meta-regression. The following covariates were considered for the meta-regression analysis: age, number of subjects in the study, and fasting and post-treatment glucose.
Results
Table 2 shows comparative studies reporting any failure of glucagon in relieving hypoglycemia; Table 2A shows studies comparing glucagon and dextrose, and Table 2B shows studies comparing IN glucagon and IM/SC glucagon. Figure 2 shows that the number of subjects failing on glucagon is not significantly different from the number of subjects failing on dextrose; one single study showed superiority of dextrose over glucagon [50], while the other studies showed similar results. Since the single study was highly different from the others, [50] a simulation was made by eliminating this study; Fig. 3 shows that the efficacy of glucagon was clearly not different from dextrose.
Meta-analysis of efficacy of glucagon compared to dextrose in the treatment of hypoglycemia. Vertical line (1) represents no difference in the groups (OR); square and horizontal line represent the point estimates and associated 95 % CI for each comparison; the diamonds represent the pooled effect size, with the center representing the point estimate and the width representing the associated 95 % CI
Figure 4 shows that the number of subjects failing on IN glucagon is not significantly different from the number of subjects failing on IM/SC glucagon. Since out of five studies, only two reported failures, a simulation was made, adding one failure for each arm in the remaining three studies, and again (Fig. 5) there was no difference between IN and IM/SC glucagon. Since heterogeneity was low in all comparisons, and not statistically significant, no meta-regression was performed. Publication bias was at all absent.
Meta-analysis of efficacy of intranasal glucagon compared to intramuscular glucagon in the treatment of hypoglycemia. Legend as in Fig. 2
Discussion
From available evidence, even with limitations such as the heterogeneity of data obtained in a variety of conditions that span from controlled studies to registries, it would appear that lack of efficacy of glucagon has to be considered. Its real frequency, according to the above reports, seems to vary from 0.0 to 2.31 %, to 7.6 %, to 14.4 %, and to percentages as high as 59 % (one study) [50]. With such a heterogeneity of sources of information and with such a discrepancy in its frequency, we can only state that lack of efficacy should be kept in mind when IM, IV, SC, and IN glucagon are administered; in other terms, one could consider to administer a second dose if other remedies are not at hand. This is reflected in the product labeling for currently available injectable glucagon; in the United States it recommends giving a second dose of glucagon and informing emergency services if the patient does not respond within 15 minutes, while in Canada and Europe it recommends administration of IV glucose if the patient does not respond within 10 minutes after injecting glucagon. Also, the reasons for these discrepancies are far from being ascertained; one study was clearly different from the others, and the high rate of inefficacy of glucagon, together with the high rate of inefficiency of dextrose, suggests some form of design flaws. In addition, even though the majority of studies were performed under standardized conditions, an error in administrations can not be ruled out. Intuitively, circulating insulin levels may be of importance, and this has been shown in ad hoc experiments, in which insulin levels had been artificially raised [53, 63]; also, glucagon can be less effective in type 2 diabetes than in type 1 diabetes simply because glucagon also stimulates insulin release, especially if a subject with type 2 diabetes is on sulfonylurea therapy [8]. For the same reason, a superiority of dextrose over glucagon would be expected in treating patients with severe insulin-induced hypoglycemia, as reported by some authors [58–60], suggesting that glucagon may be preferable in non-critical subjects and when an IV line is unavailable; nevertheless as suggested by some authors, since glucagon requires endogenous glucose, it is likely to produce a more predictable rise of blood glucose levels than when large amount of IV glucose is used, avoiding hyperglycemic rebounds [58]. Moreover, in several cases, multiple glucagon injections have been reported to be effective in managing hypoglycemic patients in a pre-hospital setting; for instance, Haymond et al. [38] showed an increase of blood glucose in 14 children non-responsive to a first administration of glucagon, after a second or a third injection. This is reminiscent of what has been observed for adrenaline in asthma children; when a first dose does not work, it is likely that a second dose might work [64].
The crucial question remains: is dextrose superior to glucagon? Table 2 and Fig. 2 show that, even considering the study by McCuish [50], the effect is not statistically different clearly indicating that glucagon and dextrose are similar in their effect in raising blood glucose levels. However, injection of glucagon is not an easy maneuver; it has been reported that relatives or caregivers can be too anxious to inject, or that they do not know how to proceed [51]. From this standpoint, IN glucagon might be a progress in overcoming hypoglycemia, easy to administer either as a self-treatment or given by a relative or caregiver.
References
The Diabetes Control and Complications Trial Research Group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
The United Kingdom Prospective Diabetes Study Research Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 352:837–853
Lithovius R, Harjutsalo V, Forsblom C, Saraheimo M, Groop P-H (2014) The consequences of failure to achieve targets of guidelines for prevention and treatment of diabetic complications in patients with type 1 diabetes. Acta Diabetol. doi:10.1007/s00592-014-0595-x
Allicar MP, Mégas F, Houzard S, Baroux A, Le Thai F, Augendre-Ferrante B (2000) Frequency and costs of hospital stays for hypoglycemia in France in 1995. Presse Med 29:657–661
Cryer PE (2002) Hypoglycaemia: the limiting factor in the glycaemic management of Type I and Type II diabetes. Diabetologia 45:937–948
Centers for Disease Control and Prevention (CDC) (2011) National diabetes fact sheet: national estimates, general information on diabetes, prediabetes in the United States, 2011. US Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, GA
MacLeod KM, Hepburn DA, Frier BM (1993) Frequency and morbidity of severe hypoglycaemia in insulin-treated diabetic patients. Diabet Med 10:238–245
Cryer PE, Davis SN, Shamoon H (2003) Hypoglycemia in diabetes. Diabetes Care 26:1902–1912
UK Hypoglycemia Study Group (2007) Risk of hypoglycemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 50:1140–1147
Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W, Frier BM, Morris AD, DARTS/MEMO Collaboration (2003) Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care 26:1176–1180
Geller AI, Shehab N, Lovegrove MC, Kegler SR, Weidenbach KN, Ryan GJ, Budnitz DS (2014) National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med 174:678–686
Merlotti C, Morabito A, Ceriani V, Pontiroli AE (2014) Prevention of type 2 diabetes in obese at-risk subjects: a systematic review and meta-analysis. Acta Diabetol 51:853–863
Cryer PE (1997) Hypoglycemia. Pathophysiology, diagnosis and treatment. Oxford Univ. Press, New York
Gossain VV, Carella MJ, Rovner DR (1994) Management of diabetes in the elderly: a clinical perspective. J Assoc Acad Minor Phys 5:22–31
Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, DE Grobbee, Kengne AP, Marre M, Heller S, ADVANCE Collaborative Group (2010) Severe hypoglycemia and risks of vascular events and death. N Engl J Med 363:1410–1418
Miller CD, Phillips LS, Ziemer DC, Gallina DL, Cook CB, El-Kebbi IM (2001) Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med 161:1653–1659
Socransky SJ, Pirrallo RG, Rubin JM (1998) Out-of-hospital treatment of hypoglycemia: refusal of transport and patient outcome. Acad Emerg Med 5:1080–1085
Lobmann R, Smid HG, Pottag G, Wagner K, Heinze HJ, Lehnert H (2000) Impairment and recovery of elementary cognitive function induced by hypoglycemia in type-1 diabetic patients and healthy controls. J Clin Endocrinol Metab 85:2758–2766
DIAMOND Project Group (2006) Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet Med 23:857–866
Köster I, Huppertz E, Hauner H, Schubert I (2011) Direct costs of diabetes mellitus in Germany—CoDiM 2000–2007. Exp Clin Endocrinol Diabetes 119:377–385
Holstein A, Patzer OM, Machalke K, Holstein JD, Stumvoll M, Kovacs P (2012) Substantial increase in incidence of severe hypoglycemia between 1997–2000 and 2007–2010: a German longitudinal population-based study. Diabetes Care 35:972–975
American Diabetes Association (2013) Standards of medical care in diabetes–diabetes—2013. Diabetes Care 36(Suppl 1):S11–S66
Zammitt NN, Frier BM (2005) Hypoglycemia in type 2 diabetes: pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care 28:2948–2961
Guettier JM, Gorden P (2006) Hypoglycemia. Endocrinol Metab Clin North Am 35:753–766
Kearney T, Dang C (2007) Diabetic and endocrine emergencies. Postgrad Med J 83:79–86
Barret KE, Barman SM (2010) Endocrine functions of the pancreas and regulation of carbohydrate metabolism. Ganong’s Review of Medical Physiology, 23rd edn. McGraw-Hill, New York, pp 315–336
Holste LC, Connolly CC, Moore MC, Neal DW, Cherrington AD (1997) Physiological changes in circulating glucagon alter hepatic glucose disposition during portal glucose delivery. Am J Physiol 273:488–496
Ramnanan CJ, Edgerton DS, Kraft G, Cherrington AD (2011) Physiologic action of glucagon on liver glucose metabolism. Diabetes Obes Metab 13(Suppl 1):118–125
Elrick H, Witten TA, Arai Y (1958) Glucagon treatment of insulin reactions. N Engl J Med 258:476–480
Vukmir RB, Paris PM, Yealy DM (1991) Glucagon: pre-hospital therapy for hypoglycemia. Ann Emerg Med 20:375–379
Mühlhauser I, Koch J, Berger M (1985) Pharmacokinetics and bioavailability of injected glucagon: differences between intramuscular, subcutaneous, and intravenous administration. Diabetes Care 8:39–42
Namba M, Hanafusa T, Kono N, Tarui S (1993) Clinical evaluation of biosynthetic glucagon treatment for recovery from hypoglycemia developed in diabetic patients. The GL-G Hypoglycemia Study Group. Diabetes Res Clin Pract 19:133–138
Shipp JC, Delcher HK, Munroe JF (1964) Treatment of insulin hypoglycemia in diabetic campers; a comparison of glucagon (1 and 2 mg.) and glucose. Diabetes 13:645–648
Gibbs GE, Ebers DW, Meckel BR (1958) Use of glucagon to terminate insulin reactions in diabetic children. Nebr State Med J 43:56–57
Cornblath M, Levin EY, Marquetti E (1958) Studies of carbohydrate metabolism in the newborn. II. The effect of glucagon on the concentration of sugar in capillary blood of the newborn infant. Pediatrics 21:885–892
Carson MJ, Koch R (1955) Clinical studies with glucagon in children. J Pediatr 47:161–170
Aman J, Wranne L (1988) Hypoglycaemia in childhood diabetes. II. Effect of subcutaneous or intramuscular injection of different doses of glucagon. Acta Paediatr Scand. 77:548–553
Haymond MW, Schreiner B (2001) Mini-dose glucagon rescue for hypoglycemia in children with type 1 diabetes. Diabetes Care 24:643–645
Miralles RE, Lodha A, Perlman M, Moore AM (2002) Experience with intravenous glucagon infusions as a treatment for resistant neonatal hypoglycemia. Arch Pediatr Adolesc Med 156:999–1004
Mohnike K, Blankenstein O, Pfuetzner A, Pötzsch S, Schober E, Steiner S, Hardy OT, Grimberg A, van Waarde WM (2008) Long-term non-surgical therapy of severe persistent congenital hyperinsulinism with glucagon. Horm Res 70:59–64
Pontiroli AE, Alberetto M, Pozza G (1983) Intranasal glucagon raises blood glucose concentrations in healthy volunteers. Br Med J (Clin Res Ed) 287:462–463
Pontiroli AE, Calderara A, Pajetta E, Alberetto M, Pozza G (1989) Intranasal glucagon as remedy for hypoglycemia. Studies in healthy subjects and type I diabetic patients. Diabetes Care 12:604–608
Freychet L, Rizkalla SW, Desplanque N, Basdevant A, Zirinis P, Tchobroutsky G, Slama G (1988) Effect of intranasal glucagon on blood glucose levels in healthy subjects and hypoglycaemic patients with insulin-dependent diabetes. Lancet. 1:1364–1366
Rosenfalck AM, Bendtson I, Jorgensen S, Binder C (1992) Nasal glucagon in the treatment of hypoglycaemia in type 1 (insulin-dependent) diabetic patients. Diabetes Res Clin Pract 17:43–50
Wolfe T, Barton E (2003) Nasal drug delivery in EMS: reducing needlestick risk. JEMS 28:52–63
Costantino HR, Illum L, Brandt G, Johnson PH, Quay SC (2007) Intranasal delivery: physicochemical and therapeutic aspects. Int J Pharm 337:1–24
Hall-Boyer K, Zaloga GP, Chernow B (1984) Glucagon: hormone or therapeutic agent? Crit Care Med 12:584–589
Lee H, Hosein EA (1982) Chronic alcohol feeding and its withdrawal on the structure and function of the rat liver plasma membrane: a study with 125I-labelled glucagon binding as a metabolic probe. Can J Physiol Pharmacol 60:1171–1176
American Medical Association, Council on Drugs (1994) AMA Drug Evaluations Annual 1994. American Medical Association, Chicago, IL, p 1045
MacCuish AC, Munro JF, Duncan LJ (1970) Treatment of hypoglycaemic coma with glucagon, intravenous dextrose, and mannitol infusion in a hundred diabetics. Lancet 2:946–949
Muhlhauser I, Berger M, Sonnenberg G, Koch J, Jorgens V, Schernthaner G, Scholz V, Padagogin D (1985) Incidence and management of severe hypoglycemia in 434 adults with insulin-dependent diabetes mellitus. Diabetes Care 8:268–273
Slama G, Reach G, Cahane M, Quetin C, Villanove-Robin F (1992) Intranasal glucagon in the treatment of hypoglycaemic attacks in children: experience at a summer camp. Diabetologia 35:398
Castle JR, Engle JM, El Youssef J, Massoud RG, Ward WK (2010) Factors influencing the effectiveness of glucagon for preventing hypoglycemia. J Diabetes Sci Technol 4:1305–1310
National EMS Information System (NEMSIS) 2011 Public Release Dataset. http://nemsis.org
AEs reported to FDA from ‘11/09 to ‘12/12. http://adverseevent.com
AEs reported to Health Canada from ‘97 to ‘12. http://adverseevent.com
Carstens S, Sprehn M (1998) Prehospital treatment of severe hypoglycaemia: a comparison of intramuscular glucagon and intravenous glucose. Prehosp Disaster Med 13:44–50
Howell MA, Guly HR (1997) A comparison of glucagon and glucose in prehospital hypoglycaemia. J Accid Emerg Med 14:30–32
Collier A, Steedman DJ, Patrick AW, Nimmo GR, Matthews DM, MacIntyre CC, Little K, Clarke BF (1987) Comparison of intravenous glucagon and dextrose in treatment of severe hypoglycemia in an accident and emergency department. Diabetes Care 10:712–715
Patrick AW, Collier A, Hepburn DA, Steedman DJ, Clarke BF, Robertson C (1990) Comparison of intramuscular glucagon and intravenous dextrose in the treatment of hypoglycaemic coma in an accident and emergency department. Arch Emerg Med 7:73–77
Stenninger E, Aman J (1993) Intranasal glucagon treatment relieves hypoglycaemia in children with type 1 (insulin-dependent) diabetes mellitus. Diabetologia 36:931–935
Slama G, Alamowitch C, Desplanque N, Letanoux M, Zirinis P (1990) A new non-invasive method for treating insulin-reaction: intranasal lyophylized glucagon. Diabetologia 33:671–674
El Youssef J, Castle JR, Bakhtiani PA, Haidar A, Branigan DL, Breen M, Ward WK (2014) Quantification of the glycemic response to microdoses of subcutaneous glucagon at varying insulin levels. Diabetes Care. doi:10.2337/dc14-0803
Rudders SA, Banerji A, Corel B, Clark S, Camargo CA Jr (2010) Multicenter study of repeat epinephrine treatments for food-related anaphylaxis. Pediatrics 125:e711–e718
Acknowledgments
The authors wish to acknowledge an unrestricted grant from Locemia Solutions ULC (Dalton-Montreal, Canada).
Conflict of interest
Augusto Boido and Valerio Ceriani declare that they have no conflict of interest. A.E.P. is a member of the Medical Advisory Board for Locemia Solutions ULC (Dalton-Montreal, Canada).
Human and animal rights disclosures
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Antonio Secchi.
Rights and permissions
About this article
Cite this article
Boido, A., Ceriani, V. & Pontiroli, A.E. Glucagon for hypoglycemic episodes in insulin-treated diabetic patients: a systematic review and meta-analysis with a comparison of glucagon with dextrose and of different glucagon formulations. Acta Diabetol 52, 405–412 (2015). https://doi.org/10.1007/s00592-014-0665-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0665-0