Abstract
Aims
Two recent randomized controlled trials of type 2 diabetes mellitus (T2DM) patients with history of, or at high risk of, cardiovascular disease (CVD) showed no risk of ischemic cardiovascular events associated with dipeptidyl peptidase-4 inhibitors (DPP4i), but an increased risk of heart failure (HF) with saxagliptin. We evaluated the risk of CVD including myocardial infarction (MI), stroke, coronary revascularization, and HF associated with DPP4i in T2DM patients with and without baseline CVD as used in the community.
Methods
Using US commercial insurance claims data (2005–2012), we conducted a cohort study that included initiators of DPP4i and non-DPP4i treatments. Composite CVD endpoints including MI, stroke, coronary revascularization, and HF were defined with a hospital discharge diagnosis or procedure code. Cox proportional hazards models compared the risk of composite and individual CVD endpoints in propensity score (PS)-matched initiators of DPP4 versus non-DPP4i.
Results
We included 79,538 (18 % with baseline CVD) persons in PS-matched pairs of DPP4i and non-DPP4i initiators. The incidence rate per 1,000 person-years for composite CVD was 30.30 (95 % CI 28.24–32.51) in DPP4i and 34.76 (95 % CI 32.34–37.36) in non-DPP4i. The PS-matched hazard ratio (HR) for composite CVD was 0.87 (95 % CI 0.79–0.96) in DPP4i versus non-DPP4i. The PS-matched HR for HF was 0.81 (95 % CI 0.70–0.94) in DPP4i versus non-DPP4i. Among patients with baseline CVD, there was no increased risk of CVD or HF associated with DPP4i use.
Conclusions
Among T2DM patients, initiating DPP4i was not associated with a greater risk of CVD or HF compared to non-DPP4i initiators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Dipeptidyl peptidase-4 inhibitors (DPP4i), such as alogliptin, sitagliptin, saxagliptin, and linagliptin, are newly available glucose-lowering drugs that can be used as monotherapy or combination therapy with other oral hypoglycemic agents for treating type 2 diabetes mellitus (T2DM) [1–5]. While a potential risk of acute pancreatitis related to use of DPP4i was suggested, more recent data do not find such risk [6, 7]. These drugs are otherwise generally well tolerated with limited specific contraindication.
It is well known that T2DM is a major risk factor for cardiovascular disease including coronary heart disease, cardiomyopathy, and stroke [8–10]. Recently, two large randomized controlled trials (RCT) in T2DM patients who had a history of, or were at risk of, cardiovascular events at baseline showed no excess risk of ischemic cardiovascular events associated with saxagliptin use for a median follow-up time of 2.1 years or alogliptin use for a median follow-up time of 1.5 years [11, 12]. However, an increased risk of hospitalization for heart failure (HF) was observed in the saxagliptin group, and a trend of similar magnitude, albeit not statistically significant, in the smaller RCT of alogliptin [11–13]. Another RCT showed a significantly decreased risk of major cardiovascular events in linagliptin users compared to glimepiride in T2DM patients inadequately controlled on metformin [4].
The objectives of this study were to evaluate the risk of composite CVD including MI, stroke, coronary revascularization, and HF associated with initiation of DPP4i compared to initiation of other diabetes drugs in ‘real-world’ patients with and without baseline CVD, to determine the risk of CVD associated with initiation of DPP4i versus non-DPP4i in patients with baseline diagnosis of CVD and to examine the risk of HF associated with initiation of DPP4i versus initiation of other diabetes drugs in patients with and without established CVD.
Methods
Data source
We conducted a cohort study using the claims data for the period January 1, 2005 to December 31, 2012, from United HealthCare, a commercial US health plan, which insures primarily working adults and their family members. This database contains longitudinal claims information including medical diagnoses, procedures, hospitalizations, physician visits, and pharmacy dispensing on its approximately 14 million subscribers across the USA on a yearly basis. Patient informed consent was not required as the dataset was de-identified to protect subject confidentiality. The study protocol was approved by the Institutional Review Board of the Brigham and Women’s Hospital.
Study cohort
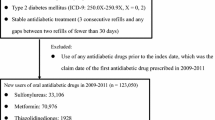
Patients who had ≥1 dispensing for an oral hypoglycemic agent any time during the study period with a visit coded with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD 9-CM) code, 250.xx, for DM were first identified for the study cohort. To avoid selecting patients with type 1 diabetes, we excluded patients aged <40 years and those who used insulin. Two mutually exclusive exposure groups were defined: (1) initiators of DPP4i monotherapy or combotherapy and (2) initiators of non-DPP4i monotherapy or combotherapy. For combotherapy, patients were required to have metformin plus a DPP4i or a non-DPP4i, as metformin is recommended as first-line therapy [14] and to exclude imbalance for renal disease where metformin would be relatively contraindicated. DPP4i drugs include linagliptin (approved in 2011), saxagliptin (approved in 2009), and sitagliptin (approved in 2006), as these are FDA approved and marketed in the USA at the time of study. Non-DPP4i drugs include metformin, sulfonylureas, thiazolidinediones (TZD), and meglitinides.
For monotherapy initiators, the index date was the first dispensing of a DPP4i or a non-DPP4i drug. For combotherapy initiators, the index date was defined as the earliest date of starting a DPP4i drug with concurrent use of metformin for the DPP4i group and the earliest date of adding a second non-DPP4i drug with concurrent use of metformin for the non-DPP4i group. All patients (monotherapy- and combination therapy initiators) were required to be naïve to DPP4i in the 180 days prior to the index date. For non-DPP4i combotherapy initiators, patients were required to have ≥180 days without using multiple oral hypoglycemic drugs prior to their index date. Furthermore, patients were required to have ≥365 days of continuous insurance enrollment before the index date. Patients with and without CVD at baseline were included. Patients with end-stage renal disease, renal transplantation, HIV, cancer, and use of glucagon-like peptide 1 agonists in the 365 days prior to the index date were excluded.
For a subgroup analysis, we selected DPP4i and TZD initiators who were naïve to both DPP4i and TZD in the 180 days prior to the index date. The TZD group was chosen based on the known risk of HF associated with TZD [15].
Follow-up began on the day after the index date. Patients were followed up to the first of any of the following censoring events: discontinuation or switching of study drugs (i.e., ‘as treated’), occurrence of CVD events (any CVD events for the composite endpoint and separately for the individual components of CVD), disenrollment from the health plan, December 31, 2012, or death. Patients were allowed to have gaps of up to 30 days between prescription fill dates in the calculation of continuous therapy. In the case of drug discontinuation or switching, the exposure risk window for each patient treatment episode extended until 30 days after the expiration of the supply of the last fill. Patients were only allowed to enter the study cohort once.
Study outcome
The primary outcome was a composite CVD endpoint including non-fatal MI, non-fatal stroke, coronary revascularization, and HF, defined with a hospital discharge diagnosis and/or procedure code. The secondary outcomes were the individual components of the primary endpoint and all-cause death. In prior studies, the positive predictive values of these claim-based algorithms for CVD events were at least 80 % [16–19]. Hospital admission or procedure dates were used as the date of outcome occurrence. To capture patients with HF not requiring a hospitalization, we also assessed incident use of loop diuretics as an outpatient.
Covariates
Variables potentially related to development of CVD were assessed using data from the 365-day baseline period before the index date. These baseline variables (see Table 1) were age, sex, year of the index date, DM-related comorbidities, CVD, other comorbidities, medications, and healthcare utilization factors, and laboratory test ordered for serum BUN, creatinine, and HbA1c. To further quantify patients’ comorbidities at baseline, we also calculated a comorbidity score that combined 20 medical conditions included in both the Charlson Index and the Elixhauser system based on ICD-9 [20]. To characterize diabetes treatment intensity, the number of oral hypoglycemic drugs taken at the index date was also determined. Baseline serum BUN, creatinine, and HbA1c levels were available in a subgroup of the study cohort.
Statistical analysis
We compared the baseline characteristics between DPP4i and non-DPP4i groups. To control for potential confounders, we used the propensity score (PS)-matching method [21]. Multivariable logistic regression including all the baseline covariates listed in Table 1 was used to estimate the PS, defined as the predicted probability of a patient receiving therapy with DPP4i versus non-DPP4i. For PS-matched analysis, we used nearest neighbor matching without replacement within a ‘caliper’ of 0.025 on the PS at a fixed ratio of 1:1 [22, 23]. Matching was stratified on two factors: baseline CVD (yes/no) and monotherapy (yes/no) so that, for example, a DPP4i combotherapy initiator with baseline CVD was matched to a non-DPP4i combotherapy initiator with baseline CVD. Incidence rates and hazard ratio (HR) of CVD outcomes with 95 % confidence intervals (CI) were calculated in DPP4i initiators versus non-DPP4i. Kaplan–Meier curves were plotted for the cumulative incidence of each outcome in the PS-matched DPP4i and non-DPP4i cohorts. Among patients with baseline CVD, separate incidence rates and HR of CVD outcomes with 95 % CI were calculated.
In patients with no loop diuretics at baseline, separate incidence rates and HRs of receiving a new prescription for loop diuretics with 95 % CI were calculated in DPP4i initiators versus their PS-matched non-DPP4i initiators. All these analyses were repeated for the subgroup analyses comparing DPP4i versus TZD initiators. Additional subgroup analysis compared initiators of DPP4i monotherapy to initiators of non-DPP4i monotherapy. The proportional hazards assumption was assessed by testing the significance of the interaction term between exposure and time and was not violated [24]. All analyses were done using SAS 9.2 Statistical Software (SAS Institute Inc., Cary, NC).
Results
Cohort selection
There were 4,353,160 dispensings for DPP4i or non-DPP4i drugs between 2006 and 2012 in the study database. After applying the inclusion and exclusion criteria, there were 43,583 patients with T2DM who started DPP4i monotherapy or combotherapy and 370,245 who started non-DPP4i monotherapy or combotherapy. Matching on PS with a 1:1 ratio further selected a total of 79,538 individuals as 39,769 pairs of DPP4i and non-DPP4i initiators (eFigure 1).
Patient characteristics
The mean age of the PS-matched patients was 55.5 years. In total, 57 % of the DPP4i group and 58 % of the non-DPP4i group were male (Table 1). Of the DPP4i group, 83 % were on sitagliptin, 15 % on saxagliptin, and 3 % on linagliptin. In total, 82 % were combotherapy users and 18 % had established cardiovascular disease at baseline. Overall, baseline characteristics were well balanced in the PS-matched DPP4i and non-DPP4i groups. The mean (SD) follow-up was 0.7 (0.8) years for DPP4i and 0.5 (0.7) years for non-DPP4i initiators. The median follow-up was 0.3 years for both groups with 42,628 individuals with over 0.3 years of follow-up. Of these, 13,297 individuals had over 1 year of follow-up. The majority of patients were censored due to drug discontinuation (71 %), followed by disenrollment (16 %) and the end of study period (11 %).
Risk of CVD in T2DM with and without baseline CVD
During the follow-up period, 775 composite CVD events occurred with 25,578 person-years of follow-up in DPP4i initiators and 740 composite CVD events with 21,291 person-years of follow-up in non-DPP4i initiators. The incidence rate for composite CVD was 30.3 per 1,000 person-years in the DPP4i group and 34.8 per 1,000 person-years in the non-DPP4i group. The incidence rate for HF was 12.8 per 1,000 person-years in the DPP4i group and 15.9 per 1,000 person-years in the non-DPP4i group. Incidence rates for other individual CVD endpoints were slightly higher in the non-DPP4i compared to DPP4i initiators. The PS-matched HR of DPP4i compared to non-DPP4i was 0.87 (95 % CI 0.79–0.96) for composite CVD and 0.81 (95 % CI 0.70–0.94) for HF. No significant association between DPP4i and the components of the composite CVD endpoint, including MI, coronary revascularization, and stroke, was noted (Table 2). Figures 1 and 2 display the Kaplan–Meier curves comparing the cumulative incidence of composite CVD between the PS-matched DPP4i and non-DPP4i groups.
Risk of CVD in T2DM with baseline CVD
Among 14,586 individuals contributing to 7,293 PS-matched pairs of DPP4i and non-DPP4i initiators who had baseline CVD, the incidence rates of all the CVD endpoints were higher compared to those in the overall study population (Table 3). The HR of DPP4i compared to the PS-matched non-DPP4i initiators was 0.88 (95 % CI 0.77–1.01) for composite CVD and 0.84 (95 % CI 0.70–1.01) for HF. The risk of other CVD endpoints was not significantly different for DPP4i compared to non-DPP4i initiators. Among 28,922 PS-matched pairs of DPP4i and non-DPP4i initiators with no baseline use of loop diuretics, 400 DPP4i and 464 non-DPP4i initiators received a new prescription for loop diuretics during the follow-up. The risk of getting a new prescription for loop diuretics was lower in DPP4i initiators compared to non-DPP4i (HR 0.74, 95 % CI 0.65–0.84).
Subgroup analysis
In the subgroup analysis comparing 21,068 DPP4i initiators to their PS-matched TZD initiators (eTable 1), HR of DPP4i was 0.93 (95 % CI 0.81–1.07) for composite CVD and 0.82 (95 % CI 0.66–1.02) for HF (eTable 2). Among 3,592 PS-matched pairs of DPP4i and TZD subgroup patients with baseline CVD, the HR of DPP4i initiators versus TZD was 0.97 (95 % CI 0.80–1.17) for composite CVD and 1.01 (95 % CI 0.77–1.34) for HF. Among the DPP4i and TZD subgroup patients who had no baseline use of loop diuretics (n = 16,222 pairs), the risk of getting a new prescription for loop diuretics was lower in DPP4i initiators compared to TZD (HR 0.59, 95 % CI 0.50–0.69). Among the initiators of DPP4i monotherapy with baseline CVD (n = 1,720 pairs), the HR was 0.85 (95 % CI 0.66–1.09) for composite CVD and 0.88 (95 % CI 0.65–1.19) for HF. Among the initiators of DPP4i monotherapy without baseline CVD (n = 5,630 pairs), the HR was 0.99 (95 % CI 0.69–1.43) for composite CVD and 0.92 (95 % CI 0.50–1.67) for HF.
Discussion
In this large cohort of T2DM patients, initiating DPP4i was not associated with an increased risk of CVD or its components including HF compared with those initiating non-DPP4i anti-diabetic drugs. In fact, we found a modestly lower risk of composite CVD and HF among DPP4i initiators compared with non-DPP4i initiators. Even among patients with established CVD, the risks of composite CVD or HF were not higher in DPP4i initiators. Subgroup analysis comparing DPP4i to TZD showed a decreased, albeit not statistically significant, risk of HF. Furthermore, the risk of being newly prescribed loop diuretics was significantly lower in DPP4i compared with TZD initiators as expected given the association of TZD with fluid retention and HF.
This study cohort consists of ‘real-world’ patients on either monotherapy or combotherapy of oral anti-diabetic drugs. Our finding of no increased CVD risk in DPP4i initiators as used in the community is consistent with RCT data on linagliptin, saxagliptin, and alogliptin [4, 11, 12, 25]. Compared to glimepiride, linagliptin reduced the risk of cardiovascular death, MI, stroke, or hospitalization for unstable angina (relative risk 0.46, 95 % CI 0.23–0.91) in T2DM patients free of recent CVD events. In an RCT of saxagliptin versus placebo that included 16,492 T2DM patients with a history of CVD or multiple cardiovascular risk factors at baseline, saxagliptin did not increase or decrease the risk of cardiovascular death, MI, or ischemic stroke (HR 1.00, 95 % CI 0.89–1.12) [11]. The risk of the secondary endpoint in this trial—cardiovascular death, MI, stroke, hospitalization for unstable angina, coronary revascularization, or HF—was also not higher (HR 1.02, 95 % CI 0.94–1.11) with saxagliptin. Another recent RCT of alogliptin included 5,380 T2DM patients with acute coronary syndrome of recent onset did not find a higher risk of cardiovascular death, MI, or stroke in the alogliptin group compared to placebo [12]. A pooled analysis of 11 RCTs of alogliptin versus placebo also did not find an increased CVD risk including HF [25].
An unexpected observation in the Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus–Thrombolysis in Myocardial Infarction 53 (SAVOR-TIMI 53) trial was a higher risk of hospitalization for HF (HR 1.27, 95 % CI 107–1.51) [11]. A smaller trial of alogliptin also noted a nonsignificant increase in the risk of HF in patients on active therapy (HR 1.19, 95 % CI 0.90–1.58) [11, 13]. The mechanism by which saxagliptin or alogliptin might increase the rates of HF is not known. Vildagliptin, only in Europe, increased left ventricle end-diastolic volume and left ventricle end-systolic volume, as well as stroke volume in an RCT setting, but did not alter ejection fraction [26]. B-type natriuretic peptides, which play key physiologic roles in the regulation of renal sodium and fluid balance, are cleaved by DPP4 in plasma. Some investigators have hypothesized that the disruption of this neurohormonal regulatory mechanism may be one explanation for the observation of increased HF in patients on saxagliptin in SAVOR-TIMI 53 [27]. We did not observe a higher risk of hospitalization for HF or incident use of diuretics in initiators of DPP4i therapy. This discrepancy could be explained by several differences between our study and the SAVOR-TIMI 53 trial. First, our study had a shorter follow-up time and included sitagliptin and linagliptin as well as saxagliptin. Second, the mean age of our patients is younger than that in the SAVOR-TIMI 53 cohort (55.4 vs. 65.1 years, respectively). Third, the severity of T2DM and CVD risk in our cohort might be lower compared to the SAVOR-TIMI 53 cohort. We included patients with and without baseline CVD, but performed an a priori secondary analysis on patients that appeared similar to the SAVOR-TIMI 53 study cohort. Additionally, we excluded patients with insulin use at baseline in order to exclude all potential type 1 diabetic patients. Fourth, a treating physician’s threshold for admitting a patient for HF might be different when a patient is enrolled in an RCT even if blinded to the treatment assignment.
This present study also makes important contributions to our understanding of challenges in evaluating comparative cardiovascular safety of anti-diabetic medications for T2DM using observational data. As seen in a relatively short period of follow-up in this study, patients’ adherence to medication was generally suboptimal and switching to a new drug or adding a new drug for T2DM was common. Second, even though we used rigorous pharmacoepidemiologic approaches in the study design and analysis including a new-user design, active comparator, and PS-matched analysis to simultaneously account for more than 45 potential confounders [21, 28, 29], residual confounding can still be an issue as in any observational studies. For example, in attempt to use TZD as ‘a positive control’ based on the known risk of HF in TZD users, we conducted a subgroup analysis comparing DPP4i to TZD initiators. There was a lower, albeit not statistically significant, risk of HF and a significantly lower risk of incident use of loop diuretics in DPP4i initiators compared to TZD. However, it is important to note that the observed risk of CVD or HF related to use of TZD in our cohort is likely underestimated as physicians correctly do not prescribe TZD to those with or at increased risk of HF. Similarly, if prescribing physicians were uncertain about cardiovascular safety of DPP4i and therefore more careful upon selecting patients for DPP4i compared to non-DPP4i, it is possible that our study underestimates the risk of CVD and HF associated with DPP4i. Finally, if risk of HF occurs with DPP4i in similar magnitude to TZD, then no increased risk with TZD would be observed, as seen in our analysis.
This study has limitations. First, the primary outcome of a composite CVD endpoint does not include cardiovascular deaths, as the causes of death are not available in the study database. Second, no data were available on race, ethnicity, socioeconomic status, duration of diabetes, family history of CVD, physical activity, dietary factors, and body mass index. Third, even though we used previously validated claim-based algorithms to define CVD outcomes with a positive predictive value at least 84 % [16–19], there is a potential for outcome misclassification. It is also possible that we did not capture mild HF treated as an outpatient because HF outcomes were based on inpatient diagnoses. However, in a subgroup analysis, DPP4i was associated with a decreased risk of incident use of loop diuretics during the follow-up (HR 0.74, 95 % CI 0.65–0.84) versus non-DPP4i. Fourth, as the mean follow-up time was relatively short mainly due to drug discontinuation in the study cohort, the long-term effect of DPP4i could not be assessed reliably. Reasons for drug discontinuation were not available in the study database. However, this study still includes 13,297 patients with at least 1 year of follow-up on treatment. Fifth, our results may not be generalizable to patients with different insurance types or no insurance coverage as having a commercial health insurance is likely related to patients’ socioeconomic status, medication adherence, and other risk factors for CVD. It is, however, unlikely the biological effect of DPP4i on CVD differs by the insurance status. Lastly, we assessed a number of potential confounders using the claims data from the 12 months prior to the index date; however, it is possible that the 12-month baseline period was not long enough to capture all the information on potential confounders and that there was incomplete ascertainment of some variables in the claims data.
Conclusions
In this large cohort study, initiation of DPP4i did not appear to be associated with a higher risk of composite CVD including HF compared to the initiation of non-DPP4i diabetes drugs. There was no increased risk of CVD or HF associated with the initiation of DPP4i in patients with baseline CVD as used in the community setting.
Abbreviations
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- DPP4i:
-
Dipeptidyl peptidase-4 inhibitors
- HbA1c:
-
Glycated hemoglobin
- HF:
-
Heart failure
- HR:
-
Hazard ratio
- ICD-9 CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification 9th edition
- PS:
-
Propensity score
- RCT:
-
Randomized controlled trial
- T2DM:
-
Type 2 diabetes
- TZD:
-
Thiazolidinedione
References
Amori RE, Lau J, Pittas AG (2007) Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA 298(2):194–206
Karagiannis T, Paschos P, Paletas K, Matthews DR, Tsapas A (2012) Dipeptidyl peptidase-4 inhibitors for treatment of type 2 diabetes mellitus in the clinical setting: systematic review and meta-analysis. BMJ 344:e1369
Aschner P, Kipnes MS, Lunceford JK, Sanchez M, Mickel C, Williams-Herman DE (2006) Sitagliptin Study 021 Group: effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care 29(12):2632–2637
Gallwitz B, Rosenstock J, Rauch T, Bhattacharya S, Patel S, von Eynatten M, Dugi KA, Woerle HJ (2012) 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet 380(9840):475–483
DeFronzo RA, Fleck PR, Wilson CA, Mekki Q (2008) Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin in patients with type 2 diabetes and inadequate glycemic control: a randomized, double-blind, placebo-controlled study. Diabetes Care 31(12):2315–2317
Faillie JL, Azoulay L, Patenaude V, Hillaire-Buys D, Suissa S (2014) Incretin based drugs and risk of acute pancreatitis in patients with type 2 diabetes: cohort study. BMJ 348:g2780
Li L, Shen J, Bala MM, Busse JW, Ebrahim S, Vandvik PO, Rios LP, Malaga G, Wong E, Sohani Z et al (2014) Incretin treatment and risk of pancreatitis in patients with type 2 diabetes mellitus: systematic review and meta-analysis of randomised and non-randomised studies. BMJ 348:g2366
Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, Mitch W, Smith SC Jr, Sowers JR (1999) Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation 100(10):1134–1146
Wit MA, de Mulder M, Jansen EK, Umans VA (2013) Diabetes mellitus and its impact on long-term outcomes after coronary artery bypass graft surgery. Acta Diabetol 50(2):123–128
Tarquini R, Lazzeri C, Pala L, Rotella CM, Gensini GF (2011) The diabetic cardiomyopathy. Acta Diabetol 48(3):173–181
Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB et al (2013) Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 369(14):1317–1326
White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S et al (2013) Alogliptin after Acute Coronary Syndrome in Patients with Type 2 Diabetes. N Engl J Med 369(14):1327–1335
White WB (2013) Results from examine. In: 49th European Association for the Study of Diabetes September 26 2013, Barcelona, Spain
American Diabetes Association (2014) Standards of medical care in diabetes–2014. Diabetes Care 37(Suppl 1):S14–80
Lipscombe LL, Gomes T, Levesque LE, Hux JE, Juurlink DN, Alter DA (2007) Thiazolidinediones and cardiovascular outcomes in older patients with diabetes. JAMA 298(22):2634–2643
Andrade SE, Harrold LR, Tjia J, Cutrona SL, Saczynski JS, Dodd KS, Goldberg RJ, Gurwitz JH (2012) A systematic review of validated methods for identifying cerebrovascular accident or transient ischemic attack using administrative data. Pharmacoepidemiol Drug Saf 21(Suppl 1):100–128
Saczynski JS, Andrade SE, Harrold LR, Tjia J, Cutrona SL, Dodd KS, Goldberg RJ, Gurwitz JH (2012) A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf 21(Suppl 1):129–140
Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH (2004) Accuracy of medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J 148(1):99–104
Choma NN, Griffin MR, Huang RL, Mitchel EF Jr, Kaltenbach LA, Gideon P, Stratton SM, Roumie CL (2009) An algorithm to identify incident myocardial infarction using Medicaid data. Pharmacoepidemiol Drug Saf 18(11):1064–1071
Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S (2011) A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol 64(7):749–759
Rubin D (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med 127(8 Pt 2):757–763
Austin PC (2007) The performance of different propensity score methods for estimating marginal odds ratios. Stat Med 26(16):3078–3094
Austin PC (2009) Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J Biom Z 51(1):171–184
Kleinbaum D, Klein M (2012) Evaluating the proportional hazards assumption. In: Gail M, Krickberg K, Samet J, Tsiatis A, Wong W (eds) Survival analysis: A self-learning text, 3rd edn. Springer, Berlin
White WB, Pratley R, Fleck P, Munsaka M, Hisada M, Wilson C, Menon V (2013) Cardiovascular safety of the dipetidyl peptidase-4 inhibitor alogliptin in type 2 diabetes mellitus. Diabetes Obes Metab 15(7):668–673
McMurray J (2013) The Vildagliptin in Ventricular Dysfunction Diabetes trial (VIVIDD). In: European Society of Cardiology Heart Failure Association: May 26 2013, Lisbon, Portugal: 99
Ussher JR, Drucker DJ (2012) Cardiovascular biology of the incretin system. Endocr Rev 33(2):187–215
Johnson ES, Bartman BA, Briesacher BA, Fleming NS, Gerhard T, Kornegay CJ, Nourjah P, Sauer B, Schumock GT, Sedrakyan A et al (2013) The incident user design in comparative effectiveness research. Pharmacoepidemiol Drug Saf 22(1):1–6
Ray WA (2003) Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol 158(9):915–920
Acknowledgments
Kim was supported by the NIH grant K23 AR059677. Goldfine is supported by the NIH grants R56 DK095451, P50 HL083813, R01 DK088214, U01 HL101422, P30-DK03836, and American Diabetes Association 7-13-CE-17.
Conflict of interest
Kim received research support from Pfizer, Inc, Glynn received research grants from AstraZeneca and Novartis, Liu has no conflict of interest, Everett receives research support from Roche Diagnostics and Novartis and Goldfine receives research support in the form of materials and supplies from Amneal Pharmaceuticals; Lifescan, a Division of Johnson and Johnson; Novo Nordisk; Mercodia and Nestle, Inc.
Human and Animal Rights disclosure
The study protocol was approved by the Institutional Review Board of the Brigham and Women’s Hospital. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent disclosure
Patient informed consent was not required as the dataset was de-identified to protect subject confidentiality.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Antonio Secchi.
Prior Presentation Parts of this study were presented in abstract form at the ICE/ENDO 2014 meeting in Chicago, IL, 21–24 June 2014.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, S.C., Glynn, R.J., Liu, J. et al. Dipeptidyl peptidase-4 inhibitors do not increase the risk of cardiovascular events in type 2 diabetes: a cohort study. Acta Diabetol 51, 1015–1023 (2014). https://doi.org/10.1007/s00592-014-0663-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0663-2