Abstract
Purpose
The outcomes of anterior cruciate ligament reconstruction in the setting of multiligamentous knee injury (M-ACLR) have not been well characterized compared to isolated ACLR (I-ACLR). This study aims to characterize and compare short-term outcomes between I-ACLR and M-ACLR.
Methods
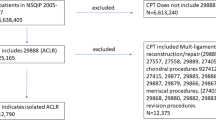
This is a retrospective cohort analysis of the American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2017. Current Procedural Terminology codes were used to identify and compare elective I- and M-ACLR patients, excluding patients undergoing concomitant meniscal or chondral procedures. Patient demographics and outcomes after I- and M-ACLR were compared using bivariate analysis. Multiple logistic regression analyzed if multiligamentous ACLR was an independent risk factor for adverse outcomes.
Results
There was a total of 13,131 ACLR cases, of which 341 were multiligamentous cases. The modified fragility index-5 was higher in multiligamentous ACLR (p < 0.001). Multiligamentous ACLR had worse perioperative outcomes, with higher rate of all complications (3.8%, p = 0.013), operative time > 1.5 h (p < 0.001), length of stay (LOS) ≥ 1 day (p < 0.001), wound complication (2.1%, p = 0.001), and intra- or post-op transfusions (p < 0.001). In multiple logistic regression, multiligamentous ACLR was an independent risk factor for LOS ≥ 1 (odds ratio [OR] 5.8), and intra-/post-op transfusion (OR 215.1) and wound complications (OR 2.4). M-ACLR was not an independent risk factor for any complication, reoperation at 30 days, readmission, urinary tract infection (UTI), or venous thromboembolism (VTE).
Conclusion
M-ACLR generally had worse outcomes than I-ACLR, including longer LOS, need for perioperative transfusions, and wound complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiligamentous injury presents a challenging case for the orthopedic surgeon compared to simple isolated anterior cruciate ligament (ACL) injuries. Multiligamentous knee injury involves at least two of the four primary stabilizing knee ligaments, and it may present as a tear of one cruciate ligament and a concomitant collateral ligament injury or as a frank knee dislocation [1]. These injuries are relatively uncommon, representing 0.02–0.2% of orthopedic injuries [2]. There is a male predominance (4:1 ratio of male to female), over half of injuries occur from motor vehicle accident trauma, and only one-third occur from sporting injuries [2]. The most common injury patterns are ACL-posterior cruciate ligament (PCL)-posterolateral corner-(PLC, 28–43%) and ACL, PCL, and medial collateral ligament (MCL) injuries (17–41%) [3, 4]. Multiligamentous knee injury without an ACL tear is relatively uncommon (9%) [3]. Operative treatment has been described to have better outcomes compared to nonoperative treatment [5]. Acute reconstruction/repair takes place within 3 weeks, and delayed reconstruction occurs more than three weeks from injury [6]. Open approach followed by arthroscopic reconstruction to repair/reconstruct the injured collateral and cruciate ligaments has been described to improve soft tissue visualization and prevent fluid extravasation into the surgical site [6].
Multiligamentous knee injuries treated surgically are associated with several complications. In a series of 130 surgically treated multiligamentous knee injuries, the complication rate was reported to be 28%, 14% required manipulation under anesthesia, and 9% needed revision surgery at minimum 1-year follow-up [7]. Lian et al. [8] reviewed outcomes of 108 multiligamentous knee injuries treated with single stage surgery, and obesity was identified as a risk factor for revision surgery (12% vs. 4% in nonobese patients) and infection requiring irrigation and debridement.
Because the incidence of ACLR in the setting of multiligamentous knee repair/reconstruction (M-ACLR) is quite rare compared to isolated ACL reconstruction (I-ACLR), orthopedic surgeons will typically not see many cases in their practice. Further, patients are more likely to have heard of I-ACLR than M-ACLR prior to their injury. Comparison of M-ACLR to the relatively common I-ACLR will offer better insight and context to surgeons about the expected perioperative outcomes after M-ACLR, and it would help surgeons counsel patients about risk factors that led to M-ACLR and their expected recovery after surgery by comparing it to the more familiar I-ACLR. Surgeons would be able to better plan perioperative care and predict complications. Published literature on outcomes of multiligamentous knee injuries often lacks a large sample size and long follow-up or provides data from outside the USA [5, 8, 9].
Given the stated limitations of prior literature, we sought to provide a comprehensive analysis of the early postoperative outcomes after arthroscopic ACLR in the setting of multiligamentous knee injuries (M-ACLR) versus I-ACLR. This study leverages the power of a large database across many states of the USA to overcome potential bias of foreign database studies and small sample sizes of previous case series. The purpose of this study is to compare the outcomes between M-ACLR and I-ACLR and determine the associated risk factors for complications.
Methods
Data collection
This is a study based on data from American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2005 to 2017, a multicenter national deidentified database that tracks perioperative data for 30 days postoperatively. Trained chart reviewers enter patient data through web-based data collection to ACS, while software automatically populates other parts of the data that do not require manual review. ACS-NSQIP has been shown to be superior to institutional databases in perioperative classification of outcomes [10,11,12]. Reviewers are certified annually to ensure high interrater reliability (IRR). IRR rate is reported to be 2.4%, with sites higher than 5% disagreement required to perform additional training and audit [13]. NSQIP database has been used for prior orthopedics studies including ACLR [14].
Patient population
Patient undergoing anterior cruciate ligament reconstruction (ACLR) was queried from NSQIP between 2005 and 2017 databases using Current Procedure Terminology (CPT) Codes. Each patient’s index surgery had associated CPT codes recorded in NSQIP, and patients were filtered based on whether they had the appropriate codes based on the inclusion and exclusion criteria of the study. Accreditation Counsel for Graduate Medical Education (ACGME) Case Log Guidelines for Orthopedic Sports Medicine and online CPT code databases provided definitions for the CPT code 29888 were used to identify all arthroscopically aided ACLR [15]. ACLR was divided into two groups: isolated (I-ACLR) and ACLR as part of multiligamentous repair/reconstruction (M-ACLR) using CPT codes (Table 1). M-ACLR included ACLR with posterior cruciate ligament reconstruction (PCLR) or collateral ligament repair. M-ACLR cases had CPT codes for multiligamentous repair/reconstruction (CPT 29889, 27556, 27557, 27558), ACLR with concomitant posterior cruciate ligament reconstruction (PCLR, CPT 29889), ACLR with concomitant collateral ligament repair/reconstruction (CPT 27405, 27409) [15]. Multiligamentous knee injury without ACLR is relatively uncommon (9%) and was excluded for a consistent comparison versus isolated ACLR [3]. Any ACLR case with concomitant knee articular cartilage procedure (CPT 27412, 27415, 29877, 29885, 29886, 29887, 29879, 29866, 29867) and ACLR with meniscectomy procedures (CPT 27403, 29868, 29880, 29881, 29882, 29883) were excluded from analysis to avoid confounding concomitant procedures. Nonelective cases were excluded based on a variable in NSQIP regarding whether the index surgery was elective or not. I-ACLR was defined as ACLR that did not include cartilage, collateral ligament repair, meniscectomy. M-ACLR was all single-stage procedure, and the database could not differentiate between early and delayed M-ACLR.
Study variables
Independent variable was whether the patient got M-ACLR versus I-ACLR. Dependent variables include differences in demographics and 30-day surgical outcomes. Demographic variables include age, sex, race, obesity (Body Mass Index [BMI] > 30 kg/m2), American Society of Anesthesiologists (ASA) score, diabetic status, history of chronic obstructive pulmonary disease (COPD), smoking status within 1 year of surgery date, dyspnea, cardiac comorbidity, renal comorbidity, inpatient/outpatient surgery setting, functional health status, weight loss > 10% before surgery, > 2 drinks/day alcohol use within 2 weeks of surgery, pre-op hematocrit level, pre-op creatinine level, pre-op albumin level, hypertensive history, steroid use for chronic conditions. Cardiac comorbidities include patients noted to have history of hypertension, congestive heart failure, and prior cardiac surgery. Similarly, renal comorbidities include history of dialysis and renal failure. Functional health status before surgery is a variable that could be independent, partially dependent, or dependent. Partially dependent and dependent mean the patient requires assistance from another person with part or all their daily activities, respectively [16]. Unless otherwise specified, history of preoperative comorbidities exists 6 months prior to surgery. Low hematocrit was defined as lower than 35.5%. Native Hawaiian, Alaskan Natives, and pacific islanders were included in the “Other” race category. Normal albumin was defined as lower than 3.4–5.4 g/dl [17]. Elevated creatinine was defined as > 1.21 mg/dl [18]. Modified fragility index (mFI-5), which is a proxy of the patient’s medical comorbidities, is calculated based on whether the patient has any of the 5 comorbidities as described in Subramaniam et al. [19]. The mFI-5 was calculated and compared between M- and I-ACLR. Thirty-day surgical outcomes include development of any complication (including medical complications, unplanned readmissions, or reoperations), operative time, length of stay (LOS), wound complication, venous thromboembolism (VTE), urinary tract infection (UTI), intraoperative/postoperative bleeding requiring transfusion, and sepsis.
Statistics
Statistical analysis was conducted using SAS software (Cary, NC, USA). Continuous variables like age were grouped into categorical variables. Chi-square test was used to conduct bivariate statistical analysis, and Fischer’s exact test was used when appropriate. Wilcoxon rank sum test was used to compare continuous variables. Multiple stepwise logistic regression forced the independent variable of surgery type and mFI-5 into the models to determine if they were predictors of adverse surgical outcomes. Regression model also attempted to fit all preoperative demographic variables into the final regression model. p < 0.05 was set as threshold for statistical significance.
Results
Demographics
There was a total of 13,131 ACLR cases, of which 341 (2.6%) were M-ACLR. Of the 341 M-ACLR, 154 (45.7%) involved the PCL, 183 (54.3%) involved the collateral ligaments, and 4 (1.17%) were unspecified (Table 2). Mean age was 32.2 ± 10.7 years old with no difference in age distribution (Table 3). A total of 63.2% of patients were male, 40.6% of patients were Caucasian, and 29.2% of patients were obese. M-ACLR patients tended to be males (p = 0.003), Caucasian or African-American (p < 0.001), obese (p < 0.001), with ASA status > 3 (p < 0.001). M-ACLR patients tended to have higher rates of preexisting medical comorbidities: bleeding disorders (p = 0.011), history of hypertension (p < 0.001), history of cardiac comorbidity (p < 0.001), current smokers (p < 0.001), have partially dependent functional status (p < 0.001), history of recent weight loss (p = 0.002), and have high creatinine levels (p = 0.048). Mean mFI-5 and proportion of patients with mFI-5 > 0 (both p < 0.001) were both higher in M-ACLR. Bolded p-values represent significance (p < 0.05).
Surgical outcomes and complications
Compared to patients undergoing I-ACLR, patients undergoing M-ACLR had higher rates of all complication (Table 4, 3.8% M-ACLR vs. 1.9% I-ACLR, p = 0.013). M-ACLR had higher rates of operative time > 1.5 h (p < 0.001), LOS 1 ≥ day (p < 0.001), wound complications (p < 0.001), bleeding transfusions intra- or postoperatively (1.2% M-ACLR vs. 0% I-ACLR, p < 0.001). M-ACLR was not associated with higher rates of reoperation, readmission, or venous thromboembolism compared to I-ACLR.
Multivariate analysis
Multivariate stepwise regression identified mFI-5 > 0 (odds ratio [OR] 1.4), male sex (OR 1.5), obesity (OR 1.5), smoking (OR 1.4), dependent functional status (OR 4.9), recent weight loss (OR 6.5), and ASA > 3 (OR 1.8) to be risk factors for undergoing a M-ACLR (Table 5). Undergoing M-ACLR was an independent risk factor for intraoperative or postoperative transfusion (OR 215.1), wound complication (OR 2.4), operative time > 1.5 h (OR 8.0), and LOS ≥ 1 day (OR 5.8). mFI-5 > 0 was also an independent risk factor for LOS ≥ 1 day (OR 2.1). M-ACLR was not an independent risk factor for all complications, readmissions, reoperations.
Discussion
This study compared the demographics and perioperative outcomes of M-ACLR and I-ACLR. The main finding was that patients undergoing M-ACLR were at increased risk for having intraoperative or postoperative transfusion, wound complication, operative time > 1.5 h, and LOS ≥ 1 day. However, M-ACLR was not an independent risk factor for all complications, readmissions, reoperations. Surgeons can use these findings to counsel patients on the likely short-term surgical outcomes of M-ACLR compared with I-ACLR.
Certain demographics and preoperative factors were significantly more prevalent in the M-ACLR population than I-ACLR: male sex, Black or African-American, White or Caucasian race, obesity, ASA status > 3, history of bleeding disorders, hypertension, cardiac comorbidity, dependent functional status, tobacco smoking, recent weight loss > 10% of body mass, high preoperative creatinine levels. In our study, mFI-5 > 0, male sex, obesity, tobacco use, dependent functional status, recent weight loss, ASA ≥ 3 are independent risk factors for undergoing M-ACLR instead of I-ACLR. The closest study to the current one comparing multiple knee ligament injury and isolated ACLR is that of Wyatt et al. [20] using the Kaiser Permanente Database. M-ACLRs were more prevalent in male patients (73.2% M-ACLR vs. 62.8% I-ACLR), patients with BMI > 30 (31.1% M-ACLR vs. 22.7% I-ACLR) [20]. The results of Wyatt et al. corresponded well to current findings of risk factors of undergoing M-ACLR, namely obesity and male sex. Previously, male sex [20,21,22], obesity [7, 20], younger age [20, 22] were commonly associated with M-ACLR. Surgeons may discuss these risk factors with patients who need M-ACLR and have higher index of suspicion for multiligamentous injury when evaluating these patients with these risk factors.
Both high (25.1–39%) and low energy trauma can cause multiligamentous knee injury, where sporting activities account for 44.2% (Skiing 29.4%) of injury [7, 23]. Arom et al. [22] report closed knee dislocations were much more common, with anterior direction being the most common after unspecified direction. During multiligamentous knee injury, Becker et al. [3] report that the ACL was injured 90% of the time, PCL in 79% of the time, posterolateral corner in 78%, MCL in 23%. In Wyatt et al. [20], ACL/MCL was most prevalent combination (58.1%) followed by ACL/PCL (15.8%). In our study, collateral ligaments were most prevalent concomitant injury that was repaired (54.30%), followed by PCL (45.70%).
In terms of short-term outcomes, higher rates of operative time > 1.5 h and LOS ≥ 1 day were seen in M-ACLR compared to I-ACLR. On multivariate analysis, M-ACLR was an independent risk factor of wound complication, postoperative or intra-operative transfusions, LOS ≥ 1 day, and operative time > 1.5 h. Even though M-ACLR had higher rates of any complication in bivariate analysis, multivariate analysis showed that any complication was driven by dependent functional status, operative time > 1.5 h, inpatient setting, and dyspnea symptoms preoperatively. Increased length of stay, inpatient operative setting, wound complication, and transfusions all are associated with increased cost of care [24]. Bokshan et al. [25] report 69.3% of patients had operative time > 90 min in isolated ACLR, which is slightly higher than that of the current study. Surgeons should plan on increasing time allotted in the OR, having blood transfusions ready, and anticipating overnight admission as opposed to ambulatory surgery for M-ACLR cases. Because direct comparison of perioperative outcomes of I-ACLR and M-ACLR is lacking in the literature, comparison of our results to published outcomes of either I-ACLR or M-ACLR is necessary.
Isolated ACLR occurs much more frequently and generally has generally good outcomes treated both operatively and nonoperatively [26]. Mihelic et al. [27] report in 17–20-year follow-up that nonoperative treatment had significantly higher rates of unstable knees with 84% having severe laxity and significantly worse Lysholm Knee Scale, Tegner scores, and International Knee Documentation Committee (IKDC) scores. Hoffelner et al. [28] report I-ACLR did not increase incidence of osteoarthritis. Smith et al. [29] report no functional difference between operative and nonoperative ACL tear management. Compared to isolated ACLR, the multiligamentous knee injury (MKI) occurs less commonly and more often require more complex surgical repair [20]. Arom et al. [22] report annual incidence of knee injury in the PearlDiver database to be 0.072 per 100 patient-years between 2004 and 2009. In Cook et al. [7], surgical intervention was performed in 37% of the MKIs. However, evidence suggests early, operative management on MKIs has superior outcomes compared to nonoperative management [2, 30].
There was only 1 transfusion in I-ACLR, which is due to the low estimated blood loss in I-ACLR to be 125–178 mL in Leo et al. [31]. By contrast, vascular injury occurs in 18–64% of knee dislocations [32, 33], which can explain the higher rate of transfusions in M-ACLR compared to I-ACLR. Cook et al. [7] report peroneal nerve injuries (20%) and vascular injuries were reported to be common after multiligamentous injury. Peroneal nerve injury was associated with posterolateral corner injury, while lateral-sided injuries were associated with popliteal artery injuries [23].
Qin et al. [34] report on M-ACLR had a 16.8% 90-day complication rate and 8.3% readmission rate in the Humana Claims Database. Jameson et al. [26] report a 30-day readmission rate of 1.36% and wound complication rate of 0.75% in all planned ACLR in the English National Health Service (NHS). Wound complication rate is similar, but readmission rate is slightly higher than reported in current study. This can be attributed to possible differences in tracking readmissions in the NHS system compared to NSQIP. The NHS system has the benefit of tracking readmission nationally, while NSQIP tracks only readmission at participating hospitals [13]. Wilson et al. [21] report a 90-day readmission rate of 4.8% and 1.94% (20/1032 patients) 90-day reoperation rate for M-ACLR in New York State. Short-term reoperation rate in our study was like that of Wilson et al., which had 90-day follow-up. However, the current study found a much lower short-term complications and readmission rates than the two prior studies, granted the follow-up was 30 days instead of 90 days. The cited short-term (30 to 90 days) readmission (4.8–8.3%), complication (16.8%), and reoperation rates (0.97–1.94%) for M-ACLR [21, 34] were higher than cited overall complication (0.65%), readmission (1.36%), reoperation (0.97%) in the I-ACLR literature [26, 35].
Ristic et al. [36] report 1.2% infection after ACLR, with more likely infection in patients undergoing surgery lasting over 1.5 h. The reported infection rate is higher than reported in this study, but the surgeries were performed in Europe [36], which could have different standards of aseptic techniques. Abram et al. [35] report a 0.97% reoperation, 0.47% infection, 0.4% UTI, 0.12% pulmonary embolism rate in 90 days after I-ACLR. These values are expectedly slightly higher than in the current study due to longer follow-up [13, 26, 35, 36]. Born et al. [37] report a 2% venous thromboembolism (VTE) rate with 3-month follow-up in primary and revision M-ACLR. The VTE rate in M-ACLR (1.2%) was lower in the current study, which had a shorter follow-up time of 30 days. Cook et al. [7] report an infection rate of 4% in M-ACLR at 1-year follow-up, with obesity being a significant risk factor for postoperative infection. Short-term wound complication of 2.1% in our M-ACLR cohort was lower than Cook et al. but higher than in the reported I-ACLR (0.47%0.75%) [26, 35].
Overall, this study provided surgeons with a broad picture of complication profile of M-ACLR compared to I-ACLR. Recognizing common complications, surgeons may alter their operative and perioperative care plan for cases. The results of this study may also lower the threshold to pursue diagnosis and intervention for complications such as bleeding and VTE. Because M-ACLR is much rarer than I-ACLR, having comparison helps put in perspective the outcomes of M-ACLR.
Limitations
The study was limited mostly by the NSQIP follow-up of 30 days post-op. Complications beyond this early perioperative period are not included in the follow-up. The outcome comparison is not completely equal to those studies with 90-day follow-up. All NSQIP index cases are single-stage procedures, and it was not possible to analyze staged M-ACLR in this study. The CPT codes collected are for the index surgery and does not capture staged surgery where the patient is discharged and brought back for the second-stage procedure under a different surgical encounter. Also, the mechanism of injury and other concomitant injuries, such as to the chest or abdomen, were not tracked by the database. The injury mechanism is also not tracked in the database. The time of injury to time of surgery is not recorded NSQIP, and it was not possible to determine whether M-ACLR was early or delayed. These factors can all affect results such as complications, readmissions, and transfusions. Further, graft choice is not included in the data, which did not allow a more nuanced analysis of grafts. There is sparse literature on M-ACLR and I-ACLR, which makes our findings difficult to compare to similar studies. The database lacks granularity such as graft type used and prior knee surgery. The database does not report patient reported outcomes, and it was not possible to compare patient reported outcomes between M- and I-ACLR. The study cannot make accurate national estimates of complication rates as hospitals participating in NSQIP may not reflect national average.
Conclusions
M-ACLR generally had worse outcomes than I-ACLR, including longer LOS, need for perioperative transfusions, and wound complications.
Data availability
The datasets generated and/or analyzed during the current study are available in the American College of Surgeons National Surgical Quality Improvement Program repository, which can be found and requested at: https://www.facs.org/quality-programs/data-and-registries/acs-nsqip/.
References
Levy BA, Fanelli GC, Whelan DB et al (2009) Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthopaedic Surg 17(4):197–206
Howells NR, Brunton LR, Robinson J et al (2011) Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury 42:1198–1204. https://doi.org/10.1016/j.injury.2010.11.018
Becker EH, Watson JD, Dreese JC (2013) Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma 27:226–231
Robertson A, Nutton RW, Keating JF (2006) Dislocation of the knee. J Bone Joint Surg Br 88:706–711. https://doi.org/10.1302/0301-620X.88B6.17448
Ng JWG, Myint Y, Ali FM (2020) Management of multiligament knee injuries. EFORT Open Rev 5:145–155. https://doi.org/10.1302/2058-5241.5.190012
Moatshe G, Chahla J, LaPrade RF, Engebretsen L (2017) Diagnosis and treatment of multiligament knee injury: state of the art. Journal of ISAKOS 2:152–161. https://doi.org/10.1136/jisakos-2016-000072
Cook S, Ridley TJ, McCarthy MA et al (2015) Surgical treatment of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc 23:2983–2991. https://doi.org/10.1007/s00167-014-3451-1
Lian NK, Nickoli M, Vaswani R, Irrgang JJ, Lesniak BP, Musahl VJP (2020) Obesity is associated with significant morbidity after multiligament knee surgery. J Knee Surg 33:525–530. https://doi.org/10.1055/s-0039-1681027
Nielsen TG, Sørensen OG, Lind M (2022) A comparison of multi-ligament reconstruction and isolated anterior cruciate ligament reconstruction at one year follow-up: results from the Danish Knee Ligament Reconstruction Registry. J Exp Orthop 9:30. https://doi.org/10.1186/s40634-022-00473-z
Cima RR, Lackore KA, Nehring SA et al (2011) How best to measure surgical quality? Comparison of the agency for healthcare research and quality patient safety indicators (AHRQ-PSI) and the American college of surgeons national surgical quality improvement program (ACS-NSQIP) postoperative adverse EV. Surgery 150:943–949. https://doi.org/10.1016/j.surg.2011.06.020
Davenport DL, Holsapple CW, Conigliaro J (2009) Assessing surgical quality using administrative and clinical data sets: a direct comparison of the university healthsystem consortium clinical database and the national surgical quality improvement program data set. Am J Med Qual 24:395–402. https://doi.org/10.1177/1062860609339936
Hutter MM, Rowell KS, Devaney LA et al (2006) Identification of surgical complications and deaths: an assessment of the traditional surgical morbidity and mortality conference compared with the American college of surgeons-national surgical quality improvement program. J Am Coll Surg 203:618–624. https://doi.org/10.1016/j.jamcollsurg.2006.07.010
Surgeons AC (2017) User Guide for the 2016 ACS NSQIP Participant Use Data File (PUF). 4–11
Crutchfield CR, Zhong JR, Lee NJ et al (2022) Operative time less than 1.5 Hours, male sex, dependent functional status, presence of dyspnea, and reoperations within 30 days are independent risk factors for readmission After ACLR. Arthrosc Sports Med Rehabil 4:e1305–e1313. https://doi.org/10.1016/j.asmr.2022.04.010
(ACGME) AC for GME (2015) Case Log Guidelines for Orthopaedic Sports Medicine Review Committee for Orthopaedic Surgery
Scarborough JE, Bennett KM, Englum BR et al (2015) The impact of functional dependency on outcomes after complex general and vascular surgery. Ann Surg 261:432–437. https://doi.org/10.1097/SLA.0000000000000767
Haldeman-Englert, Chad; Trevino, Heather; Turley K (2021) Albumin (Blood). In: Health Encyclopedia of University of Rochester. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=albumin_blood#:~:text=A normal albumin range is,surgery or a heart attack. Accessed 19 Jan 2020
Mayo Clinic (2018) Creatinine Test. https://www.mayoclinic.org/tests-procedures/creatinine-test/about/pac-20384646. Accessed 19 Jan 2021
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM (2018) New 5-factor modified frailty index using American college of surgeons NSQIP data. J Am Coll Surg 226:173-181.e8. https://doi.org/10.1016/j.jamcollsurg.2017.11.005
Wyatt RWB, Inacio MCS, Bellevue KD et al (2017) Isolated ACL versus multiple knee ligament injury: associations with patient characteristics, cartilage status, and meniscal tears identified during ACL reconstruction. Phys Sportsmed 45:323–328. https://doi.org/10.1080/00913847.2017.1321460
Wilson SM, Mehta N, Do HT et al (2014) Epidemiology of multiligament knee reconstruction. Clin Orthop Relat Res 472:2603–2608. https://doi.org/10.1007/s11999-014-3653-3
Arom GA, Yeranosian MG, Petrigliano FA et al (2014) The changing demographics of knee dislocation: a retrospective database review. Clin Orthop Relat Res 472:2609–2614. https://doi.org/10.1007/s11999-013-3373-0
Moatshe G, Dornan GJ, Løken S et al (2017) Demographics and injuries associated with knee dislocation: a prospective review of 303 patients. Orthop J Sports Med 5:2325967117706521. https://doi.org/10.1177/2325967117706521
Novak PJ, Bach BR, Bush-Joseph CA, Badrinath S (1996) Cost containment: a charge comparison of anterior cruciate ligament reconstruction. Arthroscopy: J Arthroscopic Related Surg 12:160–164. https://doi.org/10.1016/S0749-8063(96)90005-5
Bokshan SL, Mehta S, DeFroda SF, Owens BD (2019) What Are the Primary Cost Drivers of Anterior Cruciate Ligament Reconstruction in the United States? A Cost-Minimization Analysis of 14,713 Patients. Arthroscopy: J Arthroscopic Related Surg 35:1576–1581. https://doi.org/10.1016/j.arthro.2018.12.013
Jameson SS, Dowen D, James P et al (2012) Complications following anterior cruciate ligament reconstruction in the English NHS. Knee 19:14–19. https://doi.org/10.1016/j.knee.2010.11.011
Mihelic R, Jurdana H, Jotanovic Z et al (2011) Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop 35:1093–1097. https://doi.org/10.1007/s00264-011-1206-x
Hoffelner T, Resch H, Moroder P et al (2012) No increased occurrence of osteoarthritis after anterior cruciate ligament reconstruction after isolated anterior cruciate ligament injury in athletes. Arthroscopy: J Arthroscopic Related Surg 28:517–525. https://doi.org/10.1016/j.arthro.2011.09.014
Smith TO, Postle K, Penny F et al (2014) Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee 21:462–470. https://doi.org/10.1016/j.knee.2013.10.009
Levy BA, Dajani KA, Whelan DB et al (2009) Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy: J Arthroscopic Related Surg 25:430–438. https://doi.org/10.1016/j.arthro.2009.01.008
Leo BM, Krill M, Barksdale L, Alvarez-Pinzon AM (2016) Failure rate and clinical outcomes of anterior cruciate ligament reconstruction using autograft hamstring versus a hybrid graft. Arthroscopy: J Arthroscopic Related Surg 32:2357–2363. https://doi.org/10.1016/j.arthro.2016.04.016
Medina O, Arom GA, Yeranosian MG et al (2014) Vascular and nerve injury after knee dislocation: a systematic review. Clin Orthop Relat Res 472:2621–2629. https://doi.org/10.1007/s11999-014-3511-3
Seroyer ST, Musahl V, Harner CD (2008) Management of the acute knee dislocation: the Pittsburgh experience. Injury 39:710–718. https://doi.org/10.1016/j.injury.2007.11.022
Qin C, Roth C, Lee C, Athiviraham A (2020) National trends, 90-day readmission and subsequent knee surgery following multi-ligament knee reconstruction. J Orthop 21:49–52. https://doi.org/10.1016/j.jor.2020.01.030
Abram SGF, Judge A, Beard DJ, Price AJ (2019) Rates of adverse outcomes and revision surgery after anterior cruciate ligament reconstruction: a study of 104,255 procedures using the national hospital episode statistics database for England, UK. Am J Sports Med 47:2533–2542. https://doi.org/10.1177/0363546519861393
Ristić V, Maljanović M, Harhaji V, Milankov M (2014) Infections after reconstructions of anterior cruciate ligament. Med Pregl 67:11–15
Born TR, Engasser WM, King AH et al (2014) Low frequency of symptomatic venous thromboembolism after multiligamentous knee reconstruction with thromboprophylaxis. Clin Orthop Relat Res 472:2705–2711. https://doi.org/10.1007/s11999-014-3576-z
Funding
No funding was received for any part of this study.
Author information
Authors and Affiliations
Contributions
JZ contributed to research idea, analyzed patient data, and drafted the first version of the manuscript. NJ, CC, JM, CA, DT, and TSL contributed to initial research idea and made meaningful contributions to subsequent versions of the manuscript and the final version.
Corresponding author
Ethics declarations
Conflict of interest
CA receives IP royalties, is a Paid consultant, and conducts Research support from Arthrex, Inc.; he owns stock or options for Peak; he receives publishing royalties, financial, or material support from Lead Player; he conducts research support for Major League Baseball; he is on the editorial or governing board for Orthopedics Today; and he conducts research support for Stryker. TSL is a Board or committee member of American Orthopaedic Society for Sports Medicine; he is a paid consultant for CONMED Linvatec and Smith & Nephew. The remaining authors have no competing interests to disclose.
Ethics approval and consent to participate
The project described involved no identifiable patient data, direct patient contact, minimal risk to patients and was declared to the institutional review board at the affiliated institution1 to be exempt from further IRB approval under protocol #AAAS5527. Further documentation can be provided upon request.
Consent for publication
Not applicable. No individual person’s data are included.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhong, J., Lee, N.J., Crutchfield, C. et al. Perioperative outcomes in isolated versus multiligamentous anterior cruciate ligament reconstruction: a retrospective cohort analysis. Eur J Orthop Surg Traumatol 34, 1597–1607 (2024). https://doi.org/10.1007/s00590-024-03848-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-024-03848-3