Abstract
Aim
This article describes the technique of tibiotalar nailing performed using an antegrade tibial nail for salvage of distal tibia and ankle fractures in elderly patients.
Materials and methods
We report indications, surgical technique, and the clinical outcomes and complication rate in our series to date. A retrospective review was performed at our level 1 major trauma centre. Patient demographics, comorbidities, and 12-month post-operative course were collected. Fractures were classified using the OTA/AO and modified Gustilo–Anderson classification. Fifteen patients underwent the procedure. We present data with a minimum 12-month follow-up. The median age of the patients in this cohort was 83 years (range, 51–102). Five patients were diabetic. Six patients (6/15; 40%) presented with an open fracture.
Results
At final follow-up, fourteen patients reported painless walking and had returned to baseline activity.
Conclusion
This technique may serve as a salvage procedure, with indications similar to those for tibio-talar-calcaneal arthrodesis. Indications would include non-constructible pilon fractures, comminuted intra-articular fractures in low-demand patients, or patients at high risk of wound complications.
Level of clinical evidence
3
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction:
With an ageing population, the incidence of distal tibia and ankle fractures in frail elderly patients is expected to rise [1,2,3]. The treatment of unstable distal tibia and ankle fractures in frail, elderly patients remain unpredictable and associated with substantial morbidity and mortality. These patients’ comorbidities, the inherent fracture instability, and often delicate soft tissue envelope can contribute to the high risk of peri-operative complications. In addition, low bone mineral density can compromise surgical fixation and consequently increase the rates of failure of fixation [1, 4]. Furthermore, the estimated 12-month mortality of elderly patients who sustain an ankle fracture is around 10–15% [5, 6]. Strategies are therefore needed to mitigate peri-operative complications and optimize early functional outcome.
A notable limitation of conventional open reduction and internal fixation (ORIF) is the prolonged period of immobilization and weight-bearing restrictions, which are almost inevitable due to poor bone quality, regardless of aspirations of universal early weight-bearing [7]. Limiting an elderly patient’s mobility is not without its own challenges and many patients require admission to an intermediate care facility or nursing home to support activities of daily living as a result of this restriction. Hindfoot intramedullary nails have become popular as an alternative to ORIF for the management of unstable ankle fractures in elderly patients. These allow for immediate post-operative weight-bearing, facilitate early rehabilitation, and have shown a high return to pre-morbid level of mobility [8, 9]. This technique is not, however, without limitations. These include breaking or loosening of the distal calcaneal locking screw, peri-prosthetic fracture [4, 8], tibial stress fracture, and loss of subtalar motion.
As a technique to mitigate some of the drawbacks of the traditional tibio-talar-calcaneal (TTC) hindfoot nail, we describe the technique of tibiotalar nailing (TTN) performed using a traditional antegrade tibial intramedullary nail (IMN). This technique permits fixation using a load-sharing device from the proximal tibia to the talus, allowing preservation of the accommodative motion of the subtalar joint and thereby avoiding increasing mechanical loads across the distal tibia. This should, in turn, reduce the risk of peri-prosthetic or stress fractures and protect the distal locking screws from impact loading [10].
We describe the technique and review the clinical outcomes and complication rate from series of patients treated with this at our institution.
Materials and methods
A retrospective review of our electronic medical records was performed to identify all patients who underwent tibiotalar nailing with an antegrade tibial IMN for an unstable fracture or unsalvageable ankle joint. All procedures were performed at a level 1 Major Trauma Centre. For the purpose of this report, only patients with a minimum 12-month clinical follow-up. This timeframe was chosen given that these patients tend to routinely be discharged from our clinic at 12 months postoperatively.
The coordinated efforts between orthopaedic trauma surgeons and plastic surgeons, “Orthoplastics”, has led to more confidence in early wound excision, even in association with severe contamination and definitive wound closure [11]. Such an approach has been shown to lower rates of deep. Surgical site infection among adults with severe open fractures of the lower extremity [12]. Therefore, all patients who presented with open fractures underwent urgent irrigation and debridement by the Orthoplastic team at the earliest convenience. For all patients, the treating surgeon discussed all treatment options and patients underwent surgery on the basis of fully informed consent. All patients underwent surgery on the next available trauma list unless medical optimization was needed, temporary external fixation was necessary, or if patients were initially managed non-operatively with close contact casting.
Patient demographics, comorbidities, long-term complications, and re-operation rates were recorded. Fractures were classified using the OTA/AO classification. In cases of open fractures, we report injury grade using the modified Gustilo–Anderson classification [13] based upon the objective assessment of the open fracture wound at the end of the first debridement.
Surgical technique and postoperative management
In each case, preoperative imaging including anteroposterior and lateral radiographs at the ankle is obtained. A computed tomography (CT) scan is not routinely required for ankle fractures but is part of our treatment protocol for fractures involving the distal tibia, including pilon fractures.
Routine pre-operative antibiotics ± tranexamic acid is administered in line with local guidelines. The surgical procedure is performed under a general or spinal anaesthetic. The patient is positioned supine on a radiolucent table with sandbag under the ipsilateral hip. A tourniquet is not routinely used. Standard skin preparation and draping for tibial nailing are employed.
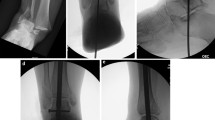
Closed reduction is performed manually by axial traction and ankle manipulation under radiographic guidance. The ankle should be in neutral position with the talus under the tibial plafond and the foot in neutral dorsiflexion to enable accurate nail insertion. When the coronal and sagittal alignments are satisfactory, two 2.0 mm K-wires are used to temporarily maintain the reduction (Fig. 1a). These are typically placed in retrograde fashion from the calcaneus into the distal tibia. These should be positioned so not to interfere with the eventual placement of the tibial nail. Depending on the fracture morphology and the condition of the soft tissue, additional K-wires may be needed to maintain temporary reduction. The technique is not predicated on thorough preparation of the ankle joint for a formal arthrodesis, but rather a subjective judgement must be made balancing the patient’s tolerance of surgery and healing with anticipated future mobility and longevity.
Our surgical preference is to use a suprapatellar tibial nail. This technique may equally be performed with an infrapatellar tibial nail, but we have found suprapatellar nailing beneficial to avoid the challenges of maintaining the provisional reduction of the ankle joint while performing nailing in deep flexion of the knee. A midline longitudinal incision is made proximal to the superior pole of the patella in usual fashion. The handle, inner protection sleeve, outer protection sleeve, and trocar are inserted through the incision into the knee joint into the ideal position for the starting point and insertion of a guide wire. To facilitate passing the 2.5 mm reaming rod through the ankle joint and into the talus, the ball tip is cut off. The reaming rod is advanced into the medullary canal to the level of the ankle joint. Orthogonal imaging is used to confirm that the tip of the wire is in a centre–centre position in the distal tibia. It is helpful to have an assistant hold the ankle reduced for the following steps in order to protect the provisional reduction while instrumentation is passed across the ankle joint. The guide wire is carefully hammered across the ankle joint and into the talus, as far as the inferior subchondral bone adjacent to the subtalar joint. The cut-end of the guide wire typically passes across the sub-chondral bone of the joint without difficulty due to the inherent low bone density in this patient group. The required nail length is measured in this position. The guide wire is then carefully advanced across the subtalar joint, through the calcaneus and out of the plantar aspect of the foot. A Kocher’s forceps or large haemostat is clamped onto the wire and helps to retain it during reamer extraction. The tibia and talus are then sequentially reamed as far distal as the inferior subchondral bone of the talus adjacent to the subtalar joint (Fig. 1b). The nail is then introduced into the intramedullary canal and advanced until it is well positioned in the talus (Fig. 1c and d).
Distal interlocking screws are introduced freehand into the talus. We aim to place one lateral-to-medial and an anteroposterior screw, with the oblique locking option in our implant of choice providing a further fixation opportunity (Fig. 1e). In poor bone quality, the angular stable locking system (ASLS) is an alternative to standard locking screws for increased stability. We gently back-slap the nail before inserting the proximal locking screws in order to provide some compression at the ankle. All wounds are thoroughly irrigated and closed in layers. A sterile dressing is applied.
Postoperatively, patients are allowed to immediately bear weight as tolerated. All patients are assessed by our physiotherapy team prior to discharge from hospital. All patients receive six weeks of venous thromboembolism prophylaxis in line with our local policy. Progress is then serially reviewed, clinically and radiologically as long as needed.
Results
We identified fifteen patients with a minimum 12-month follow-up who underwent tibiotalar nailing performed by this technique. The cohort comprised fourteen female patients and one male. The patients’ characteristics at time of surgery are summarized in Table 1. The median age of the patients in this cohort was 83 years (range, 51–102). Two patients (13%) were regular smokers. Five patients (33.3%) were diabetic and required pharmacological treatment. The majority of injuries were secondary to low energy falls.
Eight patients (53%) were treated immediately with a TTN either at the index surgery or following temporary external fixation. Seven patients (47%) underwent TTN as a salvage procedure following failed close contact cast or ORIF. Average time to definitive TTN was 23 days (range: 1–170). Four patients (27%) underwent a formal open or minimally invasive ankle joint preparation for fusion as part of the TTN procedure. For patients who were not primarily treated with a TTN, initial management strategy is presented in Table 2.
Six (6/15; 40%) patients presented with an open fracture; four were deemed type-II (26.6%) and two were type-IIIa (13.%). Three of the six patients with an open fracture had their wounds successfully closed primarily at the time of the index surgery. Two patients ultimately required a split thickness skin graft, and one patient required a free gracilis flap. All went on to heal without any complications.
All patients with open fractures were treated according to the joint standards of treatment for open fractures of the lower extremity in the United Kingdom as laid out by the British Orthopaedic Association and the British Association for Plastic, Reconstructive, and Aesthetic Surgery [14].
Complications
Two patients (13%) developed a superficial wound infection but were treated successfully with oral antibiotics—neither required revision surgery. One patient was diagnosed with failed fusion, talus loosening, and broken distal locking screws. The last clinical encounter note for each patient were reviewed. Fourteen patients with a minimum 12-month follow-up subjectively reported good functional outcomes and had return to their preferred activities of daily living.
Conclusion
Unstable ankle and distal tibia fractures in frail elderly patients continue to pose a clinical dilemma for orthopaedic surgeons. While there is convincing evidence that treating unstable ankle fractures with close contact casting in adults older than 60 years results in equivalent functional outcomes, which include quality of life, pain, ankle motion, and mobility, at six months compared to surgical fixation [15], doing so requires prolonged immobilization and weeks of non-weight-bearing. Limiting an elderly patient’s mobility is not without its own challenges, often requiring longer hospital stays or admission to an intermediate care facility or nursing home to support activities of daily living. An important consideration in choosing a management strategy should therefore be aimed at expediting pain-free mobilization. Allowing immediate post-operative weight bearing in this patient population has a significant impact on patient’s quality of life and ability to function independently and addresses the concern of non-compliance with restricted weight-bearing that comes with contemporary surgical fixation. In addition, 10% of patients reported in the Ankle Injury Management (AIM) trial [15] required a second manipulation of their ankle fracture, and 19% went on to surgical fixation due to loss of reduction.
In the light of this, hindfoot intramedullary nails were developed to facilitate early rehabilitation, restoration of function, and allow for immediate and full weight-bearing [4, 9]. In addition, intramedullary nails have the advantage of using smaller incisions, thus requiring less soft tissue dissection and therefore reducing the risks of wound complications.
While use of hindfoot nails has grown in popularity for the treatment of unstable ankle fractures in the elderly patients, they do come with their own limitations. One of these complications are peri-prosthetic tibial fractures, which can occur at the proximal tip of the hindfoot nail. To address this, several authors have investigated using longer hindfoot nails by comparison with standard TTC nails [4, 16]. Baker et al. have recently published their experience in treating unstable ankle fractures with a retrograde femoral nail used as a long hindfoot nail [16]. Using a femoral nail allows the nail to be inserted to the proximal tibia, which decreases the risk of a stress riser at the mid-tibia. Similar to our findings, they show that this technique is a safe and effective alternative to TTC nailing for the management of unstable ankle fractures in frail elderly patients. All patients in their case series regained their baseline mobility by final follow-up. They also report lower rates of wound complications compared to ORIF.
The technique described in this paper serves as a salvage procedure with indications similar to those for TTC nailing, or a long hindfoot nail, including comminuted intra-articular fractures in low-demand patients, patients at high risk of wound complications or non-constructible high-energy pilon fractures. The novelty is in the added benefit from preserving the subtalar joint. In doing so, the foot can better accommodate to the plane of the floor. While only derived from first principles, the authors also believe that by preserving subtalar motion, the distal locking screws are better protected from impact loading. By locking the distal nail in the talus, the construct can accommodate immediate weight-bearing postoperatively. Similar to using a retrograde femoral nail, these techniques can be useful in carefully selected and appropriately consented patients who would otherwise have difficulty complying with restricted weight bearing or in whom prolonged immobilization is ill-advised.
While the present study has expanded on the current literature concerning the management of unstable ankle fractures in frail elderly patients, it should be interpreted in light of its limitations. Most importantly, the findings presented in this study reflect a small case series of patients that were treated at a single centre in the United Kingdom. The decision whether or not to prepare the tibiotalar joint is a matter of judgement and not evidence based. The authors acknowledge that the technique as proposed, without routine formal joint preparation, is unlikely to result in predictable joint arthrodesis (Fig. 2). We do not believe, however, that this is essential to achieve satisfactory clinical outcomes, in patients with low functional demands. This notwithstanding, after preparation, a sound arthrodesis can be achieved with preservation of the subtalar joint (Fig. 3). A recent study [17] has shown tibiotalar arthrodesis induces compensatory changes in the subtalar joint and so the aim of our technique to preserve accommodative motion may well be open to some challenge in the longer term.
Despite this, however, we argue that in frail elderly patients who need to remain as mobile as possible in order to avoid a potential terminal decline, prioritizing a less disabling gait and a likely reduced risk of peri-prosthetic fracture offers benefit over the risk of subtalar degeneration. Further, larger scale and prospective research is needed to establish whether these theoretical benefits are realized at a population level. Should the concept continue to prove worthwhile, there may also be merit in exploring the design of a purpose-made TTN with bespoke and optimized distal locking options in the talus, as well as a locking hole in the distal tibial segment of the nail.
References:
Strauss EJ, Egol KA (2007) The management of ankle fractures in the elderly. Injury 38(Suppl 3):S2–S9. https://doi.org/10.1016/j.injury.2007.08.005
Thur CK, Edgren G, Jansson KÅ, Wretenberg P (2012) Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: a population-based study of 91,410 Swedish inpatients. Acta Orthop 83(3):276–281. https://doi.org/10.3109/17453674.2012.672091
Hoogervorst P, Bergen CV, Van den Bekerom M (2017) Management of osteoporotic and neuropathic ankle fractures in the elderly. Curr Geriatr Rep 6(1):9–14. https://doi.org/10.1007/s13670-017-0196-y
Al-Nammari SS, Dawson-Bowling S, Amin A, Nielsen D (2014) Fragility fractures of the ankle in the frail elderly patient: treatment with a long calcaneotalotibial nail. The Bone Joint J 96-B(6):817–822. https://doi.org/10.1302/0301-620X.96B6.32721
Hsu RY, Lee Y, Hayda R, DiGiovanni CW, Mor V, Bariteau JT (2015) Morbidity and mortality associated with geriatric ankle fractures: a medicare part a claims database analysis. The J Bone Joint Surg 97(21):1748–1755. https://doi.org/10.2106/JBJS.O.00095
Georgiannos D, Lampridis V, Bisbinas I (2017) Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury 48(2):519–524. https://doi.org/10.1016/j.injury.2016.11.017
Trompeter A (2020) A call to arms: it’s time to bear weight! The Bone Joint J 10-B(4):403–406. https://doi.org/10.1302/0301-620X.102B4.BJJ-2019-1482.R1
Jonas SC, Young AF, Curwen CH, McCann PA (2013) Functional outcome following tibio-talar-calcaneal nailing for unstable osteoporotic ankle fractures. Injury 44(7):994–997. https://doi.org/10.1016/j.injury.2012.11.008
Elmajee M, Gabr A, Aljawadi A, Strang M, Khan S, Munuswamy S, Pillai A, Sprott D (2020) Treatment of fragility ankle fractures using hindfoot nail, systemic review. J Orthop 22:559–564. https://doi.org/10.1016/j.jor.2020.11.006
Elghazy MA, Hagemeijer NC, Waryasz GR, Guss D, O’Donnell S, Blankenhorn B, DiGiovanni CW (2020) Tibial stress fracture following ankle arthrodesis. Foot Ankle Int 41(5):556–561. https://doi.org/10.1177/1071100720907595
Khan U, Kelly MB, Pleat J, Chesser TJ (2011) Orthoplastics: an integral evolution within comprehensive trauma care. Injury 42(10):969–971. https://doi.org/10.1016/j.injury.2011.07.022
Costa ML, Achten J, Bruce J, Tutton E, Petrou S, Lamb SE, Parsons NR, Collaboration UKWOLLF (2018) Effect of negative pressure wound therapy vs standard wound management on 12-month disability among adults with severe open fracture of the lower limb: the WOLLF randomized clinical trial. JAMA 319(22):2280–2288. https://doi.org/10.1001/jama.2018.6452
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 24(8):742–746. https://doi.org/10.1097/00005373-198408000-00009
BOA, BAPRAS (2009) Standards for Trauma. BOAST 4: the management of severe open lower limb fractures: BOA. https://www.boa.ac.uk/resources/boast-4-pdf.html. Accessed 07 Aug 2023
Willett K, Keene DJ, Mistry D, Nam J, Tutton E, Handley R, Morgan L, Roberts E, Briggs A, Lall R, Chesser TJ, Pallister I, Lamb SE, Management AI, (AIM) Trial Collaborators, (2016) Close contact casting vs surgery for initial treatment of unstable ankle fractures in older adults: a randomized clinical trial. JAMA 316(14):1455–1463. https://doi.org/10.1001/jama.2016.14719
Baker G, Mayne AIW, Andrews C (2018) Fixation of unstable ankle fractures using a long hindfoot nail. Injury 49(11):2083–2086. https://doi.org/10.1016/j.injury.2018.07.028
Lenz AL, Nichols JA, Roach KE, Foreman KB, Barg A, Saltzman CL, Anderson AE (2020) Compensatory motion of the subtalar joint following tibiotalar arthrodesis: an in vivo dual-fluoroscopy imaging study. The J Bone Joint Surg 102(7):600–608. https://doi.org/10.2106/JBJS.19.01132
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author(s) declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hasan, Y.O., Bourget-Murray, J., Page, P. et al. Tibiotalar nailing using an antegrade intramedullary tibial nail: a salvage procedure for unstable distal tibia and ankle fractures in the frail elderly patient. Eur J Orthop Surg Traumatol 34, 847–852 (2024). https://doi.org/10.1007/s00590-023-03735-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03735-3