Abstract
Objective
To compare the outcomes of patients with segmental bone loss who underwent repair with the induced membrane technique (IMT) with a matched cohort of nonunion fractures without bone loss.
Design
Retrospective analysis on prospectively collected data.
Setting
Academic medical center.
Patients
Two cohorts of patients, those with upper and lower extremity diaphyseal large segmental bone loss and those with ununited fractures, were enrolled prospectively between 2013 and 2020. Sixteen patients who underwent repair of 17 extremities with segmental diaphyseal or meta-diaphyseal bone defects treated with the induced membrane technique were identified, and matched with 17 patients who were treated for 17 fracture nonunions treated without an induced membrane. Sixteen of the bone defects treated with the induced membrane technique were due to acute bone loss, and the other was a chronic aseptic nonunion.
Main Outcome Measurements
Healing rate, time to union, functional outcome scores using the Short Musculoskeletal Functional Assessment (SMFA) and pain assessed by the Visual Analog Scale (VAS).
Results
The initial average defect size for patients treated with the induced membrane technique was 8.85 cm. Mean follow-up times were similar with 17.06 ± 10.13 months for patients treated with the IMT, and 20.35 ± 16.68. months for patients treated without the technique. Complete union was achieved in 15/17 (88.2%) of segmental bone loss cases treated with the IMT and 17/17 (100%) of cases repaired without the technique at the latest follow up visit. The average time to union for patients treated with the induced membrane technique was 13.0 ± 8.4 months and 9.64 ± 4.7 months for the matched cohort. There were no significant differences in reported outcomes measured by the SMFA or VAS. Patients treated with the induced membrane technique required more revision surgeries than those not treated with an induced membrane.
Conclusion
Outcomes following treatment of acute bone loss from the diaphysis of long bones with the induced membrane technique produces clinical and radiographic outcomes similar to those of long bone fracture nonunions without bone loss that go on to heal.
Level of evidence:
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Segmental bone loss in the setting of acute trauma or fracture nonunion is a challenging problem. External and internal fixation devices can provide mechanical stability to the affected limb, however, without sufficient biological augmentation at the bone loss site, there is a decreased chance for bony healing. As for critical sized defects, mechanical support can falter resulting in catastrophic failure of the implant(s) and residual deformity, pain, and limb dysfunction. These challenges have led to the development of treatment techniques such as bone transport that can be successful in some circumstances, but not all [1]. Furthermore, these procedures require significant patient compliance for daily manipulation of their fixation devices to allow for bone regeneration.
The induced membrane technique (IMT), also known as the Masquelet procedure, is a staged surgical procedure that was first described by Alain Charles Masquelet to repair bone defects resulting from trauma, infection, malignancy, or congenital deformities [2,3,4]. This technique requires one stage of internal fixation of the fracture with implantation of polymethylmethacrylate bone cement into the bone defect which subsequently induces the development of a bioactive membrane around the cement that is rich in bone morphogenic proteins [5,6,7]. At approximately 6 weeks after the first stage, the second stage is performed with removal of the bone cement and preservation of the induced membrane with harvesting and deposition of bone graft into the bone defect. Subsequent bone grafting procedures may be necessary to ensure full consolidation of large defects. Consolidation of large segment defects up to 22 cm have been reported with this technique [8]. The purpose of this study was to evaluate the clinical, radiologic, and patient-reported outcomes of large segment defects of the diaphysis of long bones treated with the IMT, and compare these outcomes to a matched cohort of patients with unhealed diaphyseal fracture without bone loss who underwent repair with bone grafting and fixation.
Patients and methods
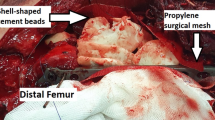
An IRB approved database of all upper and lower extremity fractures treated between September 2013 and December 2020 at a large, urban academic medical center and its affiliate level 1 trauma center was queried for long bone fractures (humerus (OTA 12A-C), radius/ulna (OTA 2R2A-C/2U2A-C), femur (OTA 32A-C), tibia/fibula (OTA 42A-C/4F2A-C) with large segmental bone loss. Inclusion criteria for study analysis was age > 18 years old, use of the IMT as the initial strategy for fracture fixation, and a minimum of twelve months follow-up (Figs. 1, 2) [9]. Large segmental bone loss was defined as any segmental defect > 3 cm. Defect size was measured intraoperatively following debridement using a standard sterile ruler. The induced membrane technique was standardized with the first stage consisting of internal fixation of the fracture with implantation of antibiotic impregnated polymethylmethacrylate bone cement into the bone defect. Antibiotics used were a combination of vancomycin and tobramycin or gentamycin. Six weeks later, the second stage IMT procedure was completed and included incision of the membrane, removal of the cement spacer with preservation of the induced membrane and deposition of bone graft into the bone defect. During the second stage, all defects were cultured to evaluate for infection. Unless there were clinical signs of gross infection, bone grafting proceeded during the second stage. If a culture test returned positive, patients were treated with culture specific intravenous antibiotic therapy under the guidance of an infectious disease specialist for six weeks.
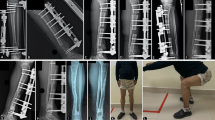
A, B AP plain radiograph and CT scan of the right femur demonstrating a comminuted, displaced, open distal femoral shaft fracture (OTA 31C) with critical size segmental bone defect of 18 cm. C Postoperative AP plain radiograph of the femur immediately after the 1st stage Induced Membrane Technique with nail-plate construct and antibiotic laden cement spacer filling the 18 cm critical size defect; D, E AP and lateral radiographs of the right femur at 2 years after the 2nd stage Induced Membrane Technique bone grafting procedure demonstrating a healed femur fracture with consolidation of the bone graft and no evidence of implant loosening or breakage
A AP plain radiograph of a left femur 1 year after retrograde intramedullary nail fixation of a segmental femoral shaft fracture demonstrating a hypertrophic nonunion of the distal third femoral shaft. B. Immediate postoperative AP plain radiograph of the femur after nonunion repair with iliac crest bone graft and supplemental plate fixation around the femoral nail. C. AP plain radiograph of the femur 1 year after nonunion repair demonstrating consolidation of the nonunion site and no evidence of implant loosening or breakage
In the IMT cohort at the second stage IMT procedure, 16 (94.1%) fractures were treated with autogenous iliac crest bone graft, 12 (70.6%) with reamer-irrigator-aspirator (RIA) autograft, 9 (52.9%) had additional cancellous bone chip allograft used as a volume expander, and 12 (70.6%) also received demineralized bone matrix. Five (29.4%) fractures were treated with 2 different bone graft sources, 3 (17.6%) with 3 different bone graft sources, and 7 (41.2%) with 4 + different bone graft sources.
A cohort of diaphyseal long bone nonunions without bone loss that underwent primary nonunion fixation with autogenous iliac crest bone grafting was identified from the same registry and matched with the IMT cohort in a 1:1 fashion based on fracture, sex, age, Anesthesia Society Association (ASA) class, and smoking status. In the matched cohort at the index nonunion surgery, 16 (94.1%) fractures were treated with autogenous iliac crest bone graft, 1 (5.88%) fracture with reamer-irrigator-aspirator (RIA) autograft, 10 (58.8%) with additional cancellous bone chip allograft, used as a volume expander and 4 (23.5%) also received demineralized bone matrix. 10 (58.8%) fractures were treated with 2 different bone graft sources, 2 (11.8%) with 3 different bone graft sources, and 0 (0.00%) with 4 + different bone graft sources.
In the IMT cohort, the definitive fixation construct was a plate in 4 (23.5%) fractures, an intramedullary nail (IMN) in 4 (23.5%) fractures, a IMN and plate in 5 (29.4%) fractures, and a multiplanar external fixator in 5 (29.4%) fractures. In the matched cohort, the definitive fixation was a plate in 8 (47.1%) fractures, an IMN in 5 (29.4%) fractures, and an IMN and plate in 3 (17.6%) fractures.
Outcomes assessed included healing status, healing time (months), complications, need for revision surgery due to failure of union, Short Musculoskeletal Functional Assessment (SMFA), and Visual Analogue Scale (VAS) for pain. The SMFA is scaled from 0 to 100, with 0 being the best possible score. A 10-point VAS pain score was used with a score of 0 correlating to no pain. All patients in the IMT cohort and the matched cohort were treated by 1 of 4 orthopedic trauma fellowship trained surgeons.
Fractures were considered healed utilizing standardized radiographic and clinical signs of healing. Radiographic union following surgery was determined by the treating orthopedic surgeon and was indicated by the presence of bridging bone on 3 cortices across the fracture site on orthogonal radiographic views. In cases where healing was uncertain, a CT scan was obtained to confirm union. Clinical union was defined as the ability of a patient to fully bear weight with minimal to no pain and swelling. Implant failure was determined by evaluating plain radiographs and comparing the imaging to immediate postoperative radiographs. Implant failure was defined as the loosening or breakage of screws, a plate, or an intramedullary nail.
Bivariate comparisons between the cohort treated with the IMT and the standard nonunion fixation (SNF) cohort was conducted with an independent t-test for analysis of continuous variables and the chi-squared test for categorical variables. Statistical analyses were conducted using SPSS version 25 (Armonk, NY). Significance was set at p < 0.05 for all analyses.
Results
The mean age for the IMT cohort was 47.0 ± 17.3, and 46.4 ± 16.6 for the standard fixation cohort (Table 1). Mean follow-up time for the IMT cohort was 17.06 months ± 10.13. Patients in the matched group had a mean follow-up time of 20.35 ± 16.68. 27.8% patients in each cohort were female. Fracture sites included 8 femurs, 6 tibias, 2 humeri and 1 ulna (Tables 1, 2). Sixteen of the segmental bone defects treated with IMT were due to acute fractures and did not have any prior surgeries. One patient had a 1.5-year-old infected humeral nonunion with bone loss and had undergone three prior surgeries with previous attempts at bone grafting. The patient also had a 1.5-year-old nonunion of the femur which had undergone previous fixation with an intramedullary nail. Both nonunions were the result of the same motor vehicle accident (Table 3).
The mean defect size of the IMT cohort was 8.85 cm (range: 3 – 36 cm). No segmental bone defects from the IMT group were infected based on intraoperative second stage culture results. There were also no infected nonunion fractures in the SNF cohort. Fifteen (88.2%) segmental defects in the IMT cohort achieved healing at a mean 13.0 ± 8.4 months compared to 17 (100.0%) nonunions in the SNF cohort at a mean of 9.64 ± 4.7 months (p = 0.145, p = 0.150) (Table 4). There was no significant difference in baseline SMFA scores between the IMT and SNF cohort (45.2 ± 21.9 vs. 42.2 ± 21.9, p = 0.556). There was also no significant difference in SMFA scores at latest follow up between the IMT and SNF cohorts (19.1 ± 16.5 vs. 18.3 ± 21.8, p = 0.756) (Table 5). No significant differences were observed in patient reported pain at both baseline and the latest follow-up visit (Table 6).
In the IMT cohort, 4 (23.5%) fractures required repeat bone grafting of their segmental bone defect site due to delayed healing. None of these fractures were noted to be infected at their 2nd stage IMT surgery. Of these 4 patients that required repeat bone grafting, 2 patients went on to heal. In the SNF cohort, no patients required repeat bone grafting of their nonunion site due to delayed healing (Table 4).
In the IMT cohort, 3 (17.6%) patients experienced implant complications. Of these 3 patients, one underwent revision fixation and ultimately healed. One patient who did not heal had segmental bone loss of the femoral meta-diaphysis, opted not to undergo revision fixation and instead underwent a distal femoral replacement. This same patient was initially fixed with an IMN and plate construct and refused a second bone grating procedure at 9 months after the second stage IMT procedure when delayed union was noted. He ultimately experienced implant failure at 1.5 years after the second stage IMT procedure with worsening thigh pain, shortening of the leg, and intra-articular penetration of the intramedullary nail into the femoral notch. The other patient who did not heal required 3 revision surgeries and experienced delayed union of the femur. In the SNF cohort one patient experienced implant failure This patient’s femur fracture went on to heal. Patients in the IMT cohort required more revision surgeries than those in the standard fixation cohort (Table 4). Patients in the IMT cohort required a mean 2.4 procedures to heal compared to a mean 1.0 surgeries for patients in the standard fixation cohort.
Discussion
While the IMT has been demonstrated to be a viable option in dealing with critical sized bone defects, little is known about patient outcomes beyond healing. In this study, we find that patient reported outcomes following treatment with the IMT produces outcomes that are similar to those of long bone nonunion fractures that go on to heal. Outcome similarities include rate of healing, time to healing, and changes in scores for the SMFA and VAS pain.
This study is the first to compare long-term outcomes of patients with long bone defects who underwent repair with the IMT to those who did not. Existing literature exclusively reports on outcomes of either the IMT or bone grafting/transport with fixation. Outcomes of standard nonunion fractures treated with bone grafting or transport and plate or nail fixation are well documented. Many tend to heal within a few months of treatment with about 5–10% failing to heal completely. Outcomes of fixation with the IMT, however, can vary.
The healing rate of 88.2% for patients treated with the IMT observed in the present study falls within the range of rates reported in a recent systematic review ranging from 67 to 100% [10]. Similar to the present study, Piacentini et al. 2019 reconstructed 18 posttraumatic bone defects with the IMT. The study reported a healing rate of 72% in 13 out of 18 cases. [11] This healing rate is less than this study’s healing rate. Piacentini et al. did not report an average for time to healing.
Zappaterra et al. 2011 repaired nine cases of upper limb defects with the IMT. This study reported bone union in eight of nine cases repaired. The healing rate for this study is the same as the present study’s rate. This study, however, did not report an average value for time to healing. [12] Moghaddam et al., 2011 repaired 88 femoral non-unions. 41 patients received treatment with a one-step IMT procedure and 47 patients underwent repair with a two-step IMT procedure. The authors of this study do not specify the healing rate, or time to union for patients who were treated solely with the IMT, but do report that 74% of all cases achieved consolidation in an average of 9.3 months. The authors state that the results of their study suggest that the Masquelet technique is an efficient means of eradicating infection in nonunions, and in combination with intramedullary nailing is the ideal method of choice for treatment of femoral shaft nonunions with large defects. [13] A combined achieved 74% rate of union for patients treated with both a one and two-step surgical process indicates a rate of union less than 74% for patients treated solely with the two-step IMT in this study. This percentage would be lower than the present study’s healing rate of 88.2%. Our study is in agreement with this study’s assessment of the IMT’s efficacy for long bone nonunion and defect treatment.
The use of iliac crest bone graft (ICBG) for nonunion repair continues to be the standard among all age groups. 94.4% of fracture nonunions in this study were treated with ICBG. Carlock et al. 2019 found no differences between an elderly and nonelderly cohort with respect to postoperative pain scores, SMFA scores, time to union, and rate of union. Of 242 total patients, 232 (95.9%) achieved union at a mean 7.1 months. This healing rate is comparable to the present study’s rate of 100%. The Carlock et al. reported healing time of 7.1 months is also similar to this study’s healing time of 9.64 months [14]. While elderly patients may be prone to fracture nonunion, Taormina et al., 2014 established that older age is not associated with poorer nonunion surgery outcomes. 80% of patients in Taormina et al. were treated with ICBG or iliac crest aspirate. [15] Iliac crest bone grafting should remain the benchmark procedure for nonunion repair as patient outcomes across all demographics are consistently favorable. Additionally, Konda et al., 2021 established that autogenous ICBG is the gold standard in the management of persistent tibial nonunion regardless of surgical approach for graft placement. [16]
The majority of fracture nonunions treated in this study were femurs and tibias. Femoral and tibial nonunion outcomes tend to be favorable as indicated by the present study’s successful healing rate. Monroy et al., 2014 demonstrated that patients undergoing treatment for a distal femoral nonunion can expect similar outcomes as patients receiving treatment for an acute distal femoral fracture. [17]
Despite the variation in reported outcomes of treatment with the IMT, the majority of the literature points to its effectiveness. Decreases in SMFA scores for both cohorts in the present study also reflect improved function, increased mobility, and a decline in how bothersome the bone defect is for patients treated with the technique. Improvements in these scores also correlate with clinical signs of healing such as increased weightbearing or increased range of motion as has been reported in various studies.
There are some limitations of this study that should be discussed. First, in a small cohort of patients treated by four surgeons, fixation with the IMT may have reduced standardization in surgical technique across all cases. This study also included patients with varied fracture sites, defects, sizes, and anatomy. Our purpose, however, was to evaluate surgical technique rather than the specifics of the fracture. Finally, the sample size for each cohort was small, and a greater sample size may have produced different results. These limitations are fairly common across the existing literature on the IMT, due to the relatively narrow indications for the procedure.
In conclusion, the IMT is an effective surgical procedure that can be used for the treatment of complex large segmental long bone loss. When compared with standard nonunion repair patients, there are no differences observed in major patient reported outcomes, however, the IMT is associated with the need for more unplanned surgical procedures and is best suited for cases of long bone trauma resulting in significant bone loss. These findings should be discussed with patients who are considering this reconstructive option.
References
Bianchi-Maiocchi A, Aronson J (1991) Operative principles of ilizarov. Williams and WIlkins, Baltimore
Azi ML, De Almeida Teixeira AA, Cotias RB et al (2019) Induced-membrane technique in the management of posttraumatic bone defects. JBJS Essent Surg Tech. https://doi.org/10.2106/JBJS.ST.18.00099
Aurégan JC, Bégué T (2014) Induced membrane for treatment of critical sized bone defect: a review of experimental and clinical experiences. Int Orthop 38:1971–1978
Masquelet AC (2003) Muscle reconstruction in reconstructive surgery: Soft tissue repair and long bone reconstruction. Langenbeck’s Arch Surg 388:344–346
El-Hadidi TT, Soliman HM, Farouk HA, Radwan MAEM (2018) Staged bone grafting for the management of segmental long bone defects caused by trauma or infection using induced-membrane technique. Acta Orthop Belg 84(4):384–396
Pelissier P, Masquelet AC, Bareille R et al (2004) Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res. https://doi.org/10.1016/S0736-0266(03)00165-7
Apard T, Bigorre N, Cronier P et al (2010) Two-stage reconstruction of post-traumatic segmental tibia bone loss with nailing. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2010.02.010
Littlefield CP, Wang C, Leucht P, Egol KA (2021) The basic science behind the clinical success of the induced membrane technique for critical-sized bone defects. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.20.00206
Meinberg E, Agel J, Roberts CS (2018) Fracture and dislocation classification compendium. J Orthop Trauma 32:S1–S170
Morelli I, Drago L, George DA et al (2016) Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury. https://doi.org/10.1016/S0020-1383(16)30842-7
Piacentini F, Ceglia MJ, Bettini L et al (2019) Induced membrane technique using enriched bone grafts for treatment of posttraumatic segmental long bone defects. J Orthop Traumatol. https://doi.org/10.1186/s10195-019-0522-6
Zappaterra T, Ghislandi X, Adam A et al (2011) Induced membrane technique for the reconstruction of bone defects in upper limb. A prospective single center study of nine cases. Chir Main. https://doi.org/10.1016/j.main.2011.06.005
Moghaddam A, Thaler B, Bruckner T et al (2017) Treatment of atrophic femoral non-unions according to the diamond concept: results of one- and two-step surgical procedure. J Orthop. https://doi.org/10.1016/j.jor.2016.10.003
Carlock KD, Hildebrandt KR, Konda SR, Egol KA (2019) Autogenous iliac crest bone grafting for the treatment of fracture nonunion is equally effective in elderly and nonelderly patients. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-18-00322
Taormina DP, Shulman BS, Karia R et al (2014) Older age does not affect healing time and functional outcomes after fracture nonunion surgery. Geriatr Orthop Surg Rehabil. https://doi.org/10.1177/2151458514532811
Konda SR, Littlefield CP, Carlock KD et al (2021) Autogenous iliac crest bone grafting for tibial nonunions revisited: does approach matter? Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03735-6
Monroy A, Urruela A, Egol KA et al (2013) Distal Femur Nonunion Patients Can Expect Good Outcomes. Journal of Knee Surgery. https://doi.org/10.1055/s-0033-1349402
Funding
No funding was secured for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this study.
Ethical approval
All ethical standards were complied with in this study.
Informed consent
All subjects enrolled in this study were required to sign an informed consent form and were included in a database approved by, and regularly audited by the Institutional Review Board at our center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Konda, S.R., Boadi, B.I., Leucht, P. et al. Surgical repair of large segmental bone loss with the induced membrane technique: patient reported outcomes are comparable to nonunions without bone loss. Eur J Orthop Surg Traumatol 34, 243–249 (2024). https://doi.org/10.1007/s00590-023-03580-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03580-4