Abstract
Introduction
International joint registries provide high volumes of information in relation to the performance of total knee arthroplasty on a global scale. Distillation of this data can be challenging, particularly with the establishment of more arthroplasty registries on a yearly basis. We therefore aim to present key information from these registries in relation to primary total knee arthroplasty. The specific questions of interest include: Which fixation type is superior in TKA? Does the level of constraint impact on clinical performance? How do partial knee replacements perform in the registries? Does patellar resurfacing lead to superior results? Are there any specific implants which perform particularly well or poorly?
Methods
A comprehensive review of the major English-speaking knee arthroplasty registries across the globe was performed. Given the expanding large number of registries worldwide, it was not possible to perform a comprehensive review of all registries and so, a detailed review of the major English-speaking knee arthroplasty registries was included. Key trends and developments in implant performance were identified and presented in the current article.
Results
Total knee replacements have lower revision rates than both unicompartmental and patellofemoral joint replacement procedures. Patellofemoral joint replacements have the highest failure rate of all knee replacement procedures. Cruciate-Retaining (CR) TKR designs have superior outcomes to Posterior-Stabilized (PS) designs across all registries. Patellar resurfacing appears to confer an advantage over non-resurfaced patellas in primary TKR.
Conclusion
We present current global trends in the utility and performance of TKA based on data from English-speaking arthroplasty registries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
International joint registries provide high volumes of information in relation to the performance of total knee arthroplasty (TKA) on a global scale. Distillation of this data can be challenging, particularly with the establishment of more arthroplasty registries on a yearly basis.
We therefore aim to present key information from these registries in relation to primary total knee arthroplasty. The specific questions of interest include: Which fixation type is superior in TKA? Does the level of constraint impact on clinical performance? How do partial knee replacements perform in the registries? Does patellar resurfacing lead to superior results? Are there any specific implants which perform particularly well or poorly?
Methods
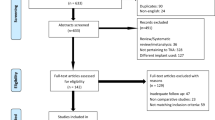
A comprehensive review of the major English-speaking knee arthroplasty registries across the globe was performed. Given the expanding large number of registries worldwide, it was not possible to perform a comprehensive review of all registries and so, a detailed review of the major English-speaking knee arthroplasty registries was included. Key trends and developments in implant performance were identified and presented in the current article.
Results
Fixation
UK [3]
A total of 50,904 knee replacements were registered in the UK National Joint Registry in 2020. A total of 43,421 total knee replacements were performed which accounted for 85.3% of all primary knee replacements in 2020. Fixation methods for primary TKR have consistently favored cemented fixation, rising from 78.4 in 2004 to 83.2% in 2020. In contrast, both cementless and hybrid fixation methods have seen a steady decline in use since 2004. The use of cementless fixation has decreased from 6.3 in 2004 to 1.8% in 2020. Likewise, with hybrid fixation, there has been a similar decrease from 2.7 in 2004 to 0.3% in 2020.
There were 6617 total UKRs performed in 2020 in the UK NJR. The rates of cemented fixation for UKR in 2006 were 8.8% (of the entire knee replacement cohort). This was followed by a decline to 5.8% in 2016 with an increase to 7.9% in 2020. Uncemented and Hybrid fixation in UKR has seen a consistent increase from 0.1 in 2004 to 5.1% in 2020.
A total of 1,136,212 cemented TKAs have been recorded in the UK registry with a 3.23% revision rate at 10 years. For cementless TKA, 47,061 procedures have been reported with a 4.06% revision rate at 10 years. Hybrid cases report at 9,851 total procedures with a 3.58% revision rate at 10 years. Cemented (n = 96,187) and cementless/hybrid (n = 29,268) UKA cases have revision rates of 10.41% and 7.61% at 10 years, respectively.
Australia [2] and New Zealand [5]
In Australia, 86.5% of all knee replacements in 2020 were primary TKR. The most common method of fixation was cemented, accounting for 66.7% of procedures in 2020. The use of cementless fixation accounted for 15.9% of implants in 2020. Hybrid fixation has decreased from approximately 30% in 2003 to 17.4% in 2020. For primary TKA, 654,260 procedures were reported with a revision rate of 4.8% at 10 years. The top three indications for revision were infection (26.4%), loosening (22.7%), and instability (9.5%). A total of 44,380 UKR procedures are reported in the Australian registry, with a revision rate of 13% at 10 years. The top three indications for revision were reported to be progression of disease (36.1%), loosening (33.4%), and pain (7.8%).
The New Zealand registry demonstrated a preference for cemented fixation at 87%. This is followed by uncemented at 9% and hybrid TKR accounting for 3% of all TKRs. Data for cementless or cemented UKR were unavailable. The New Zealand registry reports 4,421 revisions of the 126,603 primary total knee replacements with a rate of 0.47 per 100 years. Further breakdown showed a rate per 100 years of 0.46 for cemented, 0.64 for cementless, and 0.52 for hybrid TKAs. Patellofemoral joint replacement (PFJR) had 85 recorded revisions of a total 746 procedures, giving a rate of 2.03 per 100 years. Finally, there were 1245 revisions of the 14,730 UKAs with a reported revision rate of 1.15 per 100 years.
USA [4] and Canada [5]
Latest data from the American Joint Replacement Registry (AJRR) show a substantial increase in the usage of cementless TKR. There has been an increase from 1.9 to 14.2% between 2012 and 2020. In the same period, hybrid fixation has seen a decrease from 3.9% to 2.4%. The AJRR data show similarities to the NJR data with current usage of cemented TKR being steady at 83.4%. Consistent with the data from Australia, UKR has decreased from 9.1 to 4.2% between 2012 and 2020. As seen with the UK and AJRR registry, PFJR remains a small portion of knee replacements, making up 0.4% of all knee replacements. The AJRR reports a lower revision rate for cementless fixation when compared to cemented fixation in males ≥ 65 years (HR 0.755), and all patients < 65 years of age (HR 0.785). This difference was only seen in males and was not statistically significant for females for either age group.
Canadian Joint Replacement Registry data show that 90.9% of all knee replacements were TKR, 8.8% UKR, and 0.3% PFA in 2020. Specific data on type of fixation and outcomes were unavailable.
Constraint
UK [1]
The UK NJR data show that cruciate-retaining designs remain the most popular option for constraint. From 2004 to 2020, there has been an increase in cemented, cruciate-retaining forms of knee replacement from 56.3 to 63% while uncemented cruciate retaining reduced from 5.7 to 1.8% in the same time period.
Posterior-stabilized implants account for 24.9% of cemented, 7.3% of uncemented, and 8.3% of hybrid TKRs in 2020. Other forms of constraint remain a small proportion of TKRs, regardless of the fixation type.
Revision rates with CR designs were 4.49% and 5.50% at 17 years for cemented and cementless TKRs, respectively. At 17 years, PS had a revision rate of 5.63% for cemented TKRs and 8.81% for cementless designs. For primary cemented pre-assembled–hinged/linked constraint TKR, a revision rate of 10.65% has been reported at 15 years, which is the highest revision rate of all constraint type.
Australia [2] and New Zealand [3]
In the Australian registry, cruciate-retaining prostheses have consistently been the most utilized prostheses, with a minimal change from 77 in 2003 to 73.9% in 2020. Posterior stabilization had a peak of 36% in 2007, with a decline to 16.3% in 2020. Medial pivot design (MPD) has seen an increase between 2003 and 2020 from 3% to 9.8%. Fully constrained and hinged designs were used in less than 0.5% of all primary TKRs.
As seen with the UK NJR data, PS implants have higher revision rates compared to cruciate-retaining and medial pivot designs (MPD) at 15 years (7.5% vs 6.1% and 6.0%, respectively). In all forms of stability, the top two indications for revision were loosening (26.4%) and infection (22.7%). MPD prostheses had a higher incidence of revision for pain and instability compared to cruciate-retaining designs.
The New Zealand registry classifies stabilization as posterior-stabilized (PS), cruciate retaining (CR), and other (minimally stabilized). Registry data report an increase in CR from 47 in 2008 to 75% in 2020. Posterior stabilization has seen a reduction from 40 to 20% over the same time period. Other forms of stabilization have also seen a significant drop from 15 to less than 2% from 2008 to 2020.
Consistent with the NJR data, PS implants have been shown to have a significantly higher revision rate when compared to cruciate-retaining implants with a rate of 0.61/100 component years for PS compared to 0.41/100 component years for CR implants. Other forms of stabilization have revision rates of 0.46/100 component years.
USA [4] and Canada [5]
The American Joint Replacement Registry (AJRR) shows a decline in posterior stabilization from 52.6 to 44.5% between 2012 and 2020. In the same time period, cruciate retaining has seen an increase from 42.2 to 46.2% and ultracongruent designs up to 9.1% from 4.9. As seen in the UK NJR, Australian and New Zealand registries ultracongruent and cruciate-retaining designs have significantly lower rates of revision compared to posterior stabilization. At the 9-year mark, the age-adjusted hazard ratio of cruciate retaining vs posterior stabilization for revision was 0.810 (CI 0.756, 0.867 p < 0.0001) for males and 0.747 (CI 0.702, 0.79 p < 0.0001) for females.
The Canadian Joint Replacement Registry also does not report on current utilization across different stability types. However, the registry does report on revision rates for both level of constraint and patella resurfacing along with constraint and bearing type. Posterior stabilization with or without patella resurfacing had statistically higher revision rates at the 7-year mark when compared to cruciate-retaining stabilization (PS with resurfacing 3.28% vs CR with resurfacing 2.49%; PS with no resurfacing 4.01% vs CR with no resurfacing 3.38%). Taking into account the bearing type, PS with mobile bearing had the highest revision rate after 7 years at 7.45%.
Partial knee replacement
UK [4]
Total knee replacements continue to be the primary form of knee replacement comprising a total of 87.9% of all primary knee operations. This was followed by UKR at 9.3% and PFJR at 1.2% since the UK registry was created. An increase in UKA is seen from 8.1% in 2004 to 13% in 2020, while PFJR has remained largely consistent at 1%. The data from 2020 show that the majority of UK surgeons performing TKR are higher volume surgeons, performing greater than 49 TKRs a year, while the majority of surgeons performing UKR perform between 13 and 48 cases per year. The average volume of a surgeon performing PFJ replacement was between 7 and 12 cases a year.
In terms of revision rates, UKRs do significantly worse when compared to TKR with almost double the chance of revision at all time points from 1 to 15 years. Specifically, there are a total of 96,187 reported cemented UKR procedures with a revision rate of 15.74% at 15 years. Cementless/hybrid UKRs have a total of 29,268 cases reported with a revision rate of 11.52% at 15 years (less than 250 cases remained at this time point).
Australia [2] and New Zealand [6]
In the Australian registry, primary total knee replacements accounted for 86.5% of all knee replacements, while primary partial knee replacements made up 6.2%, and revision surgery accounted for 7.3% of the remaining procedures. Total knee replacements had the lowest rate of revision, with a revision rate of 8.1% at 20 years. Infection was the main indication for revision, followed by loosening, instability, and patellofemoral pain. Within partial knee replacements, unicompartmental is the commonest at 92.8% and is followed by PFJR at 6.6%. The use of UKR has decreased from 14.5% of all knee procedures in 2003 to 5.7% in 2020. UKR is also associated with a higher rate of revision with revision rates of 13% at 10 years and 30.7% at 20 years. PFJRs show a higher rate of revision with 24.5% requiring revision at 10 years.
New Zealand shows similar results as the Australian and UK registry, with TKR constituting 89.1%, UKR 10.4%, and PFJR 0.5% of all knee replacement procedures. UKR revision rates were 1.07/100 component years, more than double that of a TKR, with 24% of all UKR requiring a revision by the 20-year time point. PFJR revisions took place at a rate almost 4 times that of a TKR at 2.03/100 component years.
USA [3] and Canada [5]
American data registry shows that UKR has seen a decreasing prevalence between 2012 and 2017, down to 2.7% of all primary total knee arthroplasties; however, most recent data from 2020 show an increase to 4.2%. PFJR usage is similar to that seen in other registries at 0.4% of all primary total knee procedures in 2020. TKR constituted 88.6% of all knee replacement procedures between 2012 and 2020. Revision rates for each subtype of knee replacement were not reported in percentage form. However, the cumulative incidence of revision was considered to be significantly higher with UKR when compared with primary TKR, but this was seen in females over the age of 65 only (Hazard ratio: 1.283, p < 0.0002). In males over the age of 65, no statistical difference was seen when comparing UKR vs Total knee replacement (HR 0.875, p = 0.0659).
Canadian Joint Replacement Registry data do not indicate the breakdown of UKR, TKR, and PFJR as a percentage of total knee replacement procedures. However, the registry demonstrates that TKR with patellar resurfacing has the lowest revision rate at 7 years’ time. The reported revision rate for TKR with patellar resurfacing was 2.92%, followed by TKR without resurfacing at 3.87%, medial UKR at 7.42%, lateral UKR at 7.84%, and PFJR having the highest revision rate at 10.51% at the 7-year mark.
Patellar resurfacing
UK [4]
A total of 1,193,125 total knee replacements are registered in the UK registry, with 458,640 (38.44%) undergoing patellar resurfacing, and 734,485 (61.56%) without patellar resurfacing. The revision rate at 17 years is 4.28% for TKR with patellar resurfacing and 5.18% without.
Australia [2] and New Zealand [6]
The Australian registry reports a significant increase in the amount of TKRs undergoing patellar resurfacing with an increase from 44 in 2003 to 75.4% in 2020. There are a total of 654,260 TKRs reported in the registry, with 386,174 (59.02%) undergoing patellar resurfacing, and 268,086 (40.98%) without. At 20 years, TKRs with patellar resurfacing had a revision rate of 7.1% compared to 9.2% without. The New Zealand registry does not report data on TKRs with patellar resurfacing procedures.
USA [3] and Canada [5]
AJRR shows a consistently high usage of patellar resurfacing in total knee arthroplasty. In 2012, 95.9% of all total knee arthroplasty procedures underwent patellar resurfacing, this has seen a slight decrease to 90.4% in 2020. Consistent with data from the Australian and UK registry, there is decreased revision rate when comparing patellar resurfacing against the unresurfaced patella in individuals above the age of 65. This was only statistically significant in females (HR 1.419, p < 0.0001) and not in males (HR 1.150, p = 0.0528). The Canadian Joint Registry reports a total of 60,209 total joint replacements in 2019–2020. There were 32,878 (54.61%) TKRs with patellar resurfacing and 27,331 (45.39%) without resurfacing. The CJRR data on revision in the setting of patellar resurfacing are congruent with the other reported registry data. At the 7-year mark, TKRs with patellar resurfacing had a revision rate of 2.92% compared to 3.87% for TKRs without patellar resurfacing. The cumulative percent revision was statistically higher for TKRs without patellar resurfacing (HR 1.20 and p < 0.0001).
Specific implant performance
UK [4]
For TKR, the top three implants combinations (with at least 250 cases at risk at a given time point) with the lowest revision rates at 15 years were the PFC Bicondylar Sigma (3.28% 15-year revision rate), Genesis II (3.49% 15-year revision rate), and the Profix (3.76% 15-year revision rate).
For UKR, the top three implant combinations (with at least 250 cases at risk at a given time point) with the lowest revision rates at 10 years were the Oxford Cementless Partial knee (5.85% 10-year revision rate), Physica ZUK (5.87% 10-year revision rate), and the Sigma HP (6.43% 10-year revision rate).
There were only 5 available brands for patellofemoral replacements, and only 3 having sufficient number of cases. The top three hybrid implant combinations (with at least 250 cases at risk at a given time point) with the lowest revision rates at 10 years were the Avon (14.74% 10-year revision rate), FPV (19.31% 10-year revision rate), and the Journey PFJ Oxinium (21.97% 15-year revision rate).
Australia [2] and New Zealand [6]
The top three implant combinations for cemented TKR (with at least 400 procedures listed) with the lowest revision rates at 10 years were the Nexgen CR Flex (Fem): Natural Knee II (Tib) (2.2% 10-year revision rate), Columbus (2.4% 10-year revision rate), and Nexgen CR Flex (2.9% 10-year revision rate). The top three implant combinations for uncemented TKR (with at least 400 procedures listed) with the lowest revision rates at 10 years were the Nexgen LPS (Fem): Nexgen TM LPS (tib) (2.8% 10-year revision rate), Natural knee flex (Fem): Natural Knee II (Tib) (3.0% 10-year revision rate), and the Nexgen CR (3.0% 10-year revision rate).
The top three implant combinations for hybrid TKR (with at least 400 procedures listed) with the lowest revision rates at 10 years were the Nexgen CR Flex (2.4% 10-year revision rate), Natural Knee Flex (Fem): Natural Knee II (Tib) (2.6% 10-year revision rate), and the Nexgen CR Flex (3.0% 10-year revision rate).
In the Australian registry, the top three implant combinations for UKR (with at least 200 procedures listed) with the lowest revision rates at 10 years were the Sigma HP (7.5% 10-year revision rate), ZUK (8.1% 10-year revision rate), and the BalanSys Uni (8.1% 10-year revision rate).
New Zealand registry data report on the revision rate/100 component years. When analyzing implants with a minimum of 3000 observed component years (i.e., minimum 300 cases with a minimum of 10 years), the top three unicompartmental prosthesis combinations were the ZUK (revision rate of 0.52/100 component years), Oxford 3 uncemented (revision rate of 0.84/100 component years), and the Miller/Galante (revision rate of 1.0/100 component years).
The top three performing cemented combinations with a minimum of 3,000 observed component years (i.e., minimum 300 cases with a minimum of 10 years) were the Duracon (revision rate of 0.329/100 component years), PFC Sigma (revision rate of 0.357/100 component years), and the Sigma (revision rate of 0.371/100 component years).
The top three performing hybrid combinations with a minimum of 3,000 observed component years (i.e., minimum 300 cases with a minimum of 10 years) were the Duracon (revision rate of 0.316/100 component years), LCS (revision rate of 0.44/100 component years), and the Nexgen (revision rate of 0.44/100 component years).
For uncemented prostheses, there were only two combinations with a minimum of 3000 observed component years (i.e., minimum 300 cases with a minimum of 10 years) which were the Duracon (revision rate of 0.209/100 component years) and the LCS (revision rate of 0.728/100 component years).
USA [3] and Canada [5]
The American Joint Replacement Registry (AJRR) reports on 7-year cumulative revision rates for cemented and hybrid TKA implant combinations only. The top three performing combinations in the AJRR for cemented TKR were Nexgen Pegged (1.16% revision rate at 7 years), PFC Sigma (1.32% revision rate at 7 years), and Nexgen CR Flex (1.39% revision rate at 7 years). There were only 3 reported hybrid TKA implant combinations with revision data at the 7-year mark. These included the PFC Sigma CR (1.29% revision rate at 7 years), Triathlon CR (2.07% revision rate at 7 years), and Vanguard CR (Fem): Maxin (Tib) (2.90% revision rate at 7 years).
Specific implant combination revision rates were not available for the Canadian Joint Replacement Registry. A summary of the above findings is demonstrated in Table 1.
Discussion
This current review of English-speaking International Joint registries provides a valuable insight into trends emerging in the field of knee arthroplasty. Understanding the current utility and performance of the various fixation methods, levels of constraint and subtotal arthroplasty allow the global arthroplasty community to refine its approach to knee arthroplasty procedures in general.
Fixation
Data show a continually high utilization of cemented TKA across English-speaking registries; however, there has been an increase in cementless TKA in the AJRR and Australian registries. A meta-analysis conducted by Prasad et al. compared the outcomes of cemented vs cementless primary TKA and found no significant difference in revision rates and function at an average 8.4-year follow-up [9]. An additional meta-analysis by Zhou et al. further confirmed these results, indicating no difference in survivorship and functional outcomes when analyzing 7 studies with a mean follow-up of 7.1 years [11]. The UK and New Zealand registry showed higher revision rates for cementless TKA at the 10-year mark, while the AJRR reported a statistically significant lower revision rate for cementless TKA in males over 65 and all patients younger than 65 between the years of 2012 and 2020. Further data in the registry and longer follow-up studies are needed to analyze the performance of cementless versus cemented TKA.
UKA
Across all registries, a consistent trend was seen with decreased usage and higher revision rates for UKA compared to TKA. In the UK registry, there was a greater than double the revision rate seen at all times points from 1 to 15 years [4]. Migliorini et al. compared UKA and TKA in a meta-analysis of 13,879 patients with a mean follow-up of 42.69 months. This study showed that UKA had significantly higher revision rates (OR 2.16, p < 0.0001) with better functional outcomes and shorter hospital stays compared to TKA [7]. These results were further corroborated by Wang et al. in their meta-analysis of 54 studies and a total of 4,577 patients [10]. The group concluded that UKA had statistically significant higher revision rates but was associated with fewer early complications such as pain and blood loss with superior functional scores and decreased surgical times when compared to TKA [10]. Careful consideration should be given when selecting patients for UKA as there is clear evidence of significant increase in revision rates seen in the literature; however, there are numerous reported short-term benefits associated with its use.
Constraint
All registries have shown an inferiority with PS implants compared to non-PS unconstrained implants. The exact reason for the poorer performance of the PS implants is not entirely clear, but it may be related to some inherent weakness in the polyethylene post of the PS polyethylene insert. Evidence from the senior author has highlighted the potential for post fracture, particularly with HXLPE (highly cross-linked polyethylene) liners [1]. With the increased adoption of CR implants, especially with condylar stabilized or equivalent designs, PS designs are likely to continually decline in utility moving into the future, particularly with the concern over higher revision rates compared to their CR counterparts.
Patellar resurfacing
The issue around whether or not to resurface a patella in knee arthroplasty is a well-established point of contention. The proponents of resurfacing will claim that revision for anterior knee pain is lower as the PFJ degeneration as a pain generator has been addressed. However, there is evidence to suggest that in the unresurfaced TKA with persistent anterior knee pain, revision to resurface the patella does not address the persistent anterior knee pain in the majority of cases [8]. It is not clear why TKA with resurfaced patellae perform better in these registries. It may be the case that revision to a patellar resurfacing exclusively is a relatively simple procedure, and so, a lower threshold exists for undergoing subsequent revision when compared to the already resurfaced cohort.
Robotic assistance
The inclusion of data from robotically assisted arthroplasty is a new feature of the registries and will become more prominent and meaningful as the years progress. To date, the UK National Joint Registry does not report any robot-assisted or computer-navigated knee replacement data. The Australian Joint Registry reports that technology-assisted total knee replacements (computer navigation, image derived instrumentation, and robotic assistance) account for 60% of all primary knee procedures in 2020. A total of 17,353 robotic-assisted TKR procedures have been recorded since 2017, and in 2020 robotic-assisted TKR accounted for 16.6% of all primary total knee replacement procedures. Robotically assisted TKR had a revision rate of 1.9% at the 3-year mark which was lower than not robotically assisted which was 2.3 (HR 0.80, p = 0.009). Registry data showed that in patients aged ≥ 65 years, the use of robotic-assisted TKR leads to lower revision rates compared to not robotically assisted TKR procedures (HR = 0.74, p = 0.007). This same difference was not seen in individuals < 65 years (HR 0.96, p = 0.713). The New Zealand Joint registry reported a total of 126,607 total knee replacements with 15% (19,000) requiring surgical adjuncts in the form of computer navigation (18,753), robotic-assisted (235), and patient-specific guides (12).
The American Joint Replacement Registry and the Canadian Joint Registry do not report any robot-assisted or computer-navigated knee replacement data.
Conclusion
We present current global trends in the utility and performance of TKA based on data from English-speaking arthroplasty registries.
References
Diamond OJ, Howard L, Masri B (2018) Five cases of tibial post fracture in posterior stabilized total knee arthroplasty using prolong highly cross-linked polyethylene. Knee 25(4):657–662. https://doi.org/10.1016/j.knee.2018.05.005
https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2018th%20Annual%20Report%202021.pdf
https://www.cihi.ca/sites/default/files/document/cjrr-full-annual-report-2019-2020-en.pdf
https://www.nzoa.org.nz/sites/default/files/NZJR_22_Year_Report_Final.pdf
Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J (2019) Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol Orthop Traumatol 29(4):947–955. https://doi.org/10.1007/s00590-018-2358-9
Mockford BJ, Beverland DE (2005) Secondary resurfacing of the patella in mobile-bearing total knee arthroplasty. J Arthroplasty 20(7):898–902. https://doi.org/10.1016/j.arth.2005.02.009
Prasad AK, Tan JHS, Bedair HS, Dawson-Bowling S, Hanna SA (2020) Cemented vs. cementless fixation in primary total knee arthroplasty: a systematic review and meta-analysis. EFORT Open Rev 5(11):793–798. https://doi.org/10.1302/2058-5241.5.200030
Wang H, Ma Q, Ma B (2021) Unicompartmental versus total knee arthroplasty for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trial. Int J Surg Global Health 4(2):e51–e51. https://doi.org/10.1097/GH9.0000000000000051
Zhou K, Yu H, Li J, Wang H, Zhou Z, Pei F (2018) No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 53:312–319
Funding
No funding was received in relation to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Arsh Sidhu declares that there is no conflict of interest to disclose in relation to this work. Gerard A. Sheridan declares that there is no conflict of interest to disclose in relation to this work. Nelson V. Greidanus declares that there is no conflict of interest to disclose in relation to this work. Michael E. Neufeld declares that there is no conflict of interest to disclose in relation to this work. Lisa C. Howard declares that there is no conflict of interest to disclose in relation to this work. Bassam A. Masri declares that there is no conflict of interest to disclose in relation to this work. Donald S. Garbuz declares that there is no conflict of interest to disclose in relation to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sidhu, A., Sheridan, G.A., Greidanus, N.V. et al. International primary knee arthroplasty registry review: findings from current reports. Eur J Orthop Surg Traumatol 33, 2729–2735 (2023). https://doi.org/10.1007/s00590-023-03521-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03521-1