Abstract
Background
The purpose of this study is to assess the short-term survivorship of a new uncemented TKA design in a high-volume centre to evaluate the safety of this design prior to widespread adoption.
Methods
We performed a retrospective cohort study of all primary TKAs (cemented and uncemented) between May 2018 and May 2019. Primary outcome variables included aseptic revision, all-cause revision, time to revision, operative time and radiological outcomes. Predictor variables considered included age, gender, BMI, ASA, implant type (cruciate-retaining, posterior-stabilised or totally-stabilised) and the use of cemented or uncemented implants.
Results
There were 300 cemented TKAs and 249 uncemented TKAs (Triathlon, Stryker Inc., Mahwah, NJ) implanted. The mean follow-up for all cases was 31.6 months (minimum follow-up 2 years). Of the entire 549 implants only 4 were revised. Two of these were for infection, 1 was for patellar maltracking and 1 was for knee stiffness. All 4 revisions occurred in the cemented cohort. The aseptic revision rate in the cemented cohort was 0.7% compared to 0.0% in the uncemented cohort (p = 0.298). Operative times were significantly reduced in the uncemented cohort from 57.9 to 51.7 min (p < 0.001). There were 8/300 (2.6%) patients with RLLs in the cemented cohort and 4/249 (1.6%) patients with RLLs in the uncemented cohort (p = 0.56).
Conclusion
The uncemented Triathlon TKA demonstrates excellent survivorship at short-term follow-up when compared to the cemented Triathlon TKA, thus eliminating any potential clinical concerns with this novel implant in the early post-operative phase.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uncemented total knee arthroplasty (TKA) has had a turbulent evolution over the past few decades due to historical mechanisms of failure which included aseptic loosening, the presence of radiolucent lines and tibial tray screw track osteolysis [3]. Some have reported major issues with early loosening of uncemented patellar components within the first 2 years after uncemented TKA [11]. One of the most characteristic failings with the early generation uncemented TKA was tibial tray subsidence with medial tibial collapse [12]. Barrack et al. [1] reported an 8% revision rate at 2 years for tibial tray subsidence in a mobile bearing uncemented TKA compared to a 0% revision rate for the same indication in cemented TKA of the same design. Inadequate bone ingrowth into the tibial tray in early generation uncemented technology is felt to be the cause of these short-term failures in these early uncemented TKA designs. Newer tibial tray designs, such as the uncemented Triathlon Tritanium TKA (Triathlon, Stryker Inc., Mahwah, NJ), include bullet cruciform pegs that increase the contact surface area, thus reducing early micromotion (Fig. 1). This adds to the overall stability of the construct. In addition, by having the tibial implant as a three dimensionally printed implant, the porous substrate is a part of the implant and is not a coating that can potentially shear off. Also, the porous ingrowth surface has a theoretically higher ingrowth potential compared to the porous coating of previous generation cementless implants, due to the enhanced porous design, similar to revision acetabular components. This has the ability to potentially guarantee better bone ingrowth.
Improvements and technological advancements in uncemented design, improved operative times, higher patient demand, increased load due to escalating prevalence of obesity and a hopeful increase in implant longevity have allowed uncemented TKA to make a return to the field of arthroplasty with many designs having been recently approved for the market. The purpose of this study is to assess the short-term survivorship of a new uncemented TKA design in a high-volume single-centre study.
Materials and method
We performed a retrospective cohort study at a single-centre between May 1st 2018 and May 31st 2019. We included consecutive primary Triathlon TKAs (Stryker, Mahwah, NJ, USA) (cemented and Tritanium uncemented designs) implanted during this time. When the patella was resurfaced, a cemented patella was used. The primary outcome variables included aseptic revision, all-cause revision, time to revision (months) and operative time (minutes). Secondary outcome measures included radiological outcomes which included the presence of tibial tray subsidence and radiolucent lines on post-operative radiographs (Fig. 2). A radiolucent line (RLL) was defined as a gap measuring 2 mm or greater at the bone-implant interface for cementless implants or bone cement interface for cemented implants [9]. The location of RLLs was reported in accordance with The Knee Society roentgenographic evaluation and scoring system [5]. Predictor variables included age, gender, BMI, ASA, femoral implant type (cruciate-retaining (CR), posterior-stabilised (PS) or totally-stabilised (TS)) and the use of cemented or uncemented implants. The follow-up time for all patients was recorded.
Statistics
Demographic data were analysed using descriptive statistics. Interval variables were expressed using mean values, standard deviations and 95% confidence intervals. When assessing the predictors of aseptic revision, the chi-squared (χ2) test was used for bivariate categorical predictor variables. For interval predictor variables, simple logistical regression analysis was used. When analysing the impact of fixation type on operative time, the two independent samples T-test was used. Univariate analysis was performed for each predictor variable relative to each outcome variable. The two-sample Kolmogorov–Smirnov test for equality of distribution functions was used to assess for normal distribution of data. Kaplan—Meier curves using all-cause revision as the failure point were generated for both the cemented and uncemented TKA cohorts. A p-value of less than 0.05 was taken to be statistically significant. The statistical software package used was Stata/IC 13.1 for Mac (64-bit Intel).
Results
Demographics
In total there were 300 cemented TKAs (Triathlon, Stryker Inc, Mahwah, NJ) and 249 uncemented TKAs (Triathlon, Stryker Inc, Mahwah, NJ) implanted during the study time period. Data were distributed normally as per the two-sample Kolmogorov–Smirnov test for equality of distribution functions (p = 0.337). When assessing inter-group variability, there were no differences noted in BMI and ASA grades. The mean BMI in the uncemented cohort was 31.6 (σ = 6.35, 95% CI 30.8–32.4). The mean BMI in the cemented cohort was 32.2 (σ = 6.91, 95% CI 31.4–33.0).
In the uncemented cohort, there was a significantly increased association with male gender (p < 0.001), younger age (p < 0.001) and CR femoral implants (p < 0.001). In the uncemented cohort, 43.7% were female compared to the cemented cohort where 78.3% were female (p < 0.001). The mean age in the uncemented cohort was 62.5 years (σ = 8.26, 95% CI 61.5–63.5), compared to 68.4 years (σ = 10.58, 95% CI 67.2–69.6) in the cemented cohort (p < 0.001). For the uncemented cohort (n = 249), 77.8% were CR femoral implants, 18.2% were PS implants and the remainder were TS implants. For the cemented cohort (n = 300), 36.8% were CR implants, 49% were PS implants and the remainder were totally-stabilised implants (p < 0.001).
Revision
Of the entire 549 implants in both groups, only 4 knees were revised. Two of these were for infection, 1 was for patellar maltracking and 1 was for knee stiffness. All 4 revisions occurred in the cemented cohort. Therefore, the overall all-cause revision rate for the cemented cohort was 1.3% compared to 0.0% in the uncemented cohort. The aseptic revision rate in the cemented cohort was 0.7%.
When analysing the predictors of aseptic revision, it was found that age, gender, BMI, ASA grade, use of cement and implant type all had no predictive effect on the risk of aseptic or all-cause revision in this cohort. A Kaplan–Meier curve was generated to demonstrate all-cause revision at the point of failure up to 2 years post-operatively (Fig. 3). All-cause survival was 98.7% in the cemented cohort and 100% in the uncemented cohort.
Radiographic outcomes
For all cases, there was no evidence of tibial tray subsidence in both the cemented and uncemented cohorts. In total, RLLS were noted in 2.1% of patients. There were 8/300 (2.6%) patients with RLLs in the cemented cohort and 4/249 (1.6%) patients with RLLs in the uncemented cohort (p = 0.56). Seven patients were noted to have RLLS in the femur. The commonest area for RLLS in the femur was zone 2 (n = 4). Four patients were noted to have RLLs on the anterior tibial radiograph. The commonest areas in the tibia for RLLs were zones 1, 2 and 4 (n = 2). Five patients were noted to have RLLs on the lateral tibial radiograph with the commonest zones involved being zone 1 and 2 (n = 2). Mean time to radiographic follow-up for the entire cohort was 9 months (σ = 8.9, range 0–36).
Operative time
The mean operative time was significantly shorter in the uncemented cohort at 51.7 min (σ = 12.82, 95% CI 50.1–53.3) compared to 57.9 min (σ = 13.67, 95% CI 56.3–59.4) in the cemented cohort (p < 0.001).
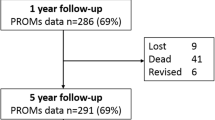
Follow-up
The mean follow-up for all cases in this study was 31.6 months (σ = 3.05, range 27–40). Mean follow-up was 32.2 months (σ = 3.25, range 31.8–32.6) in the cemented cohort and 30.8 months (σ = 2.57, range 30.4–31.1) in the uncemented cohort. No cases were lost to follow-up. At final review, there were no patients from either cohort that were awaiting revision.
Discussion
Many studies projecting the future burden of TKA have confirmed an expected significant increase in the demand for this procedure [18]. There has been a shift in the demographic demanding TKA toward a younger, fitter cohort in the context of an overall more obese population [7]. As such, implant longevity is more of an emphasis which mandates that newer uncemented technologies should be explored. These newer technologies may offer long-term osseointegration which may be preferable in a higher demand population to cemented implants [6]. The improved manufacture of porous metal and its incorporation into the 3D printed tibial component, and the enhanced fixation with the bullet cruciform peg had improved initial fixation to allow predictable bone ingrowth and survivorship of modern cementless tibial components as in the Triathlon Tritanium tibial component. Other benefits include shorter operative times and the ability to avoid using cement in the procedure [7].
Regarding the individual TKA components, uncemented femoral fixation has been proven to be comparable to cemented femoral components in some studies [2]. Hybrid fixation with uncemented femoral components and cemented tibial components has been shown to be superior to fully cemented TKA [10]. Of all the variables to consider, the type of tibial fixation appears to be the most consequential when considering uncemented TKA as a regularly inserted implant in the future arthroplasty procedures. Recent registry data have demonstrated inferior results of uncemented TKA designs when compared to both cemented and hybrid designs [15]. As such, uncemented TKA fixation may still be problematic.
Recent efforts to alter tibial baseplate designs have proven effective [4]. The addition of pegs to the tibial baseplate have been shown to improve mechanical stability. The porous structures of the Triathlon Tritanium Baseplate are strategically positioned on the proximal portion of the cruciform pegs and keel to avoid porous metal in the distal areas. This may reduce the risks of stress shielding and therefore address the issue of suboptimal uncemented tibial tray outcomes.
Recent radiostereometric analyses of this specific uncemented Triathlon tibial baseplate have also demonstrated excellent results with no concerning tibial migration [8, 19]. Based on these promising results, the senior author and the entire surgeon group saw merit in transitioning to the uncemented Triathlon TKA design with a view to supporting further advancements in new technology. This current study assesses the early outcomes of this implant to ensure that it is safe to use with no concerning clinical results in the short term.
A recent prospective randomised trial of 205 knees confirmed excellent survivorship of two uncemented TKA designs at long-term follow-up of 10 years [9]. In this study by Hegarty et al., it was found that the addition of a HA coat and tibial pegs reduced the incidence of radiolucent lines, demonstrating the importance of both biological and mechanical factors in determining the success of new uncemented technologies [9]. The use of uncemented technology has also been shown to be superior for more complex TKA cases including revision TKA requiring stemmed prostheses [17]. Traditionally, the uncemented TKA has been reserved for young healthy male patients. In the current study, we note a higher rate of younger males in the uncemented TKA cohort as this has often been used as a surrogate marker for good bone that will support the process of osseointegration. Recent literature, however, has shown that uncemented TKA may now be suitable for patients that are elderly, obese or suffering from rheumatoid arthritis and osteonecrosis [16].
We describe the excellent survivorship at short-term follow-up of the uncemented Triathlon TKA which has recently been introduced to the market. A recent prospective randomised controlled trial analysing this same implant included 147 patients and demonstrated a significantly lower operative time in the uncemented cohort with no aseptic failures at two years follow-up [14]. We report a much larger cohort size of 549 implants with no aseptic failure in any uncemented implant. We also demonstrate a significantly shorter operative time in the uncemented cohort when compared to the cemented cohort. Other retrospective studies of the uncemented Triathlon TKA confirm similar excellent short-term results to the current study with patient sample sizes ranging from 128 to 400 in total [13, 14]. We describe the largest cohort of the uncemented Triathlon TKA from a single-centre in the literature to date.
One multicentre trial analysing 699 uncemented Triathlon TKAs has shown that the uncemented Triathlon has similar aseptic failure rates and time to failure as the cemented Triathlon [20]. Further multicentre large-scale trials will need to be performed in the future to analyse this implant as it progresses from short-term through mid-term into long-term follow-up times.
Limitations
As this was a retrospective study, there are limitations inherent to this design. Confounding variables can be problematic in retrospective studies and in an effort to combat this, we reported bivariate as well as multivariate analysis by way of regression analysis. This study is also reflective of surgeon bias, particularly when deciding the use of cementless vs cemented implants, early in our experience. The decisions made in these patients; however, reflect real-life decisions that are part of every-day surgical decision making, and do play a role in answering this clinical question. Future prospective studies would help to reduce this bias, because now most patients undergo cementless fixation at our centre.
A limitation of our study was the higher rate of younger males in the uncemented TKA cohort. The discrepancy between the group baseline characteristics can be explained by an intentional selection bias early in our experience, where younger males were seen as a surrogate marker for better bone and therefore more suitable for uncemented TKA. These decisions reflect real-life decisions that all surgeons face when selecting adequate implants. As our experience improved with this implant, we started to include more females and older patients. At present, the senior author uses cementless implants in about 90% of their cases and the only contraindication is poor bone stock that cannot support cementless fixation. We included a multivariate regression analysis in order to control for this asymmetry, and it does not appear that gender influences the early revision rate. However, with small event numbers, there is the chance for error. In the future studies, the authors plan to analyse the results of uncemented TKA exclusively in a female population.
The time to follow-up is short by design. This is due to the recency of introduction of this implant to the market. It is imperative to rigorously assess any new orthopaedic implant with numerous short-term studies in order to identify any potential implant defects that may only come to light with the reporting of larger sample sizes. We will continue to report at longer follow-up intervals as well in the future to show ongoing performance of this implant which is important given that our study includes the largest single-centre cohort of the uncemented Triathlon TKA to date.
There were also significantly more PS implants in the cemented cohort. This is likely to reflect a surgeon preference, as the surgeons in our group were transitioning from a posterior stabilized design to a cruciate-retaining condylar stabilized design (CR-CS) when they transitioned from a previous manufacturer to the use of the Triathlon knee. The senior author; however had the largest cohort of cementless knees, and was the first to switch to almost exclusively CR-CS and was also the first to incorporate a larger proportion of cementless knees in his practice. This explains the difference in implant designs between the two cohorts. As our group’s practice has transitioned to primarily CR-CS, this will be controlled for in the future studies.
Conclusion
The Uncemented Triathlon TKA demonstrates excellent survivorship at short-term follow-up (24 months) when compared to the cemented Triathlon TKA, thus eliminating any potential short-term clinical concerns with this novel implant. Operative times are significantly shorter with the uncemented Triathlon. Further large-scale trials are needed to monitor the future performance of this implant and the utility of uncemented TKA in the future.
References
Barrack RL, Nakamura SJ, Hopkins SG, Rosenzweig S (2004) Winner of the 2003 James A. Rand young investigator’s award. Early failure of cementless mobile-bearing total knee arthroplasty. J Arthroplasty 19(7 Suppl 2):101–106
Batailler C, Malemo Y, Demey G, Kenney R, Lustig S, Servien E (2020) Cemented vs uncemented femoral components: a randomized, controlled trial at 10 years minimum follow-up. J Arthroplasty 35(8):2090–2096
Behery OA, Kearns SM, Rabinowitz JM, Levine BR (2017) Cementless vs cemented tibial fixation in primary total knee arthroplasty. J Arthroplasty 32(5):1510–1515
Bhimji S, Meneghini RM (2014) Micromotion of cementless tibial baseplates: keels with adjuvant pegs offer more stability than pegs alone. J Arthroplasty 29(7):1503–1506
Costales TG, Chapman DM, Dalury DF (2020) The natural history of radiolucencies following uncemented total knee arthroplasty at 9 years. J Arthroplasty 35(1):127–131. https://doi.org/10.1016/j.arth.2019.08.032
Dalury DF (2016) Cementless total knee arthroplasty: current concepts review. Bone Jt J 98-B(7):867–873
Gold PA, Garbarino L, Sodhi N, Barrack R, Springer BD, Mont MA (2020) The case for cementless total knee arthroplasty. Surg Technol Int 36:388–396
Hasan S, van Hamersveld KT, de Marang-van Mheen PJ, Kaptein BL, Nelissen R, Toksvig-Larsen S (2020) Migration of a novel 3D-printed cementless versus a cemented total knee arthroplasty: two-year results of a randomized controlled trial using radiostereometric analysis. Bone Jt J 102B(8):1016–1024
Hegarty P, Walls A, O’Brien S, Gamble B, Cusick L, Beverland DE (2020) A prospective randomized study comparing postoperative pain, biological fixation, and clinical outcomes between two uncemented rotating platform tibial tray designs. J Arthroplasty 35(2):429–437
Lizaur-Utrilla A, Miralles-Muñoz FA, Ruiz-Lozano M, González-Parreño S, Alonso-Montero C, Lopez-Prats FA (2020) Better clinical outcomes and overall higher survival with hybrid versus cemented primary total knee arthroplasty: a minimum 15 years follow-up. Knee Surgery Sports Traumatol Arthrosc Off J ESSKA. https://doi.org/10.1007/s00167-020-06028-y.Advanceonlinepublication.10.1007/s00167-020-06028-y
Lombardi AV Jr, Berasi CC, Berend KR (2007) Evolution of tibial fixation in total knee arthroplasty. J Arthroplasty 22(4 Suppl 1):25–29
Meneghini RM, de Beaubien BC (2013) Early failure of cementless porous tantalum monoblock tibial components. J Arthroplasty 28(9):1505–1508
Miller AJ, Stimac JD, Smith LS, Feher AW, Yakkanti MR, Malkani AL (2018) Results of cemented vs cementless primary total knee arthroplasty using the same implant design. J Arthroplasty 33(4):1089–1093
Nam D, Kopinski JE, Meyer Z, Rames RD, Nunley RM, Barrack RL (2017) Perioperative and early postoperative comparison of a modern cemented and cementless total knee arthroplasty of the same design. J Arthroplasty 32(7):2151–2155
Nugent M, Wyatt MC, Frampton CM, Hooper GJ (2019) Despite improved survivorship of uncemented fixation in total knee arthroplasty for osteoarthritis, cemented fixation remains the gold standard: an analysis of a national joint registry. J Arthroplasty 34(8):1626–1633
Salem HS, Tarazi JM, Ehiorobo JO, Marchand KB, Mathew KK, Sodhi N et al (2020) Cementless fixation for total knee arthroplasty in various patient populations: a literature review. J Knee Surgery 33(9):848–855
Sheridan GA, Garbuz DS, Masri BA (2021) Hybrid stems are superior to cemented stems in revision total knee arthroplasty: a systematic review and meta-analysis of recent comparative studies. Eur J Orthop Surgery Traumatol 31(1):131–141
Singh JA, Yu S, Chen L, Cleveland JD (2019) Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rheumatol 46(9):1134–1140
Sporer S, MacLean L, Burger A, Moric M (2019) Evaluation of a 3D-printed total knee arthroplasty using radiostereometric analysis: assessment of highly porous biological fixation of the tibial baseplate and metal-backed patellar component. Bone Jt J 101-B(7_Suppl_C):40–47
Yazdi H, Choo KJ, Restrepo C, Hammad M, Sherman M, Parvizi J (2020) Short-term results of triathlon cementless versus cemented primary total knee arthroplasty. Knee 27(4):1248–1255
Funding
There were no funding sources for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to report.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sheridan, G.A., Garbuz, D.S., Nazaroff, H. et al. Short-term results of the uncemented triathlon total knee arthroplasty: a large cohort single-centre comparative study. Eur J Orthop Surg Traumatol 33, 2325–2330 (2023). https://doi.org/10.1007/s00590-022-03422-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03422-9