Abstract
Purpose
To investigate (1) healthcare utilization, (2) in-hospital metrics and (3) total in-hospital costs associated with simultaneous versus staged BTKA while evaluating staged BTKA as a single process consisting of two combined episodes.
Methods
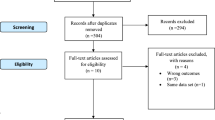
The national readmissions database was reviewed for simultaneous and staged (two primary unilateral TKAs12 months apart) BTKA patients (2016–2017). A total of 19,382 simultaneous BTKAs were identified, and propensity score matched (1:1) to staged BTKA patients (19,382 patients; 38,764 surgeries) based on demographics, comorbidities, and socioeconomic determinants. Outcomes included healthcare utilization [length of stay (LOS) and discharge disposition], in-hospital periprosthetic fractures, non-mechanical complications, and costs. Staged BTKA was evaluated as one process consisting of two episodes. For each staged patient, continuous outcomes were evaluated via the sum of both episodes. Categorical outcomes were added, and percents were expressed relative to total number of surgeries (n = 38,764).
Results
Simultaneous BTKA had longer LOS (5.0 days ± 4.7 vs. 4.5 days ± 3.5; p < 0.001), higher non-home discharge [36.9% (n = 7150/19,382) vs. 13.6% (n = 5451/38,764)], in-hospital periprosthetic fractures [0.13% (26/19,382) vs. 0.08% (31/38,764); p = 0.049], any non-mechanical complication [33.76% (6543/19,382) vs.15.93% (6177/38,764); p < 0.0001], hematoma/seroma formation [0.11% (22/19,382) vs. 0.05% (20/38,764); p = 0.0088], wound disruption [0.08% (16/19,382) vs. 0.04% (16/38,764); p = 0.0454], and any infection [1.13% (219/19,382) vs. 0.50% (194/38,764); p < 0.0001]. Average in-hospital costs for the two staged BTKA episodes combined were $5006 higher than those of simultaneous BTKA ($28,196 ± $18,488 vs. $33,202 ± $15,240; p < 0.001).
Conclusion
Simultaneous BTKA had higher healthcare utilization and in-hospital complications than both episodes of staged BTKA combined, with a minimal in-hospital cost savings. Future studies are warranted to further explore patient selection who would benefit from BTKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The United States continues to age yet with increasing functional demands and expectations [1]. This trend drives an anticipated exponential increase in demand for total knee arthroplasty (TKA), projected to exceed 85% by 2030[2]. TKA is the most effective pain relief and functional restoration option among individuals with end-stage knee osteoarthritis through providing, on average, a 0.17 increase in quality-adjusted life years [3,4,5]. Of this exponentially growing TKA patient population, Santana et al. [6] reported that 40% would require contralateral TKA within the ensuing eight years from the index surgery [6, 7]. Bilateral TKA (BTKA) has been advocated as an effective intervention to address osteoarthritis of both knee joints within a predefined time frame, thereby mitigating the potential for hindered functional improvement by unaddressed contralateral knee osteoarthritis. Based on the second TKA’s timing, BTKA can be categorized as simultaneous, which involves performing both procedures during the same surgical episode [5]; or staged, which affords patients a planned inter-surgical interval for recovery before the contralateral procedure [8].
Simultaneous BTKA has been associated with certain advantages such as the convenience of a single surgical intervention with a single exposure to anesthesia, and potential for mitigated cost [9,10,11]. In addition, recent investigations highlight non-inferiority in pain relief and patient satisfaction for simultaneous BTKA compared to unilateral and staged BTKA [11,12,13]. Nevertheless, there remains controversy regarding simultaneous BTKA’s safety profile. Several investigations have indicated a significant association between simultaneous BTKA and pulmonary embolism, deep vein thrombosis, superficial, deep, and prosthetic joint infection, increased length of stay, need for transfusion, early revision surgery, and mortality compared to its staged counterpart [4, 14,15,16]. Such increase in postoperative complications led Warren et al. [17] to conclude that simultaneous BTKA may not be safe even among the healthiest of patients.
However, investigations highlighting the high-risk profile predominantly utilize unilateral TKA comparison cohorts or analyze staged BTKA as two completely dissociated surgical episodes, which may misrepresent its bilateral nature. Such limitation derogated the conclusively of evidence outlining the more favorable safety profile of staged BTKA, thereby hindering a potentially widespread shift in clinical practice towards staged BTKA. Therefore, the present study aimed to investigate (1) healthcare utilization, (2) in-hospital metrics and (3) total in-hospital costs associated with simultaneous vs. staged BTKA while evaluating staged BTKA as a single process consisting of two combined episodes.
Methods
Study design and data source
The Agency of Healthcare Research and Quality’s (AHRQ’s) National Readmissions Database (NRD) was retrospectively queried for patients who received BTKA (January 2016–December 2017). The NRD is a nationally representative all-payer database and comprises hospitalization captured in the State Inpatient Database (SID). The NRD includes data from 28 SIDs across the nation and encompasses patients who have undergone one or more inpatient admission. Each patient is assigned a verified deidentified patient linkage number which facilitates tracking this patient from the initial hospitalization and up to one year postoperatively. Therefore, admission details, including surgical hospitalizations that occurred within one year from the index surgical episode, are captured. The NRD is a publicly available deidentified database; therefore, institutional review board approval was not required for the present investigation.
Data collection and population characteristics
All patients who received primary BTKA within the study period were eligible for inclusion. These patients were identified using ICD-10 codes (Appendix 1). Simultaneous BTKA patients were defined as those who received primary TKA on both knees during the same hospitalization. Conversely, patients who received staged BTKA were identified through isolating linkage numbers associated with two discrete hospitalizations for primary unilateral TKA. This was facilitated by NRD’s temporal capture of hospitalizations for each linkage number (indicative of a single patient) for one year from the index procedure. Patient demographics, baseline comorbidities, healthcare utilization (LOS and discharge disposition), hospitalization costs, and in-hospital complications were extracted for each patient.
A total of 27,555 simultaneous and 20,279 staged BTKAs were identified. Baseline characteristics of the prematched cohorts are detailed in Table 1. Propensity score matching (1:1) was performed to obtain similar cohorts of patients who received simultaneous (Patients: n = 19,382; surgeries: n = 19,382) and staged (patients: n = 19,382; surgeries: n = 38,704) BTKA (Table 2). Propensity score matching was based on age, sex, insurance, elective status, hospital details, income percentile, and Elixhauser comorbidity score, thereby eliminating differences in baseline determinants.
Outcome measures
In-hospital metrics included LOS, discharge disposition, and in-hospital complications [intra-/postoperative periprosthetic fractures and non-mechanical complications including shock, hematoma/seroma, infections, acute hemorrhagic anemia, blood transfusion, pulmonary embolism, deep venous thrombosis (DVT), respiratory failure, and unspecified system-wide complications] [18]. In-hospital costs reflected the actual expenses incurred during the surgical hospitalization. Such outcomes were captured for the duration of the TKA admission, corresponding to either one hospitalization for simultaneous BTKA or first and second primary TKA admissions for staged BTKA. A patient was considered to have received staged bilateral TKA if the second surgery occurred within 365 days of the initial TKA and was subsequently captured as a hospital admission within the NRD. The outcomes of interest were recorded for each surgical episode of staged BTKA, and combined to provide a “net” estimate of staged BTKA as a single entity rather than two independent surgeries.
Statistical analysis
Univariate analysis was conducted to compare the distribution of demographic determinants and healthcare settings among patients who received simultaneous versus staged BTKA. Propensity score matching (PSM) was performed on a nearest-neighbor, 1:1 basis and utilized a caliper of 0.1. Matched variables included age, sex, insurance status, elective status, income quartile, hospital details, and Exhauster comorbidity category [19]. Matching eliminated differences in baseline characteristics between both cohorts, as outlined in Table 2. All outcomes were compared between the propensity score-matched cohorts.
Continuous variables, including length of stay and in-hospital costs for patients who received simultaneous BTKA, were reported as the hospitalization duration/expenses associated with this single surgical episode. Similarly, categorical variables (discharge status and in-hospital complications) for simultaneous BTKA were those specific to this individual surgery. Conversely, continuous variables for each patient who underwent staged BTKA were recorded as a sum of both surgical episodes’ hospitalization duration/expenses. Categorical variables in staged BTKA were evaluated relative to both procedures, and percentages were reported relative to the total number of surgical episodes. This allowed for evaluating staged BTKA as a single entity despite consisting of two separate surgeries.
Continuous variables were assessed via means ± standard deviation (SD) and compared using independent 2-sample t tests. Categorical variables were evaluated via counts (%) and compared through chi-squared tests. All tests were 2-sided and statistical significance was set at an alpha-level of 0.05 (p < 0.05). All analyses were performed using SAS, v9.4 (SAS Institute, Cary, NC).
Results
In-hospital healthcare utilization associated with simultaneous versus staged BTKA
Simultaneous BTKA was associated with a longer length of stay (5.0 days ± 4.7 vs. 4.5 days ± 3.5; p < 0.0001), and higher non-home discharge rates (36.9% vs. 13.6%; p < 0.001) compared to staged BTKA (Table 3). The rates of intra-/perioperative periprosthetic fractures were significantly higher within the simultaneous BTKA cohort (0.13% vs. 0.08%; p = 0.0491). Simultaneous BTKA exhibited higher rates of any in-hospital non-mechanical complications (33.76% vs. 15.93%; p < 0.0001). Specifically, patients who received simultaneous BTKA had a higher incidence of developing hematomas/seromas (0.11% vs. 0.05%; p = 0.0088), wound dehiscence (0.08% vs. 0.04%; p = 0.0454), and any postoperative infection (1.13% vs. 0.50%; p < 0.0001) compared to patients who underwent staged BTKA. The simultaneous BTKA cohort demonstrated more than a two-fold increase in the incidence of acute post-hemorrhagic anemia (25.63% vs. 10.88%; p < 0.0001) and a seven-fold increase in blood transfusion rates (7.23% vs. 1.12%; p < 0.0001) compared to staged BTKA. Simultaneous BTKA demonstrated higher rates of system-specific complications, including the central nervous (0.33% vs. 0.18%; p = 0.0006), cardiac (9.23% vs. 5.56%; p < 0.0001), respiratory (0.54% vs. 0.15%; p < 0.0001), gastrointestinal (0.37% vs. 0.07%; p < 0.0001), and genitourinary (0.19% vs. 0.08%; p = 0.0003) systems.
Net in-hospital costs associated with simultaneous versus staged BTKA
Compared to the combined in-hospital costs of the two surgical episodes comprising the staged BTKA, the mean cost of a single surgical episode of simultaneous BTKA was $5006 less (simultaneous BTKA: $28,196 ± 18,488 vs. staged BTKA: $33,202 ± 15,240; p < 0.0001; Table 3).
Discussion
The safety, efficacy, and cost differential of performing BTKA in a single-episode as opposed to 2 staged procedures has been extensively debated [4, 20,21,22]. The use of simultaneous BTKA gained initial momentum owing to its elimination of a second surgery with the associated re-hospitalization, anesthesia, and recovery duration [10, 11, 23]. However, emerging evidence of simultaneous BTKA’s higher risk profile compared to unilateral TKA prompted surgeons to reassess its utility and value [17]. The present study utilized an extensive nationwide propensity score-matched sample and found that simultaneous BTKA exhibited longer LOS, higher rates of non-home discharge, intra-/perioperative periprosthetic fractures, and in-hospital non-mechanical complications including hematoma/seromas wound dehiscence, infection, and system-specific complications compared to both surgical episodes of staged BTKA combined.
Contemporary investigations question the safety of simultaneous BTKA. Warren et al. [17] retrospectively analyzed 30-day mortality and any complications using a cohort of 8291 patients who underwent bilateral TKA matched 1:1 by morbidity probability with a unilateral TKA control cohort (n = 315,219). The authors found that BTKA was associated with higher risk for all complications [odds ratio (OR): 3.58, 95% confidence interval (CI): 3.22–3.9; p < 0.001] and major complications (OR: 2.02, 95% CI: 1.66–2.47; p < 0.001) versus unilateral TKA regardless of health status. Furthermore, the incidence of mortality in unilateral TKA varied from 0.0% in the first quartile of comorbidity burden (least comorbidities) to 0.2% in the fourth quartile of comorbidity burden (highest comorbidities), while in simultaneous BTKA, it varied from < 0.1% in the first quartile to 0.2% in the fourth quartile. Similarly, Tsay et al. [5] analyzed 27,301 simultaneous and 45,419 staged BTKA patients from national discharge hospital data between 2005 and 2014 and found that simultaneous BTKA was associated with higher odds of mortality (OR: 1.36; 95% CI: 1.06–1.75; p = 0.015), myocardial infarction (OR: 2.74, 95% CI: 2.15–3.49; p < 0.001), ischemic stroke (OR: 2.33, 95% CI: 1.64–3.3); p < 0.001, cardiac complications (OR: 1.34; 95% CI: 1.16–1.55; p < 0.001), respiratory complications (OR: 1.26; 95% CI: 1.02–1.55; p = 0.034), digestive complications (OR: 1.91; 95% CI: 1.65–2.2; p < 0.001), urinary complications (OR: 1.37; 95% CI: 1.15–1.63; p < 0.001), hematoma formation (OR: 0.58; 95% CI: 0.47–0.7; p < 0.001) as well as deep infection (OR: 0.71; 95% CI: 0.6–0.85; p < 0.001) and major mechanical complications (OR: 0.75; 95% CI: 0.58–0.98; p = 0.036) up to one-year postoperatively. These findings were evident despite the better baseline health status of simultaneous BTKA recipients compared to their staged BTKA counterparts. Liu et al. [4] conducted recent systematic review of 18 studies comparing simultaneous (n = 73,617) staged (n = 61,838) BTKA. The authors found that simultaneous BTKA was associated with increased mortality (OR: 1.41; 95% CI: 1.10–1.80; p = 0.006), pulmonary embolism (OR: 1.39; 95% CI: 1.16–1.67; p < 0.001), and deep vein thrombosis (OR: 1.21; 95% CI: 1.06–1.39; p = 0.006) compared with staged BTKA. Notably, a stark limitation common to the aforementioned reports is the use of unilateral TKA (isolated unilateral or only the second surgical episode of the staged BTKA process) as a benchmark that is representative of staged BTKA. The present study’s findings demonstrate added value and increased safety with staged BTKA. As such, an approach that involved pre-planned staged procedures or one that addresses the more severely affected knee followed by a delayed “as-needed” intervention for a less severely impacted contralateral joint may be reasonable. The latter approach may be particularly feasible among bilateral knee osteoarthritis with substantially dissimilar involvement of both joints; a pattern frequently encountered in clinical settings. Indeed, among patients with dissimilar bilateral joint involvement, performing simultaneous BTKA routinely may promote potentially premature or even unnecessary contralateral TKA in up to 60% of patients. Therefore, future investigations are required to outline appropriate use criteria for performing simultaneous BTKA. Such criteria should account for extent of joint degeneration, pain/functional limitations, and patients’ comorbidity burden.
The present study found approximately a $5000 cost savings with simultaneous BTKA, which may be explained by the need for a single surgical episode compared to 2 discrete hospitalizations and surgical episodes with staged BTKA. However, this number does not account for the additional costs of non-home discharge (costs associated with residing in a skilled nursing facility or post-discharge institutional healthcare), which was found to be significantly higher among simultaneous BTKA recipients. Indeed, discharge to a skilled nursing facility has been shown to incur an average cost of $6620 as opposed to $3709 and $3241 for discharge to home and home health and home, respectively [24]. In addition, the cost differential demonstrated in the current study does not consider the additional management expenses, nor those incurred from readmission and/or reoperation secondary to postoperative complications. Notably, in a recent study by Kahlenberg et al. [25], the authors demonstrated significantly fewer total days of missed work for employed patients (17 fewer days of total missed work) with simultaneous BTKA as opposed to bilateral TKA in a staged fashion. As cost-effective high-value care provision is becoming a tenet of the U.S. healthcare system, future prospective investigations may be warranted to analyze the financial implications of both surgeries while accounting for the multitude of peri- and postoperative expenses and sources of lost income [26,27,28].
There are several limitations to the current investigation. First, the retrospective nature of our database study confers some selection biases. However, given the large sample size and data from patients nationwide, coupled with the propensity score matching process performed to eliminate differences between cohorts, we anticipate that these biases are unlikely to impact the study’s findings. Notably, given the large sample size, some findings may demonstrate statistical significance despite having limited clinical relevance. The present study leveraged nationwide data from the National Readmissions Database (NRD) [29]. Patient records in this dataset are matched by linkage numbers associated with each episode of care and provide up to one year follow-up. Therefore, the present study was limited to capturing hospitalizations only up to one year following the index procedure, and repeat hospitalizations beyond this timeframe may be missed. Finally, the present study did not analyze differences in patient-reported outcomes, functional or pain scores, thus comparing only discharge state, complication profile, and cost associated with stage bilateral versus simultaneous TKA. However, we aimed to highlight multiple important complications occurring at significantly higher rates with simultaneous bilateral TKA compared to staged TKA as well as cost comparison between staged versus simultaneous bilateral TKA.
Simultaneous BTKA is associated with a higher risk profile than staged BKTA. Specifically, the simultaneous bilateral procedures confer higher healthcare utilization and in-hospital complications than both episodes of staged BTKA combined. Total in-hospital costs are higher in staged BTKA owing to the need for two discrete hospitalizations and surgical episodes. However, such cost differential may be offset by simultaneous BTKA’s post-discharge expenses, evidenced by its higher non-home discharge and overall complication rates. Therefore, simultaneous BTKA should be considered as the exception rather than the rule. Further prospective investigations are warranted to investigate the net cost differential between both surgeries while accounting for post-discharge expenses, rehabilitation cost, and the value of missed workdays (missed income).
References
Pallin DJ, Espinola JA, Camargo CAJ (2014) US population aging and demand for inpatient services. J Hosp Med 9:193–196. https://doi.org/10.1002/jhm.2145
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Jt Surg Am 100:1455–1460. https://doi.org/10.2106/JBJS.17.01617
Konopka JF, Lee Y-Y, Su EP, McLawhorn AS (2018) Quality-adjusted life years after hip and knee arthroplasty: health-related quality of life After 12,782 joint replacements. JBJS open access 3:e0007–e0007. https://doi.org/10.2106/JBJS.OA.18.00007
Liu L, Liu H, Zhang H et al (2019) Bilateral total knee arthroplasty: Simultaneous or staged? A systematic review and meta-analysis. Medicine (Baltimore) 98:e15931. https://doi.org/10.1097/MD.0000000000015931
Grace TR, Tsay EL, Roberts HJ et al (2020) Staged bilateral total knee arthroplasty: increased risk of recurring complications. J Bone Jt Surg Am 102:292–297. https://doi.org/10.2106/JBJS.19.00243
Santana DC, Anis HK, Mont MA et al (2020) What is the likelihood of subsequent arthroplasties after primary TKA or THA? Data from the osteoarthritis initiative. Clin Orthop Relat Res 478:34–41. https://doi.org/10.1097/CORR.0000000000000925
McMahon M, Block JA (2003) The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol 30:1822–1824
Latifi R, Thomsen MG, Kallemose T et al (2016) Knee awareness and functionality after simultaneous bilateral versus unilateral total knee arthroplasty. World J Orthop 7:195–201. https://doi.org/10.5312/wjo.v7.i3.195
Patil N, Wakankar H (2008) Morbidity and mortality of simultaneous bilateral total knee arthroplasty. Orthopedics 31:780–781. https://doi.org/10.3928/01477447-20080801-23
Stubbs G, Pryke SER, Tewari S et al (2005) Safety and cost benefits of bilateral total knee replacement in an acute hospital. ANZ J Surg 75:739–746. https://doi.org/10.1111/j.1445-2197.2005.03516.x
Odum SM, Springer BD (2014) In-hospital complication rates and associated factors after simultaneous bilateral versus unilateral total knee arthroplasty. J Bone Jt Surg Am 96:1058–1065. https://doi.org/10.2106/JBJS.M.00065
Ritter MA, Harty LD, Davis KE et al (2003) Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Jt Surg Am 85:1532–1537. https://doi.org/10.2106/00004623-200308000-00015
Kim Y-H, Choi Y-W, Kim J-S (2009) Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Jt Surg Br 91:64–68. https://doi.org/10.1302/0301-620X.91B1.21320
Lindberg-Larsen M, Pitter FT et al (2019) Simultaneous versus staged bilateral total knee arthroplasty: a propensity-matched case–control study from nine fast-track centres. Arch Orthop Trauma Surg 139:709–716. https://doi.org/10.1007/s00402-019-03157-z
Restrepo C, Parvizi J, Dietrich T, Einhorn TA (2007) Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Jt Surg Am 89:1220–1226. https://doi.org/10.2106/JBJS.F.01353
Fu D, Li G, Chen K et al (2013) Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: a systematic review of retrospective studies. J Arthroplast 28:1141–1147. https://doi.org/10.1016/j.arth.2012.09.023
Warren JA, Siddiqi A, Krebs VE et al (2021) Bilateral simultaneous total knee arthroplasty may not be safe even in the healthiest patients. J Bone Jt Surg Am 103:303–311. https://doi.org/10.2106/JBJS.20.01046
Klika AK, Myers T, Szubski CR et al (2015) Early postoperative outcomes of primary total knee arthroplasty after solid organ transplantation in the United States, 1998–2011. J Arthroplast 30:1716–1723. https://doi.org/10.1016/j.arth.2015.04.044
Menendez ME, Neuhaus V, van Dijk CN, Ring D (2014) The elixhauser comorbidity method outperforms the charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res 472:2878–2886. https://doi.org/10.1007/s11999-014-3686-7
Richardson SS, Kahlenberg CA, Blevins JL et al (2019) Complications associated with staged versus simultaneous bilateral total knee arthroplasty: an analysis of 7747 patients. Knee 26:1096–1101. https://doi.org/10.1016/j.knee.2019.06.008
Taylor BC, Dimitris C, Mowbray JG et al (2010) Perioperative safety of two-team simultaneous bilateral total knee arthroplasty in the obese patient. J Orthop Surg Res 5:38. https://doi.org/10.1186/1749-799X-5-38
Makaram NS, Roberts SB, Macpherson GJ (2021) Simultaneous bilateral total knee arthroplasty is associated with shorter length of stay but increased mortality compared with staged bilateral total knee arthroplasty: a systematic review and meta-analysis. J Arthroplast 36:2227–2238. https://doi.org/10.1016/j.arth.2021.01.045
Hutchinson JRM, Parish EN, Cross MJ (2006) A comparison of bilateral uncemented total knee arthroplasty: simultaneous or staged? J Bone Jt Surg Br 88:40–43. https://doi.org/10.1302/0301-620X.88B1.16454
Zeng F, Waldo D (2016) Total knee arthroplasty post acute care costs by discharge status. Value Heal 19:A13–A14. https://doi.org/10.1016/j.jval.2016.03.273
Kahlenberg CA, Krell EC, Sculco TP et al (2021) Differences in time to return to work among patients undergoing simultaneous versus staged bilateral total knee arthroplasty. Bone Jt J 103-B:108–112. https://doi.org/10.1302/0301-620X.103B6.BJJ-2020-2102.R1
Macario A, Schilling P, Rubio R, Goodman S (2003) Economics of one-stage versus two-stage bilateral total knee arthroplasties. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000079265.91782.ca
Houdek MT, Wyles CC, Watts CD et al (2017) Single-anesthetic versus staged bilateral total hip arthroplasty: a matched cohort study. J Bone Jt Surg Am 99:48–54. https://doi.org/10.2106/JBJS.15.01223
Grove A, Johnson R, Clarke A, Currie G (2016) Evidence and the drivers of variation in orthopaedic surgical work: a mixed methods systematic review. Heal Syst Policy Res 3:6. https://doi.org/10.21767/2254-9137.100025
Tripathi A, Abbott JD, Fonarow GC et al (2017) Thirty-day readmission rate and costs after percutaneous coronary intervention in the United States: a national readmission database analysis. Circ Cardiovasc Interv. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005925
Funding
No source of funding was required for the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AKE, ME, AKK, GJ, and SK have nothing to disclose. NSP has the following disclosures, none of which are related to the topic of the present study: American Association of Hip and Knee Surgeons: Board or committee member. ISCT: Board or committee member. Journal of Hip Surgery: Editorial or governing board. Journal of Knee Surgery: Editorial or governing board. Orthopaedic Research Society: Board or committee member. Regeneron: Paid consultant. RegenLab: Research support. Stryker: Paid consultant. Zimmer: Research support. RMM has the following disclosures none of which are related to the topic of the present study: American Association of Hip and Knee Surgeons: Board or committee member. Stryker: Paid consultant; Paid presenter or speaker; Research support. Zimmer: Research support.
Ethical statement
The present study utilized a publicly available deidentified database; therefore, institutional review board approval was not required. All research activities conformed to the Helsinki Accord (1964) and all subsequent amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Erossy, M., Emara, A.K., Zhou, G. et al. Simultaneous bilateral total knee arthroplasty has higher in-hospital complications than both staged surgeries: a nationwide propensity score matched analysis of 38,764 cases. Eur J Orthop Surg Traumatol 33, 1057–1066 (2023). https://doi.org/10.1007/s00590-022-03248-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03248-5